Abstract
We investigated the effect of nicotine on three behavioral markers of risk for schizophrenia: sustained attention (using the Continuous Performance Task (CPT)), antisaccade performance, and smooth pursuit. Smooth pursuit was investigated in two conditions, one in which attention was enhanced (monitoring target changes) and one in which attention was not enhanced (no monitoring). Patients with schizophrenia (n = 15) and controls (n = 14) were given a 14-mg nicotine patch in a double-blind, placebo-controlled, crossover design and plasma nicotine concentrations were monitored. Nicotine concentrations were similar in both groups. A Group × Drug interaction (p < .02) on CPT hits indicated that nicotine improved sustained attention in patients but not in controls. Nicotine significantly decreased antisaccade errors (p < .01) in both groups. A Drug × Monitoring condition interaction (p < .01) on pursuit gain indicated that nicotine significantly increased pursuit gain in the no-monitoring condition in patients and controls equally, but did not improve pursuit in the monitoring condition. Thus, improvement in pursuit may have been mediated via an effect on attention rather than by an effect on oculomotor function per se. In patients, the magnitude of improvement in attention on nicotine was correlated with the improvement on eye movement tasks. Thus, nicotine improves performance on both attention and oculomotor markers of risk for schizophrenia, possibly via common mechanisms.
Similar content being viewed by others
Main
Nicotinic mechanisms have been implicated in the pathophysiology of schizophrenia. Schizophrenic patients have a high prevalence of smoking, higher than any other psychiatric population (Hughes et al. 1986). It has been postulated that schizophrenic patients may smoke as an attempt to self-medicate, that is, to correct a physiological deficit in nicotinic cholinergic mechanisms (Leonard et al. 1996). Evidence in support of this interpretation include the findings that: (1) schizophrenic patients have fewer nicotinic receptors in post-mortem brain tissue than normal smokers (Freedman et al. 1995; Breese et al. 2001); (2) nicotine transiently normalizes sensory gating deficits among schizophrenic patients (Adler et al. 1993) and unaffected first-degree relatives (Adler et al. 1992); and (3) sensory gating deficits in schizophrenia have been linked to an allele of chromosome 15, the gene locus for a specific nicotinic receptor (i.e. α7-nicotinic receptor) (Freedman et al. 1997).
Family, twin and adoption studies have demonstrated that genetic factors play a major role in the etiology of schizophrenia (Bertelsen 1985; Gottesman et al. 1987; Kendler 1986). The risk for developing the illness is increased among first-degree relatives of schizophrenic patients (Gottesman et al. 1987; Kety et al. 1994), and they can pass on vulnerability for schizophrenia without having expressed the clinical disorder themselves (Gottesman and Bertelsen 1989). A subpopulation of schizophrenic patients' first-degree relatives have cognitive or motor deficits similar to those observed in affected probands (Adler et al. 1992; Levy et al. 1993; Cornblatt and Keilp 1994; Clementz et al. 1994). Thus, such deficits may be related to genetic vulnerability for schizophrenia (i.e., may be “behavioral markers of risk” for the illness) (Holzman 1992).
The data that Freedman and colleagues (1997) have provided implicating nicotine in the pathophysiology of schizophrenia suggest that nicotine is involved in the pathophysiology of risk for the disorder as well. Specifically, sensory gating deficits which occur at elevated rates in relatives of schizophrenic patients are normalized by nicotine (Adler et al. 1992) and are associated with an allele for a nicotinic receptor (Freedman et al. 1997). We were interested in the possibility that nicotinic mechanisms may be implicated as well in the pathophysiology of other markers of risk for schizophrenia.
Abnormalities in sustained attention (Cornblatt and Keilp 1994), antisaccade (Clementz et al. 1994), and smooth pursuit (Levy et al. 1993) performance are all thought to be markers of risk for schizophrenia. Each are found at elevated rates in schizophrenic patients (Orzack and Kornetsky 1966; Holzman et al. 1973; Fukushima et al. 1990) their first-degree relatives (Levy et al. 1993; Cornblatt and Keilp 1994; Clementz et al. 1994) and other populations at high risk for the disorder (Siever et al. 1984; Roitman et al. 1997; O′Driscoll et al. 1998), but at low rates in the general population. In addition, genetic studies suggest a significant hereditary component to sustained attention (Cornblatt et al. 1988), antisaccade performance (Myles-Worsley et al. 1999) and smooth pursuit (Iacono and Lykken 1979; Bell et al. 1994).
Nicotine has previously been shown to improve sustained attention (Rusted and Warburton 1992; Warburton and Arnall 1994; Levin et al. 1998) and smooth pursuit performance (Domino et al. 1997) in normal controls, while the effect of nicotine on antisaccade performance has not been investigated. On sustained attention tasks, nicotine was found to increase accuracy and decrease reaction time (Warburton and Mancuso 1998) as well as to prevent the decline in performance that occurs over time (Frankenhaeuser et al. 1971). To date, no double-blind studies of the effect of nicotine on oculomotor markers of risk have been conducted and there has been only one controlled study of the effect of nicotine on sustained attention in schizophrenia (Levin et al. 1996).
The current study investigated the effect of nicotine on three putative markers of risk for schizophrenia, sustained attention, antisaccade performance and smooth pursuit eye movements using a double-blind, placebo-controlled, crossover design. Because schizophrenic patients have deficits on these tasks, and because there is evidence that they have abnormal nicotinic function, we hypothesized that nicotine would improve the performance of patients to a greater extent than that of controls. Preliminary results from this study have been published in abstract form (O′Driscoll et al. 1999a; Dé patie et al. 2001a,b).
SUBJECTS AND METHODS
Subjects
Twenty-nine smokers, 15 patients (3 women, 12 men) who met DSM-IV criteria (APA 1994) for schizophrenia and 14 normal controls (3 women, 11 men) participated in the study. The two groups were highly similar both demographically and in terms of nicotine dependence (Fagerström Test for Nicotine Dependence, FTND score) (Fagerströ m 1978) (Table 1).
Patients were recruited from the inpatient and outpatient population of the Douglas Hospital, Verdun, Québec. DSM-IV diagnosis of schizophrenia was confirmed through chart review. Current symptoms were rated using the Positive and Negative Syndrome Scale (PANSS) (Kay et al. 1987). Patients were found to have an average score of 62.87 (±11.64). All patients were receiving neuroleptic treatment with an average dose of 737.22 mg/day (±647.49 mg/day chlorpromazine equivalents) (Bezchlibnyk-Butler and Jeffries 1998). Six patients were receiving atypical neuroleptics (risperidone and/or olanzapine) and nine were receiving typical neuroleptics. Eight of the patients were taking antimuscarinic antiparkinsonian medication. All patients were maintained on their regular medications, including dose and time of administration, for at least one month before the commencement of the study and throughout the investigation. For patients on long-acting neuroleptics, medication was unchanged for at least three months.
The inclusion criteria applied to all subjects were: age between 18 and 65 years, current smokers (i.e., minimum of 10 cigarettes/day for at least six months), normal or corrected-to-normal vision, and an estimated full-scale IQ above 80 (Block Design and Vocabulary subtests of the WAIS-R (Wechsler 1981)). Moreover, all subjects were required to be physically healthy based on a medical history, physical examination, routine laboratory tests including thyroid function and electrocardiogram, and to have no contraindication for the use of a nicotine patch. Pregnant women were excluded from the study. All women underwent a pregnancy blood test to confirm that they were not pregnant. Schizophrenic patients were required to meet DSM-IV criteria for schizophrenia. Control subjects were screened with the non-patient edition of the Structured Clinical Interview for DSM-IV Axis I Disorders (First et al. 1996). They were required to have no personal or family history of schizophrenia or psychotic disorders. In addition, controls were required to have no personal history of major affective disorders or substance abuse or dependence and to be taking no medication.
