Abstract
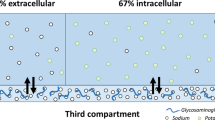
Water balance depends essentially on fluid intake and urine excretion. Mild dehydration and the consequent hypertonicity of the extracellular fluid induce an increase in vasopressin secretion, thus stimulating urine concentrating processes and the feeling of thirst. The osmotic threshold for the release of vasopressin is lower than that for thirst and also shows appreciable individual variation. Sustained high levels of vasopressin and low hydration induce morphological and functional changes in the kidney. However, they could also be risk factors in several renal disorders, such as chronic renal failure, diabetic nephropathy and salt-sensitive hypertension.
Similar content being viewed by others
Introduction
Water balance depends essentially on two parameters: thirst that influences input, and urine excretion that determines output. In humans and most other mammals, the rate at which the kidneys excrete free water is regulated primarily by antidiuretic hormone or vasopressin. Vasopressin is the first hormone to be secreted during dehydration. Changes in the plasma level of other hormones are also observed (increases in atrial natriuretic peptide and catecholamines, fall in aldosterone), but they occur later and in response to severe dehydration.
Vasopressin is synthesized in specific neurons in the supraoptic and paraventricular nuclei and stored in the neurohypophysis. Under physiological conditions, the most important stimulus of vasopressin secretion is the effective osmotic pressure of the plasma. Increase in plasma osmolality is related physiologically to dehydration and a change in water balance, and can be induced experimentally by infusing hypertonic solutions. Vasopressin secretion is also influenced by hemodynamic factors (reduction of blood pressure or blood volume), emetic factors (nausea, drugs such as nicotine or morphine) and factors such as stress, temperature, angiotensin (Berl & Robertson, 2000). Increase in plasma osmolality is also the main stimulus for thirst. However, the desire to drink is triggered by an osmotic level considerably higher than that leading to the secretion of vasopressin (Robertson, 1984). AVP release begins at an average plasma osmolality of about 280 mosm/kg H2O, whereas thirst is not perceived until plasma osmolality reaches about 290 mosm/kg H2O. Thus, during normal living conditions, vasopressin is constantly present in the blood, whereas the perception of thirst is intermittent. The sensitivity and threshold of the osmoregulatory systems show wide inter-individual variability in both humans and rats (Zerbe et al, 1991; Bankir, 2001). These individual differences are constant over prolonged periods and appear to be determined mainly by genetic factors (Zerbe et al, 1991). Since the osmoregulatory mechanisms are not equally sensitive in all healthy individuals, one could expect some subjects to tend to be continuously in a state of slight dehydration, and to have a high level of vasopressin to compensate.
Three vasopressin receptors have been identified and cloned, V2 with cAMP as second messenger, and V1a and V1b with calcium as second messenger. The antidiuretic action of vasopressin depends mainly on V2 receptor-mediated effects in the renal collecting duct. This minireview addresses the functional impact on the kidney of mild dehydration and activation of V2 receptor of vasopressin, in health and disease.
Renal consequences of a high level of vasopressin in a healthy subject
In healthy subjects, high vasopressin levels induce morphological and functional changes in the kidney resulting in greater urine-concentrating activity. Urine concentration depends on the water permeability of the collecting duct and on the presence of a corticomedullary osmotic gradient. Vasopressin contributes to the urine-concentrating mechanism by influencing the permeability to water and urea, and sodium transport in the distal part of the tubule.
At least six types of water channel proteins (aquaporins, AQP) are known to be expressed in the kidney. Among these, AQP2, localized in the luminal membrane of the principal cells of the collecting duct, is the chief target for the short-term regulation of the collecting duct permeability by vasopressin. AQP2, and also AQP3 and AQP4 (basolateral water channels of the collecting duct), are regulated via the long-term effects of chronic dehydration that change the total abundance of these three channels in collecting duct cells (Figure 1a) (Yamamoto et al, 1995; Ishibashi et al, 1997; Murillo-Carretero et al, 1999; Kwon et al, 2001) (the effect on AQP3 is only partially mediated by stimulating vasopressin V2 receptors). As urinary AQP2 excretion is very low compared to the total AQP2 in the kidney (≈3%), it may not reflect intrarenal changes in the protein. Nevertheless, a positive correlation has been found recently between the maximum changes in the urinary excretion of AQP2 and the maximum changes in plasma vasopressin in healthy subjects (Pedersen et al, 2001) (Figure 1b).
