Abstract
Two recent meta-analyses of randomised salt reduction trials have concluded that there is little purpose in reducing salt intake in the general population. However, the authors, as with other previous meta-analyses, included trials of very short duration (eg 1 week or less) and trials of acute salt loading followed by abrupt reductions to very low salt intake (eg from 20 to less than 1 g of salt/day). These acute salt loading and salt depletion experiments are known to increase sympathetic tone, and with salt depletion cause a rise in renin release and, thereby, plasma angiotensin II. These trials are not appropriate, therefore, for helping to inform public health policy, which is for a more modest reduction in salt intake, ie, from a usual intake of ≈10 to ≈5 g of salt per day over a more prolonged period of time. We carried out a meta-analysis to assess the effect of a modest salt reduction on blood pressure. Our data sources were MEDLINE, EMBASE, Cochrane library, CINAHL, and the reference lists of original and review articles. We included randomised trials with a modest reduction in salt intake and a duration of 4 or more weeks. Meta-analysis, meta-regression, and funnel plots were performed. A total of 17 trials in hypertensives (n=734) and 11 trials in normotensives (n=2220) were included in our study. The median reduction in 24-h urinary sodium excretion was 78 mmol (equivalent to 4.6 g of salt/day) in hypertensives and 74 mmol in normotensives. The pooled estimates of blood pressure fall were 4.96/2.73±0.40/0.24 mmHg in hypertensives (P<0.001 for both systolic and diastolic) and 2.03/0.97±0.27/0.21 mmHg in normotensives (P<0.001 for both systolic and diastolic). Weighted linear regression analyses showed a dose response between the change in urinary sodium and blood pressure. A reduction of 100 mmol/day (6 g of salt) in salt intake predicted a fall in blood pressure of 7.11/3.88 mmHg (P<0.001 for both systolic and diastolic) in hypertensives and 3.57/1.66 mmHg in normotensive individuals (systolic: P<0.001; diastolic: P<0.05). Our results demonstrate that a modest reduction in salt intake for a duration of 4 or more weeks does have a significant and, from a population viewpoint, important effect on blood pressure in both hypertensive and normotensive individuals. This meta-analysis strongly supports other evidence for a modest and long-term reduction in population salt intake, and would be predicted to reduce stroke deaths immediately by ≈14% and coronary deaths by ≈9% in hypertensives, and reduce stroke and coronary deaths by ≈6 and ≈4%, in normotensives, respectively.
Similar content being viewed by others
Introduction
Public health recommendations in most developed countries are to reduce salt intake by about half, ie, from ≈10 to ≈5 g/day. This is because salt intake is thought to play an important role in regulating population blood pressure in epidemiological, migration, intervention, genetic, and animal studies.1,2,3,4,5 At the same time, many trials on the effect of salt reduction on blood pressure have shown consistent reductions in blood pressure in those with high blood pressure, but there is controversy about the magnitude of the fall in blood pressure in normotensive individuals. Several meta-analyses of these salt reduction trials have been performed.6–10 In two meta-analyses8,10 including the most recent one,10 it was claimed that the results showed that salt reduction had no or very little effect on blood pressure in normotensive individuals. The authors concluded that a reduction in population salt intake is not warranted. Furthermore, these papers formed the major basis of a journalistic article in Science11 casting doubt on the link between salt intake and blood pressure, and have also been used to oppose public health recommendations for any reduction in salt intake.12
However, detailed examination of these two latter meta-analyses8,10 shows that from this perspective they are flawed. Both meta-analyses included trials of very short duration of salt restriction, many for only 5 days. On average, the median duration of salt reduction in the normotensives was only 8 days in one meta-analysis10 and 14 days in the other.8 Furthermore, around half of the trials in normotensives compared the effects of acute salt loading to abrupt and severe salt restriction, for example from 20 to less than 1 g of salt/day.10 These acute and large changes in salt intake cause an increase in sympathetic tone, which is particularly evident in normotensive individuals. At the same time, the acute and severe reductions in salt intake cause large compensatory increases in plasma renin activity and angiotensin II.13 It is also already known that most blood-pressure-lowering drugs do not exert their maximal effect within 5 days, and this is particularly true with diuretics, which are likely to work on a similar mechanism to a reduction in salt intake. For these reasons, it is completely inappropriate to include the acute salt restriction trials in a meta-analysis, where the implications of the findings are to try to apply them to public health recommendations for a longer-term modest reduction in salt intake. We therefore carried out a meta-analysis of salt reduction trials that excluded these inappropriate studies and only included studies of modest reductions in salt intake of the same order as the public health recommendations and only included trials that had a duration of salt reduction of 4 or more weeks, albeit recognising that even these studies of 4 weeks may not be long enough to show the full effects of a long-term reduction in salt intake on blood pressure. Furthermore, we included the recently published very well controlled salt reduction study, that is the DASH-Sodium study (Dietary Approaches to Stop Hypertension).14
Methods
Literature search
We developed a search strategy (Table 1) to search for randomised salt reduction trials from electronic databases: MEDLINE (1966 to September 2001), EMBASE (1980 to September 2001), and CINAHL (1982 to June 2001). We also searched the Cochrane library (The Cochrane Controlled Trials Register and the Cochrane Database of Systematic Reviews) with terms of ‘dietary sodium’, ‘dietary salt’, ‘sodium restriction’, and ‘salt restriction’. Furthermore, we reviewed the reference lists of original and review articles to search for more trials. There were no language restrictions.
