Abstract
Summary:
Our objective was to evaluate, probably for the first time, the impact of CD34 subsets on engraftment kinetics in allogeneic PBSC transplantation (PBSCT). PBSC graft components were analyzed in 62 cases for the absolute count/kg of total CD34+ and the following subsets: DR− and +, CD71+/−, CD38+/−, CD33+/− and CD61+/−. Time to ANC >0.5 and >1 × 109/l and platelets >20 and >50 × 109/l was reported. The median value for each parameter was used to discriminate rapid from slow engraftment. Four parameters showed significant predictive power of early neutrophil engraftment, namely CD34+/DR− (P=0.002), CD34+/38− (P=0.02), CD34+/CD61− (P=0.04) and total CD34+ cell dose (P=0.04). Four parameters showed significant predictive power of early platelet engraftment, namely CD34+/CD61+ (P=0.02), CD34+/CD38− and total CD34+ cell dose (P=0.04) and CD34+/CD71− (P=0.05). Comparing patients who received >to those who received < the threshold dose(s), only CD34+/CD38− lost its significance for neutrophil engraftment; and only CD34+/CD61+ retained its significance for platelet engraftment (P=0.03); furthermore, the former group required significantly fewer platelet transfusions (P=0.018). We concluded that in allogeneic PBSCT, the best predictor of early neutrophil engraftment is the absolute CD34+/DR− and for early platelet engraftment is the absolute CD34+/CD61+ cell dose.
Similar content being viewed by others
Main
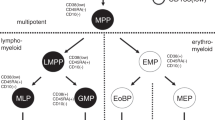
Engraftment kinetics in BM or PBSC transplantation (PBSCT) depends on the number and efficiency of stem cells in the graft. Currently, stem cell evaluation is performed by counting CD34+ cells. However, the phenotypic characterization of primitive cells as CD34+ is far from sufficient and more accurate characterization of progenitors with stem cell potential within the CD34+ population is needed.1,2
In general, the higher the count of CD34+ cells, the more rapid the engraftment and transplanters tend to infuse all the available CD34+ cells even if in very high numbers. Recently, however, infusion of high number of CD34+ cells was shown to be associated with increased risk of chronic GVHD, a highly morbid sequel of BMT.3
Unlike autologous transplantation, securing enough number of CD34+ cells for engraftment is not a common problem in allogeneic BMT except in cord blood transplantation or in case of children donating to adults.4 Many studies have evaluated the impact of CD34+ subsets on engraftment kinetics in autologous PBSCT, but none has addressed this issue in the allogeneic setup. With the introduction of allogeneic PBSCT, concern was raised about the expected higher incidence of GVHD. This was denied by the majority for the acute form, yet increased incidence and severity of chronic GVHD is documented.5 A higher T-cell dose delivered with the graft was implicated by these authors; however, a more recent study pointed to the total CD34+ cell dose as the main factor contributing to chronic GVHD and neither CD3+ nor CD14+ cell dose seemed to play any role.3
CD34+ cells are a heterogeneous population including the early uncommitted fraction as well as different subsets committed to one or the other lineage. Hence, defining the CD34 subset that is most predictive of engraftment and its threshold value would be of utmost importance. Care should be taken to infuse an appropriate number of total CD34+ cells or of the relevant subset(s) to secure engraftment and to avoid infusion of excess CD34+ cells to minimize the risk of chronic GVHD.
In this work, we have analyzed the graft components from 62 PBSC harvests for total CD34+ cells and its subsets. Correlation of the different parameters with time toneutrophil and platelet engraftment as well as their value in predicting rapid engraftment was evaluated. Patients were followed up for a minimum of 19 months. The impact of CD34+ cell dose and subsets on acute and chronic GVHD as well as on relapse and transplantation-related mortality (TRM) was analyzed.
Patients and methods
Patients
The study included 62 patients who received allogeneic PBSCT from HLA-identical siblings in the period between September 2001 and May 2002 at Nasser Institute Hospital and Research center and NCI, Cairo University. Patient's characteristics are shown in Table 1. Written informed consents were obtained from each patient and donor or the parents in those less than 21 years, and the institutional review boards approved the protocol.
Donors
The donors' ages ranged from 2 to 49 with a mean of 22.7+11.8 and a median of 21 years. Donors were treated with GCSF (Filgrastin; Amgen Inc., Thousand Oaks, CA, USA) at a dose of 10 μg/kg per day. Leukapheresis was performed using continuous flow blood separator (Cobe Spectra) in 55 and interrupted flow separator (Hemonetics) in seven cases. Leukapheresis started from day 5 until a CD34+ cell dose of ⩾3 × 106/kg patient body weight was collected. The target was achieved in one setting in 56 and two collections were needed in six cases.