Influence of water intake on the expression of aquaporin 2. (a) Relative mRNA levels of AQP2 in the renal cortex and medulla of rats maintained for 2.5 days on different water intake levels resulting in urine osmolality values of 906, 3140 and 380 mosm/kg H2O in control (open bars), thirsty (solid bars) and highly hydrated (hatched bars) rats, respectively, adapted from Murillo-Carretero et al (1999). (b) Correlation between the maximum changes in plasma vasopressin (ΔAVP) and maximum changes in urinary AQP2 (Δu-AQP2) rate in healthy subject during water deprivation for 24 h, reproduced from Pedersen et al (2001).
The driving force behind the water flux and urine concentration is an osmotic corticomedullary gradient that is built-up as a result of the reabsorption of sodium in the thick ascending limb and the accumulation of urea in the inner medulla. An increase in the abundance of the bumetamide-sensitive Na–K–2Cl cotransporter protein in the thick ascending limb has been observed in the rat kidney in response to either chronic water restriction or chronic infusion of a vasopressin V2 receptor agonist (Kim et al, 1999). However, this direct effect of vasopressin on the reabsorption of sodium in the thick ascending limb occurs only in some rodents. In humans, this nephron segment is devoid of vasopressin-sensitive adenylate cyclase activity (Morel et al, 1987). Facilitated urea transporters are responsible for accumulation of urea in the renal inner medulla. Three major urea transporters have been cloned and located in different structures of the kidney: UT-A1, UT-A2 and UT-B1 (Figure 2a). In rats and human beings, UT-A1 is located in the terminal part of the inner medullary collecting duct and accounts for the vasopressin-dependent increase in the urea permeability of this segment (Knepper & Star, 1990; Bagnasco et al, 2001). Like the aquaporins, chronic vasopressin infusion affects not only UT-A1 but also another urea transporter, UT-A2, located in the thin descending limb of Henle's loop (Bankir & Trinh-Trang-Tan, 2000) (Figure 2b). This effect on UT-A2 must be indirect because there are no vasopressin receptors in the thin descending limb.
Influence of vasopressin on urea transporters. (a) Pathway for urea recycling in the kidney in the presence of vasopressin, reproduced from Bankir and Trinh-Trang-Tan (2000). C: cortex; OS: outer stripe of the outer medulla; IS: inner stripe of the outer medulla; IM: inner medulla; DVR: descending vasa recta; AVR: ascending vasa recta; LH: loop of Henle; CD: collecting duct; UT: urea transporter; AVP: vasopressin. (b) Northern blotting of RNA extracted from the inner stripe of the outer medulla (IS) and the inner medulla (IM) of the kidneys of rats with different levels of urine concentrating activity, reproduced from Bankir and Trinh-Trang-Tan (2000).
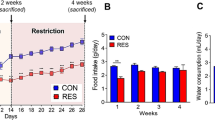
In addition to its effects on water and urea permeability, vasopressin also improves urine concentration by stimulating the reabsorption of sodium from the connecting tubule and the collecting duct, which promotes additional iso-osmotic water reabsorption. This effect involves the activation of the amiloride-sensitive epithelial sodium channel (ENaC). It has been shown recently that vasopressin not only has an acute impact on ENaC-dependent sodium transport (Tomita et al, 1985; Verrey, 1994; Blot-Chabaud et al, 1996; Djelidi et al, 1997) but also has a delayed effect on the expression of β and γENaC subunits, in the kidney, by activating the V2 receptors (Ecelbarger et al, 2000; Nicco et al, 2001) (Figure 3). This effect is accompanied by a significant increase in sodium and water transport (Nicco et al, 2001) (Figure 4), suggesting associated changes in functional ENaC membrane proteins. Interestingly, an increase in the mRNA expression of β and γENaC subunits has also been observed in the lung of rats with either chronic water restriction or chronic infusion of a vasopressin V2 receptor agonist. The concomitant decrease in extrarenal water losses (water intake minus urine flow rate) suggests indirectly that mRNA upregulation is followed by an increase in functional channels and sodium transport and, consequently, in the reabsorption of water (Nicco et al, 2001).
