Abstract
In the 5 years since the cloning of the cystic fibrosis (CF) gene, several experimental trials of CF carrier screening have been performed and reported. Two particular groups have been targetted: young adults near reproductive age, and pregnant women. The three trials directed at young adults have shown that the method of presentation is a major determinant of take-up rates; an offer of screening by personal intervention gives high acceptance while an offer by mail or leaflet produces disappointing results. There is a strong suggestion that screening is being foisted on an unreceptive group, whose response is one of politeness rather than conviction — ‘supply push’ rather than ‘demand pull’. Trials of screening during pregnancy have been more extensive and more satisfactory. Two models have been tested. In sequential delivery, women are screened first and their partners only tested when they are found positive for CF alleles. This can lead to anxiety, during the period while positive women await their partner’s result. In couple screening both partners agree to be treated as a unit and reported as high risk only when both are positive. In other situations they are regarded as negative. Couple screening has turned out to be remarkably efficient, trouble-free and consumer-friendly, and has become the method of choice for integration into routine health care.
Similar content being viewed by others
Introduction
When the cystic fibrosis (CF) gene was cloned in 1989, two radical new approaches to the management of the disease became possible. The most important was the prospect of somatic gene therapy. In this area the scientific advances have been astonishingly rapid, and preliminary clinical trials are underway in several major centres [1,2]. However, the public perception of gene therapy is that it is fraught with unknown dangers, and that treatment of patients must therefore be carried out with the types of safeguard not required for conventional drug testing. Recruits for gene therapy trials have tended to be older patients with relatively advanced disease where the assessment of benefit is difficult. Inevitably, this means that it will be some time before it is possible to make any real judgement of whether gene therapy works and to what extent it can prevent or slow the progress of the lung damage that is a source of most of the morbidity and mortality in CF.
An alternative and complementary approach is to try and reduce the number of CF births by the early recognition of parental heterozygosity. As CF is an autosomal recessive disorder, it has been natural to see heterozygote screening as aimed at the detection of individuals with a single copy of a mutant CF allele. In many parts of Europe and North America this may represent between 2 and 4% of the population. However, CF heterozygosity is a harmless trait which only assumes significance in the context of a planned or actual pregnancy. At this point it is the carrier couple who is at risk. Of course, it can be argued that early knowledge of individual carrier status allows people to choose courses of action that avoid an affected child. In practice, the experience with other autosomal recessive disorders, such as Tay-Sachs disease [3], β-thalassaemia [4] and sickle cell anaemia [5], suggests that these alternatives are seldom exercised. The usual response of those who find themselves at risk of bearing a child with a recessive disorder is to stay with their chosen partner and to ask for prenatal diagnosis and a monitored pregnancy.
The probability that CF heterozygote testing would be closely tied to prenatal diagnosis has influenced the discussion of when to perform screening. One school of thought argues that the most effective time is during pregnancy, for only then will it be possible to focus the minds of the general population on the risks of carrier status. The alternative view is that screening during pregnancy places an unacceptable burden of decision making on a susceptible and captive group, and that attempts must be made to permit individuals to make up their minds about the implications of carrier status before they embark on a pregnancy.
In order to try and resolve these issues, several experimental trials of CF carrier screening have been performed and reported. Although no final conclusions have yet been reached, the results that have emerged have provided firm data on the acceptability and take-up rates of the different models.
Allelic Heterogeneity
Soon after the CF gene was cloned it became apparent that screening for heterozygosity could not be carried out on the gene product, the CF transmembrane conductance regulator, since it was not expressed in any readily accessible tissue [6]. In contrast to the experience with Tay-Sachs disease, β-thalassaemia and sickle cell anaemia, testing would have to be based on genotype rather than phenotype analysis. Furthermore, in virtually every major population group analysed, the CF gene showed considerable allelic heterogeneity [7]. Centres contemplating screening had therefore to survey their local population for the nature and frequency of CF alleles, and then to calculate how many of these it was possible to cover in laboratory analyses. This in turn was determined by the size of the population to be screened. It is easy to assay for 20 or 30 mutant alleles if the only subjects are a small group of high-risk individuals. With available gene technology it is much more difficult to assay for more than a handful of CF alleles if any substantial through-put of samples is to be achieved.