All patients had a central venous line and were nursed under strict protective isolation barrier nursing units with HEPA-filtered air. For the remaining supportive care (including antimicrobial prophylaxis, hydration, hemorrhagic cystitis prophylaxis, parental nutrition and blood component support), all patients were managed using the same protocol. A total of 23 patients received CY–TBI regimen in the form of a total dose of radiotherapy of 10 Gy fractionated over 4 consecutive days (4 × 2.5 Gy), followed by cyclophosphamide 60 mg/kg/day for 2 consecutive days. In all, 16 patients received BU–CY regimen in the form of busulfan 4 mg/kg/day for 4 consecutive days followed by cyclophosphamide 60 mg/kg/day for 2 consecutive days. Eight patients (SAA) received CY/ATG in the form of cyclophosphamide 50 mg/kg/day for 4 consecutive days followed by ATG 10 mg/kg/day for 3 consecutive days. A total of 15 patients received Alk/Flu (nonmyeloablative) in the form of Alkerane 70 mg/m2/day for 2 consecutive days followed by Fludarabine 30 mg/m2/day for 4 consecutive days. Cyclosporine (CSP) + methotrexate (MTX) was given to myeloablated and CSP + MMF (Cellcept, Roche) to nonmyeloablated patients as GVHD prophylaxis.
CD34+ and subsets evaluation
Enumeration of CD34+ cells and the various uncommitted and lineage committed subsets namely DR−/+, CD38−/+, CD71−/+, CD33−/+ and CD61−/+ were performed using double and triple staining with the following panel of monoclonal antibodies (mAbs):
-
CD45 FITC/CD34 PE/CD38 Cy5
-
CD71 FITC/CD34 PE/CD33 Cy5
-
CD61 FITC/CD34 PE
-
DR FITC/CD34 PE
-
Isocontrol IgG1-FITC/IgG1R-PE/IgG1 Cy-Q, IQP-491 FRC
CD34 (HPCA-2PE) and isocontrol were obtained from Becton and Dickinson, San Jose CA, USA. Other mAbs were obtained from Dako A/S Denmark, Pharmingen, San Diego, CA, USA, and Serotec, UK/International.
Whole blood staining was performed as previously described.6 In short, 10 μl of specific mAb or isotype control was added to 100 μl whole blood and incubated for 30 min at 4°C in the dark. Cells were washed once with hemolysing solution (lyse no wash method). Analysis was performed on Coulter XL Flow Cytometer using the ISHAGE protocol to determine the percentage of CD34+ cells.7 Percentage of various subsets was evaluated by gating on CD34+ cells. Absolute values for CD34+ and various subsets were calculated.
Evaluation of engraftment
Five patients died before engraftment and were excluded from analysis. Time to neutrophil engraftment was defined as the first of 3 consecutive days in which the absolute neutrophil count (ANC) was ⩾0.5 × 109/l; time to TLC and neutrophil count ⩾1 × 109/l was also determined. Time to platelet engraftment was defined as the first of 3 consecutive days in which the transfusion-independent platelet count was ⩾20 × 109/l; time to platelet count of ⩾50 × 109/l was also determined. The median for each parameter was used to discriminate rapid from slow engraftment.
Follow up of the patients
Patients were followed up for a period of 19–30 months with a median of 25 months. Acute and chronic GVHD were reported as well as relapse and transplantation related mortality (TRM).
Statistical analysis
Statistical Package for Social Sciences (SPSS) version 10.0. was used for data analysis. The absolute values of CD34+ cells and its subsets were expressed as mean±s.d./kg recipient body weight, minimum, maximum and median were also recorded. Non parametric t test (Mann–Whitney test) was used for comparing means of two groups. Correlation between infused dose of CD34+ cells and various subsets with time to neutrophil and platelet engraftment was performed using Pearson correlation analysis. The predictive power for early engraftment (⩽median value) of each component was evaluated using receiver operator characteristic curve (ROC) and the threshold value for rapid hematopoietic recovery defined by the optimal sensitivity. To test the validity of the threshold value to discriminate between rapid and slow engraftment, the Kaplan–Meier test was used to evaluate the difference in engraftment kinetics between patients who received ⩾and those who received < the threshold dose; statistical significance was determined by log rank. For all the tests performed, a P-value of ⩽0.05 was considered significant.
Results
The percentage and absolute count of CD34+ cells and subsets obtained from different donors were extremely variable. No correlation was encountered between the yield of any of the components with either age, body weight or surface area of the donor.
The infused dose of total CD34+ cells and its subsets was extremely variable for different patients (Table 2). No correlation was encountered between total CD34+ cells and any of the subsets or between the subsets and each other. The time to achieve transfusion independent TLC of ⩾1 × 109/l, ANC of ⩾0.5 × 109/l, and ⩾1 × 109/l and platelets ⩾20 and ⩾50 × 109/l in the evaluable 57 patients is shown in Table 3.