Influence of vasopressin on the mRNA level of the three subunits (α, β, γ) of the epithelial sodium channel (ENaC) in the renal cortex. (a) Brattleboro rats chronically treated with a V2 agonist of vasopressin (n=6, solid bars) or untreated (n=5, open bars). (b) Sprague–Dawley rats chronically treated with a V2 agonist of vasopressin (n=6, solid bars), with restricted drinking water (n=6, hatched bars) or untreated (n=6, open bars). Mean±SEM, *P<0.05, **P<0.002, ***P<0.0005, reproduced from Nicco et al (2001).
Acute effect of vasopressin on transepithelial sodium (right) and water (left) net fluxes in isolated perfused cortical collecting duct from Brattleboro rats pretreated with a V2 agonist of vasopressin (n=4, solid bars) or untreated (n=5, open bars). Mean±SEM, *P<0.01, adapted from Nicco et al (2001).
But overall, the most important consequence of urine concentrating activity is the effect on renal hemodynamics. Several studies have shown that a sustained increase in vasopressin concentration is accompanied by a rise in the renal plasma flow and glomerular filtration rate. Chronic infusion of vasopressin to Brattleboro rats, which are devoid of endogenous vasopressin, increased their renal blood flow and glomerular filtration rate by 40% (Gellai et al, 1984) (Figure 5a). In rats exhibiting various levels of experimentally induced urine concentrating activity, glomerular filtration was highly and positively correlated with urine osmolality (but only if the kidney was producing hyperosmotic urine to plasma) (Bouby et al, 1996) (Figure 5b). The increase in the glomerular filtration rate induced by a protein meal is lower in subjects with high hydration levels than those with low hydration levels (Hadj-Aissa et al, 1992) (Figure 5c). Recently, a positive correlation has been observed between the glomerular filtration rate and urine osmolality with normal fluid intake, but not in the context of water diuresis (Anastasio et al, 2001) (Figure 5d). The normal human glomerular filtration rate is approximately 150 l/day, and 95–99.5% of the water and 99% of the sodium are reabsorbed. So an increase of only 20% of the glomerular filtration rate corresponds to a large additional work load for the kidney.
Influence of vasopressin on the glomerular filtration rate in rats and humans. (a) Effect of the chronic infusion of vasopressin on the glomerular filtration rate in Brattleboro rats. Mean±SEM of five rats, adapted from Gellai et al (1984). (b) Relationship between glomerular filtration rate (averaged 24 h inulin clearance) and urine osmolality in Sprague–Dawley rats, reproduced from Bouby et al (1996). (c) Glomerular filtration rate during the control period and 3 h after a protein meal in 10 healthy subjects on high (open dots) or low hydration (closed dots). Mean±SEM, P<0.05, reproduced from Hadj-Aissa et al (1992) (d) Correlation analysis of glomerular filtration rate and urine osmolality in 12 healthy individuals on low (open dots) or high (closed dots) hydration regimens (average of two consecutive 45 min measurements), reproduced from Anastasio et al (2001).
The mechanism behind the effect of vasopressin on the glomerular filtration rate has not been fully elucidated. It seems to be indirect and related to the depression of tubuloglomerular feedback. It is noteworthy that in contrast during severe dehydration and volume contraction, the kidney perfusion and glomerular filtration rate both decrease.