The study was approved by the Douglas Hospital Research Ethics Board, Verdun, Québec. After a full description of the study, subjects gave informed consent. Subjects were compensated for their participation.
Procedures
Subjects were asked to abstain from smoking from 11:00 P.M. the night before each testing session. They arrived at the laboratory at 8:30 A.M. at which point vital signs (blood pressure, pulse, temperature, breath/min) were assessed and an Angiocath (20 GA) was inserted into an arm vein. At 9:00 A.M., a sample of blood was drawn following which a nicotine patch or an identical looking placebo patch was applied to the upper back. Each participant received nicotine in the form of a Nicoderm nicotine patch (14 mg) (Hoechst Marion Roussel, Frankfurt, Germany) and a placebo in a double-blind, crossover fashion using a counterbalanced design. Ten samples of blood were drawn throughout each testing session and were used to determine nicotine plasma levels. At 4:30 P.M. the catheter was removed, vital signs were reassessed and testing commenced. Testing lasted for 1.5 h. The choice of time for administration of the neurocognitive tests was based on the fact that plasma nicotine concentrations using the Nicoderm 14-mg patch reach a plateau within 5.5 h after a single application, and remain relatively constant for the ensuing 4 h (Gorsline et al. 1993). Nicotine plasma radioimmunoassay analysis revealed that, in controls and patients, peak nicotine levels were achieved 2 h following the patch application, and testing was conducted after the plateau had been established (Figure 1). The patch was removed following testing completion by a nurse who was otherwise not involved in the study. Subjects were instructed not to smoke until the following morning to avoid side effects.
Nicotine Plasma Concentrations. Plasma concentrations (ng/ml) following exposure to a 14-mg Nicoderm nicotine patch in schizophrenic patients and normal controls (data are presented as means ± SE). Baseline indicates the average nicotine plasma level at the time of medical screening (i.e., on a day prior to testing) when participants received no specific instructions about smoking. There were no significant differences in the nicotine plasma concentrations of patients and controls.
The procedure was repeated after a minimum interval of seven days (mean = 19.4 days; SD = 23.4 days) using the crossover patch. On average, placebo and nicotine testing occurred 19.26 (±20.57) days apart for patients and 19.31 (±23.49) days apart for controls (t(33) = 0.01, p> .9). For women, testing sessions were conducted one month apart so that they were tested during the follicular phase of their menstrual cycle when estrogen levels are at their lowest to control for possible hormonal effects. In subjects on long-acting neuroleptics, the placebo and nicotine testing were done at the same interval following the injection on two different injection cycles.
Nicotine Measurements
Blood samples were collected in heparinized tubes and centrifuged at 3000 rpm for 10 min. Plasma was collected, divided into two aliquots, frozen at −23°C and later analyzed for nicotine by radioimmunoassay. The reagents used for nicotine analysis were purchased from Brandeis University (Waltham, MA) and were prepared according to the method described by Van Vunakis et al. (1987). This assay is highly specific and does not cross-react with neuroleptics or caffeine (Van Vunakis et al. 1987). The intra-assay coefficient of variance was ±3.88.
Continuous Performance Task
A 100 MHz IBM clone computer with a monitor refresh rate of 120.79 Hz was used to administer Cornblatt's identical-pairs version of the Continuous Performance Test (CPT) (Cornblatt et al. 1988). Data were collected in a well lit room. Stimuli were presented in the center of the computer screen against a dark background. The task involved the presentation of two types of stimuli, namely, four-digit numbers and nonsense shapes, which were presented in two separate blocks. Subjects performed 25 practice trials which were followed by 150 trials in each block. Each stimulus appeared for 50 ms (inter-stimulus interval: 950 ms.). Subjects were instructed to respond with a finger lift from the mouse button (held in the dominant hand) every time two identical stimuli were presented consecutively. Identical stimuli appeared successively on 20% of the trials. False alarm trials, in which two consecutive stimuli were similar but not identical, were presented on 20% of the trials. The rest of the trials were filler trials in which the two successive stimuli presented were not similar.
Eye Movements
Apparatus
The same computer was used for oculomotor recordings. Oculomotor data were collected in a darkened room while the subjects were seated 57 cm away from the computer monitor. For all of the oculomotor tasks, the stimulus consisted of a 0.5° × 0.5° white square presented against a dark background. Eye movements were recorded from the subject's dominant eye through the use of an infrared pupil tracker (250 Hz) mounted on a headband (Eyelink, SR Research Ltd., Mississauga, Ont.). The spatial resolution of this system is approximately 0.25° of visual angle. Subjects completed a 3-point calibration across 24° of visual angle. The average fixation error on validation was less than 0.5°. The system automatically computes a drift correction prior to the start of each task.
The order of administration of the tasks was as follows: subjects first performed the smooth pursuit task, then the CPT, then the antisaccade task and a visually guided control task, with the order of the last two tasks counterbalanced.
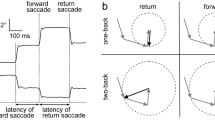
Visually Guided Saccades and Antisaccades
For both the visually guided saccade and antisaccade tasks, subjects fixated a central target which appeared for 800, 1000, or 1200 ms at random. A peripheral target then appeared 10 degrees either to the left or to the right of the central target with direction pseudo-randomized (i.e., the target moved at random to the left or right with the restriction that it could not move in the same direction on more than three consecutive trials). The central target disappeared either 200 ms before the appearance of the peripheral target (gap condition), at the same time that the peripheral target appeared (step condition) or remained on the screen after the appearance of the peripheral target (overlap condition). The three different fixation conditions were randomly intermixed. There was a total of 105 trials, 35 in each of the gap, step, and overlap conditions. The first nine trials were practice trials and were not included in the analysis. In the visually guided saccade task, the subjects were instructed to look toward the peripheral target. In the antisaccade task, subjects were instructed not to look toward the target but to look away from the peripheral target to the mirror position on the opposite side of the computer screen.
Smooth Pursuit
Subjects were instructed to keep their gaze on a target that moved horizontally at 0.4 Hz across 24° of visual angle with a sinusoidal velocity profile. Subjects first performed a practice trial, then two 30-s trials of pursuit in each of two pursuit conditions (i.e.., “monitoring” and “no-monitoring”). In the “monitoring” condition, the center of the target changed from an “X” to an “O” and back at random intervals. Subjects were asked to indicate each change by pressing a response button. Monitoring manipulations such as this one increase attention and improve pursuit performance in patients and controls equally (Sweeney et al. 1994). In the “no-monitoring” condition, there were no changes within the target and subjects were asked to simply keep their gaze on the target as it moved.
Data Analyses
Plasma Nicotine Levels
Plasma nicotine concentrations at plateau were calculated based on samples collected between 3:00 and 4:30 P.M., when plasma levels were at a relatively stable level. An independent sample t-test was used to test whether nicotine plasma levels of patients and controls differed. Plasma nicotine levels were calculated using the assay software AssayZap (Biosoft Ltd., Cambridge, UK).
Preliminary Analyses
Preliminary analyses revealed that there was no difference in performance between patients receiving anticholinergic medications and those who were not receiving such medications on any of the dependent measures. Therefore, the analyses were performed on all patients as one group.
A preliminary set of analyses was performed on the patient group in order to determine whether PANSS score and neuroleptic dose were significantly correlated with the performance measures on each task. Where there was a significant correlation, the analysis were run again in patients alone with the relevant variable as a covariate. These results are reported after the results of the ANOVA.