One patient directly attained the threshold for both TLC and ANC of ⩾1 × 109/l on the same day; on the previous day he had ANC <0.5 × 109/l. Excluding this patient, the range for TLC ⩾1 × 109/l would be 7–22 days and for ANC ⩾0.5 × 109/l would be 8–26 days and ⩾1 × 109/l would be 9–27 days. Two patients suffered from complications before platelet engraftment and were excluded from analysis. Platelet count ⩾100 × 109/l was recorded in 38 patients and achieved after a median of 15.5 days (range 10–31) days. There was no relation between engraftment time and either age or gender of the patients. There was no difference in the engraftment time between patients who received myeloablative or nonmyeloablative conditioning regimen. Within the former group there was no impact of TBI on engraftment kinetics (Table 4).
Impact of total CD34+ cells and subsets on engraftment kinetics
Some correlation was encountered between time to ANC ⩾0.5 × 109/l and three parameters namely total CD34+ cell dose (r −0.28, P=0.03), CD34+/CD61− (r −0.27, P=0.045) and CD34+/CD33− (r −0.253, P=0.058). No correlation was encountered between any of the parameters and either TLC or ANC ⩾1 × 109/l or platelet engraftment.
The median value for time to achieve the target counts was used to discriminate rapid from slow engraftment. Only CD34+/DR− subset showed predictive power for early TLC engraftment at <13 days (71%, P=0.02) at a threshold dose of 1.29 × 106/kg. The 40 patients who received ⩾ the threshold engrafted at 12.6±2.1 days with a range of 7–20 and a median of 12 days; the 17 patients who received <1.29 × 106/kg engrafted at 15.7±6.3 with a range of 8–32 and a median of 15 days (P=0.009).
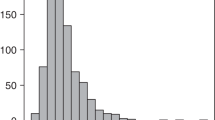
Four parameters were predictive of early neutrophil engraftment (Figure 1). They included CD34+/DR−, CD34+/CD38−, CD34+/CD61− and total CD34+ cell dose at a threshold of 2.12, 3.51, 8.11 and 8.95 × 106/kg, respectively. The probability for early engraftment was 80% (P=0.002), 73% (P=0.02), 70% (P=0.04) and 69% (P=0.04) for the four subsets. Comparing engraftment time of patients who received ⩾ to those who received < the threshold dose, the CD34+/CD38− subset lost its significance. Significant difference was obtained with the other three parameters. For CD34+/CD61− subset, the 28 patients who received ⩾8.11 × 106/kg engrafted at 12.9±1.8 days (range 8–19, median 12) compared to 15.9±3.5 days (range 8–32, median 15) in the 29 patients who received <8.11 × 106/kg (P=0.001). For total CD34+ cell dose, the 30 patients who received ⩾8.95 × 106/kg engrafted at 13±2.5 days (range 8–19, median 13) compared to 16.1±5.1 days (range 8–32, median 15) in the 27 patients who received <8.95 × 106/kg (P=0.004). For the CD34+/DR− subset, the 26 patients who received ⩾2.12 × 106/kg engrafted at 13.1±2.7 days (range 8–20, median 13) compared to 15.6±3.7 days (range 9–32, median 15) in the 31 patients who received <2.12 × 106/kg (P=0.01).
Four parameters were predictive of early platelet engraftment to ⩾20 × 109/l (Figure 2). They included CD34+/CD61+, CD34+/CD38−, total CD34+ and CD34+/CD71− cell dose at a threshold of 1.19, 4.99, 8.85 and 6.51 × 106/kg, respectively. The probability for early engraftment was 71% (P=0.02), 69% (P=0.04), 69% (P=0.04) and 68% (P=0.05) for the four subsets. Comparing engraftment time in patients who received ⩾ to those who received < the threshold dose, only CD34+/CD61+ retained its statistical significance. The 30 patients who received CD34+/CD61+ dose of ⩾1.19 × 106/kg had a transfusion independent platelet count of ⩾20 × 109/l at 11.9±3.8 days with a range of 7–25 and a median of 10 days; the 25 patients receiving lower doses had an engraftment at 16.4±9.8 days with a range of 8–46 and a median of 13 days (P=0.03). The former group required significantly fewer platelet units being 2.6±3.15 (range 0–10, median 1) compared to 4.31±3.5 (range 0–12, median 3) in the second group (P=0.018). No significant difference in the time to platelet count of ⩾50 × 109/l was encountered between the two groups.
Impact of total CD34+ cell count and subsets on GVHD
Acute GVHD was encountered in nine out of the 57 evaluable patients; five had grade 1 and four had grades 2–4. There was no significant impact of CD34+ cells or any of its subsets (% or absolute) on occurrence or severity of acute GVHD.