Functional consequences of high levels of vasopressin in disease states
Animal and human studies have demonstrated that under normal conditions, chronic low hydration plus a high level of vasopressin induce an increase in the expression and activity of water and solute transporters in the kidney, leading to an improvement in the efficiency of the urine concentrating mechanism, and an increase in the glomerular filtration rate. Although several findings suggest that high levels of vasopressin could have deleterious effects in some diseases, there has been little investigation of this topic. We investigated the functional consequences of sustained high levels of vasopressin and urine concentrating activity in the rat in three pathological conditions: chronic renal failure, diabetic nephropathy and salt-sensitive hypertension.
Chronic renal failure
Chronic renal failure can result from various primary renal diseases, but inevitably leads to deterioration of renal function. Owing to the reduced number of functional nephrons, the final urine concentration is reduced, although the glomerular filtration rate and concentrating activity of the individual nephrons are increased. We assume that this hyperconcentration work must have a deleterious effect on the remaining nephrons. This hypothesis was supported by the fact that several studies have shown that a reduction in protein intake slows the progression of chronic renal failure, and we demonstrated that the hyperfiltration induced by high protein intake in normal rats depends, at least in part, on vasopressin and increased urine concentrating activity (Bankir & Kriz, 1995). We devised two experiments in which chronic changes in the concentrating activity were induced by manipulating water intake and/or vasopressin without changing protein intake. The first experiment was undertaken in Sprague–Dawley rats, in which chronic renal failure was induced by 5/6 nephrectomy, and in which the urine concentrating activity was reduced by increasing water intake. In the second experiment, we studied the effect of restoring urine concentrating activity by chronic infusion of a V2 agonist in 5/6 nephrectomized Brattleboro rats (which are devoid of endogenous vasopressin). Both these experiments showed that rats with the lowest urine concentrating activity displayed the slowest progression of chronic renal failure as assessed by the reduction in proteinuria, kidney hypertrophy, incidence of glomerulosclerosis and mortality (Bouby et al, 1990, 1999) (Figure 6). In another study, it has been shown that Brattleboro rats, unlike normal rats, do not present any increase in the single-nephron glomerular hyperfiltration rate after 5/6 nephrectomy (Bregman et al, 1990). These findings show that ADH plays an essential role in the hyperfiltration and degradation of renal function observed in chronic renal failure. Reducing this hyperconcentration work load could therefore be expected to enhance the preservation of the remaining nephrons, at least during the early stages of CRF.
Influence of urine concentrating activity on the progression of chronic renal failure. Left: Sprague–Dawley rats with 5/6 nephrectomy were given an increased water intake for 10 weeks by mixing a water-rich agar gel with their feed (open dots) and were compared to rats with similar initial renal impairement but normal water intake (closed dots). Mean±SEM, n=9 rats per group at the beginning of the experiment, three rats in each group died or were killed during weeks 6–7, adapted from Bouby et al (1990). Right: Brattleboro rats with 5/6 nephrectomy were given an i.p. infusion of a V2 agonist of vasopressin for 15 weeks (open triangles) and were compared to rats with similar initial renal impairment, but no agonist infusion (open dots). Mean±SEM, n=10 rats per group at the beginning of the experiment, adapted from Bouby et al (1999).
Diabetic nephropathy
Diabetic nephropathy develops in 30–50% of type-I and about 10% of type-II diabetic patients. This disease is the most common cause of the end-stage renal disease in the United States and Europe. The presence of elevated microalbuminuria, an early marker of diabetic nephropathy, further increases the risk of cardiovascular disease in diabetic patients at least threefold. Thus, it is important to identify the factors that influence the appearance and onset of albuminuria. In diabetes mellitus, the urine flow rate is markedly increased and urine osmolality decreased, which suggests that kidney's concentrating ability is impaired. However, if we calculate the free water reabsorption that takes into account the load of solutes excreted, it seems that urine concentrating activity is in fact considerably enhanced in diabetes. It was already known that the level of vasopressin increases during diabetes (Bankir et al, 2001), and this elevation of vasopressin is probably an adaptation that limits the osmotic diuresis caused by the high load of solutes originating from glucose wasting and hyperphagia. Secondarily this change could contribute to the development of diabetic nephropathy by a mechanism similar to that responsible for the deleterious effect of vasopressin on the progression of chronic renal failure.