Inclusion criteria
For inclusion, trials needed to satisfy the following criteria:
-
1)
Random allocation either to a reduced salt intake or usual salt intake (ie control)
-
2)
No concomitant interventions (ie nonpharmaco-logical interventions, antihypertensive, or other medications) in either group
-
3)
Net reduction in 24-h urinary sodium must be ⩾40 mmol (2.5 g of salt/day). Net reduction in 24-h urinary sodium was calculated as UNa (Post) − UNa(Pre) for crossover trials, where UNa(Post) denotes urinary sodium on reduced salt intake and UNa(Pre) denotes urinary sodium on usual salt intake. In a parallel trial, the net change in urinary sodium was calculated as {[UNa(Post) − UNa(Pre)]treatment group} − {[UNa(Post)−UNa(Pre)]control group}
-
4)
Duration of salt reduction must have been for 4 or more weeks. By excluding trials with very short duration, we excluded all the trials with severe reductions in salt intake
-
5)
Study participants were not children or pregnant
Study quality
Criteria for assessment of trial quality were as follows:
-
1)
Concealment of allocation sequences.15 The allocation sequences were defined as adequately concealed if participants and investigators cannot foresee assignment, for example, a prior numbered or coded drug container of identical appearance prepared by an independent pharmacy; central randomisation, and as inadequately concealed if participants and investigators can foresee assignment, for example, open list of random numbers
-
2)
Blinding. We distinguished trials by the methods of blinding, that is, double-blind, blood pressure observer blind, or open study
-
3)
Completeness of follow-up. We defined trials as using intention-to-treat analysis if all subjects were analysed in the groups to which they were randomly allocated, and as not using intention-to-treat analysis if only subjects who completed the trial were included in the ana-lysis. We also recorded the number of subjects who were lost to follow-up after randomisation
Data extraction and outcome measures
Data were extracted independently by two persons (F He and L Ruddock) using a standard form and differences were resolved by discussion with a third reviewer (GA MacGregor). Relevant data recorded were characteristics of the study, design details, study duration, and pre- and post-intervention results. The main outcome measures extracted were the net changes in systolic and diastolic blood pressure and 24-h urinary sodium excretion. These were calculated as the differences between the reduced salt and usual salt groups for mean change from baseline for parallel trials. For crossover trials, the net changes were calculated as the mean differences between the end of reduced salt and usual salt period. Other variables recorded were plasma renin activity, aldosterone, noradrenaline, and lipids. For the purpose of pooled analyses, statistics that could be used to estimate the variances of the outcome measures were also recorded.