Chronic GVHD occurred in 14 out of the 57 patients being de novo in 12 and secondary to acute GVHD in two cases. There was no impact of CD34+ cells or subsets on the occurrence of chronic GVHD except for a lower absolute CD34+/CD33+ cell dose in the 14 patients who developed (3.17±4.7 × 106/kg) compared to the 43 patients who did not develop chronic GVHD (5.4±6.3 × 106/kg). The difference was statistically significant (P=0.037). Using ROC curve analysis, CD34+/CD33+ cell dose was a negative predictor of chronic GVHD at a threshold of 1.33 × 106/kg with a sensitivity of 64%, a specificity of 77.1% and a total accuracy of 72.6%. Comparing patients who received ⩾ to those who received < the threshold dose, 5/41 (12.2%) of the first group developed chronic GVHD compared to 9/21 (42.9%) of the second. The difference was found to be statistically significant (P=0.006) (Figure 3).
Impact of CD34+ cell dose and subsets on relapse and TRM
Patients were followed up for a period of 19–30 months with a median of 25 months. Relapse occurred in six patients at 135–305 days post transplant. They included one CLL, two ALL, two ANLL and one MDS patient. Autologous reconstitution occurred in one patient with SAA at day 200. All seven patients died. In all, 16 more patients died, 13 with infection associated with VOD in one, with acute GVHD in another and with chronic GVHD in a third. The remaining three cases died, one with isolated VOD and the other two with severe acute GVHD. CD34+ cell dose and subsets had no impact neither on relapse nor on TRM. There was no statistically significant difference in the doses of various subsets transfused between patients who relapsed and those that were still in remission and between those who died and those who were still alive at last follow-up.
Discussion
Rapid and durable engraftment is the immediate post transplantation concern. Hence, proper assessment of the graft potential to achieve this goal is essential. The specific biological factors leading to a more rapid engraftment are yet to be identified fully and represent a gap in the basic understanding of stem cell biology.8 With the introduction of PBSC as a substitute for BM in many cases, it was realized that there are important phenotypic and biologic distinction between them; the former is claimed to be associated with more rapid engraftment.9,10,11,12 These considerations make it essential to evaluate, properly, the engraftment potential especially in case of PBSCT. Although the specific identification of stem cells remains illusive, they can be phenotypically identified as a subset of all circulating CD34+ cells; standardized methods of their enumeration are well established7,13 and total CD34+ cell dose is currently the golden standard in evaluation of the graft. However, with the same CD34+ cell dose/kg body weight variability in engraftment kinetics are still encountered. Very high doses of CD34+ cells are always associated with prompt engraftment;14,15 on the other, hand low doses are known to result in delayed engraftment.16,17,18 It is the intermediate dose that exhibits marked variability that is not directly correlated to the total CD34+ cell dose.16 The clinical importance of an accurate indication of graft stem cell content and the definition of an optimal PBSC dosage has become clear.2 Among other reasons, the minimum threshold dose of PBSCs required to obtain adequate engraftment can be affected by the composition of the stem cell graft, that is, the balance of subpopulations of CD34+ HSC.19 Accordingly, search for CD34+ subset(s) that could be better predictor(s) of engraftment has gained a lot of interest in the past few years.20 All the studies available in the literature deal with autologous transplantation. However, the kinetics of engraftment would be expected to be the same whether the graft is an auto or an allo one. Marked variability in the relative constitution of the graft with regard to CD34 subsets was reported after mobilization with GCSF alone21,22 or with both chemotherapy and GCSF.13,21 A range of 0-90% for CD34+/CD33− of the total CD34+ population was reported by Millar et al22 and of 0–99% by Pecora et al.21 Ranges of 4.8–47.5% for CD34+/CD38−, of 2–48.4% for CD34+/DR−, of 46.4–89.5% for CD34+/CD71+ and of 47.6–97.2% for CD34+/CD13+ were also reported.20
With the introduction of PBSCT, concern was raised about the potential higher risk of GVHD. Many randomized controlled trials6,9,11,22,23 and many cohort studies12,24,25,26 have examined the relative risk of acute and chronic GVHD after PBSCT. All have concluded that the risk of acute GVHD is not higher in PBSCT compared to BMT, but the findings in relation to chronic GVHD were controversial. A comparable incidence was claimed by some authors.21,27 However increasing evidence supports that with PBSCT, chronic GVHD is of higher incidence, likely to be more severe3,5 and more difficult to control.28 A higher T-cell dose delivered with the graft was accused by Cutler et al;5 however, the study of Zauch et al3 pointed to the total CD34+ cell dose as the main factor contributing to chronic GVHD and neither CD3+ nor CD14+ cell dose seemed to play any role. A highly morbid condition as it is, chronic GVHD is claimed to be protective against relapse5,29 and may be associated with better long-term survival particularly in high-risk patients.12,30,31 Accordingly, proper evaluation of the engraftment potential of the CD34+ population and its subsets included in the graft might be helpful to determine the dose needed to secure engraftment and at the same time to decrease the risk of chronic GVHD especially in standard-risk patients.
