Abstract
Study design:
Case report.
Objective:
To examine the unusual and unknown, severe side effect of a therapeutic dose of oral Baclofen on cardiac function.
Setting:
Spinal Cord Unit, Rehabilitation Centre Amsterdam, Amsterdam, The Netherlands.
Methods:
Review of relevant literature.
Results:
A 53-year-old patient with an incomplete C2 tetrapareses (ASIA B) developed severe and painful muscle spasms together with respiratory failure and autonomic dysreflexia. Spasmolytic treatment was started. After the first admission of 5 mg of oral Baclofen, he collapsed in bed with extreme bradycardia, hypotension, hyperventilation and decreased oxygen saturation. A second dosage of 5 mg Baclofen resulted in the same complications. After implantation of a pacemaker, restarting oral Baclofen induced a pacemaker rhythm with episode of hypotension and respiratory failure and also a delirium. Intrathecal Baclofen also resulted in a pacemaker rhythm with hypotension and a decreased cardiac output. To our knowledge, this is the first time a severe heart conduction problem was induced in a spinal cord injury patient after a single therapeutic dose of Baclofen.
Conclusion:
In this case therapeutic oral Baclofen has caused serious cardiac conduction problems.
Similar content being viewed by others
Introduction
Baclofen is commonly used to reduce spasticity and is associated with increased quality of life of spinal cord patients.1 The therapeutic mechanism is by binding to the presynaptic γ-aminobutyric acid type b (GABA-b) receptor of the inhibitory interneuron at the level of the spinal cord and other parts of the central nervous system, resulting in a decrease of muscle tone.
Therapeutic doses of oral Baclofen are low and generally well tolerated but lack sufficient effect in cases of severe spasticity. Intrathecal admission makes it possibility to increase the therapeutic doses effectively and overcome side effects. Overdose or intoxication can result in coma, respiratory failure, seizures, autonomic disturbances and cardiovascular problems which can be fatal.2
We present a case of a tetraplegic, spinal cord injury patient who developed heart conduction problems after the admission of therapeutic dosage of oral and intrathecal Baclofen.
Case report
A 53-year-old man with a traumatic, spinal cord injury was admitted to our rehabilitation clinic in January 2006 with an incomplete C2 tetrapareses (ASIA-B). He was able to breathe without support and was unable to control urine and stools. His medical history showed alcohol, nicotine and cocaine abuse but no previous cardiological problems. He had a normal renal function. After a short spinal shock period, severe and painful muscle spasms developed on all extremities and the thoracic muscles, with episodes of respiratory failure and autonomic dysreflexia (hypertension, flushing and tachycardia/bradycardia). No syrinx or compression of the myelum/radices was seen on magnetic resonance imaging. Events were treated as autonomic dysreflexia by positioning the patient in an upright position.
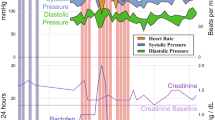
Because of the muscle spasms, oral Baclofen was started and, within minutes after the first admission of 5 mg, he collapsed in bed with extreme bradycardia (heart rate <15 per min), hypotension, hyperventilation and decreased oxygen saturation. After resuscitation, cardiologic analysis showed signs of decompensatio cordis. Ultrasonography showed a hypertrophic left ventricle. Oxygen therapy and diuretics were given. On ICU, a second dosage of 5 mg of Baclofen was given and again extreme bradycardia (with asystolic episodes), hypotension and hyperventilation within minutes appeared.
Because of persisting spasticity with respiratory failure, treatment was still mandatory.
A pacemaker (type DDR-R) was implanted. Oral Baclofen was restarted and increased until 30 mg a day. After 2 weeks of sinus rhythm, a pacemaker rhythm appeared on ECG's together with episode of hypotension and respiratory failure. He also developed a delirium with paranoid-obsessive behaviour and hallucinations. When Baclofen was changed into intrathecal admission up to 0.2 ml h−1, 10 mg ml−1, the delirium disappeared and a sinus rhythm was found again. After 7 days, a pacemaker rhythm reappeared with episodes of hypotension and decreased cardiac output. Intrathecal Baclofen was stopped and oral benzodiazepine was started which resulted in decreased muscle spasms but also in respiratory failure for which chronic respiratory support was necessary.
Discussion
Cardiovascular complications are known in spinal cord injury patients and can be caused by different pathology. During the acute phase, the spinal cord injury itself can comprise the cardioaccelerator sympathetic reflex mechanism causing brady-arrhythmias including bradycardia and atrioventricular (AV) block.2 Orthostatic hypotension can occur in spinal cord patients in the upright position by pooling of blood in the lower extremities, reduction of cardiac output and inadequate compensatory, autonomic mechanism.2 After a short spinal shock period events occurred in our patient in a horizontal position and were first treated by verticalization.
Autonomic dysreflexia can trigger bradycardia, left ventricular failure, cardiomegaly, tachycardia, myocardial ischaemia and arrhythmia.2 Electrocardiographic findings include: AV dissociation, prolonged PR interval, second-degree AV-block with nodal escape beats, premature atrial and ventricular contractions and acute fibrillation.2 Our patients showed extreme bradycardia and asystolic episodes without signs of autonomic dysreflexia immediately after the first doses of Baclofen.
Substance abuse is associated with cardiovascular complications, including myocardial infarction, left ventricular hypertrophy, arrhythmias and cardiomyopathy. Cardiomyopathy in our patient can be caused by his smoking, cocaine or alcohol abuse. His medical history did not show any previous cardiac complications.
Cardiovascular side effects of Baclofen are most pronounced during anaesthetics or after overdose.3, 4, 5 Haemodynamic changes and conduction abnormalities including bradycardia, prolonged QTc, first-degree heart block, premature atrial contractions and supraventricular tachycardia have been published.3 Our patient did not use any other medication (or interaction of medication) that could have caused conduction problems.Conduction problems including bradycardia have been described after therapeutic dosage in patients with renal failure or in patients after longtime treatment.4, 5 As far as we know this is the first time a spinal cord injury patient showed a severe heart conduction problem after a therapeutic dosage of Baclofen.
References
Zahavi A, Geertzen JH, Middel B, Staal M, Rietman JS . Long term effect (more than five years) of intrathecal baclofen on impairment, disability, and quality of life in patients with severe spasticity of spinal origin. J Neurol Neurosurg Psychiatr 2004; 75: 1553–1557.
Bravo G, Guízar-Sahagún G, Ibarra A, Centurion D, Villalón CM . Cardiovascular alterations after spinal cord injury: an overview. Curr Med Chem 2004; 2: 133–148.
Leung NY, Whyte IM, Ibister GK . Baclofen overdose; defining the spectrum of toxicity. Em Med Austr 2006; 18: 77–82.
Lyew MA, Mondy C, Eagle S, Chernich SE . Hemodynamic instability and delayed emergence from general anaesthesia associated with inadvertent intrathecal baclofen overdose. Anesthesiology 2003; 98: 265–268.
Lee TH, Chen SS, Su SL, Yang SS . Baclofen intoxication: report of four cases and review of the literature. Clin Neuropharm 1992; 15: 56–62.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Smit, C., Slim, E. Heart conduction problems in a tetraplegic patient caused by a single therapeutic dosage of Baclofen. Spinal Cord 46, 317–318 (2008). https://doi.org/10.1038/sj.sc.3102123
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102123