Statistical analyses
For each trial, we calculated the variance of the treatment effect for systolic and diastolic blood pressure. This was derived from standard deviations or standard errors of paired differences between baseline and the end of follow-up for each group in a parallel trial16 or between the two treatment periods in a crossover trial, or if these statistics were not given, from confidence intervals, exact t or P values. If the exact variance of paired difference was not derivable, it was imputed either by inverting a boundary P value (eg P<0.05 became P=0.05) or assuming a correlation coefficient of 0.5 between the initial and final blood pressure.17 Among the 28 trials included in our meta-analysis,14,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41 10 had to have variance imputed.18,19,23,24,27,31,32,38,39 Mean effect sizes were calculated by weighting each trial by the inverse of the variance.16 Weighted linear regression was used to examine the dose response relationship between the change in urinary sodium and the change in blood pressure. We used funnel plot asymmetry to detect publication and other biases in the meta-analysis.42,43
Results
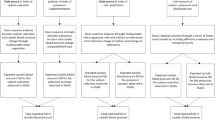
Figure 1 shows the number of studies assessed and excluded through the stages of the meta-analysis. A total of 28 trials with 2954 subjects14,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41 were found that fitted the inclusion criteria: 17 trials were in hypertensive14,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33 and 11 in normotensives14,23,33,34,35,36,37,38,39,4041 (in three trials14,23,33 where both hypertensives and normotensives were studied, the data on hypertensives and normotensives were recorded separately). In two trials14,28 where three levels of salt intakes were studied, we included the high and intermediate levels (ie urinary sodium reduced from 190 to 108 mmol/day) in one trial,28 and in the other (DASH-Sodium study)14 we included the high and low levels (ie urinary sodium reduced from 145 to 65 mmol/day in hypertensives and from 139 to 64 mmol/day in normotensives on the normal American diet). Table 2 summarises the characteristics of the trials included in the meta-analysis.
Effect on blood pressure
Trials in hypertensive individuals: A total of 734 hypertensive individuals were studied in 17 trials.14,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33 The median age was 50 years (ranging from 24 to 73 years). Of the 17 trials, 11 employed crossover design14,18,20,21,24,27,28,31,32,33 and six used paralleled comparisons.19,22,23,25,26,30 Nine out of the 17 trials were double-blind,20,21,27,28,29,30,31,32,33 seven were blood pressure observer-blind,14,19,22,23,24,25,26 and one did not report any blinding procedure.18 The study duration varied from 4 weeks to 1 year (median: 6 weeks). The median blood pressure on usual salt intake was 150/93 mmHg. The median net change in 24-h urinary sodium was −78 mmol (4.6 g of salt/day) and ranged from −53 to −117 mmol. The median 24-h urinary sodium on the usual salt intake was 161 mmol (9.5 g of salt/day) and on the reduced salt intake it was 87 mmol (5.1 g of salt/day). This reduction in salt intake is the same as that of the current public health recommendations.
Figure 2 shows the net change in systolic blood pressure in individual trials included in the meta-analysis. The pooled estimates of changes in blood pressure were −4.96±0.40 mmHg (mean±s.e.m) (P<0.001, 95% CI: −5.75 to −4.17 mmHg) for systolic and −2.73±0.24 mmHg (P<0.001, 95% CI: −3.21 to −2.25 mmHg) for diastolic.
Average net change in systolic blood pressure and corresponding 95% CI in individual trials included in the meta-analysis. The overall effect represents the pooled estimate of mean net change in systolic blood pressure for hypertensives and normotensives, respectively. The size of the symbol is in proportion to the weight (ie inverse of the variance of the net change in systolic blood pressure) of the trial. The numbers in parenthesis are the reference numbers.
To examine whether there was a dose response relationship between the changes in 24-h urinary sodium and the changes in blood pressure, we performed weighted linear regression assuming a zero intercept. The assumption for using this model was that absence of a change in urinary sodium would be associated with no change in blood pressure, that is, all other factors being equal between two randomised treatments. The results showed a significant dose response to salt reduction. A reduction of 100 mmol/day in salt intake predicted a fall in blood pressure of 7.11/3.88 mmHg (P<0.001 for both systolic and diastolic) (Figure 3).
Relationship between the net change in urinary sodium excretion and systolic blood pressure. The open circles represent normotensives and the solid circles represent hypertensives. The slope is weighted by the inverse of the variance of the net change in systolic blood pressure. The size of the circle is in proportion to the weight of the trial.
Trials in normotensive individuals: A total of 2220 normotensive individuals were studied in 11 trials.14,23,33,34,35,36,37,38,39,40,41 The median age was 47 years (ranging from 22 to 67 years). Of the 11 trials, six employed cross-over design.14,33,34,35,38,40 and five used paralleled comparisons.23,36,37,39,41 Seven of the 11 trials were double-blind33,34,35,36,38,39,40 and four were blood pressure observer-blind.14,23,37,41 The study duration varied from 4 weeks to 3 years (median: 4 weeks). The median blood pressure on usual salt intake was 127/78 mmHg. The median net change in 24-h urinary sodium was –74 mmol (4.4 g of salt/day) and ranged from −40 to −118 mmol. The median 24-h urinary sodium on the usual salt intake was 154 mmol (9.1 g of salt/day), and on the reduced salt intake it was 82 mmol (4.8 g of salt/day). This reduction in salt intake is the same as that of the current public health recommendations. It is important to note that in the only two longer-term trials (18 months and 3 years)37,41 the reduction in salt intake was about half that found in the trials of 4–6 weeks.
