Abstract
A pattern of aberrations in the T-cell cytokine system that is typical for autoimmune disorders has also been reported in patients with schizophrenia, namely a decreased interleukin-2 (IL-2) production and increased levels of the soluble IL-2 receptor (sIL-2R). It has also been reported that the production of interferon-γ (IFN-γ) may be lowered. In a longitudinal design, we studied the production of both IFN-γ and IL-2 and their correlation in patients with schizophrenia during treatment and investigated whether associations exist between cytokine production and clinical variables. The production of IFN-γ and IL-2 was measured in equal numbers (n = 29) of patients with schizophrenia (DSM-IV) and controls who were matched for age and gender. Patients were measured 1 day after admission (T1), after 14 (T2) and 28 (T2) days of treatment. Psychopathology was assessed after these times. The production of both IFN-γ and IL-2 was significantly lower in patients than in controls throughout the whole investigation period (T1–T3). The productions of both cytokines were significantly correlated in controls (r = 0.60, P ≤ 0.001) as well as in patients with schizophrenia (mean production T1–T3: r = 0.71, P ≤ 0.001). No associations between cytokine measurements and psychopathology or age-at-onset could be found. Our findings of lowered and correlated IFN-γ and IL-2 production indicate that alterations in the cytokine system of patients with schizophrenia might resemble those in autoimmune disorders. It is suggested that these immunological abnormalities are associated with acute exacerbation, rather than with a clinical subtype of schizophrenia.
Similar content being viewed by others
Introduction
As early as 1937, the neuropsychiatrist Lehmann-Facius1 pointed to the possible role of autoimmunity in the pathophysiology of schizophrenia. Even today this assumption is still supported by certain clinical features that can be observed in both schizophrenia and autoimmune diseases, such as type-1 diabetes, lupus erythematosus or multiple sclerosis. Both groups of disorders often have juvenile onset and can be triggered by psychosocial distress, infections, drug abuse and physical injury.2 A considerable variability of course, often with acute disease episodes and subsequent reduced level of functioning is also observed in both groups of diseases.
Over the last decade, knowledge concerning the pathophysiology of autoimmune disorders has significantly increased as a result of research on the role of cytokines in these diseases. There is to date considerable evidence that an altered regulation of a number of cytokines exist not only at inflammatory sites, but also in the peripheral blood, especially with systemic autoimmune disorders. An in vivo activation of T cells in these disorders is typically reflected by increased serum levels of their products, namely interleukin-2 (IL-2) and the soluble interleukin-2 receptor (sIL-2R). Paradoxically, a decreased in vitro production of IL-2 upon mitogen stimulation is found in these patients. These common features of autoimmune disorders2, 3 have lately been supplemented by the demonstrations of a decreased in vitro production of interferon-gamma (IFN-γ) upon mitogenic stimulation.4 IFN-γ is a 143-amino acid residue glycoprotein with multiple biological functions including potent anti-viral activity, stimulation of macrophage activity, modulation of Major Histocompatibilty Complex (MHC) class I/class II expression and regulation of a diversity of specific immune responses. It is produced predominantly by CD4+ (TH-1) cells and particularly by CD4+CD45R0+ memory-cell.5 With respect to their immunological functions, both TH1-cytokines IL-2 and IFN-γ are related and the release of IL-2 is stimulated by IFN-γ. Both cytokines have largely immune-stimulatory effects which apparently exacerbate the inflammatory process in autoimmune disorders.
