Abstract
Study design: Case report.
Objective: To report a case of spinal cord infarction after a self-inflicted needle stick injury, following an injection of heroin into the cord.
Setting: National spinal injury unit in a Scottish University teaching hospital, Glasgow, UK.
Case report: A 20-year-old male, injected street heroin accidentally into the cord through the left side of the neck, leading to sudden loss of power to all four limbs. Initial magnetic resonance imaging scans showed extensive cord oedema and follow-up scans showed signal changes within the anterior horns of the spinal cord in keeping with a cord infarct.
Conclusion: Self-inflicted spinal cord injury with a small needle is difficult, but not impossible. Cord infarct as a result of a self-inflicted injury has not been previously reported. The mechanism of the injury resulting in cord infarction is explained by the vascular anatomy of the spinal cord circulation, and this may also explain the residual neurological status of the patient.
Similar content being viewed by others
Introduction
Spinal ischaemia or infarction is a rare cause of spinal cord injury. We report an accidental self-inflicted spinal cord injury due to a needle stick injury leading to cord ischaemia.
Case history
The patient was a 27-year-old man addicted to intravenous heroin. He had a history of hepatitis C and convulsions. He had been prescribed anticonvulsants and was on methadone treatment for withdrawal.
Since he was unable to gain intravenous access to his peripheral veins he tried to inject heroin (diluted with water and citric acid) into the vessels on the left side of his neck using a size 23 G needle. After injecting a small amount he felt tingling and pain in all four limbs after which he lost the power in his legs and collapsed. He was admitted to the local hospital and then he was transferred to the National Spinal Injuries Unit.
Initial examination showed a puncture mark on the left side of the neck just posterior to the clavicular insertion of the sternocleidomastoid and just above the clavicle. He had a sensory deficit below the C-8 level and complete weakness of the upper limbs below C-6 level and also of the left lower limb. There was some movement of the right lower limb. He had urinary retention and decreased anal tone. On admission to the unit he had an ASIA1 motor score of 48.
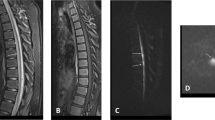
Plain radiographs of the cervical spine were normal. Magnetic resonance imaging (MRI) showed extensive abnormally high signal within the cord on the T2-weighted scans from C2 to T1 level (Figure 1). These findings were compatible with cord oedema due to cord ischaemia/infarct.
He was treated with thromboprophylaxis and antibiotics. Methadone treatment was continued. His neurological deficit recovered rapidly over the next few days except for the weakness of his hands. He was commenced on a programme of rehabilitation and was discharged after 4 months.
He continued to improve and had an ASIA motor score of 72 at discharge. At 4 years after the injury he had residual weakness in the hands and also mild weakness of the left lower limb (ASIA motor score of 84). He also had some bowel, bladder and sexual dysfunction. He had patchy sensory disturbance over the chest and also blunting of sensation of the right lower limb.
Follow-up MRI scans showed cord atrophy and myelomalacic changes within the anterior horns of the spinal cord from the C5/6 level to the C7/T1 level (Figure 2).
Discussion
Penetrating injuries of the spinal cord may be caused either by gun shot wounds2, 3 (more commonly seen in the countries where gun violence is high) or by stab injuries3, 4 (seen in places where sharp weapons are used in violent crimes).
Pathology of the lesion4, 5
The spinal cord is usually well protected in the spinal canal by the bony vertebral column. The usual portal of injury due to a sharp instrument in the cervical, thoracic and lumbar regions is between the lamina or through the intervertebral foramen. In penetrating injuries due to gun shot wounds, the spinal cord injury can also occur from direct damage from the front.
The cord damage is usually due to a combination of insults:
-
direct injury to the cord by the weapon,
-
in driven bony fragments damaging the cord,
-
vascular injury to the cord,
Vascular anatomy of the cord6
The anterior spinal artery (ASA) supplies the anterior two-thirds of the cord and the central grey matter core via the radiculo-medullary arteries. The ASA may be thought of as an anterior spinal axis that is fed by the vertebral arteries, deep and ascending cervical arteries and by the thoracic (intercostal) and lumbar segmental arteries (Figure 3a). The rest of the cord is supplied by the radiculo-pial arteries via the pial network (the posterior spinal arteries correspond to the dominant flow within the pial network and not to any embryonic vessel like the ventral axis). The radiculo-pial arteries may anastomose with the anterior spinal axis via the vasa corona (Figure 3b). Sulcal penetrating arteries from the ASA are essentially end arteries and the few feeding vessels to the ASA make this system quite vulnerable and may explain the typical anterior location or predominant anterior grey matter involvement of spinal cord infarcts. The pial network has extensive anastomoses, which explain the rarity of posterior infarcts.