Order of drug administration (nicotine/placebo vs. placebo/nicotine) was entered as a factor in the original analyses. There were no significant main effects of Order nor interactions of Order with any of the other independent variables. Therefore, this term was dropped from the analyses and the analyses were conducted as presented below.
Continuous Performance Task
Dependent variables analyzed included hits (correct responses), false alarms (errors of commission) and reaction time to hits. In addition, a signal detection index, d′, calculated from the proportion of hits and false alarms, was computed using the statistical computer software package Systat 9 (SPSS Inc., Chicago, IL). This index is a measure of the ability of participants to discriminate a signal from background noise. The higher the d′, the better the processing capacity (Swets 1973). All measures on the CPT were analyzed by repeated measures ANOVAs with Group (patients, controls) as the between-subjects factor and Drug (nicotine, placebo) and Task (number, shape) as within-subject factors. In order to test whether performance declined over time and whether nicotine prevented this decline (as reported by Frankenhaeuser et al. (1971)), the task was separated into two halves and a preliminary set of analyses was performed with Task Half (first half, second half) as a within-subjects factor. Where there was no main effect or interactions of Task Half, this term was dropped from the analysis. For one patient, CPT data were unavailable for one session.
Eye Movements
All eye movements were parsed quantitatively using a semiautomated custom analysis software package (Eyelink, SR Research, Mississauga, Ont.), and were visually inspected by the experimenter. Due to technical difficulties, the oculomotor data for two patients were unavailable.
Visually Guided Saccades and Antisaccades
Saccades were automatically identified using velocity (22°/s) and acceleration (4000°/s2) criteria. Trials were not included in the analyses if the subject did not respond (saccade amplitude <3°), if the subject blinked either 100 ms before the target appearance or during the saccade, if the subject misfixated the central target (fixation >2.5° off the central target) or if the subject's latency to respond was below 70 ms (anticipatory response). Saccade latency, amplitude and peak velocity were the dependent variables. In addition, in the antisaccade task, percent error (proportion of trials in which the first saccade greater than 3° was toward the target) was calculated. We also calculated the proportion of express saccades (proportion of trials in which saccade latency was between 70 and 100 ms) in the visually guided saccade task, since this was reported to be affected by nicotine in an earlier study (Aizawa et al. 1999).
Repeated measures ANOVAs were performed on the performance measures of these tasks with Group (patients, controls) as the between-subjects variable and Drug (placebo, nicotine), Fixation (gap, step, overlap), Direction of saccade (left, right) and Task Half as within-subject variables. Where there were no main effects or interactions of Task Half or saccade Direction, these terms were dropped from the analyses. PANSS score was significantly correlated with peak velocity on the visually guided saccade task. In addition, neuroleptic dose (chlorpromazine equivalents) was significantly correlated with peak velocity on the antisaccade task. Accordingly, these two variables were also analyzed using Analyses of Covariance (ANCOVA) in the patient group only. The antisaccade data for one session were unavailable for one patient.
Smooth Pursuit
Pursuit gain (eye velocity/target velocity) was used as the measure of the smooth component of the pursuit task. For the gain calculation, the portion of the pursuit in a 451-ms window centered on the peak velocity in each half cycle was used (i.e., peak gain). Saccades and blinks were excluded from the eye trace for gain analysis. The first half cycle of each trace was also excluded from the analyses along with the portion of pursuit 200 ms before and after each blink. Gain was calculated separately for the monitoring and no-monitoring pursuit conditions.
Saccades with a peak velocity equal to or greater than 22°/s above the ongoing pursuit eye speed and average acceleration greater than 3500°/s2 were also analyzed. Saccades were categorized as catch-up saccades, anticipatory saccades, or square wave jerks (SWJ) according to the criteria of Friedman and colleagues (1992).
The data were analyzed with mixed ANOVAs with Group as the between-subjects factor and Drug, Pursuit Condition (monitoring, no-monitoring) and Trace Half (first half, second half of each 30-s trace) as within-subject factors.
The α level was set at .01 for each task in order to maintain the family-wise Type I error rate at the nominal α level of .05 on all tasks. Data are presented as the mean ± standard deviation (X ± SD).
Correlations
For variables that showed a significant effect of nicotine, we evaluated whether performance change on these variables was correlated, and also whether performance change on these variables was related to neuroleptic dose (i.e., chlorpromazine equivalents). Since these variables were continuous, correlations were evaluated with Pearson's r. We also evaluated whether the magnitude of performance change was related to the number of cigarettes currently smoked per day. Because number of cigarettes smoked per day was recorded on a 4-point scale (i.e.: 1 = 0 to 10 cigarettes/day; 2 = 11 to 20; 3 = 21 to 30; 4 = 31 or more), Spearman's rho was used for these analyses.
RESULTS
Plasma Nicotine Levels
Nicotine levels did not differ between the two groups at baseline (t(24) = −0.86, p = .4) or at plateau (t(27) = −1.33, p = .2) (Figure 1)
Continuous Performance Task
The analyses revealed a significant main effect of Group on hits (F1,26 = 18.04, p = .001) indicating that patients made fewer hits (15.4 ± 4.5) than controls (22.5 ± 4.68). There was also a Group × Drug interaction on this measure (F1,26 = 6.68, p = .016). Post hoc comparisons showed that nicotine increased hits in patients (t(13) = 3.45, p = .004) but not in controls (t(13) = 0.18, p = .86) (Figure 2). The lack of improvement on nicotine in controls was not due to a ceiling effect in their performance on placebo as controls made on average 22.5 ± 4.5 of a possible 30 hits in this condition (i.e., 75% correct).
Effect of Nicotine on CPT Hits. CPT hits in patients with schizophrenia and normal controls on placebo and nicotine (data are presented as means ± SE). There was a significant Group × Drug interaction (p = .016) on hits. Post hoc tests indicated that nicotine increased hits in patients but not in controls. Neither group approached ceiling (max hits = 30).
There was a significant Group × Task Half interaction on hits (F1,26 = 12.16, p = .002). Post hoc comparisons showed that patients' performance declined from the first to the second half of the task (first half: 8.57 ± 2.2; second half: 6.71 ± 2.36, t(13) = 6.50, p = .001) while controls' performance did not (first half: 11.52 ± 2.13; second half: 11.16 ± 2.75, t(13) = 1.11 p = .29). Drug did not interact with Task Half, indicating that although nicotine improved hits, it did not do this by preventing a decline in performance over time.
The analyses yielded a significant main effect of Group on d′ (F1,25 = 13.54, p = .001) indicating that patients had lower d′ (2.83 ± 1.66) than controls (4.5 ± 1.59). There was a trend for a main effect of nicotine on d′ (F1,25 = 5.25, p = .03) indicating that participants were better at signal detection on nicotine (1.87 ± 0.78) than placebo (1.69 ± 0.88). This effect was similar in the two groups (Group × Drug interaction (F1,25 = 2.19, p = .15). There was a significant main effect of Task Half on d′ (F1,25 = 11.15, p = .003). Signal detection was lower in the second half of the task (1.67 ± 0.73) than in the first half (1.84 ± 0.71). Group did not interact with Task Half, indicating that the magnitude of the decline was similar in the two groups. Drug did not interact with Task Half, indicating that nicotine's effect was not to prevent the decline in d′ over time.
There was no main effect of Group or Drug on false alarms or reaction time, and no interaction of Group or Drug with other independent variables on these two measures.