Aberrant proportions of immune-competent cells, indicating immunological dysfunctions, have often been reported in schizophrenia since the early work of Bruce and Peebles,6 although there are conflicting results concerning the precise nature of these changes.7 The search for tissue-specific antibodies which can serve as markers for schizophrenia has as yet not been successful.7 However, recent studies which have focused on the physiology of cytokine production have provided increasingly consistent results. Six different groups, including our own, have independently demonstrated that mitogen stimulated IL-2 production by peripheral blood mononuclear cells (PBMC) is decreased in patients with schizophrenia.8, 9, 10, 11, 12, 13, 14, 15 This is the most frequently confirmed finding in the immunology of schizophrenia and there has not as yet been a failure in demonstrating this phenomenon. In the cerebrospinal fluid (CSF) of drug-free patients, increased levels of IL-2 were found16 and also significantly predicted the recurrence of psychotic symptoms in relapse-prone schizophrenics.17 Elevated levels of the sIL-2R in peripheral blood, a sign that also indicates lymphocyte activation, were also repeatedly observed in schizophrenia.14, 18, 19 Hence concerning cytokines and their role as indicators for T-cell activation, there are impressive parallels between autoimmune disorders and schizophrenia.
The few existing reports on IFN-γ production in schizophrenia, however, paint a rather incomplete picture. Whilst there is some evidence that the mean serum levels of IFN-γ in schizophrenics (except in one report)20 resemble those of normal controls,21, 22, 23 the production of IFN-γ after mitogenic stimulation was only mildly and on the whole not significantly decreased in schizophrenia,14, 24, 25, 26 although one study did find a significant decrease.27 The lack of coherence in these results can be explained by the fact that studies varied considerably with respect to the use of bioassays, cell preparation techniques, and also recruitment of patients. Although in some studies cells were separated from the sera and subsequently stimulated by mitogens, our group used a whole blood assay28 whereby the lymphocytes were incultured with as little deviation as possible from their physiological milieu, ie cell populations were present in their natural frequency and distribution. It is therefore likely that in vitro stimulation effects better reflect actual in vivo cytokine production by immunocompetent cells. Using the same methods as were used in our pilot study,14 we have demonstrated a significantly reduced production of IFN-γ in an acutely ill subsample of a larger group of patients with schizophrenia.15 Recently this finding could be confirmed in samples of hospitalized acutely psychotic schizophrenics29 and in acutely schizophrenic members of multiplex families.30 However, as in the majority of studies in this area, only a cross-sectional approach was employed, which did not yield any information about changes in cytokine production while patients were undergoing remission.31
Encouraged by our preliminary findings, patients undergoing treatment due to worsening of schizophrenic symptoms were investigated in this study and the production of IFN-γ and IL-2 by lymphocytes of patients and healthy age- and gender-matched controls were examined. It was our intention to investigate in a larger patient sample whether IFN-γ as well as IL-2 is reduced in acute schizophrenia. We chose a prospective longitudinal approach with three time-points for investigation, timed at 14-day intervals from one another. Thus a 1-month period of observation was covered between the times of acute illness and clinical remission, so as to investigate whether changes in interferon production occurred which correlated with reduction of psychotic symptomatology.
Methods
Recruitment
Patients
Twenty-nine patients with schizophrenia were recruited from the Department of Psychiatry of the University of Luebeck School of Medicine. The Department of Psychiatry (DP) provides most of the psychiatric inpatient services for the 220 000 inhabitants of the city of Luebeck, a north German town near the Baltic Sea. The DP is the community mental health center for the whole city of Luebeck and the surrounding rural areas and its patient population is therefore representative for the whole region. Patients were included in the study after it was described to them orally and by a study guide, according to the University of Luebeck Ethics Committee regulations. The patients underwent a structured clinical interview. DSM-IV diagnoses were made by consensus at a staff conference of four psychiatric researchers (VA, DE, MR, CW) who reviewed the results of the interview, along with all available information, including clinical records and information from relatives. The initial diagnostic assessment at day 1 (T1) was reviewed at every point of investigation, ie after 14 days (T2) and 28 days (T3). Only subjects who met DSM-IV criteria throughout the whole assessment period were retained in the sample. Patients with any form of psychiatric comorbidity, including substance abuse, were excluded. All patients were monitored for somatic illness throughout the investigation period and were excluded if symptoms of infections or symptoms of systemic somatic illness were present. Furthermore, the level of C-reactive protein (CRP) was controlled to validate clinical symptoms of infections, and all patients with a CRP ≥ 0.5 ml dl−1 were excluded from the study. Only physically healthy patients were included. The patients had not been treated with immunosuppressive drugs or steroids during the 3 months which preceded blood sampling. By these criteria, originally 52 patients were recruited. Since only 29 of these completed 4 weeks of treatment (T1–T3), only these patients were included in the study. Seventeen of the patients were male and 12 were female. The mean age was 34.0 (SD ± 12.7) years of age, ranging from 17 to 62. The mean duration of illness was 101.3 (SD ± 102.3) months. Prior to admission, 19 patients were treated with typical, eight with atypical neuroloeptic drugs, two were non-medicated. During their hospital stay, 25 patients were treated with standard neuroleptic drugs, and four were treated with clozapine. The following chlorpromazine equivalents were obtained: T1: 495.6 (±375.1) mg; T2: 508.9 (±330.5) mg; T3: 482.6 (±269.0) mg.