Experimental diabetes was induced by destroying the β cells of the islets of Langherans (injection of streptozotocin), in Long–Evans rats, which do have endogenous vasopressin secretion, and in Brattleboro rats, which are devoid of endogenous vasopressin. These rats were compared to the corresponding healthy control rats. At 4 weeks after inducing of diabetes, the glomerular filtration rate rose significantly in the Long–Evans rats but not in the Brattleboro rats, even though they had similar blood glucose values. Urine albumin excretion, which reflects the degree of glomerular damage and renal mass, increased much less in rats without vasopressin than those with endogenous vasopressin (Bardoux et al, 1999) (Figure 7). In another experiment, we showed that albuminuria was prevented during experimental diabetes in Wistar rats when a V2 receptor antagonist was administered for several weeks (Bardoux et al, 2003). These findings suggest that the action of vasopressin on the kidney is necessary for the manifestation of diabetic hyperfiltration, and that this hormone plays a crucial role in the onset of the renal complications of diabetes.
Creatinine clearance and urinary albumin excretion in control (cont) and diabetic (DM) rats with (Long–Evans) or without (Brattleboro) endogenous vasopressin, 4 weeks after induction of diabetes. Mean±SEM, n=7–8 per group, **P<0.01, ***P<0.001, adapted from Bardoux et al (1999).
Salt-sensitive hypertension
A reduced capacity to excrete sodium is considered to be involved in the pathogenesis of some forms of hypertension. The nature of the defect in renal function responsible for this impaired sodium excretion remains unclear. Several factors are likely to be involved in salt-sensitive hypertension. These include the possible contribution of vasopressin related to its pressor effects, through the activation of V1-vascular receptors, and its water-retention effects, via activation of V2-tubular receptors. However, a high level of vasopressin could increase the risk of sodium retention as a result of its effect on epithelial sodium channel activity. Our hypothesis was based on three main arguments: (1) The importance of the epithelial sodium channel in the sodium balance has been demonstrated by the finding that mutations in the genes coding for its subunits lead to permanent activation of the channel and are responsible for Liddle's syndrome, which is characterized by a severe hypertension (Lifton, 1996; Rossier, 1997). (2) High levels of vasopressin or a tendency to concentrate urine are often associated with a tendency to develop salt-sensitive hypertension (Matsuguchi et al, 1981; Yagil et al, 1996; Zhang et al, 1999). (3) Under physiological conditions, the urinary excretion of water and solutes are independently regulated, but only within given limits. However, when the urine flow rate is relatively low and vasopressin high, the excretion of solutes and especially that of sodium decreases with water excretion (Andersen et al, 1990; Bankir et al, 1995, 1998; Choukroun et al, 1997). In some studies, vasopressin has been reported to have a natriuretic effect, but this was observed only when intense diuresis was interrupted by the systemic infusion of vasopressin, resulting in a volume expansion (Walter et al, 1996). During severe dehydration, it is the fall in aldosterone that is responsible for natriuresis (Merrill et al, 1986).