The pooled estimates of changes in blood pressure were –2.03±0.27 mmHg (P<0.001, 95% CI: −2.56 to −1.50 mmHg) for systolic and −0.97±0.21 mmHg(P<0.001, 95% CI: −1.39 to −0.55 mmHg) for dia-stolic. The dose response analysis with fixing the intercept showed that a reduction of 100 mmol/day in salt intake predicted a fall in blood pressure of 3.57/1.66 mmHg (P<0.001 for systolic and P<0.05 for diastolic) (Figure 3).
Effect on hormones and lipids (Table 3)
Plasma renin activity: Of the 28 trials, nine reported the data of plasma renin activity20,21,24,28,32,33,38,40 (six in hypertensives20,21,24,28,32,33 and three in normotensives33,38,40). The median plasma renin activity was 1.17 ng/ml/h on the usual salt and 1.55 ng/ml/h on the reduced salt intake. The pooled estimate of the change in plasma renin activity was 0.36 ng/ml/h (P<0.001, 95% CI: 0.23–0.49 ng/ml/h).
Aldosterone: Of the 28 trials, eight had plasma aldosterone measured20,24,28,31,32,33,40 (six in hypertensives20,24,28,31,32,33 and two in normotensives33,40). One trial was excluded from the aldosterone analysis as the plasma aldosterone was extremely high after the unit conversion31 (235277.8 pmol/l on the usual salt and 269166.7 pmol/l on the low salt). The median plasma aldosterone was 298 pmol/l on the usual salt and 411 pmol/l on the reduced salt intake. The pooled estimate of the change in aldoste-rone was 98.5 pmol/l (P< 0.001, 95% CI: 74.0–122.9 pmol/l).
Noradrenaline: Plasma noradrenaline was meas-ured in five trials.24,27,28,31,38 Only one trial showed a significant increase (increased by 79 pg/ml, P<0.05)38 and the others did not show significant changes.
Lipids: Three trials reported the data of total cholesterol27,38,40 and two reported the data of triglyceride, low-density lipoprotein and high-density lipoprotein cholesterol.38,40 None showed any significant change in total cholesterol, triglyceride, low-density lipoprotein or high-density lipoprotein cholesterol.
Discussion
Our meta-analysis is the first to only include randomised trials of more modest and longer-term reductions in salt intake. It demonstrates a significant effect on systolic and diastolic blood pressure in both hypertensive and normotensive individuals. The blood pressure fell, on average, by 5/3 mmHg in hypertensives and 2/1 mmHg in normotensives. These falls in blood pressure would have an immediate and significant impact on population blood pressure and would, therefore, be predicted to reduce stroke deaths immediately by ≈14% and coronary deaths by ≈9% in hypertensives, and to reduce stroke and coronary deaths by ≈6% and ≈4%, respectively,44 in normotensives.
Study quality
Among the 28 trials included in our meta-analysis, 20 were adequately concealed (16 were double-blind20,21,27,28,29,30,31,32,33,34,35,36,38,39,40 and four were centrally randomised at a site remote from the study14,37,41). In eight trials, the information on concealment of allocation was not available.18,19,22,23,24,25,26 The number of trials using intention-to-treat analysis was small (seven out of 28 trials).14,26,29,30,36,37 However, the percentage of subjects who were lost to follow-up after randomisation was small (6% on average).
Although double-blind trials were of good quality, we included double-blind, blood pressure observer-blind, and open studies for the following reasons: (1) Some trials, for example, the DASH-Sodium,14 although non-double-blinded, were well conducted with good compliance to different diets. (2) It is very difficult to make any dietary intervention study double-blind. In relation to salt, this can only be done by the use of salt tablets (Slow Sodium and placebo). Among the 28 trials included in our meta-analysis, 16 were double-blind,20,21,27,28,29,30,31,32,33,34,35,36,38,39,40 11 were blood pressure observer-blind,14,19,22,23,24,25,26,37,41 and only one small trial in hypertensives was non-blind.18 Reanalysing the data by excluding the non-blind study18 showed that the results were unchanged. The mean net change in blood pressure was −4.94/−2.76 mmHg (P<0.001 for both systolic and diastolic) when the non-blind study18 was excluded.