Controls
Healthy non-psychiatric controls were recruited from the Blood Transfusion Service of the Department of Immunology and Transfusion Medicine at the University of Luebeck. These individuals were chosen after analysis of full medical history and examination, especially for psychiatric disorders, and additional blood testing by a qualified physician at the department. The blood was analyzed to ensure that the healthy donors had not been taking any medical or illegal substances. Each schizophrenic patient was matched with one control with regard to gender and age. The mean age of controls was 34.1 (SD ± 12.7) years of age, ranging from 19 to 60 years.
Clinical assessments
At the beginning and during psychiatric inpatient treatment (T1, T2, T3), the psychopathology of the patients with schizophrenia was measured by the Brief Psychiatric Rating Scale (BPRS).32 Measurement by the Positive and Negative Syndrome Scale (PANSS)33 was also taken at T1. Age of schizophrenia onset was defined as the age at which symptoms first appeared, as reported by the patient, the family or medical staff.
Immunological methods
Heparinized blood was drawn by venous puncture from patients and controls always at 8.00 am, in order to avoid diurnal variation effects. Although we did not record possible sleep disturbance patterns in patients with schizophrenia and controls, the clinically treated patients generally slept undisturbed after 7–10 days of treatment, due to sleep medication. After the blood was drawn, it was stored at 4°C and cultured in a whole-blood assay within 1–2 h according to a technique previously described.26 In a 5-ml polystyrene tube (Greiner, Nuertingen, Germany), 100 μl of blood was added to 850 μl of Roswell Park Memorial Institute 1640 medium (Biochrom, Berlin, Germany) supplemented at a ratio of 1:10 with 2 mmol L-glutamine, 100 U of penicillin per ml, and 100 μg of streptomycin per ml (Gibco, Karlsruhe, Germany). For the induction of cytokines, phytohaemagglutinine (PHA, Burroughs Wellcome, Dartford, UK) was added at a concentration of 1.78 mitogenic units (0.1 mg ml−1). Tubes were covered and incubated in a humidified atmosphere of 95% air/5% CO2 at 37°C for 48 h (IL-2), or 96 h (IFN-γ) respectively. The supernatants were recovered and kept frozen at −80°C. Cytokine concentrations were determined by ELISA techniques, whereby recombinant cytokines were used as standards. We used ELISA kits supplied by BioSource International, Camarillo, USA (IL-2, IFN-γ) for the determination of cytokines, carried out according to the manufacturer's instructions.