We studied the influence of stimulating ENaC by the V2 effect of vasopressin in an experimental model of sodium-dependent hypertension: the deoxycorticosterone acetate-salt model. DOCA-salt hypertension was induced in uninephrectomized rats. Three levels of water intake and urine osmolality were obtained by chronically pretreating rats with a V2 agonist or a V2 antagonist or giving no treatment. These treatments induced no major changes in blood volume, and plasma osmolality and natremia were similar in all the groups. Blood pressure was significantly increased by V2 agonist pretreatment (+11 mmHg) and this effect was exacerbated after DOCA–salt-induced hypertension (+17 mmHg) (Figure 8). The V2-agonist-treated rats had a fivefold higher albuminuria, higher mortality rate (50% vs 0% and 0%) and cardiac and renal hypertrophy than those in the other groups. Histological renal lesions were exacerbated by V2 agonism and prevented by V2 antagonism (Fernandes et al, 2002). These findings provide evidence that chronic stimulation of vasopressin V2 receptor raises basal blood pressure in rats, and exacerbates the development of DOCA-salt hypertension, organ damage and mortality. These effects could be, at least in part, due to the sustained stimulation of sodium reabsorption by ENaC in the distal part of the nephron, which promotes sodium retention.
Effects of vasopressin on DOCA-salt hypertensive rats treated with V2-antagonist (hatched bars) or V2-agonist (solid bars) or untreated (open bars). Mean±SEM, n=7 per group,*P<0.05, ***P<0.0001, adapted from Fernandes et al (2002).
References
Anastasio P, Cirillo M, Spitali L, Frangiosa A, Pollastro RM & DeSanto NG (2001): Level of hydration and renal function in healthy humans. Kidney Int. 60, 748–756.
Andersen LJ, Andersen JL, Schütten HJ, Warberg J & Bie P (1990): Antidiuretic effect of subnormal levels of arginine vasopressin in normal humans. Am. J. Physiol. 259, R53–R60.
Bagnasco SM, Peng T, Janech MG, Karakashian A & Sands JM (2001): Cloning and characterization of the human urea transporter UT-A1 and mapping of the human Slc14a2 gene. Am. J. Physiol. Renal Physiol. 281, F400–F406.
Bankir L (2001): Antidiuretic action of vasopressin: quantitative aspects and interaction between V1a and V2 receptor-mediated effects. Cardiovas. Res. 51, 372–390.
Bankir L, Bardoux P & Ahloulay M (2001): Vasopressin and diabetes mellitus. Nephron 87, 8–18.
Bankir L & Kriz W (1995): Adaptation of the kidney to protein intake and to urine concentrating activity: similar consequences in health and CRF. Kidney Int. 47, 7–24.
Bankir L, Niesor R & Bouby N (1995): Sodium excretion is impaired by high urinary concentration. FASEB J. 9, A5.
Bankir L, Pouzet B, Choukroun G, Bouby N, Schmitt F & Mallie JP (1998): Concentrer l'urine ou excréter le sodium: deux exigences parfois contradictoires. Néphrologie 19, 203–209.
Bankir L & Trinh-Trang-Tan MM (2000): Renal urea transporters. Direct and indirect regulation by vasopressin. Exp. Physiol. 85, 243S–252S.
Bardoux P, Bruneval P, Heudes D, Bouby N & Bankir L (2003): Diabetes-induced albuminuria: role of antidiuretic hormone as revealed by chronic V2 receptor antagonism in the rat. Nephrol. Dial. Transplant. 18, 1755–1763.
Bardoux P, Martin H, Ahloulay M, Schmitt F, Bouby N, Trinh-Trang-Tan MM & Bankir L (1999): Vasopressin contributes to hyperfiltration, albuminuria, and renal hypertrophy in diabetes mellitus: study in vasopressin-deficient Brattleboro rats. Proc. Natl. Acad. Sci. USA 96, 10397–10402.
Berl T & Robertson GL (2000): Pathophysiology of water metabolism. In The Kidney. ed. BM Brenner, pp 866–924. Philadelphia: Saunders.
Blot-Chabaud M, Laplace M, Cluzeaud F, Capurro C, Cassingéna R, Vandewalle A, Farman N & Bonvalet JP (1996): Characteristics of a rat cortical collecting duct cell line that maintains high transepithelial resistance. Kidney Int. 50, 367–376.
Bouby N, Ahloulay M, Nsegbe E, Déchaux M, Schmitt F & Bankir L (1996): Vasopressin increases glomerular filtration rate in conscious rats through its antidiuretic action. J. Am. Soc. Nephrol. 7, 842–851.