In the present work, we analyzed the impact of total CD34+ cells as well as different subsets on neutrophil engraftment presented by ⩾0.5 and ⩾1 × 109/l and platelet engraftment presented by ⩾20 and ⩾50 × 109/l as well as their impact on acute and chronic GVHD, relapse and TRM.
No significant correlation to platelet engraftment was encountered while fair correlation to neutrophil engraftment was encountered with three subsets namely total CD34+, CD34+/CD38− and CD34+/CD61− cell dose. Four parameters were predictors of rapid neutrophil engraftment (⩽14 days); the best being CD34+/DR−, CD34+/CD38−, CD34+/CD61− and total CD34+. Comparing engraftment kinetics in patients who received ⩾ to those who received < the threshold dose, statistically significant shorter time to engraftment was encountered with all except CD34+/CD38− subset. Four parameters were predictors of early platelet engraftment (⩽11 days), namely CD34+/CD61+, CD34+/CD38−, total CD34+ and CD34+/CD71−. Comparing engraftment kinetics in patients who received ⩾ to those who received < the threshold dose, a significantly shorter time to platelet engraftment was encountered only with CD34+/CD61+ subset. A relationship between the dose of CD34+ cells and the tempo of hematological recovery has been demonstrated for both BMT17 and PBSCT.18 The higher the CD34+ cell dose, the quicker the recovery.14,32,33,34 The relative importance of total CD34+ cells and its different subsets as predictors of early and/or durable engraftment was quite variable in different reports. For neutrophil engraftment, total CD34+ cell dose was claimed to be a better predictor.35,36 However, this was denied by the majority of workers; the most commonly reported predictors were CD34+/CD33−, CD34+/CD38− and CD34+/L-selectin+ cell dose.37,38,39 CD34+/Thy1+ cell dose was claimed to be important for durability.13 The relative importance of subsets may be more evident when low numbers of CD34+ cells are infused; the presence of higher numbers of CD34+/CD33− or CD34+/CD38− cells predicts early neutrophil engraftment.20,40 For platelet recovery, total CD34+ cell dose was recognized as a predictor as well as the following subsets: CD34+/CD33−, CD34+/CD38−, CD34+/CD38+, CD34+/CD41 &/or CD61+ and CD34+/L-selectin+.13,37 Platelet recovery has been reported to be more sensitive to CD34+ dose than neutrophil recovery;8,41 the threshold dose to achieve rapid platelet recovery varied between 5 × 106/kg42,43,44,45 and 15 × 106/kg.46 Patients who received >5 × 106 CD34+ cells/kg required significantly fewer platelet units,45 shorter duration of antibiotic therapy45,47 and shorter hospital stay.47 Studies on cord blood were of special importance on account of the longer time needed for hemopoietic reconstitution especially of platelets. The observation that the best predictor of neutrophil recovery is the total progenitor cell dose transplanted for kg body weight of the patient,48 prompted analysis whether the dose of the progenitor cell subset specific for megakaryocytic differentiation (measured in colony assay as Meg-CFC) would better predict time for platelet recovery. However, this was not found to be the case49 because in cord blood there is a perfect correlation between the Meg-CFC and the total CFC content. Apparently, this perfect correlation is not maintained after mobilization whether by GCSF alone or in combination with chemotherapy20,21,22, which was further emphasized by the results of the current study.
In this work, comparing platelet engraftment kinetics in patients who received ⩾ to those who received < the threshold dose of CD34+ cells and different subsets, only CD34+/CD61+ retained its statistical significance (P=0.03). Furthermore, the former group required significantly lower number of platelet units compared to the latter group (P=0.018).
The marked variability in the literature may be attributed to the variability in the subsets tested in each study, the method of statistical analysis using univariate vs Cox proportional hazards models35 and the studied patient population. One important explanation may be derived from ISHAGE, 1999 report46 who documented rapid trilineage engraftment in all cases receiving ⩾10–15 × 106/kg total CD34+ and slow engraftment with a dose <2 × 106/kg body weight. With doses in the range of 2–10 × 106/kg, platelet engraftment could not be predicted from total CD34+ cells but in 75% of cases it could be predicted from CD34/CD61+ (P<0.02) and CD34+/CD38− (P<0.001) and in the remainder from CD34+/GlycoA (P<0.05) and CD34+/TPO+ (P<0.01). Accordingly, in cases giving excellent yield as in cancer breast, all patients would lie within the high-dose category with rapid short recovery not correlated to any CD34+ cell subset.36 While in other cases with variable yields, different subsets may gain a predictive power, not only for rapid engraftment but also as an indicator of post transplant G-CSF administration.50,51 These latter authors proposed a cutoff of 5 × 106/kg CD34+/CD38− cell dose to justify the need for post transplant G-CSF.