In only a few populations has it been possible to define the majority of segregating CF alleles. However, in most of the centres that have run trials on screening, there has been acceptance that only 85–90% of CF alleles could realistically be analysed. Inevitably this creates a problem for couples where one partner carries a mutant allele while the other does not. Such ‘positive-negative’ couples have a residual risk of bearing a CF child which depends on the proportion of CF alleles detectable and the incidence of the disorder (table 1). For groups with a birth incidence above 1 in 2,500, the residual risk for a positive-negative couple only falls below the population risk when over 96% of CF alleles are analysable. The American Society of Human Genetics took the view that this should be the target detection figure before any population screening programmes were initiated [8]. Others felt that this was an impossible precondition, and pointed to the success of established screening programmes at substantially lower sensitivities [9]. It was argued that provided those undergoing screening were carefully informed of the imperfect nature of the testing process, the potential for reducing the chances of an affected child was such as to legitimise CF heterozygote screening.
Screening at School Age
Although it makes sense to time the CF carrier test as close to pregnancy as possible, there are also theoretical advantages in directing screening at children of high school age. Scriver and his colleagues [10, 11] had demonstrated that this worked well for Tay-Sachs and β-thalassaemia screening in Montreal schools. The whole concept of genetic risk could be tied into an imaginative programme of biology teaching. In a small pilot study aimed at ascertaining CF heterozygotes in Montreal high schools in 1991, they showed a take-up rate of 42% [12]. Response to a questionnaire soliciting participants’ attitudes to the project suggested overwhelming (96%) approval of the concept of genetic screening in high schools. However, it was conceded that these were not necessarily typical attitudes, and Scriver and Clow [13] have stated that school age carrier screening for Tay-Sachs disease would probably not work as well elsewhere. In the United Kingdom, for example, a Working Party of the Clinical Genetics Society [14] has recommended against testing children for their carrier status where this would be of purely reproductive significance to the child in the future.
Largely for these reasons, the major pilot programmes of CF heterozygosity testing which have been reported have been concerned with adults. The issue has been whether to screen before or during pregnancy.
Screening before Pregnancy
In many respects screening young adults at a time when they are beginning to think about their reproductive future is the ideal programme. It is the most compatible with the principle of individual autonomy. An identified carrier has a variety of options. She can ignore the information, select an appropriate mating partner, have artificial insemination by a screened donor, forego reproduction or have a pregnancy monitored by prenatal diagnosis. Even when the last option is chosen, there is time for considered reflection of how to react to an affected pregnancy.
The first pilot trials of CF carrier screening through primary health care services were carried out in London and produced some unsettling results. Williamson’s group [15] showed that the method of presentation was critical in determining take-up rates. When the offer of screening was made opportunistically and in person by a dedicated member of the research team, between 66 and 87% of those approached agreed to be tested. In contrast, when presentation was by an invitation letter, the take-up rate was only 10%. This was confirmed by Bekker et al. [16] in another study carried out in general practitioner surgeries. When there was direct contact between those offering the test and those to who it was offered, and the possibility of immediate testing, the acceptance rate was 70%. For all other methods of presentation participation was feeble. Bekker et al. [16] concluded that the most important variable determining participation rates in screening was the personal approach by a professional and the offer of immediate carrier testing.
Similar conclusions have now emerged from a study in the USA. Tambor et al. [17] offered carrier testing to reproductive-age enrollees in a Health Maintenance Organisation in the Baltimore area. When letters were sent to the 18 to 44 age band, inviting participation in a free trial but also demanding attendance at a pretesting educational session, the response was 3.7%. In contrast, when counsellors approached patients who were already in the waiting room for an appointment, and carried out explanation of the test on the spot, the overall test utilisation was 23.5%.
The implications of these three pilot trials (table 2) are obvious. In order to achieve respectable participation rates in individual-directed CF carrier screening programmes, some form of personal explanation of the purposes and achievements of screening has to be made. Letters and leaflets will not suffice. The cost consequences of this degree of professional staff involvement are considerable. It is no surprise that none of the programmes of primary care screening appear to have survived the trial period.