Dose response to salt reduction
Weighted linear regression with the regression line forced through the origin shows a significant dose response between salt reduction and blood pressure, suggesting the lower the salt intake achieved, the greater the effect. For instance, a 100 mmol reduction in salt intake predicts a fall in blood pressure of 7/4 mmHg in hypertensives and 4/2 mmHg in normotensives. The reasons to force the regression line through the origin were the following: (1) Most trials did not report confounding factors. We assumed that in randomised well-controlled studies the confounding factors did not change throughout the trial in crossover studies and were comparable between the two treatment groups in parallel studies. (2) When we performed weighted linear regression without fixing the origin, the intercepts were not significantly different from zero. In fact, the slopes (mmHg/mmol) with the regression line forced through the origin (0.071/0.039 (systolic/diastolic) in hypertensives and 0.036/0.017 in normotensives) were very similar to those without fixing the origin (0.116/0.030 in hypertensives and 0.033/0.011 in normotensives).
More importantly, the dose response relationship observed in our meta-analysis is in good agreement with two well-controlled studies of three levels of salt intake.14,28
Study duration
In spite of including studies of 1 month or more, the median duration of salt reduction in our meta-analysis was 6 weeks in the hypertensives and 4 weeks in the normotensives. Whether salt reduction has exerted its maximum effect by 4 weeks is not known, but much evidence would suggest that this is unlikely.3 The finding that the two longer-term trials37,41 in normotensives that were included had no greater effect on blood pressure is likely to be because salt intake was only reduced on average by 2.5 g/day, whereas in the other trials it was reduced on average by 4.4 g/day.
Publication bias
We plotted the funnel plots by plotting the treatment effect against the reciprocal of the standard error of the treatment effect (Figure 4a and b). For diastolic blood pressure the funnel plots were symmetrical about the mean effect size line (asymmetry test:42 P= 0.53). For systolic blood pressure the graphic plot was suggestive of bias (asymmetry test: P=0.07). This asymmetry of funnel plot might be because smaller studies showing no effects were under-reported in the literature. However, in our meta-analysis it is more likely to be because of the smaller effects of two larger and longer-term trials.37,41 The smaller effects in these two trials are because of the much smaller reduction of salt intake achieved in the longer-term trials. By taking any of these trials off the analysis, the asymmetry test was not significant (ie P > 0.1).
Any adverse effects of modest salt reduction?
The previous meta-analyses by Midgley et al8 and Graudal et al10 have implied that salt reduction has adverse effects, which might mitigate any benefit that might occur from reduction in blood pressure. However, it has been persistently pointed out that there is no evidence for any adverse effects from salt reduction, and this is particularly true for the more modest reductions in salt intake that are the current public health recommendations.45 Our meta-analysis shows that with modest reductions in salt intake, there are only very small increases in plasma renin activity, no detectable change in sympathetic tone, and no changes in total cholesterol, triglyceride, low-density or high-density lipoprotein cholesterol.
Mortality studies
One of the difficulties of drawing conclusions about the importance of dietary or other lifestyle changes in cardiovascular disease is the gap in the evidence that relates to mortality. One has to accept that outcome studies of dietary or lifestyle changes in the population are extremely difficult. Indeed, there is unlikely to ever be outcome evidence on mortality for the important dietary variants, that is, saturated fat, fruit and vegetables, or other lifestyle changes (eg losing weight or taking exercise). For instance, a study on salt would need to randomise subjects at the time of conception to a lower and higher salt intake, and then follow up the two groups of offspring on a high and low salt intake for the rest of their lives. Such studies are impractical and would be unethical in the light of current knowledge.
Alderman et al have attempted to look at the effect of salt intake on cardiovascular disease in two cohort studies, one is a follow-up study of a work-site screening project in New York,46 and the other involved the NHANES 1—a dietary survey of US adults from the mid 1970s.47 They suggested that a low salt diet might increase the risk of cardio-vascular disease. However, these two analyses are deeply flawed and have been severely criticised elsewhere.48,49,50,51,52 A further analysis of the same NHANES 1 data showed that a high salt intake was significantly associated with an increased risk of cardiovascular disease and all cause mortality in overweight persons.53
A recent study from Finland using a random sample of the Finnish adult population showed that salt intake was directly related to increased cardiovascular mortality and total mortality.54 For a 6 g increase in salt intake, there were large increases in both coronary heart disease, cardiovascular disease and total mortality (Figure 5).