Eye Movements
Visually Guided Saccades
The analyses revealed no effect of Group on the dependent measures of this task and no interaction of Group with other independent variables. In addition, there was no significant main effect of Drug nor interaction of Drug with any of the other independent variables in this task. Thus, schizophrenic patients had normal visually guided saccades, and nicotine did not influence visually guided saccade performance in either group. There was no main effect of Task Half nor interactions on any of the performance measures of this task indicating that performance did not change over time. Because PANSS score had been found in the preliminary analysis to be significantly correlated with peak velocity in patients, we ran an analysis of covariance in patients on peak velocity with PANSS score as the covariate. Again there were no significant effects of Drug or Task Half and no interactions.
Antisaccades
There was a significant main effect of Group on antisaccade percent error (F1,24 = 30.39, p = .001) indicating that patients made significantly more antisaccade errors (32.0% ± 13.0%) than controls (9.3% ± 8.0%). There was a significant main effect of nicotine (F1,24 = 8.80, p = .007) on this measure. Nicotine significantly improved antisaccade performance by decreasing error rates in patients (−13.81% ± 21.33%) and controls (−16% ± 61.24%) (Figure 3). There was no Group × Drug interaction on this measure, indicating that nicotine decreased antisaccade errors in patients and controls equally.
There was a significant main effect of Group on antisaccade latency (F1,23 = 7.82, p = .01). Patients were significantly slower (312 ms ± 58 ms) to generate antisaccades than controls (257 ms ± 42 ms). There was no main effect of Drug nor interactions of Drug with other variables on antisaccade latency, indicating that nicotine did not affect this measure.
There was no main effect of Group on antisaccade amplitude. There was a significant Drug × Fixation × Direction interaction on antisaccade amplitude (F2,46 = 4.93, p = .01). Post hoc comparisons showed that nicotine significantly increased antisaccade amplitudes to the right in the overlap (nicotine: 16.33° ± 5.47°; placebo: 14.45° ± 6.44°, t(25) = 3.09, p = .005) and step (nicotine: 15.67° ± 2.97°; placebo: 14.24° ± 2.92°, t(24) = 2.40, p = .02) conditions and increased amplitude to the left as well in the step condition (nicotine: 16.26° ± 5.18°; placebo: 15.0° ± 6.07°) (t(25) = 2.50, p = .02). Nicotine did not affect amplitude in the gap condition.
There was no significant main effect of Group or Drug on other characteristics of antisaccades and no interactions.
Because neuroleptic dose had been found in the preliminary analysis to be significantly correlated with peak velocity in patients, we ran an analysis of covariance in patients on peak velocity with neuroleptic dose (i.e., chlorpromazine equivalents) as the covariate. Again there was no significant effect of Drug and no interactions.
Smooth Pursuit
There was a main effect of Group on pursuit gain (F1,25 = 11.18, p = .003) indicating that patients had significantly lower peak gain (0.93 ± 0.05) than controls (0.97 ± 0.01). There was a significant Drug × Monitoring interaction (F1,25 = 7.73, p = .01). Post hoc comparisons indicated that while nicotine did not affect peak gain in the monitoring condition (the enhanced attention condition) (t(26) = 0.51, p = .62), nicotine did increase peak gain in the no-monitoring condition (the low attention condition) in both subject groups (t(26) = 2.46, p = .02) (Figure 4. There was no Group × Drug interaction on gain (F1,25 = 1.09, p = .31) indicating that the effect of nicotine on peak gain was observed in patients and controls equally. The Group × Drug × Monitoring interaction was not significant (F1,25 = 2.53, p = .12).
Effect of Nicotine on Pursuit Gain. Pursuit gain in patients with schizophrenia and normal controls on placebo and nicotine (data are presented as means ± SE). There was a significant Drug × Monitoring interaction (p = .01) on gain. Post hoc analyses revealed that nicotine did not significantly increase gain in the monitoring (MON) condition (p = .62) but did significantly improve gain in the no-monitoring (NO-MON) condition (p = .02). This effect was observed in patients and controls equally.
We observed a significant main effect of Trace Half on gain (F1,25 = 12.46, p = .002). Participants had lower gain in the second half of each presented trial (first half: 0.92 ± 0.03; second half: 0.90 ± 0.05) in both pursuit conditions (i.e., monitoring and no-monitoring). Although nicotine significantly improved pursuit performance overall, there was no significant Drug × Trace Half interaction on gain (F1,25 = 0.19, p = .66) indicating that nicotine's action was not to prevent the decline in pursuit performance over time.
There was no significant main effect of Group on catch-up saccades (F1,25 = 0.58, p = .45) indicating that patients did not differ from controls on this measure. The analyses revealed a main effect of Drug (F1,25 = 9.04, p = .006) indicating that participants made fewer catch-up saccades on nicotine (12.4 ± 4.3) than placebo (14.1 ± 3.4). There was no Group × Drug interaction on this measure (F1,25 = 0.32, p = .58) indicating that the effect of nicotine on catch-up saccades was observed in both patients and controls equally. There was no main effect of monitoring condition nor interactions of monitoring condition with other independent variables on catch-up saccades.
There was no significant main effect of Group on overall number of saccades (F1,25 = 30, p = .59) (i.e., total catch-up saccades, anticipatory saccades, back-up saccades, and square wave jerks) indicating that patients (19.9 ± 5.3) did not make significantly more saccades than controls (19.1 ± 4.0) despite having lower gain. There was a significant Monitoring × Trace Half interaction on number of saccades (F1,25 = 7.19, p = .01). Post hoc comparisons revealed that subjects made significantly more saccades in the second half (29.6 ± 7.9) than the first half (26.9 ± 8.2) of the no-monitoring pursuit condition (t(26) = −3.34, p = .003), just as they had lower gain in the second half. However, in the monitoring condition there was no increase in the number of saccades in the second half of the trial (t(26) = −0.99, p = .33) even though gain declined in the second half of this condition as well. There was no main effect of Drug nor interactions of Drug with other variables on overall number of saccades.
There was no significant main effect of Group on SWJs (F1,25 = 0.41, p = .53) indicating that patients did not differ from controls on this measure. There was a trend for a Drug × Monitoring interaction on SWJs (F1,25 = 3.98, p = .06). Post hoc comparisons revealed that SWJs were increased on nicotine (2.52 ± 2.04) compared with placebo (1.83 ± 1.97) in the monitoring condition (t(26) = 2.70, p = .02), but not in the no-monitoring condition (t(26) = −0.07, p = .94).
Correlations with Task Performance
Pearson correlations revealed that performance change from placebo to nicotine on the measures that showed an effect of nicotine (i.e., change in CPT hits, antisaccade errors, antisaccade amplitude, smooth pursuit gain in the no-monitoring condition and catch-up saccades in both conditions) were not correlated across tasks in controls (Table 2). In patients, nicotine-related performance changes were correlated across tasks. The change in number of catch-up saccades in the monitoring condition of pursuit was significantly correlated with change in CPT hits from placebo to nicotine. In addition, change in both gain and catch-up saccades in the no-monitoring condition were correlated with change in antisaccade errors (Table 3). Thus, change in pursuit performance from placebo to nicotine was related to change in CPT performance and to change in antisaccade performance. Change in CPT performance was not related to antisaccade errors. Antisaccade amplitude changes were not related to changes in other measures.
We evaluated whether the level of habitual nicotine exposure and neuroleptic medication affected the degree of nicotine-related performance change. In patients, the number of cigarettes smoked per day was correlated with performance change from placebo to nicotine in the number of catch-up saccades in the no-monitoring condition (rho = 0.56, p < .05) (the more cigarettes smoked habitually the greater the drop in number of catch-up saccades from placebo to nicotine). For all other measures, there was no correlation between the number of cigarettes habitually smoked per day and the magnitude of nicotine's effect (all p > .2) in patients or controls. Neuroleptic medication (i.e. chlorpromazine equivalents) was not correlated with the magnitude of performance change from placebo to nicotine on any measure (all p > .3).