Screening during Pregnancy
In the many countries most pregnant women attend antenatal clinics during their confinement. Such clinics, whether in hospitals, community centres or private offices, represent ‘turnstiles’ where the offer of heterozygote testing for CF may be efficiently made. Furthermore, following the success of biochemical screening for the detection of fetal neural tube defects and Down syndrome, pregnancy screening has become a fairly routine aspect of antenatal care. Heterozygote screening may therefore be added to existing programmes with minimal input of additional staff.
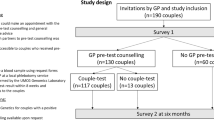
Two different, but not mutually exclusive, types of screening for CF during pregnancy have been proposed: ‘sequential’ and ‘couple’. In the sequential model the woman is tested first and her partner involved only if she is positive. (Although both partners can be screened simultaneously, this effectively doubles the number of tests carried out and renders the whole operation uneconomic.) It is therefore possible in principle for a woman to be tested while her partner refuses to participate. In contrast, in the couple model each partner must provide a sample before testing begins. For 95% of couples only one partner need be tested, since a negative result on the first sample means that the couple cannot be at high risk.
A large trial of sequential screening in antenatal clinics was reported by Mennie et al. [18, 19]. The offer of testing was made by a specially designed leaflet sent with a booking clinic appointment at an early stage of pregnancy. Women agreeing to participate were tested for six mutant CF alleles, representing 85% of CF chromosomes. If positive, the partner was also tested. No action was taken when a woman was negative, or if she were positive and her partner negative. Prenatal diagnosis was offered to couples where both partners were identified carriers. The take-up rate of screening among the 7,011 women offered testing was 83% for the eligible group (table 3), and 71% for all women attending the clinic. Only 1 of the 190 carriers identified was unable to persuade her partner to undergo testing. Each of the seven 1 in 4 risk couples elected to undergo prenatal diagnosis. One couple had 2 successive pregnancies with an affected fetus, and in each case the pregnancy was terminated and the diagnosis confirmed.
Similar results have been reported for a Danish population where ‘more than 80%’ of 3,054 women accepted the offer of screening [20]. In a small study in East Berlin, where screening was offered to 638 women, there was only one refusal [21]. This extraordinary programme attracted adverse editorial cornmen [22] in the journal in which it was published!
Sequential screening has been shown to generate moderate anxiety amongst women found to be positive for CF alleles during the period (average 4 days) of waiting for their partner’s test result. Quantitative measures of this stress, using several different psychological instruments, proved that it was of short duration and did not return later in pregnancy. However, there was a need for specialist counselling during the waiting period and this has cost implications for sequential screening. Furthermore, there was a strong sense among the obstretricians taking part in the programme that additional anxiety generated during pregnancy should be avoided.
An alternative to the sequential process is to treat the screening unit as the couple [23]. Positive couples are those where both partners carry a CF allele, while negative couples are those where only one partner is tested or where both partners are tested and only one found to be a carrier. While sequential screening leads to two types of screen-negative couple — a large group with a low risk and a smaller group with an intermediate risk — couple screening produces a single-class of screen-negative couple, whose composite risk is satisfactorily low (fig. 1). Because, in a majority of cases, it is only necessary to test one sample from a couple, the number of assays performed is no different to that in sequential screening.
The initial response to the idea of couple screening was to question its ethical basis. There is something disturbing about the deliberate withholding of genetic information. Discussion on this point was eventually resolved by it being pointed out that there is no moral imperative to disclose a risk situation for which no ameliorating action is possible. Because of the incomplete nature of CF heterozygosity testing, ‘positive-negative’ couples have a risk of bearing a CF child that is higher than the population risk. However, as there is nothing practical that can be done to reduce this risk, it is in the individual’s interest that he or she should not be forced to confront his or her carrier status. If the information is sought, it is freely disclosed; if not sought, it is not volunteered.
On this basis an extended trial of couple screening in the antenatal clinics of two Edinburgh maternity hospitals [24, 25] shows that the take-up rates are little different to those encountered in sequential screening (table 4). Some 76% of eligible couples participated, while the figure for the overall group was 69%. There was little sign that participants wished to know their individual carrier status. The data was freely available either in the obstetric notes or on application to the screening coordinator; only 1.5% of participants sought this information. Couple screening is a remarkably easy and trouble-free mode of delivery of carrier testing, and has become the method of choice in Edinburgh maternity hospitals. Wald et al. [26] have also reported a satisfactory 68% take-up of couple screening in an antenatal clinic in Oxford.