Hazard ratios for coronary heart disease (CHD), cardiovascular disease (CVD), and all-cause mortality associated with a 6 g/day increase in salt intake as judged by 24-h urinary sodium excretion (Adapted from Tuomilehto et al54).
One cost-effectiveness analysis in a Norwegian population showed that a reduction in population salt intake with a 2 mmHg fall in systolic blood pressure increases life expectancy by 1.8 months in men and by 1.4 months in women, and a reduction in population salt intake saves costs to individuals and society by £85 million.55 In the United Kingdom the population is larger and a modest reduction in population salt intake would, according to this paper, save over £1 billion.
Other evidence in support of a reduction in population salt intake
In assessing both the evidence that salt reduction may be beneficial and its likely long-term impact on public health, it is important to look at other types of evidence. Epidemiological studies have demonstrated that salt intake is an important factor in determining population blood pressure level and the rise in blood pressure with age.1 Studies in migrant populations have also shown an increase in blood pressure from a traditional rural to an urban environment, where salt intake also increased along with other changes.2 An intervention study in two similar villages in Portugal, where salt intake was successfully reduced in one by the provision of processed foods with less salt and appropriate dietary advice, demonstrated a large difference in blood pressure between the two villages by the first year and a more pronounced difference in the second year.3 Two other intervention studies, one in Belgium56 and one in North Karelia,57 did not achieve any reduction in salt intake so, unsurprisingly, there was no change in blood pressure. Evidence in animals, particularly in chimpanzees—our closest relative, also supports the role of salt in controlling blood pressure.5 Recently described rare mutations in humans that may either cause high or low blood pressure all involve a defect in the kidney's ability to excrete salt, and are exacerbated by a high and low salt intake, respectively.4 There is also evidence early in life that humans are particularly sensitive to salt intake, and a small reduction in salt intake in the first 6 months of life appeared to have a long-lasting effect on blood pressure subsequently.58 This evidence alone suggests that a modest reduction in salt intake throughout the population would have a large impact on population blood pressure. Furthermore, increasing evidence now suggests that a modest reduction in salt intake has other beneficial effects on human health, for example, a reduced risk of stomach cancer, a direct effect on stroke, left ventricular hypertrophy, progression of renal disease and proteinuria independent of and additional to salt's effect on blood pressure, a positive calcium balance with a reduced risk of renal stones, and bone demineralisation.59
Conclusions
Our meta-analysis demonstrates that a modest re-duction in salt intake does have a significant effect on blood pressure in both hypertensive and normotensive individuals. Our findings in conjunction with other previous evidence relating salt to blood pressure, particularly the recent DASH-Sodium study, make a strong case for a reduction in population salt intake, which will lower population blood pressure and therefore reduce cardiovascular mortality, and may have other beneficial effects on health. Both our study and the DASH-Sodium study suggest a dose response to salt reduction. Current recommendations to reduce salt intake to 5–6 g/day will be effective, but are not ideal.
Contributors
Both authors were involved in the design of the review. Feng J He conducted the search, data extraction and statistical analyses. Graham A MacGregor supervised all aspects of the review conduct. Both authors wrote the original draft of the manuscript, and contributed to the revision and final version of the paper. Both authors acted as guarantors.