DISCUSSION
The findings in the current investigation suggest that nicotine administered via a single transdermal patch improves performance on sustained attention and eye movement tasks in medicated schizophrenic patients and normal controls who smoke. Nicotine improved sustained attention (CPT-IP hit rate) in patients, but not in controls, and improved antisaccade and smooth pursuit eye movements in both groups. Thus, the hypothesis to the effect that patients would show greater improvement following nicotine than controls was only partially supported. The findings suggest that nicotinic cholinergic mechanisms may be implicated in cognitive and motor functions that are thought to be markers of risk for schizophrenia.
The effect of nicotine on task performance may have been mediated via a direct effect of nicotine at nicotinic receptor sites. Two subtypes of nicotinic receptors have been identified in the mammalian brain, high-affinity and low-affinity (Paterson and Nordberg 2000). Pharmacological (Luntz-Leybman et al. 1992) and genetic (Stevens et al. 1996; Freedman et al. 1997) studies have suggested a role for the low-affinity nicotinic receptor, the α7-nicotinic cholinergic receptor, in the modulation of the P50 sensory gating response, a risk marker investigated in previous studies. In humans, most studies conducted on nicotine's effect on the P50 have used cigarette smoking as the method of administration (e.g. Adler et al. 1993). Cigarette smoking provides acute high doses of nicotine to the brain. This type of administration affects both low and high affinity receptors (Alkondon et al. 2000). In contrast, a nicotine patch administers a chronic low dose of nicotine (Gorsline et al. 1992). Since low-affinity receptors are rapidly desensitized (Leonard et al. 1996), it is not likely that the effects of nicotine in the current study were due to nicotine's effects at the α7-nicotinic cholinergic receptor sites. Rather, a low chronic nicotine dose likely exerts its effects through high-affinity nicotinic receptors. Thus, the mechanisms of improvement in the current study may implicate different nicotinic receptors than those in previous studies. It is not known at this point to what extent abnormalities in different nicotinic receptor systems may be correlated.
Nicotine's behavioral effects are believed to reflect activity not only at cholinergic receptors but also indirect action at other neurotransmitter sites (Wonnacott et al. 1989). For example, it is possible that nicotine improved performance on the antisaccade and smooth pursuit tasks via an indirect action at GABAergic sites. In high concentrations, nicotine decreases the release of GABA (Zhu and Chiappinelli 1999). Nicotinic receptors are found in the superior colliculus, a structure important for both attention and eye movements. Nicotine injections into the motor layers of the superior colliculus induce an increase in the frequency of short latency express saccades in non-human primates (Aizawa et al. 1999). This finding is consistent with a disinhibition of the structure induced by an antagonist effect of nicotine on GABA. In contrast, in low doses nicotine increases the release of GABA (Zhu and Chiappinelli 1999). Thus, it is possible that at the relatively low dose used in the current study nicotine improved antisaccade and smooth pursuit performance by increasing inhibition in the superior colliculus and thereby decreasing antisaccade errors and decreasing saccades during ongoing pursuit.
Nicotine is also known to enhance dopaminergic (DA) function (Imperato et al. 1986). DA function, which is thought to be abnormal in schizophrenia (Meltzer and Stahl 1976), is known to play an important role in attention (Coull 1998) and eye movements (Tedeschi et al. 1983; Gibson et al. 1987; Straube et al. 1998). Dopamine related effects on eye movements could be mediated via either the mesocortical or the nigrostriatal dopamine pathways, or both. Nicotine receptors are found in high density on DA neurons in the ventral tegmental area (VTA), the origin of DA neurons in the mesocortical pathway, and in the nigrostriatal pathway in the substantia nigra and the caudate and putamen (Clarke et al. 1985), structures critical for eye movements (Hikosaka and Wurtz 1983; Hikosaka et al. 1989; Tian and Lynch 1997). Dysfunction of DA cells in the VTA is associated with hypofrontality and can be reversed by nicotine administration in rats (Tsung et al. 1990). Hypofrontality has been observed repeatedly in schizophrenia (Ingvar and Franzen 1974; Weinberger et al. 1986; Buchsbaum et al. 1992). Further, there is some evidence that schizophrenic patients may have reduced density of frontal D1 receptors (Okubo et al. 1997). DA innervation in the frontal cortex is greatest in the precentral gyrus (Brown et al. 1979), the location of the frontal eye fields (Paus 1996) a structure important for smooth pursuit (MacAvoy et al. 1991, O′Driscoll et al. 1999b) and antisaccades (Guitton et al. 1985; O′Driscoll et al. 1995) as well as for attention (Kodaka et al. 1997). Reduced activity in the frontal eye fields (measured by regional cerebral blood flow) has been linked to abnormal pursuit in schizophrenia (Ross et al. 1995; O′Driscoll et al. 1999b). Thus, it is possible that nicotine's effects on eye movements and attention may be mediated by an indirect action on the mesocortical DA system, particularly in oculomotor and attentional structures in the frontal cortex. That the mechanism of action may have been similar for attention and smooth pursuit is suggested by the correlational findings: in the patients, improvements in smooth pursuit performance from placebo to nicotine were significantly correlated with improvements in CPT performance.
It is possible and even probable that nicotine's effects on different oculomotor functions are mediated by discrete neural mechanisms. For example, nicotine was found to increase antisaccade amplitude, an effect which did not correlate with any other changes in the eye movement tasks. Nicotine's effect on saccade amplitude may have been mediated by the nigrostriatal DA system. Saccade amplitude increases following an oral dose of L-dopa (an indirect DA agonist) in patients with Parkinson's disease (Gibson et al. 1987; Rascol et al. 1989). In contrast, saccade amplitude decreases after DA depletion (Kori et al. 1995) in monkeys; saccade amplitudes are also reduced in patients with degenerative diseases of the basal ganglia including Parkinson's disease (Straube et al. 1998). Thus, saccade amplitude is sensitive to changes in nigrostriatal DA function (Rascol et al. 1989) and may have been the neural substrate of the nicotine-related changes in amplitude observed in the current study.
Two previous controlled studies have been conducted on the effect of nicotine on the CPT, one in schizophrenic patients (Levin et al. 1996) and one in normal controls (Levin et al. 1998). In the former study, each patient received a placebo as well as a 7-, 14-, and 21-mg/day nicotine patch in a randomized fashion, and performance on Conner's CPT was assessed. The investigators found no effect of nicotine on correct responses or error rate (Levin et al. 1996). In the second study, the authors (Levin et al. 1998) reported that in non-smoking normal controls, a 7-mg nicotine patch increased CPT hits on Conner's CPT. In the current study, we used a 14-mg patch and found an increase in hits in schizophrenic patients but not in controls. The differences between our results and those reported by Levin et al. (1996, 1998) may arise from differences in the methodology of the studies. An important difference between the study of Levin and colleagues (1998) and the current study was that, in Levin's study, the controls were non-smokers. Thus, the 7-mg nicotine patch may be sufficient to induce an effect in non-smokers, while the higher 14-mg nicotine patch used in the current study may not be sufficient to induce a change for normal subjects chronically exposed to nicotine. Moreover, the nicotine plasma levels had started to decline at the time of testing (Figure 1) and it is possible that this resulted in a diminished effect of nicotine.