One of the problems of screening in antenatal clinics is that the time of first booking may be too late to allow necessary action to be taken in the first trimester of pregnancy. Harris et al. [27] have suggested that this problem can be circumvented if general practitioners offer heterozygote testing to women at the time of a positive pregnancy test. A pilot trial claimed that this was a viable option, although no data on take-up rates were provided. However, it was pointed out that there are 33,839 general practitioners in the United Kingdom, and the chance of persuading a reasonable number of these to participate in CF screening seems improbable. At best, such screening must be seen as a useful adjunct to more generally applicable programmes.
In the USA, where antenatal care is usually managed by private physicians, there has been a brief trial of delivering CF couple screening. This was to counter the suggestion that the couple concept, with non-disclosure of individuals’ carrier status, was unacceptable in an American context. Doherty et al. [28] reported that the take-up of screening in a decentralised primary care setting was greater than 50%.
Ancillary Testing
When a woman is at increased risk of bearing a child with a congenital abnormality and undergoes invasive and potentially hazardous procedures such as amniocentesis or choronic villus biopsy, it can be argued that she is entitled to obtain maximum information from the process. Two trials have investigated grafting CF testing onto more routine prenatal tests. Schwartz et al [20] offered heterozygote testing to 3,545 women about to undergo first-trimester prenatal diagnosis usually because of advanced maternal age, and recorded an acceptance rate of 98%. Instead of screening mothers and fathers for heterozygosity, Brambati et al. [29] chose to test the fetal sample in 780 pregnancies undergoing first and early second-trimester transabdominal chorionic villus sampling. The acceptance rate was 98%. One affected fetus was detected as well as 12 who were apparently heterozygous for the ΔF508 allele. However, in two of the latter cases termination of pregnancy was requested. A worrying aspect of this type of ancillary testing is that women at a heightened state of anxiety may not be able to accept CF heterozygosity in their fetus as normal.
Testing Families by Cascade
In many genetic centres CF heterozygosity testing is now available to the first- and second-degree relatives of an index affected proband. Usually such testing is a response, after counselling, to an individual’s request. An alternative and more pro-active approach has been proposed by Super et al. [30], who suggest taking screening into the wider population by ‘cascading’ through the relatives of index cases. They argue that there are many advantages to cascade testing: the ratio of carriers detected to people tested will be higher, assays can be restricted to the mutant alleles in the index case, and less anxiety will be generated among the screened population.
In a pilot trial in the Manchester area, Super et al. [31] carried out CF heterozygosity testing on 1,563 relatives and partners in 129 index families with an affected proband. In this group they identified 15 heterozygous couples, in 8 of whom prenatal diagnosis was carried out. By extrapolating to a total of 10,000 relatives and partners, it was suggested that 100 heterozygous couples would be detected and thus 25 affected fetuses found. It was claimed that this is equal to the number of CF children born annually in their region, and that pro-active cascade testing was a genuine substitute for population screening.
However, inspection of the data does not support the claim. Among the relatives tested no less than 427/1,122 (38%) were carriers. Thus the study was obviously concentrating predominantly on first-degree relatives. In the next phase, as the cascade moves to more distant relatives of the index case, the proportion of carriers detected will drop. It is misleading to extrapolate the proportion of heterozygous couples found in the easy part of the programme to more difficult parts. Furthermore, it cannot be assumed that all heterozygous couples would be planning pregnancies, or that all would seek prenatal diagnosis and act on the results. In fact of the 15 heterozygous couples in the study, 1 had completed their family and another 5 did not request prenatal diagnosis.
It is impossible to measure the theoretical effectiveness of cascade testing by simple extrapolation. Models need to be created, with family size distributions and alternative testing strategies. Our own projections [32], using different models, show that the cascade needs to reach the fourth cousin level (fig. 2) to achieve the same cover as population screening. Most people have difficulty in remembering the names and addresses of their first cousins. Even if the cascade is restricted to second cousin level it would only detect between 10 and 25% of heterozygous couples (depending on the model assumed). In contrast, it has been demonstrated that over 50% of heterozygous couples can be detected by either of the two major forms of antenatal screening [18,25].