References
Elliott P et al. for the Intersalt Cooperative Research Group. Intersalt revisited: further analyses of 24-hour sodium excretion and blood pressure within and across populations BMJ 1996 312: 1249–1253
Poulter N et al. The Kenyan Luo migration study: observations on the initiation of a rise in blood pressure BMJ 1990 300: 967–972
Forte JG et al. Salt and blood pressure: a community trial J Hum Hypertens 1989 3: 179–184
Lifton RP . Molecular genetics of human blood pressure variations Science 1996 272: 676–680
Denton D et al. The effect of increased salt intake on blood pressure of chimpanzees Nat Med 1995 1: 1009–1016
Law MR, Frost CD, Wald NJ . Analysis of data from trials of salt reduction BMJ 1991 302: 819–824
Cutler JA, Follmann D, Elliott P, Suh II . An overview of randomized trials of sodium reduction and blood pressure Hypertension 1991 17: (Suppl I) I-27–I-33
Midgley JP, Matthew AG, Greenwood CM, Logan AG . Effect of reduced dietary sodium on blood pressure: a meta-analysis of randomised controlled trials JAMA 1996 275: 1590–1597
Cutler IA, Follmann D, Alleder PS . Randomized trials of sodium reduction: an overview Am J Clin Nutr 1997 65: (Suppl) 643s–651s
Graudal NA, Galloe AM, Garred P . Effect of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride: a meta- analysis JAMA 1998 279: 1383–1391
Taubes G . The (political) science of salt Science 1998 281: 898–907
Swales J . Population advice on salt restriction: the social issues Am J Hypertens 2000 13: 2–7
He FJ, Markandu ND, MacGregor GA . Importance of the renin system for determining blood pressure fall with acute salt restriction in hypertensive and normotensive Whites Hypertension 2001 38: 321–325
Sacks FM et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet N Engl J Med 2001 344: 3–10
Jüni P, Altman DG, Egger M . Assessing the quality of controlled clinical trials BMJ 2001 323: 42–46
Cappuccio FP, MacGregor GA . Does potassium supplementation lower blood pressure? A meta-analysis of published trials J Hypertens 1991 9: 465–473
Follmann D, Elliott P, Suh I, Cutler J . Variance imputation for overviews of clinical trials with continuous response J Clin Epidemiol 1992 45: 769–773
Parijs J et al. Moderate sodium restriction and diuretics in the treatment of hypertension Am Heart J 1973 85: 22–34
Morgan TO, Myer JB . Hypertension treated by sodium restriction Med J Aust 1981 2: 396–397
MacGregor GA et al. Double-blind randomised cross-over trial of moderate sodium restriction in essential hypertension Lancet 1982 1: 351–355
Watt GCM et al. Dietary sodium restriction for mild hypertension in general practice BMJ 1983 286: 432–436
Silman AJ, Locke C, Mitchell P, Humpherson P . Evaluation of the effectiveness of a low sodium diet in the treatment of mild to moderate hypertension Lancet 1983 1: 1179–1182
Puska P et al. Controlled, randomised trial of the effect of dietary fat on blood pressure Lancet 1983 1: 1–5
Richards AM et al. Blood-pressure response to moderate sodium restriction and to potassium supplementation in mild essential hypertension Lancet 1984 1: 757–761
Erwteman TM et al. Beta-blockade, diuretics, and salt restriction for the management of mild hypertension: a randomised double blind trial BMJ 1984 289: 406–409
Chalmers J et al. Australian National Health and Medi-cal Research Council dietary salt study in mild hyper-tension J Hypertens 1986 4: (Suppl 6) S629–S637
Grobbee DE et al. Sodium restriction and potassium supplementation in young people with mildly elevated blood pressure J Hypertens 1987 5: 115–119
MacGregor GA et al. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension Lancet 1989 2: 1244–1247
Australian National Health and Medical Research Council Dietary Salt Study Management Committee. Effects of replacing sodium intake in subjects on a low sodium diet: a crossover study Clin Exp Hypertens 1989 A11: 1011–1024
Australian National Health and Medical Research Council Dietary Salt Study Management Committee. Fall in blood pressure with modest reduction in dietary salt intake in mild hypertension Lancet 1989 1: 399–402
Benetos A et al. Arterial effects of salt restriction in hypertensive patients. A 9-week, randomized, double-blind, crossover study J Hypertens 1992 10: 355–360
Fotherby MD, Potter JF . Effects of moderate sodium restriction on clinic and twenty-four-hour ambulatory blood pressure in elderly hypertensive subjects J Hypertens 1993 11: 657–663
Cappuccio FP et al. Double-blind randomised trial of modest salt restriction in older people Lancet 1997 350: 850–854
Watt GC et al. Dietary sodium and arterial blood pressure: evidence against genetic susceptibility BMJ 1985 291: 1525–1528