Another methodological difference between the current investigation and the two studies of Levin and colleagues (1996, 1998) is the CPT version used. In their studies, Levin and colleagues used Conner's CPT. In this version of the CPT, subjects are instructed to respond on every trial but to abstain from responding when a predetermined stimulus (the letter X) appears. Conner's CPT is primarily a measure of response inhibition and is, in fact, used as a measure of impulsivity in Attention Deficit Hyperactivity Disorder ADHD (e.g. Epstein et al. 2001). In contrast, in the identical-pairs version of the CPT, subjects are asked to respond only when two consecutive stimuli are identical. In the current study, this occurred on 20% of the trials. Thus, there is no need to inhibit an established tendency to respond. Moreover, there is no predetermined target. Instead, the subject must keep every stimulus in working memory until it can be compared with the following stimulus. Therefore, the identical-pairs version of the CPT emphasizes sustained attention and working memory while the Conner's CPT seems to tap selective attention and skeletomotor inhibition. These executive functions may be differentially affected by nicotine.
Five previous studies have been conducted on the effect of nicotine on oculomotor function, two in schizophrenia (Klein and Andresen 1991; Olincy et al. 1998) and three in normal controls (Sibony et al. 1988; Thaker et al. 1991; Domino et al. 1997). None of these studies have been double-blind. All but one study (Thaker et al. 1991) focused exclusively on smooth pursuit eye movements. Three studies reported that nicotine improved smooth pursuit performance: two studies found a decrease in anticipatory saccades or leading saccades (Klein and Andresen 1991; Olincy et al. 1998), one found a trend for improved pursuit gain (Olincy et al. 1998), and one study reported improved pursuit without reporting specific individual measures (Domino et al. 1997). Two studies (Sibony et al. 1988; Thaker et al. 1991) found no improvement in pursuit but in the study of Thaker and colleagues (1991) pursuit gain was not assessed. Thus, our findings are generally in agreement with previous non-blind studies, in which nicotine-related improvements in pursuit have been noted. Further, the finding in the current study that nicotine tended to increase SWJs is in agreement with the findings of both Sibony and colleagues (1988) and Thaker and colleagues (1991), although in their studies subjects were not required to monitor target changes during pursuit.
The interpretation of the results in the current study is constrained by some aspects of the methodology. First, all subjects were smokers. Thus, the positive effects of nicotine in both groups may have been due to the amelioration of withdrawal-related deficits rather than an improvement of function above baseline levels. In the current study, it was not possible to include a non-smoking group due to ethical concerns regarding exposing non-smokers to nicotine. Because the response to nicotine patch exposure may differ between smokers and non-smokers, we can provide information only regarding the former group. However, the major goal of this study was to investigate the effect of nicotine on markers of risk for schizophrenia in schizophrenic patients. Since the vast majority of schizophrenic patients smoke (Lohr and Flynn 1992), the current study provides information on a large segment of this population. Moreover, while we cannot address why schizophrenic patients begin to smoke, our results provide suggestive evidence as to why they may continue to smoke.
Another limitation of the current study is that patients were medicated. It is possible that the antidopaminergic and antimuscarinic medications that patients received blunted the effect of nicotine on task performance in patients or, less likely, acted synergistically to improve performance. However, in the current study, nicotine had significant effects in controls who were medication free, and the magnitude of the effects in controls was generally similar to that observed in patients. In future studies, the inclusion of a medication-free group of patients would be desirable.
The current findings indicate that nicotine improves neurocognitive performance on tasks that are putative behavioral markers of risk for schizophrenia. However, the underlying neural mechanisms by which nicotine improves behavioral markers of risk for schizophrenia remain to be determined.
References
Adler LE, Hoffer LD, Wiser A, Freedman R . (1993): Normalization of auditory physiology by cigarette smoking in schizophrenic patients. Am J Psychiatry 150: 1856–1861
Adler LE, Hoffer LJ, Griffith J, Waldo MC, Freedman R . (1992): Normalization by nicotine of deficient auditory sensory gating in the relatives of schizophrenics. Biol Psychiatry 32: 607–616
Aizawa H, Kobayashi Y, Yamamoto M, Isa T . (1999): Injection of nicotine into the superior colliculus facilitates occurrence of express saccades in monkeys. J Neurophysiol 82: 1642–1646
Alkondon M, Pereira EF, Almeida LE, Randall WR, Albuquerque EX . (2000): Nicotine at concentrations found in cigarette smokers activates and desensitizes nicotinic acetylcholine receptors in CA1 interneurons of rat hippocampus. Neuropharmacology 39: 2726–2739
APA . (1994): Diagnostic and Statistical Manual of Mental Disorders. Washington, DC, American Psychiatric Association Press
Bell BB, Abel LA, Li W, Christian JC, Yee RD . (1994): Concordance of smooth pursuit and saccadic measures in normal monozygotic twin pairs. Biol Psychiatry 36: 522–526
Bertelsen A . (1985): Controversies and consistencies in psychiatric genetics. Acta Psychiat Scand 319: 61–75
Bezchlibnyk-Butler KK, Jeffries JJ . (1998): Clinical Handbook of Psychotropic Drugs. Seattle, Hogrefe & Huber
Breese CR, Lee MJ, Adams CE, Sullivan B, Logel J, Gillen KM, Marks MJ, Collins AC, Leonard S . (2001): Abnormal regulation of high affinity nicotinic receptors in subjects with schizophrenia. Neuropsychopharmacology 23: 351–364
Brown RM, Crane AM, Goldman PS . (1979): Regional distribution of monoamines in the cerebral cortex and subcortical structures of the rhesus monkey: concentrations and in vivo synthesis rates. Brain Res 168: 133–150
Buchsbaum MS, Haier RJ, Potkin SG, Nuechterlein K, Bracha HS, Katz M, Lohr J, Wu J, Lottenberg S, Jerabek PA . (1992): Frontostriatal disorder of cerebral metabolism in never-medicated schizophrenics. Arch Gen Psychiat 49: 935–942
Clarke PB, Schwartz RD, Paul SM, Pert CB, Pert A . (1985): Nicotinic binding in rat brain: autoradiographic comparison of [3H]acetylcholine, [3H]nicotine, and [125I]-alpha-bungarotoxin. J Neurosci 5: 1307–1315
Clementz BA, McDowell JE, Zisook S . (1994): Saccadic system functioning among schizophrenia patients and their first-degree biological relatives. J Abnorm Psychol 103: 277–287
Cornblatt BA, Risch NJ, Faris G, Friedman D, Erlenmeyer-Kimling L . (1988): The Continuous Performance Test, identical pairs version (CPT- IP): I. New findings about sustained attention in normal families. Psychiatry Res 26: 223–238
Cornblatt BA, Keilp JG . (1994): Impaired attention, genetics, and the pathophysiology of schizophrenia. Schizophr Bull 20: 31–46
Coull JT . (1998): Neural correlates of attention and arousal: insights from electrophysiology, functional neuroimaging and psychopharmacology. Prog Neurobiol 55: 343–361
Dépatie L, O′Driscoll GA, Wolff A-L, Atkinson V, Thavundayil JX, Ng Ying Kin N, Lal S . (2001a): Nicotine improves attention and eye movement performance in schizophrenia. Psychophysiol 38: S36
Dépatie L, O′Driscoll GA, Wolff A-L, Atkinson V, Thavundayil JX, Ng Ying Kin N, Lal S . (2001b): The effect of nicotine on attention and eye movements in schizophrenia. Schizophr Res 49: 213
Domino EF, Ni LS, Zhang H . (1997): Effects of tobacco smoking on human ocular smooth pursuit. Clin Pharmacol Ther 61: 349–359
Epstein JN, Johnson DE, Varia IM, Conners CK . (2001): Neuropsychological assessment of response inhibition in adults with ADHD. J Clin Exp Neuropsychol 23: 362–371
Fagerström KO . (1978): Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav 3: 235–241
First MB, Spitzer RL, Gibbon M, Williams JBW . (1996): Structured Clinical Interview for DSM-IV Axis I Disorders. New York, New York State Psychiatric Institute.