In this work, the cutoff threshold of total CD34+ cells to secure rapid engraftment was 8.95 × 106/kg body weight. Although we are dealing with allografts, yet this compares well to the ⩾10 × 106/kg reported for the autografts. It would be recommended that this latter dose should not be exceeded to avoid long-term deleterious effects in the form of chronic GVHD at least in standard-risk patients. With lower doses it is important to analyze the CD34+ subsets. In this work, however, we could not confirm the previous finding that a higher dose of CD34+ cells is associated with a higher incidence of chronic GVHD. The only significant finding was a negative impact of absolute CD34+/CD33+ cell dose on chronic GVHD. A large scale study including all possible subsets on a large number of patients is recommended to define the most relevant predictor(s) of rapid engraftment, to define the cutoff threshold that would secure engraftment (even if delayed) and to define the cutoff at which GCSF should be started immediately post transplant not waiting for the possible delay as well as to document the potential impact on incidence and/or severity of chronic GVHD.
References
Andrews RG, Briddell RA, Hill R et al. Engraftment of primates with G-CSF mobilized peripheral blood CD34+ progenitor cells expanded in G-CSF, SCF, MGDF decreases the duration and severity of neutropenia. Stem Cells 1999; 17: 210–218.
Siena S, Schavo R, Pedrazzoli P, Carlo-Stella C . Therapeutic relevance of CD34 cell dose and blood cell transplantation for cancer therapy. J Clin Oncol 2000; 18: 1360–1377.
Zaucha JM, Gooley T, Bensinger WI et al. CD34 cell dose in granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear allografts affects engraftment kinetics and development of extensive chronic graft versus host disease after human leukocyte antigen-identical sibling transplantation. Blood 2001; 98: 3221–3227.
Belvedere O, Feruglio C, Malangone W et al. Increased blood volume and CD34+/CD38− progenitor cell recovery using a novel umbilical cord blood collection system. Stem Cells 2000; 18: 245–251.
Cutler C, Giri S, Jeyapalan S . Incidence of acute and chronic graft versus host disease after allogeneic peripheral blood stem cell and bone marrow transplantation: a meta-analysis. Blood 2000; 96: 205a (Abstract).
Mahmoud HK, Fahmy OA, Kamel A et al. Peripheral blood vs bone marrow as a source for allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 1999; 24: 355–358.
Sutherland DR, Anderson L, Keeney M et al. The ISHAGE guidelines for CD34+ cell determination by flow cytometry. J Hematother 1996; 5: 213–226.
Cutler C, Antin JH . Peripheral blood stem cells for allogeneic transplantation: a review. Stem Cells 2001; 19: 108–117.
Schmitz N, Bacigalupo A, Hasenclever D . Allogeneic bone marrow transplantation vs filgrastim-mobilised peripheral blood progenitor cell transplantation in patients with early leukaemia: first results of randomised multicentre trial of European Group for Blood and Marrow Transplantation. Bone Marrow Transplant 1998; 21: 995–1002.
Blaise D, Kuentz M, Bontrop RE, Fortanier C . Randomized trial of bone marrow versus lenogastrim-primed blood cell allogeneic transplantation in patients with early-stage leukemia: a report from the Societe Francaise de Greffe de Moelle. J Clin Oncol 2000; 18: 534–546.
Powles R, Mehta J, Kulkarni S . Allogeneic and bone marrow stem cell transplantation in hematological malignant diseases: a randomised trial. Lancet 2000; 335: 1231–1237.
Champlin RE, Schmitz N, Horowitz MM et al. Blood stem cells compared with bone marrow as a source of hematopoieic cells for allogeneic transplantation. Blood 2000; 95: 3702–3709.
Pratt G, Rawstron AC, English AE et al. Analysis of CD34+ cell subsets in stem cell harvests can more reliably predict rapidity and durability of engraftment than total CD34+ cell dose, but steady state levels do not correlate with bone marrow reserve. Br J Haematol 2001; 114: 937–943.
Miflin G, Russell NH, Hutchinson RM . Allogeneic blood stem cell transplantation for haematological malignancies – an analysis of kinetics of engraftment and GVHD risk. Bone Marrow Transplant 1997; 19: 9–13.
Shpall EJ, Champlin R, Glaspy JA . Effect of CD34+ peripheral blood progenitor cell dose on hematopoietic recovery. Biol Blood Marrow Transplant 1998; 4: 84–92.
Johnsen HE, Knudsen LM, Shiodt I et al. Delayed platelet recovery is predicted by CD34+ subset enumeration and not by CD34+ quantification in most patients autotransplanted. The International Society for Hematotherapy and Graft Engineering (ISHAGE), Oslo, Norway, May 28–June 1 (Abstract).