There is no doubt that cascade testing is an effective way of identifying large numbers of carriers and carrier couples with a great deal less effort than in any standard population screening. However, it could also be argued that restricting maternal serum α-fetoprotein testing to mothers who had already had a child with a neural tube defect would increase the proportion of positive tests. Neither programme would be screening in the conventional sense of the word, nor would either have the necessary impact on the birth incidence of affected cases. Thus cascade testing may be seen as a useful adjunct to population screening but certainly not as a substitute for it.
Psychological Aspects of Screening
It has been suggested that the institution of poorly prepared screening programmes can lead to considerable harm [33]. Although negative test results are usually reassuring, positive results may lead to loss of self-esteem and worries about future health. Experience in another autosomal recessive disorder has been gained from Tay-Sachs disease screening programmes amongst Jewish communities. McQueen [34] reported that 45% of participants claimed that it would matter a great deal if they were found to be gene carriers, despite the recessive nature of the disease. Zeesman et al. [10] found that some 8 years after a screening programme, 19% of carriers were anxious about their status. Marteau et al. [15] reported similar data; Tay-Sachs disease carriers were in general less optimistic about their future health than control groups. It was thought that the problem lay in a poor level of understanding of what it really meant to be a carrier of a recessive disease.
This issue is relevant to programmes of CF screening. An added complexity is that those who test negative for CF alleles still have a substantial residual risk of carrier status — at an 85% detection rate the chance of being a carrier declines from 1 in 25 to 1 in 167. The lack of sensitivity in CF testing was a prime factor in leading the NIH Workshop on Population Screening for the Cystic Fibrosis Gene to advocate that no mass programmes of heterozygote testing should be carried out until carefully conducted pilot studies were complete. This advice was repeated in a Statement of the American Society of Human Genetics [36].
The caution in North American circles may well be a product of understandable worries about medicolegal action. In the UK a more robust approach to screening has been adopted, with the influential local Cystic Fibrosis Trust soliciting bids for pilot trials. A factor in this decision was the awareness that population attitudes to CF heterozygote screening have been generally favourable. Before the gene was cloned, Williamson et al. [37] found that 84% of a mixed London population answered ‘yes’ to the question ‘given that cystic fibrosis is an inherited disease and that a healthy person may unknowingly carry it and pass it on to his/her children, would you want to know if you were a carrier?’ In a later study, Williamson [38] stated that when several hundred students between 16 and 20 were asked whether they wished to be screened for CF carrier status, 90% said the test should be available to those who request it and 70% stated that they wished to be tested themselves. Similar attitudes amongst the general public have been recorded in Holland [39] and in Belgium [40]. Even amongst CF families, where a more ambivalent attitude to screening might be anticipated, opinion has been strongly in favour of population screening [41, 42].
Completed pilot trials now make it possible to ask whether screening has had harmful consequences. In a programme carried out in primary care, Watson et al. [43] found that 81% of carriers were glad that they had been tested, and although varying degrees of anxiety were found to be initially associated with a positive result, most of this was allayed by genetic counselling with no adverse long-term psychological consequences. At 6 months after the test 55% of carriers reported that they were not worried. A large proportion (87%) of partners of carriers were also tested. In this group it was difficult to ascertain attitudes to future reproduction; however, significantly fewer individuals in ‘at-risk’ partnerships felt that they would refrain from having children after testing and counselling than before. This may be the consequence of an increased awareness of the availability of prenatal diagnosis or simply that carriers now give more concerted thought to potential risks in future pregnancies.
Carrier testing during pregnancy, particularly using the two-step mode of delivery, might be expected to generate some anxiety. Mennie et al. [44] showed that this was of comparatively short duration with a reversion to the normal state by the time that the partner was tested. Partners of identified female carriers also showed some stress, but again this was of short duration [45]. Most of the participants in this study reported that they were glad that they had taken the carrier test and asserted that it should be offered routinely to all pregnant women [46]. The experience with couple antenatal screening is, as expected, even more favourable, with a high degree of satisfaction expressed by participants [25].