Frankenhaeuser M, Myrsten A-L, Post B, Johansson G . (1971): Behavioural and physiological effects of cigarette smoking in a monotonous situation. Psychopharmacology (Berl). 22: 1–7
Freedman R, Coon H, Myles-Worsley M, Orr-Urtreger A, Olincy A, Davis A, Polymeropoulos M, Holik J, Hopkins J, Hoff M, Rosenthal J, Waldo MC, Reimherr F, Wender P, Yaw J, Young DA, Breese CR, Adams C, Patterson D, Adler LE, Kruglyak L, Leonard S, Byerley W . (1997): Linkage of a neurophysiological deficit in schizophrenia to a chromosome 15 locus. Proc Natl Acad Sci USA 94: 587–592
Freedman R, Hall M, Adler LE, Leonard S . (1995): Evidence in postmortem brain tissue for decreased numbers of hippocampal nicotinic receptors in schizophrenia. Biol Psychiatry 38: 22–33
Friedman L, Jesberger JA, Malki A, Brar R, Meltzer HY . (1992): A methodology for the assessment of smooth pursuit dysfunction. Int J Meth Psychiatry Res 2: 209–216
Fukushima J, Morita N, Fukushima K, Chiba T, Tanaka S, Yamashita I . (1990): Voluntary control of saccadic eye movements in patients with schizophrenic and affective disorders. J Psychiatry Res 24: 9–24
Gibson JM, Pimlott R, Kennard C . (1987): Ocular motor and manual tracking in Parkinson's disease and the effect of treatment. J Neurol Neurosurg Psychiatry 50: 853–860
Gorsline J, Gupta SK, Dye D, Rolf CN . (1993): Steady-state pharmacokinetics and dose relationship of nicotine delivered from Nicoderm (Nicotine Transdermal System). J Clin Pharmacol 33: 161–168
Gorsline J, Okerholm RA, Rolf CN, Moos CD, Hwang SS . (1992): Comparison of plasma nicotine concentrations after application of nicoderm (nicotine transdermal system) to different skin sites. J Clin Pharmacol 32: 576–581
Gottesman II, Bertelsen A . (1989): Confirming unexpressed genotypes for schizophrenia. Risks in the offspring of Fischer's Danish identical and fraternal discordant twins. Arch Gen Psychiatry 46: 867–872
Gottesman II, McGuffin P, Farmer AE . (1987): Clinical genetics as clues to the “real” genetics of schizophrenia (a decade of modest gains while playing for time). Schizophr Bull 13: 23–47
Guitton D, Buchtel H, Douglas RM . (1985): Frontal lobe lesions in man cause difficulties in suppressing reflexive glances and generating goal-directed saccades. Exp Brain Res 58: 455–472
Hikosaka O, Wurtz RH . (1983): Visual and oculomotor functions of monkey substantia nigra pars reticulata. IV. Relation of substantia nigra to superior colliculus. J Neurophysiol 49: 1285–1301
Hikosaka O, Sakamoto M, Usui S . (1989): Functional properties of monkey caudate neurons. I. Activities related to saccadic eye movements. J Neurophysiol 4: 780–798
Hollingshead A, Redlich F . (1958): Social Class and Mental Illness. New York, NY
Holzman PS . (1992): Behavioral markers of schizophrenia useful for genetic studies. J Psychiatr Res 26: 427–445
Holzman PS, Proctor LR, Hughes DW . (1973): Eye-tracking patterns in schizophrenia. Science 181: 179–181
Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA . (1986): Prevalence of smoking among psychiatric outpatients. Am J Psychiatry 143: 993–997
Iacono WG, Lykken DT . (1979): Eye tracking and psychophathology. New procedures applied to a sample of normal monozygotic twins. Arch Gen Psychiatry 36: 1361–1370
Imperato A, Mulas A, Di Chiara G . (1986): Nicotine preferentially stimulates dopamine release in the limbic system of freely moving rats. Euro J Pharmacol 132: 337–338
Ingvar DH, Franzen G . (1974): Abnormalities of cerebral blood flow distribution in patients with chronic schizophrenia. Acta Psychiatr Scand 50: 425–462
Kay SR, Fiszbein A, Opler LA . (1987): The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261–276
Kendler K . (1986): Genetics of schizophrenia. In Frances AJ, Hales RE (eds), Psychiatry Update: American Psychiatric Association Annual Review. Washington, DC, American Psychiatric Association Press, pp 5: 25–41
Kety SS, Wender PH, Jacobsen B, Ingraham LJ, Jansson L, Faber B, Kinney DK . (1994): Mental illness in the biological and adoptive relatives of schizophrenic adoptees. Replication of the Copenhagen Study in the rest of Denmark. Arch Gen Psychiat 51: 442–455
Klein C, Andresen B . (1991): On the influence of smoking upon smooth pursuit eye movements of schizophrenics and normal controls. J Psychophysiol 5: 361–369
Kodaka Y, Mikami A, Kubota K . (1997): Neuronal activity in the frontal eye field of the monkey is modulated while attention is focused on to a stimulus in the peripheral visual field, irrespective of eye movement. Neurosci Res 28: 291–298
Kori A, Miyashita N, Kato M, Hikosaka O, Usui S, Matsumura M . (1995): Eye movements in monkeys with local dopamine depletion in the caudate nucleus. II. Deficits in voluntary saccades. J Neurosci 15: 928–941
Leonard S, Adams C, Breese CR, Adler LE, Bickford P, Byerley W, Coon H, Griffith JM, Miller C, Myles-Worsley M, Nagamoto HT, Rollins Y, Stevens KE, Waldo M, Freedman R . (1996): Nicotinic receptor function in schizophrenia. Schizophr Bull 22: 431–445
Levin ED, Wilson W, Rose JE, McEvoy J . (1996): Nicotine-haloperidol interactions and cognitive performance in schizophrenics. Neuropsychopharmacology 15: 429–436
Levin ED, Conners CK, Silva D, Hinton SC, Meck WH, March J, Rose JE . (1998): Transdermal nicotine effects on attention. Psychopharmacology (Berl) 140: 135–141
Levy DL, Holzman PS, Matthysse S, Mendell NR . (1993): Eye tracking dysfunction and schizophrenia: a critical perspective. Schizophr Bull 19: 461–536
Lohr JB, Flynn K . (1992): Smoking and schizophrenia. Schizophr Res 8: 93–102
Luntz-Leybman V, Bickford PC, Freedman R . (1992): Cholinergic gating of response to auditory stimuli in rat hippocampus. Brain Res 587: 130–136
MacAvoy MJ, Gottlieb JP, Bruce CJ . (1991): Smooth pursuit eye movement representation in the primate frontal eye field. Cereb Cortex 1: 92–102
Meltzer HY, Stahl SM . (1976): The dopamine hypothesis of schizophrenia: a review. Schizophr Bull 2: 19–76
Myles-Worsley M, Coon H, McDowell J, Brenner C, Hoff M, Lind B, Bennett P, Freedman R, Clementz B, Byerley W . (1999): Linkage of a composite inhibitory phenotype to a chromosome 22q locus in eight Utah families. Am J Med Genet 88: 544–550
O′Driscoll GA, Alpert NM, Matthysse SW, Levy DL, Rauch SR, Holzman PS . (1995): The functional neuroanatomy of antisaccade performance investigated with positron emission tomography. Proc Natl Acad Sci USA 92: 925–929
O′Driscoll GA, Lenzenweger MF, Holzman PS . (1998): Antisaccades and smooth pursuit eye tracking and schizotypy. Arch Gen Psychiatry 55: 837–843