Mavroudis DA, Read EJ, Cottler-Fox M et al. CD34+ cell dose predicts survival, post transplant morbidity and rate of hematologic recovery after allogeneic marrow transplants for hematologic malignancies. Blood 1996; 88: 3223–3229.
Ilhan O, Arslan O, Arat M . The impact of the CD34+ cell dose on engraftment in allogeneic peripheral blood stem cell transplantation. Transfus Sci 1999; 20: 69–71.
Banett D, Granger V, Kraan J et al. Reduction of intra- and inter laboratory variation in CD34+ stem cell enumeration using stable test material, standard protocol and targeted training. Br J Haematol 2000; 108: 784–792.
Gonzalez-Requejo A, Madero L, Diaz MA et al. Progenitor cell subset and engraftment kinetics in children undergoing autologous peripheral blood stem cell transplantation. Br J Haematol 1998; 101: 104–110.
Pecora AL, Preti RA, Gleim GW et al. CD34+CD33- cells influence days to engraftment and transfusion requirements in autologous blood stem-cell recipients. J Clin Oncol 1998; 16: 2093–2104.
Millar BC, Millar JL, Shepherd V et al. The importance of CD34+/CD33− cells in platelet engraftment after intensive therapy for cancer patients given peripheral blood stem cell rescue. BMT 1998; 22: 469–475.
Vigorito AC, Azevedo WM, Marques JF . A randomized prospective comparison of allogeneic bone marrow and peripheral blood progenitor cell transplantation in the treatment of haematological malignancies. Bone Marrow Transplant 1998; 22: 1145–1151.
Bensinger WI, Martin PJ, Storer B et al. Transplantation of bone marrow as compared with peripheral blood cells from HLA identical relatives in patients with hematologic cancers. N Engl J Med 2001; 244: 175–181.
Azevedo WM, Aranha FJP, Gouvea AC et al. Allogeneic transplantation with blood stem cells mobilized by rhG-CSF for hematological malignancies. Bone Marrow Transplat 1995; 16: 647–653.
Przepiorka D, Smith TL, Folloder J . Risk factors for acute graft-versus-host disease after allogeneic blood stem cell transplantation. Blood 1999; 94: 1465–1470.
Kubel M, Leiblein S, Ponisch W . Comparison of HLA-identical transplantation of unselected blood stem cells (PBSCT) and bone marrow (BMT) from related donors in patients with hematologic malignancy: a single center report. Bone Marrow Transplant 1998; 22 (Suppl. 2): S27 (Abstract).
Couban S, Simpson DR, Barnett MJ et al. A randomized multicenter comparison of bone marrow and peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood 2002; 100: 1525–1531.
Flowers MED, Parker PM, Johnston LJ et al. Comparison of chronic graft-versus-host disease after transplantation of peripheral blood stem cells versus bone marrow in allogeneic recipients: long term follow up of a randomized trial. Blood 2002; 100: 415–419.
Elmaagacli A, Beelen DW, Opalka B . The risk of residual molecular and cytogenetic disease in patients with Philadelphia-chromosome positive first chronic phase chronic myelogenous leukemia is reduced after transplantation of allogeneic peripheral blood stem cells compared with bone marrow. Blood 1999; 94: 384–389.
Bensinger WI, Martin P, Clift R . A prospective randomized trial of peripheral blood stem cells (PBSC) or bone marrow (BM) for patients undergoing allogeneic transplantation for hematologic malignancies. Blood 1999; 94 (Suppl 1): 10a (Abstract).
Diez-Campelo M, Perez-Sim JA, Martino A et al. Impact of CD34+ cell dose on the outcome of patients undergoing reduced intensity conditioning allogeneic peripheral blood stem cell transplantation. Hematol J 2003; 4 (Suppl 2): 0460 (Abstract).
Haas R, Witt B, Mohle R et al. Sustained long-term hematopoiesis after myeloablative therapy with peripheral blood progenitor cell support. Blood 1995; 85: 3754–3761.
Salazar R, Sola C, Maroto P . Factors affecting CD34+ cell mobilization with cyclophosphamide and G-CSF and hematopoietic recovery after high-dose chemotherapy and stem cell support in solid tumor patients. Proc Am Soc Clin Oncol 1996; 17: 95a (Abstract).
Beguin O, Baudoux E, Sautois B . Hematopoietic recovery in cancer patients after transplantation of autologous peripheral blood CD34+ cells or unmanipulated peripheral blood stem and progenitor cells. Transfusion 1998; 38: 199–208.
Stewart DA, Guo D, Luider J et al. The CD34+90+ cell dose does not predict early engraftment of autologous blood stem cell as well as the total CD34+ cell dose. Bone Marrow Transplant 2000; 25: 435–440.
Dazzi C, Cariello A, Rosti G et al. Relationships between total CD34+ cells reinfused, CD34+ subsets and engraftment kinetics in breast cancer patients. Hematologica 2000; 85: 396–402.