References
Zabner J, Couture LA, Gregory RJ, Graham SM, Smith AE, Welsh MJ: Adenovirus-mediated gene transfer transiently corrects the chloride transport defect in nasal epithelia of patients with cystic fibrosis. Cell 1993;75:207–216.
Crystal RG, McElvaney NG, Rosenfield MA, Chu C, Mastrangeli A, Hay JG, Brody SL, et al: Administration of an adenovirus containing the human CFTR cDNA to the respiratory tract of individuals with cystic fibrosis. Nature Genet 1994; 8:42–51.
Kaback MM, Nathan TJ, Greenwald S: Tay-Sachs disease: Heterozygote screening and prenatal diagnosis — US experience and world perspective; in Kaback MM (ed): Tay-Sachs Disease: Screening and Prevention. New York, Liss, 1977, pp 13–36.
Modell B, Berdoukas V: The Clinical Approach to Thalassaemia. London, Grune & Stratton, 1984, pp 354–378.
Bowman JE: Invited editorial: Prenatal screening for hemoglobinopathies. Am J Hum Genet 1991;48:433–438.
Riordan JR, Rommens JM, Kerem B, et al: Identification of the cystic fibrosis gene: Cloning and characterisation of complementary DNA. Science 1989;245:1066–1073.
The Cystic Fibrosis Genetic Analysis Consortium: Worldwide survey of the ΔF508 mutation. Am J Hum Genet 1990;47:354–359.
Workshop on Population Screening for the Cystic Fibrosis Gene: Statement from the National Institutes of Health Workshop on population screening for the cystic fibrosis gene. New Engl J Med 1990;323:70–71.
Brock DJH: Population screening for cystic fibrosis. Am J Hum Genet 1990;47:164–165.
Zeesman S, Clow CL, Cartier L, Scriver CR: A private view of heterozygosity: Eight-year follow-up study on carriers of the Tay-Sachs gene detected by high-school screening in Montreal. Am J Med Genet 1984;18:769–778.
Scriver CR, Bardanis M, Cartier L, et al: β-Thalassaemia disease prevention: Genetic medicine applied. Am J Hum Genet 1984;35:1024–1038.
Kaplin F, Clow C, Scriver CR: Cystic fibrosis carrier screening by DNA analysis: A pilot study of attitudes among participants. Am J Hum Genet 1991;49:240–242.
Scriver CR, Clow CL: Carrier screening for Tay-Sachs disease. Lancet 1991;336:191.
Working Party of the Clinical Genetics Society (UK): The genetic testing of children. J Med Genet 1994;31:785–797.
Watson EK, Mayall E, Chappell J, et al: Screening for carriers of cystic fibrosis through primary health care services. Br Med J 1991;303:504–507.
Bekker H, Modell M, Denniss G, et al: Uptake of cystic fibrosis testing in primary care: Supply, push or demand pull? Br Med J 1993;306:1584–1586.
Tambor ES, Bernhardt BA, Chase GA, Faden RR, Geller G, Hofman KJ, Holtzman NA: Offering cystic fibrosis screening in an HMO population: Factors affecting utilization. Am J Hum Genet 1994;55:626–637.
Mennie ME, Gilfillan A, Compton M, Curtis L, Liston WA, Pullen I, Brock DJH: Prenatal screening for cystic fibrosis. Lancet 1992;340:214–216.
Mennie ME, Liston WA, Brock DJH: Prenatal cystic fibrosis carrier testing: Designing an information leaflet to meet the specific needs of the target population. J Med Genet 1992;29:308–312.
Schwartz M, Brandt NJ, Skovby F: Screening for carriers of cystic fibrosis among pregnant women; a pilot study. Eur J Hum Genet 1993;1:239–244.
Jung U, Urner U, Grade K, Coutelle C: Acceptability of carrier screening for cystic fibrosis during pregnancy in a German population. Hum Genet 1994;94:19–24.
Schmidtke J: Proceed with more caution. Hum Genet 1994;94:24–27.
Wald NJ: Couple screeening for cystic fibrosis. Lancet 1991;338:1318–1319.