Statistical analysis
As descriptive measures of cytokine production, the means (±SD percentile) are given, since the majority of the variables were normally distributed in patients (Kolmogorov–Smirnov test: IL-2/T1: Z = 1.03, P = 0.23; II-2/T2: Z = 1.22, P = 0.10; IL-2/T3: Z = 0.91, P = 0.39; IFN-γ/T1: Z = 1.31, P = 0.07; IFN-γ/T2: Z = 1.51, P = 0.02; IFN-γ/T3: Z = 0.67, P = 0.77) and in controls (IL-2: Z = 0.92, P = 0.37; IFN-γ: Z = 0.98, P = 0.29). Hence, intercorrelations between variables were examined by the use of Pearson's product-moment-correlation coefficient r. In order to correlate cytokine production variables with chlorpromazine equivalents, Spearman's Rank test was used (coefficient rho, ρ). The differences in cytokine production between the schizophrenic and healthy control samples at three time-points of investigation (T1–T3) were examined by Friedman two-way ANOVAs. Differences in mean cytokine production at the different time-points of investigation were tested by the t-tests for matched pairs and for independent samples. When the production of IFN-γ at T2, which was not normally distributed, was compared with the values of controls, the Wilcoxon test was used.
Results
Psychopathology
At admission (T1 = day of admission), the mean PANSS total score was 117.0 ± 28.0, the PANNS negative score was 32.4 ± 7.5 and the positive score 28.0 ± 9.3. The mean BPRS score at T1 was 69.4 ± 15.8. During 28 days of inpatient treatment (T2 = 14th day after admission, T3 = 28th day after admission), the mean BPRS total score improved significantly from T1 to T2 (60.4 ± 18.3) and T3 (53.9 ± 18.0; Friedman two-way ANOVA: χ2 = 32.2, df = 2, P ≤ 0.001) corresponding to a mean reduction of 22.3% in psychopathological signs.
Immunological findings
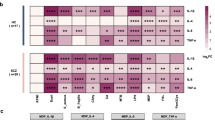
The mean (±SD) in vitro production of IFN-γ after mitogenic stimulation was measured in patients with schizophrenia at T1 (2627 ± 3220 pg ml−1), at T2 (4096 ± 5236 pg ml−1) and at T3 (3217±2139 pg ml−1) and compared to their age- and sex-matched controls (5718 ± 5265 pg ml−1; Friedman two-way ANOVA: χ2 = 19.4, df = 3, P = 0.0002. When the IFN-γ productions in the schizophrenic sample at the different time-points were tested, they were not found to be significantly different from one another (Friedman two-way ANOVA: χ2 = 3.6, df = 2, P = 0.17). The IFN-γ productions of the patients with schizophrenia were tested post hoc against the controls at the single time points and were significantly lowered at T1 (t-test for matched pairs: t = 2.97, P = 0.006), T2 (Wilcoxon-test, Z = −2.28, P = 0.02) and T3 (t = 2.70, P = 0.012) (Figure 1).
Production of interferon-γ of patients with schizophrenia at three treatment points (T1, admission; T2, after 14 days; T3, after 28 days) and healthy controls. Differences of the IFN-γ production (mean) of controls and schizophrenics were tested (significance is marked by *) at T1 (t = 2.97, P ≤ 0.006), T2 (Z = −2.3, P = 0.023) and T3 (t = 2.7, P = 0.012).
Concerning IL-2, the mean (±SD) production in the patients with schizophrenia at T1 (90 ± 78 pg ml−1), at T2 (166 ± 156 pg ml−1) and at T3 (121 ± 86 pg ml−1) was compared with their age- and sex-matched controls (269 ± 222 pg ml−1, Friedman two-way ANOVA: χ2 = 21.2, df = 3, P = 0.0001). When the means of the IL-2 productions by patients with schizophrenia were tested against one another, the result was also significant (Friedman two-way ANOVA: χ2 = 8.3, df = 2, P = 0.02). However, when the results at each of the time-points were tested post hoc against the controls, they were significantly lower at T1 (t-test for matched pairs: t = −4.50, P ≤ 0.001) and at T3 (t = −3.9, P = 0.001), but not at T2 (t = −1.93, P = 0.06) (Figure 2).
Production of interleukin-2 of patients with schizophrenia at three treatment points (T1, admission; T2, after 14 days; T3, after 28 days) and healthy controls. Differences of the IL-2 production (mean) of controls and schizophrenics were tested (significance is marked by *) at T1 (t = −4.50, P ≤ 0.001), T2 (t = −1.93, P = 0.06) and T3 (t = −3.9, P = 0.001).