O′Driscoll GA, Wolff A-L, Atkinson V, Affifi T, Dépatie L, Lal S . (1999a): Nicotine and behavioral markers of risk for schizophrenia: A double-blind, crossover study. Schizophr Res 36: 312
O′Driscoll GA, Benkelfat C, Florencio PS, Wolff AL, Joober R, Lal S, Evans AC . (1999b): Neural correlates of eye tracking deficits in first-degree relatives of schizophrenic patients: a positron emission tomography study. Arch Gen Psychiatry 56: 1127–1134
Okubo Y, Suhara T, Suzuki K, Kobayashi K, Inoue O, Terasaki O, Someya Y, Sassa T, Sudo Y, Matsushima E, Iyo M, Tateno Y, Toru M . (1997): Decreased prefrontal dopamine D1 receptors in schizophrenia revealed by PET. Nature 385: 634–636
Olincy A, Ross RG, Young DA, Roath M, Freedman R . (1998): Improvement in smooth pursuit eye movements after cigarette smoking in schizophrenic patients. Neuropsychopharmacology 18: 175–185
Orzack MH, Kornetsky C . (1966): Attention dysfunction in chronic schizophrenia. Arch Gen Psychiatry 14: 323–326
Paterson D, Nordberg A . (2000): Neuronal nicotinic receptors in the human brain. Prog Neurobiol 61: 75–111
Paus T . (1996): Location and function of the human frontal eye-field: a selective review. Neuropsychologia 34: 475–483
Rascol O, Clanet M, Montastruc JL, Simonetta M, Soulier-Esteve MJ, Doyon B, Rascol A . (1989): Abnormal ocular movements in Parkinson's disease. Evidence for involvement of dopaminergic systems. Brain 112: 1193–1214
Roitman SE, Cornblatt BA, Bergman A, Obuchowski M, Mitropoulou V, Silverman JM, Siever LJ . (1997): Attentional functioning in schizotypal personality disorder. Am J Psychiatry 154: 655–660
Ross DE, Thaker GK, Holcomb HH, Cascella NG, Medoff DR, Tamminga CA . (1995): Abnormal smooth pursuit eye movements in schizophrenic patients are associated with cerebral glucose metabolism in oculomotor regions. Psychiatry Res 58: 53–67
Rusted JM, Warburton DM . (1992): Facilitation of memory by post-trial administration of nicotine: evidence for an attentional explanation. Psychopharmacology 108: 452–455
Sibony PA, Evinger C, Manning KA . (1988): The effects of tobacco smoking on smooth pursuit eye movements. Ann Neurol 23: 238–241
Siever LJ, Coursey RD, Alterman IS, Buchsbaum MS, Murphy DL . (1984): Impaired smooth pursuit eye movement: vulnerability marker for schizotypal personality disorder in a normal volunteer population. Am J Psychiatry 141: 1560–1566
Stevens KE, Freedman R, Collins AC, Hall M, Leonard S, Marks MJ, Rose GM . (1996): Genetic correlation of inhibitory gating of hippocampal auditory evoked response and alpha-bungarotoxin-binding nicotinic cholinergic receptors in inbred mouse strains. Neuropsychopharmacology 15: 152–162
Straube A, Ditterich J, Oertel W, Kupsch A . (1998): Electrical stimulation of the posteroventral pallidum influences internally guided saccades in Parkinson's disease. J Neurol 245: 101–105
Sweeney JA, Clementz BA, Haas GL, Escobar MD, Drake K, Frances AJ . (1994): Eye tracking dysfunction in schizophrenia: characterization of component eye movement abnormalities, diagnostic specificity, and the role of attention. J Abnorm Psychol 103: 222–230
Swets JA . (1973): The relative operating characteristic in psychology. Science 182: 990–1000
Tedeschi G, Bittencourt PR, Smith AT, Richens A . (1983): Effect of amphetamine on saccadic and smooth pursuit eye movements. Psychopharmacology 79: 190–192
Thaker GK, Ellsberry R, Moran M, Lahti A, Tamminga C . (1991): Tobacco smoking increases square-wave jerks during pursuit eye movements. Biol Psychiatry 29: 82–88
Tian JR, Lynch JC . (1997): Subcortical input to the smooth and saccadic eye movement subregions of the frontal eye field in cebus monkey. J Neurosc 17: 9233–9247
Tsung CS, Grenhoff J, Svensson TH . (1990): Nicotine counteracts midbrain dopamine cell dysfunction induced by prefrontal cortex inactivation. Acta Physiol Scand 138: 427–428
Van Vunakis H, Gjika HB, Langone JJ . (1987): Radioimmunoassay for nicotine and cotinine in environmental carcinogens methods of analysis and exposure measurement. In O′Neill IK Brunnemann KD Dodet B Hoffmann D (eds),Environmental Carcinogens Methods of Analysis and Exposure Measurement. Lyon, W.H.O. International Agency for Research on Cancer, pp 317–330
Warburton DM, Arnall C . (1994): Improvements in performance without nicotine withdrawal. Psychopharmacology (Berl) 115: 539–542
Warburton DM, Mancuso G . (1998): Evaluation of the information processing and mood effects of a transdermal nicotine patch. Psychopharmacology 135: 305–310
Wechsler D . (1981): Wechsler Adult Intelligence Scale - Revised. San Antonio, TX, The Psychological Corporation
Weinberger DR, Berman KF, Zec RF . (1986): Physiologic dysfunction of dorsolateral prefrontal cortex in schizophrenia. I. Regional cerebral blood flow evidence. Arch Gen Psychiatry 43: 114–124
Wonnacott S, Irons J, Rapier C, Thorne B, Lunt GG . (1989): Presynaptic modulation of transmitter release by nicotinic receptors. Prog Brain Res 79: 157–163
Zhu PJ, Chiappinelli VA . (1999): Nicotine modulates evoked GABAergic transmission in the brain. J Neurophysiol 82: 3041–3045
Acknowledgements
This work was supported in part by grants from the Medical Research Council, Canada (Dr. O′Driscoll) and the G.W. Stairs Memorial Fund (Dr. Lal). We thank Xing Dai and Sanjay Machado for their assistance with testing, Dr. Ridha Joober and Diane Fortin, RN, for assistance with subject recruitment, and Dr. Alain Dagher, for helpful comments on earlier versions of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dépatie, L., O′Driscoll, G., Holahan, AL. et al. Nicotine and Behavioral Markers of Risk for Schizophrenia: A Double-Blind, Placebo-Controlled, Cross-Over Study. Neuropsychopharmacol 27, 1056–1070 (2002). https://doi.org/10.1016/S0893-133X(02)00372-X
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(02)00372-X
Keywords
This article is cited by
-
Effects of nicotine on smooth pursuit eye movements in healthy non-smokers
Psychopharmacology (2019)
-
Antipsychotic medication and tobacco use among outpatients with schizophrenia: a cross-sectional study
Annals of General Psychiatry (2014)
-
The nicotinergic receptor as a target for cognitive enhancement in schizophrenia: Barking up the wrong tree?
Psychopharmacology (2014)
-
Smoking improves divided attention in schizophrenia
Psychopharmacology (2014)
-
Reverse translation of the rodent 5C-CPT reveals that the impaired attention of people with schizophrenia is similar to scopolamine-induced deficits in mice
Translational Psychiatry (2013)