Bouby N, Bachmann S, Bichet D & Bankir L (1990): Effect of water intake on the progression of chronic renal failure in the 5/6 nephrectomized rat. Am. J. Physiol. (Renal Fluid Electrolyte Physiol. 27) 258, F973–F979.
Bouby N, Hassler C & Bankir L (1999): Contribution of vasopressin to progression of chronic renal failure: study in Brattleboro rats. Life Sci. 65, 991–1004.
Bregman R, Boim MA, Santos OFP, Ramos OL & Schor N (1990): Effects of systemic hypertension, antidiuretic hormone, and prostaglandins on remnant nephrons. Hypertension 15(Suppl 1), I.72–I.75.
Choukroun G, Schmitt F, Martinez F, Drüeke TB & Bankir L (1997): Low urine flow reduces the capacity to excrete a sodium load in humans. Am. J. Physiol. (Regulatory Integrative Comp. Physiol. 42) 273, R1726–R1733.
Djelidi S, Fay M, Cluzeaud F, Escoubet B, Eugene E, Capurro C, Bonvalet JP, Farman N & Blot-Chabaud M (1997): Transcriptional regulation of sodium transport by vasopressin in renal cells. J. Biol. Chem. 272, 32919–32924.
Ecelbarger CA, Kim GH, Terris J, Masilamani S, Mitchell C, Reyes I, Verbalis JG & Knepper MA (2000): Vasopressin-mediated regulation of epithelial sodium channel abundance in rat kidney. Am. J. Physiol.—Renal Physiol. 279, F46–F53.
Fernandes S, Bruneval P, Hagege A, Heudes D, Ghostine S & Bouby N (2002): Chronic V2-vasopressin receptor stimulation increases basal blood pressure and exacerbates deoxycorticosterone acetate–salt hypertension. Endocrinology 143, 2759–2766.
Gellai M, Silverstein JH, Hwang JC, LaRochelle FT & Valtin H (1984): Influence of vasopressin on renal hemodynamics in conscious Brattleboro rats. Am. J. Physiol. (Renal Fluid Electrolyte Physiol. 15) 246, F819–F827.
Hadj-Aissa A, Bankir L, Fraysse M, Bichet DG, Laville M, Zech P & Pozet N (1992): Influence of the level of hydration on the renal response to a protein meal. Kidney Int. 42, 1207–1216.
Ishibashi K, Sasaki S, Fushimi K, Yamamoto T, Kuwahara M & Marumo F (1997): Immunolocalization and effect of dehydration on AQP3, a basolateral water channel of kidney collecting ducts. Am. J. Physiol. 272, F235–F241.
Kim GH, Ecelbarger CA, Mitchell C, Packer RK, Wade JB & Knepper MA (1999): Vasopressin increases Na–K–2Cl cotransporter expression in thick ascending limb of Henle's loop. Am. J. Physiol. 276, F96–F103.
Knepper MA & Star RA (1990): The vasopressin-regulated urea transporter in renal inner medullary collecting duct. Am. J. Physiol. 259, F393–F401.
Kwon TH, Hager H, Nejsum LN, Andersen ML, Frokiaer J & Nielsen S (2001): Physiology and pathophysiology of renal aquaporins. Semin. Nephrol. 21, 231–238.
Lifton RP (1996): Molecular genetics of human blood pressure variation. Science 272, 676–680.
Matsuguchi H, Schmid PG, Van-Orden D & Mark AL (1981): Does vasopressin contribute to salt-induced hypertension in the Dahl strain? Hypertension 3, 174–181.
Merrill DC, Skelton MM & Cowley Jr AW (1986): Humoral control of water and electrolyte excretion during water restriction. Kidney Int. 29, 1152–1161.
Morel F, Imbert-Teboul M & Chabardes D (1987): Receptors to vasopressin and other hormones in the mammalian kidney. Kidney Int. 31, 512–520.