Significant intercorrelations between the production of IFN-γ and IL-2 were detected, not only with the control subjects (r = 0.60, P = 0.001) but also in the schizophrenic sample, at all three time-points (Table 1). The productions of both cytokines at T2 were also significantly correlated with the productions at T3 (Table 1). This also held true when these results were controlled for the effects of multiple testing using the Bonferroni correction, albeit with a reduced significance level of P ≤ 0.003. When each of the productions of IFN-γ and IL-2 were added up over the three time-points for every patient and then correlated, the result was highly significant (r = 0.71, P ≤ 0.001). The distribution of the sums of the cytokine productions are demonstrated in Figure 3.
The productions of cytokines were correlated with the respective chlorpromazine dosage equivalent to the neuroleptic intake of the patients and three points of treatment. The results were all non-significant: (T1) IFN-γ: ρ = 0.24, P = 0.40; IL-2: ρ = −0.06, P = 0.83; (T2) IFN-γ: ρ = −0.16, P = 0.56; IL-2: ρ = −0.21, P = 0.44; (T3) IFN-γ: ρ = 0.24, P = 0.38; IL-2: ρ = 0.11, P = 0.68.
Regarding the clinical features of the patients with schizophrenia, neither IFN-γ nor IL-2 production at admission were found to be correlated significantly with age, onset of illness, duration of illness, the BPRS total score, the PANSS positive score, and the PANSS negative score (Table 2). Furthermore, no significant correlations between both of the cytokine productions and these clinical variables could be found (Table 2).
Discussion
To our knowledge, this is the first study to date on cytokine production in schizophrenia in which a longitudinal design was employed, not only with respect to the production of IL-2, but particularly in the case of IFN-γ. Our results confirm the association between acute schizophrenia and low IL-2 production,8, 9, 10, 11, 12, 13, 14, 15 but also clearly confirm our earlier results30 which showed a decreased IFN-γ production in acute schizophrenia. Deficient lymphocyte productions of both IL-2 and IFN-γ were also found throughout the time period of clinical remission, which were also significantly intercorrelated with one another at all three time-points of the investigation.
A decreased in vitro production of IL-2, together with an increased serum level of the shedded sIL-2R is a common characteristic of some autoimmune diseases. As an example, lowered IL-2 production was demonstrated for insulin-dependent (type I) diabetes mellitus,34, 35 which was not altered by insulin treatment.35 This was also present only in affected children from monozygotic twin pairs who were discordant for the disease.36 In rheumatoid arthritis, a lowered IL-2 production can be seen,37 especially in the active disease when the joints become eroded.38 Increased levels of sIL-2R have also repeatedly been reported39 which were correlated with the rheumatic disease activity. Similar findings have been reported for systemic lupus erythematosus40, 41, 42, 43 and even for Grave's disease.44, 45 In multiple sclerosis, cytokines have also become a subject of intense interest,46 whereby a decreased production of IL-2,47, 48 elevated serum levels of IL-249 and increased PBMC expression of high-affinity IL-2 receptors are all present which correlate with disease activity.50
Since the biological functions of IL-2 and IFN-γ are physiologically interconnected, it might be expected that there would also be an aberrant regulation of IFN-γ production in autoimmune disorders. Although fewer reports exist concerning this cytokine, a reduced in vitro production was found in type I diabetes,51 even though IFN-γ seems to play an essential role in pancreatic β-cell destruction of52 and diminishes β-cell responsiveness to glucose.53 Also in rheumatoid arthritis, the in vitro production of IFN-γ is lowered,4, 54 although increased IFN-γ levels play a significant role at the inflammatory sites of the disease.55, 56 In multiple sclerosis, IFN-γ seems to promote the disease process.57 An elevated production was found which preceded the manifestation of clinical symptoms,58 although this was not seen in acute episodes or remissions.48
Despite the fact that the complex pathophysiological functions of TH1-cytokines in autoimmune disorders are not yet fully understood and that the above mentioned inconsistencies of data remain to be clarified, mounting evidence suggests a major role for these (and other) cytokines, not only as indicators of T cell activity but also as direct inflammatory agents. Considering the current knowledge about cytokine production in PBMCs and autoimmune disorders, some striking similarities exist between these diseases and schizophrenia. The data suggesting a decreased production of IFN-γ during acute schizophrenia directly support the idea that autoimmune activity plays an important role in pathogenesis.2 The fact that this feature was observed only in the acutely ill, but not in the residual patients15, 30 is also worthy of note. Furthermore, as with type-I diabetes, where low IL-2 production is obviously acquired, and not inherited,36 we found decreased IFN-γ production in the acutely schizophrenic, but not in unaffected first degree relatives within families showing multiple occurrence of schizophrenia.30 This finding also suggests that the deficit is associated with the active disease, rather than with a genetic predisposition.