We believe that the mechanism of injury was possibly due to direct injection of the chemicals (street heroin and citric acid) in the vicinity of the ASA or a feeding vessel from the vertebral, ascending cervical or deep cervical arteries and subsequent vasospasm of the ASA resulted in cord ischaemia and infarction. This may explain the sudden onset of pain and tingling of all four limbs and also subsequent paralysis, which recovered completely except for the residual weakness of the hands (C8–T1). This is also supported by the initial MRI pictures, which showed signs of cord oedema and the follow-up MRI pictures showed myelomalacic changes within the anterior horn cells.
Direct injury to the ASA is unlikely to be due to its location. This is also supported by the absence of haemorrhage into the cord or the subarachnoid space on the early or follow-up MRI scans.
There is a small incidence of iatrogenic injury7, 8, 9 to the spinal cord after anaesthetic procedures7 or after acupuncture.10 These injuries may be either a direct injury during the procedure8 or delayed presentation due to the migration of a broken needle,11 but the possibility of self-inflicted injury to the cord using a size 23 G needle is very difficult, due to the well-protected position of the cord in the spinal canal. We believe that the injury could have been sustained as the patient was emaciated and that the needle would have gone in just lateral to the trachea and through the lateral foramen to enter the spinal canal.
Conclusion
This is an unusual case of a self-inflicted penetrating spinal cord injury in a young patient, which resulted in cord infarction as a result of injecting street heroin into the neck. This may have led to vasospasm of the vessels supplying the cord leading to ischaemia/infarction of the cord from C2–T1 level. To our knowledge this is the first reported case of self-inflicted spinal cord infarction due to a penetrating lesion.
This highlights the possibility of cord injury even when a small 23 G needle is used and hence care is needed when performing procedures near the spine.
References
Fredrick Jr MM et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Heary RF, Vaccaro AR, Mesa JJ, Balderston RA . Thoracolumbar infections in penetrating injuries to the spine. Orthop Clin North Am 1996; 27: 69–81.
Velmahos GC, Degiannis E, Hart K, Souter I, Saadia R . Changing profiles in spinal cord injuries and risk factors influencing recovery after penetrating injuries. J Trauma 1995; 38: 334–337.
Peacock WJ, Shrosbree RD, Key AG . A review of 450 stab-wounds of the spinal cord. S Afr Med J 1977; 51: 961–964.
Stab wounds of the spinal cord. In: Yashon D (ed) Spinal Injury, 2nd edn. Appleton-Century-Crofts: East Norwalk, CT, 1986 pp 307–317 (Chapter 14).
Spinal cord artery and veins. In: Lasjaunias P, Berenstein A (eds). Surgical Neuro-angiography (Vol 3). Springer-Verlag: Berlin, Heidelberg, 1990. pp 41–53.
Furman MB, O'Brien EM, Zgleszewski TM . Incidence of intravascular penetration in transforaminal lumbosacral epidural steroid injections. Spine 2000; 25: 2628–2632.
McLaughlin RE, Miller WR, Miller CW . Quadriparesis after needle aspiration of the cervical spine. Report of a case. J Bone Joint Surg Am 1976; 58: 1167–1168.
Reina MA, DeLeon-Casasola OA, Lopez A, DeAndres J, Martin S, Mora M . An in vitro study of dural lesions produced by 25-gauge Quincke and Whitacre needles evaluated by scanning electron microscopy. Reg Anesth Paw Med 2000; 25: 393–402.
Kondo A, Koyama T, Ishikawa J, Yamasaki T . Injury to the spinal cord produced by acupuncture needle. Surg Neurol 1979; 11: 155–156.
Silvestro C, Cocito L, Pisani R . Delayed effects of a migrated foreign body (sewing needle) in the cervical spine: a case report. Spine 2001; 26: 578–579.
Acknowledgements
We extend our thanks to Dr J Bhattacharya for the illustrations.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Joseph, G., Santosh, C., Marimuthu, R. et al. Spinal cord infarction due to a self-inflicted needle stick injury. Spinal Cord 42, 655–658 (2004). https://doi.org/10.1038/sj.sc.3101619
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101619
Keywords
This article is cited by
-
Acute myelopathy in association with heroin addiction
Spinal Cord (2006)