Murillo-Carretero MI, Ilundain AA & Echevarria M (1999): Regulation of aquaporin mRNA expression in rat kidney by water intake. J. Am. Soc. Nephrol. 10, 696–703.
Nicco C, Wittner M, DiStefano A, Jounier S, Bankir L & Bouby N (2001): Chronic exposure to vasopressin upregulates ENaC and sodium transport in the rat renal collecting duct and lung. Hypertension 38, 1143–1149.
Pedersen RS, Bentzen H, Bech JN & Pedersen EB (2001): Effect of water deprivation and hypertonic saline infusion on urinary AQP2 excretion in healthy humans. Am. J. Physiol. Renal Physiol. 280, F860–F867.
Robertson GL (1984): Abnormalities of thirst regulation. Kidney Int. 25, 460–469.
Rossier BC (1997): Cum grano salis: the epithelial sodium channel and the control of blood pressure. J. Am. Soc. Nephrol. 8, 980–992.
Tomita K, Pisano JJ & Knepper MA (1985): Control of sodium and potassium transport in the cortical collecting duct of the rat. J. Clin. Invest. 76, 132–136.
Verrey F (1994): Antidiuretic hormone action in A6 cells: effect on apical Cl and Na conductances and synergism with aldosterone for NaCl reabsorption. J. Membr. Biol. 138, 65–76.
Walter SJ, Tennakoon V, McClune JA & Shirley DG (1996): Role of volume status in vasopressin-induced natriuresis: studies in Brattleboro rats. J. Endocrinol. 151, 49–54.
Yagil C, Ben-Ishay D & Yagil Y (1996): Disparate expression of the AVP gene in Sabra hypertension-prone and hypertension-resistant rats. Am. J. Physiol. (Renal Fluid Electrolyte Physiol. 40) 271, F806–F813.
Yamamoto T, Sasaki S, Fushimi K, Kawasaki K, Yaoita E, Oota K, Hirata Y, Marumo F & Kihara I (1995): Localization and expression of a collecting duct water channel, aquaporin, in hydrated and dehydrated rats. Exp. Nephrol. 3, 193–201.
Zerbe RL, Miller JZ & Robertson GL (1991): The reproducibility and heritability of individual differences in osmoregulatory function in normal human subjects. J. Lab. Clin. Med. 117, 51–59.
Zhang X, Hense HW, Riegger GAJ & Schunkert H (1999): Association of arginine vasopressin and arterial blood pressure in a population-based sample. J. Hypertens. 17, 319–324.
Acknowledgements
We thank L Bankir for fruitful scientific discussions, and Carole Nicco and Pascale Bardoux, PhD students, who performed some of the work reported in this paper.
Author information
Authors and Affiliations
Contributions
Guarantor: N Bouby
Contributors: NB was primarily responsible for the writing of the paper. SF took part in the acquisition of some experimental data and preparation of the paper.
Corresponding author
Rights and permissions
About this article
Cite this article
Bouby, N., Fernandes, S. Mild dehydration, vasopressin and the kidney: animal and human studies. Eur J Clin Nutr 57 (Suppl 2), S39–S46 (2003). https://doi.org/10.1038/sj.ejcn.1601900
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601900
Keywords
This article is cited by
-
Renal transcriptome profiles in mice reveal the need for sufficient water intake irrespective of the drinking water type
Scientific Reports (2022)
-
Impact of water consumption on renal function in the general population: a cross-sectional analysis of KNHANES data (2008–2017)
Clinical and Experimental Nephrology (2021)
-
The effect of long-term dehydration and subsequent rehydration on markers of inflammation, oxidative stress and apoptosis in the camel kidney
BMC Veterinary Research (2020)
-
Contribution of Vesicular Glutamate Transporters to Stress Response and Related Psychopathologies: Studies in VGluT3 Knockout Mice
Cellular and Molecular Neurobiology (2018)
-
Fructokinase activity mediates dehydration-induced renal injury
Kidney International (2014)