Livingstone J, Axton RA, Mennie M, Gilfillan A, Brock DJH: A preliminary trial of couple screening for cystic fibrosis: Designing an appropriate information leaflet. Clin Genet 1993;43:57–62.
Livingstone J, Axton RA, Gilfillan A, Mennie ME, Compton M, Brock DJH: Antenatal screening for cystic fibrosis: A trial of the couple model. Br Med J 1994;308:1459–1462.
Wald NJ, George LM, Wald NM, MacKenzie IZ: Couple screening for cystic fibrosis. Lancet 1993;342: 1307–1308.
Harris H, Scotcher D, Hartlie N, et al: Cystic fibrosis carrier testing in early pregnancy by general practitioners. Br Med J 1993;306:1580–1583.
Doherty RA, Palomaki GE, Kloza EM, et al: Prenatal screening for cystic fibrosis. Lancet 1994;343:172.
Brambati B, Tului L, Fattore S, Ferec C: First-trimester fetal screening of cystic fibrosis in low risk population. Lancet 1993;342:624.
Super M, Schwarz MJ, Malone G: Screening for cystic fibrosis earners. Lancet 1992;340:490–491.
Super M, Schwarz MJ, Malone G, Roberts T, Haworth A, Dermody G: Active cascade testing for carriers of cystic fibrosis gene. Br Med J 1994;308:1462–1468.
Holloway SH, Brock DJH: Cascade testing for identification of carriers of cystic fibrosis. J Med Screening 1994;1:159–164.
Marteau TM: Psychological costs of screening. Br Med J 1989;299:527.
McQueen DV: Social aspects of genetic screening for Tay-Sachs disease; the pilot community screening programme in Baltimore and Washington. Soc Biol 1975;22:125–133.
Marteau TM, van Duijn M, Ellis I: Effects of screening on perceptions of health: A pilot study. J Med Genet 1992;29:24–26.
Statement of the American Society of Human Genetics on cystic fibrosis carrier screening. Am J Hum Genet 1992;51:1443–1444.
Williamson R, Allison MED, Bentley TJ, et al: Community attitudes to cystic fibrosis carrier testing in England: A pilot study. Prenat Diagn 1989;9:727–734.
Williamson R: Universal community carrier screening for cystic fibrosis? Nature Genet 1993;3:195–201.
Ten Kate LP, Tijmstra TJ: Carrier screening for cystic fibrosis. Lancet 1989;ii:973–974.
Decruyenaere M, Evers-Kiebooms G, Denayer L, Van den Berghe H: Cystic fibrosis: Community knowledge and attitudes towards carrier screening and prenatal diagnosis. Clin Genet 1992;41:189–196.
Turner G, Wilcken B, Griffiths H: Cystic fibrosis screening and community genetics. J Med Genet 1991;28:575–576.
Watson EK, Marchant J, Bush A, Williamson B: Attitudes towards prenatal diagnosis and carrier screening for cystic fibrosis among the parents in a paediatric cystic fibrosis clinic. J Med Genet 1992;29:490–491.
Watson EK, Mayall ES, Lamb J, Chappell J, Williamson R: Psychological and social consequences of community carrier screening programme for cystic fibrosis. Lancet 1992;340:217–220.
Mennie ME, Compton ME, Gilfillan A, Brock DJH: Prenatal screening for cystic fibrosis: Psychological effects on carriers and their partners. J Med Genet 1993;30:543–548.
Mennie M, Gilfillan A, Compton ME, Liston W, Brock DJH: Prenatal cystic fibrosis carrier screening: Factors in a woman’s decision to decline testing. Prenat Diagn 1993;13:807–814.
Mennie ME, Compton ME, Gilfillan A, Axton RA, Brock DJH: Prenatal screening for cystic fibrosis: Attitudes and responses of participants. Clin Genet 1993;44:102–106.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Brock, D.J.H. Heterozygote Screening for Cystic Fibrosis. Eur J Hum Genet 3, 2–13 (1995). https://doi.org/10.1159/000472268
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1159/000472268
Key Words
This article is cited by
-
Präkonzeptionsscreening
Gynäkologische Endokrinologie (2022)