Baech J, Johnsen HE . Concise review: technical aspects and clinical impact of hematopoietic progenitor subset quantification. Stem Cells 2000; 18: 76–86.
Drecksen MW, Gerritsen WR, Rodenhuis S et al. Expression of adhesion molecules on CD34+ cells: CD34+ L-selectin+ cells predict a rapid platelet recovery after peripheral blood stem cell transplantation. Blood 1995; 11: 3313–3319.
Drecksen MW, Rodenhuis S, Dirkson MKA et al. Subsets of CD34+ cells and rapid hematopoietic recovery after peripheral-blood stem-cell transplantation. J Clin Oncol 1995; 13: 1922–1932.
Verfaillie CM, Ploemacher R, Di Persio J et al. ISHAGE scientific committee report: assays to determine hematopoietic stem cell content in blood or marrow grafts. Cytotherapy 1999; 1: 41–49.
Watts MJ, Sullivan AM, Jamieson E et al. Progenitor-cell mobilization after low-dose cyclophosphamide and granulocyte colony-stimulating factor: an analysis of progenitor-cell quantity and quality and factors predicting for these parameters in 101 pretreated patients with malignant lymphoma. J Clin Oncol 1997; 15: 535–546.
Van-der Wall E, Richel DJ, Holtkamp MJ et al. Bone marrow reconstitution after high-dose chemotherapy and autologous peripheral blood stem cell transplantation: effect of graft size. Ann Oncol 1994; 5: 795–802.
Bensinger WI, Appelbaum FR, Rowley S et al. Factors influencing collection and engraftment of autologous peripheral blood stem cells. J Clin Oncol 1995; 13: 2547–2555.
Glaspy J, Lu ZJ, Wheeler C . Economic rationale for infusing optimal numbers of CD34+ cells in peripheral blood progenitor cell transplants. Blood 1997; 90 (Suppl. 1): 370a (Abstract).
Kiss JE, Rybka WB, Winkelsein A et al. Relationships of CD34+ cell dose to early and late hematopoiesis following autologous peripheral-blood stem-cell transplantation. Bone Marrow Transplant 1997; 19: 303–310.
Ketterer N, Salles G, Raba M et al. High CD34+ cell counts decrease hematologic toxicity of autologous peripheral blood progenitor cell transplantation. Blood 1998; 91: 3148–3155.
Migliaccio AR, Adamson JW, Stevens CE et al. Cell dose and speed of engraftment in placental/umbilical cord blood transplantation: graft progenitor cell content is a better predictor than nucleated cell quantity. Blood 2000; 96: 2717–2722.
Von Drygalski A, Xu G, Constantinescu D et al. The frequency and proliferative potential of megakaryocytic colony-forming cells (Meg-CFC) in cord blood, cytokine mobilized peripheral blood and bone marrow, their correlation with total CFC numbers: implications for the quantitation of Meg-CFC to predict platelet engraftment following cord blood transplantation. BMT 2000; 25: 1029–1034.
Sola C, Maroto P, Salazar R . High dose chemotherapy (HDC) and peripheral blood stem cell (PBSC) autologous transplantation: influence of the number of infused CD34+ cells in hematopoietic recovery and support measures required. Oncol 1996; 15: 538 (Abstract).
Henon PH, Sovalat H, Bourderont D . Importance of CD34+ cell subsets in autologous PBSC transplantation, the mulhouse experience using CD34+ CD38− cells as predictive tool for hematopoietic engraftment. J Biol Regul Homeost 2001; 15: 62–67.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kamel, A., El-Sharkawy, N., Mahmoud, H. et al. Impact of CD34 subsets on engraftment kinetics in allogeneic peripheral blood stem cell transplantation. Bone Marrow Transplant 35, 129–136 (2005). https://doi.org/10.1038/sj.bmt.1704755
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704755
Keywords
This article is cited by
-
Nomogram for Predicting Early Mortality after Umbilical Cord Blood Transplantation in Children with Inborn Errors of Immunity
Journal of Clinical Immunology (2023)
-
Allogeneic transplantation of peripheral blood stem cell grafts results in a massive decrease of primitive hematopoietic progenitor frequencies in reconstituted bone marrows
Bone Marrow Transplantation (2020)
-
Filgrastim-alone versus pegylated filgrastim-alone for autologous peripheral blood stem cells mobilization in newly diagnosed multiple myeloma patients
Wiener klinische Wochenschrift (2017)
-
Multi-color immune-phenotyping of CD34 subsets reveals unexpected differences between various stem cell sources
Bone Marrow Transplantation (2016)
-
Prospective cohort study of the circadian rhythm pattern in allogeneic sibling donors undergoing standard granulocyte colony-stimulating factor mobilization
Stem Cell Research & Therapy (2013)