Whilst our state of knowledge on the pathophysiological effects of cytokines in autoimmune disorders is rapidly increasing, the involvement of aberrant immune functions in the pathogenesis of schizophrenia is poorly understood. Experimental and clinical studies have provided some evidence that cytokines play an important role in the development of central nervous system (CNS) tissue.59 IFN-γ activates embryonic microglia, which results in the activation of a soluble molecule that promotes the differentiation of cholinergic neuronal cell precursors in both the septal nuclei and adjacent basal forebrain and stimulates the development of cholinergic embryonic septal neurons.60 These findings highlight the role of IFN-γ in the development of neurotransmitter systems. IL-2 modulates neuronal activity; IL-2 and its receptors have a widespread localization in gray matter areas of the CNS.61 It is of considerable interest to schizophrenia research that IL-2 modulates dopamine release in the striatum by influencing the function of excitatory amino acids.62, 63 On the other hand, the number of studies is increasing that demonstrate lesions of hypothalamic structures lead to substantial disruptions of the immune system integrity.64 However, considering that limited observations on the complex interactions of CNS tissue, neurotransmitters and cytokines are presently possible, caution must be exercised in interpreting psycho-immunological data, particularly since, despite considerable research, the mechanisms underlying the aberrant immune functions of PBMC from schizophrenics are as yet not understood at the cellular level.
Four hypotheses have been put forward as explanation for the cellular mechanisms underlying reduced TH-cytokine production in schizophrenia: (1) the lowered cytokine production is a trait phenomenon, resulting from a genetic predisposition; (2) cytokine production is ‘down-regulated’ by negative feedback after initial overproduction; (3) the cells are producing cytokines in excess in vivo, so that when they are isolated they have apparently become ‘exhausted’ and produce less in vitro; (4) cytokines produced in vitro are rapidly ‘consumed’ by receptors which are also overtly expressed after stimulation. This process might thereby bring about a false indication of a decreased cytokine production. Most of the empirical data from recent studies support the last two hypotheses. However, it would exceed the scope of this article to discuss these underlying mechanisms in closer detail. In future studies, with respect to evaluation of the last hypotheses, the IL-2 production should be analyzed more comprehensively through use of anti-CD25 monoclonal antibodies.65 It should also be noted that studies of the messenger-RNAs for IL-2 and IFN-γ are currently under way in order to gain information at the intracellular level.
Few studies have been performed whereby the association between psychopathological symptoms of schizophrenia and cytokine production has been investigated. Cross-sectional studies have shown that negative symptoms of schizophrenia were significantly negatively correlated with both increased soluble IL-2-receptor concentration66 and lowered IL-2 production in non-medicated schizophrenics.67 In the latter study, a highly significant positive correlation was found between age-of-onset and IL-2 production. This is particularly important, since it suggests an association between lowered IL-2 production and the structural brain abnormalities which are supposed to be associated with these clinical features. However, earlier cross-sectional studies by our group14, 15 failed to show such correlations. Also in the present study, no correlations between negative or positive symptoms and production of IL-2 or IFN-γ could be observed at T1. There were also no correlations between the BPRS total score, or its subscores, and cytokine production at T1, T2, or T3.