Mascioli S et al. Sodium chloride raises blood pressure in normotensive subjects: the study of sodium and blood pressure Hypertension 1991 17: (Suppl I) I21–I26
Cobiac L, Nestel PJ, Wing LMH, Howe PRC . A low-sodium diet supplemented with fish oil lowers blood pressure in the elderly J Hypertens 1992 10: 87–92
The Trials of Hypertension Prevention Collaborative Research Group. The effects of nonpharmarmacologic interventions on blood pressure of persons with high normal levels: results of the Trials of Hypertension Prevention. phase I JAMA 1992 267: 1213–1220
Ruppert M et al. Neurohormonal and metabolic effects of severe and moderate salt restriction in non-obese normotensive adults J Hypertens 1993 117: 743–749
Nestel PJ et al. Enhanced blood pressure response to dietary salt in elderly women, especially those with small waist:hip ratio J Hypertens 1993 11: 1387–1394
Schorr U, Distler A, Sharma AM . Effect of sodium chloride- and sodium bicarbonate-rich mineral water on blood pressure and metabolic parameters in elderly normotensive individuals: a randomized double-blind crossover trial J Hypertens 1996 14: 131–135
The Trials of Hypertension Prevention Collaborative Research Group. Effect of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, Phase II Arch Intern Med 1997 157: 657–667
Egger M, Davey Smith G, Schneider M, Minder C . Bias in meta-analysis detected by a simple, graphical test BMJ 1997 315: 629–634
Sterne JAC, Egger M, Davey Smith G . Investigating and dealing with publication and other biases. In: Egger M, Davey Smith G, Altman DG (eds) Systematic Reviews in Health Care. Meta-analysis in Context BMJ Books: London 2001 pp 189–208
Stamler R . Implications of the INTERSALT study Hypertension 1991 17: (Suppl I) I16–I20
De Wardener HE, Kaplan NM . On the assertion that a moderate restriction of sodium intake may have adverse effect. Editorial Am J Hypertens 1993 6: 810–814
Alderman MH et al. Low urinary sodium is associated with greater risk of myocardial infarction among treated hypertensive men Hypertension 1995 25: 1144–1152
Alderman MH, Cohen H, Madhaven S . Dietary sodium intake and mortality. The National Health and Nutrition Examination Survey (NHANES 1) Lancet 1998 351: 781–785
MacGregor G . Low urinary sodium and myocardial infarction Hypertension 1996 27: 156 (Letter)
de Wardener H . Salt reduction and cardiovascular risk: the anatomy of a myth J Human Hypertens 1999 13: 1–4
de Wardener H, MacGregor GA . Sodium intake and mortality Lancet 1998 351: 1508 (Letter)
Engelman K . Sodium intake and mortality Lancet 1998 351: 1508 (Letter)
Karppanen H, Mervaala E . Sodium intake and mortality Lancet 1998 351: 1509 (Letter)
He J et al. Dietary sodium intake and subsequent risk of cardiovascular disease in overweight adults JAMA 1999 282: 2027–2034
Tuomilehto J et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study Lancet 2001 357: 848–851
Selmer RM et al. Cost and health consequences of reducing the population intake of salt J Epidemiol Community Health 2000 54: 697–702
Staessen J et al. Salt intake and blood pressure in the general population: a controlled intervention trial in two towns J Hypertens 1988 6: 965–973
Tuomilehto J et al. Community-based prevention of hypertension in North Karelia, Finland Ann Clin Res 1984 16: (Suppl 43) 18–27
Geleijnse JM et al. Long-term effects of neonatal sodium restriction on blood pressure Hypertension 1996 29: 913–917
Antonios TF, MacGregor GA . Salt-more adverse effects Lancet 1996 348: 250–251
Acknowledgements
We thank Lawrence Ruddock for independently extracting data to check our own analysis. We also thank the authors who kindly provided the data necessary for the computation of some of the variables included in the analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
He, F., MacGregor, G. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens 16, 761–770 (2002). https://doi.org/10.1038/sj.jhh.1001459
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001459
Keywords
This article is cited by
-
Environments affect blood pressure in toddlers: The Japan Environment and Children’s Study
Pediatric Research (2024)
-
Daily self-reported behavioural efficacy records on hypertension digital therapeutics as digital metrics associated with the reduction in morning home blood pressure: post-hoc analysis of HERB-DH1 trial
Hypertension Research (2024)
-
Comprehensive mapping of Epithelial Na+ channel α expression in the mouse brain
Brain Structure and Function (2024)
-
Dietary salt intake predicts future development of metabolic syndrome in the general population
Hypertension Research (2023)
-
The effect of obesity and subsequent weight reduction on cardiac structure and function in dogs
BMC Veterinary Research (2022)