The factors suspected of having a major confounding influence on the lowered cytokine production in schizophrenia include: (a) number of producer-cells; (b) production of counter-regulatory cytokines, especially IL-4 and IL-10; (c) medication; (d) non-specific stress; and (e) diurnal variation of cytokine production.
(a) In no study cited until now14, 15, 29 could significant differences in the relevant lymphocyte populations be detected. The CD4CD45RO+ memory-cells were studied in particular by our group, since they are supposed to be the main producers of IFN-γ,5 however without detecting differences between patients with schizophrenia and controls.15 No differences were found in an extensive analysis of cell counts for leukocytes, lymphocytes, pan T cells, activated T cells and absolute numbers of B cells; however, a slight elevation of CD3/CD25+ cells carrying the IL-2 receptor and absolute/relative monocyte counts could be detected.68
(b) In earlier studies we reported that there was also no evidence for an influence of IL-415 or IL-1029 on cytokine production. The production of IL-10 was in fact lowered in schizophrenia,29 a finding which even suggests a malfunction in the physiological antagonism between the TH-1 and the TH-2 systems. On the other hand, Cazullo et al26 found an increased IL-10 production in patients with paranoid schizophrenia. It seems possible that this difference is due to the fact that different laboratory techniques were used in this study, eg lymphocytes were separated and washed. This may also be of relevance for their non-detection of lowered IFN-γ and IL-2 production.
(c) The possible influence of antipsychotic medication has regularly been debated. In this study, no significant correlations between neuroleptic dosages and cytokines could be obtained. In one early study, Moises et al27 did not find an in vitro effect of haloperidol, on either the proliferation of lymphocytes or on IFN-γ production. In two clinical studies lymphocyte subpopulations were not influenced by neuroleptic treatment.69, 70 Never-medicated first-episode patients with schizophrenia showed similar abnormalities in IL-2 production65 as were found in medicated patients, and both IL-2 production and supernatant levels of sIL-2R remained unaffected by subsequent neuroleptic treatment.10, 13, 71 It has preliminarily been reported that patients receiving haloperidol or risperidone produce less IL-2 than those receiving clozapine.26 Interestingly, an in vitro study72 has shown that both haloperidol and clozapine reduce lymphocyte proliferation and production of IL-2 and IFN-γ in a dose-dependent manner. Although the suppression effect was visible only above a threshold concentration of 1 μM, which is hardly reached in clinical treatment, there might still be an effect of long-term application on the immune system. An in vivo immune-suppressive effect of clozapine was recently confirmed by another study,73 whereas these authors reported an immune stimulation in vitro, in disagreement with the results of Leykin et al.72 In another study,74 elevated levels of sIL-2R were observed only in patients with schizophrenia who were treated with the atypical neuroleptic compound clozapine. These findings, however, did not stand uncontradicted.75 By employing a ‘criss-cross’ technique, we found no significant influence of the sera of medicated schizophrenic subjects on IL-2- or IFN-γ production by lymphocytes from normal individuals.68 Hence the notion of a major in vivo influence by neuroleptic medication is not strongly supported by current findings, but can also not be completely ruled out.
(d) Until now, no evidence has been acquired which suggests an influential role for non-specific influence of stress on cytokine production in schizophrenia. Ganguli et al were unable to find correlations between anxiety and tension BPRS scores and cytokine production. Ambiguous results were reported concerning distress-related cortisol levels in schizophrenia. Whilst there are reports of increased levels associated with decreased IL-2 production,2 other groups were unable to detect increased cortisol levels.15, 76 In the present study no correlations between cortisol levels and production of IL-2 or IFN-γ could be detected (data not shown).
(e) The possible influence of sleep disturbance on cytokine production has hardly been regarded in studies of schizophrenia and TH-2 cytokines. However this might be an important point since it is known that in healthy persons serum levels of IL-1β and IL-6 temporally increase during sleep.77 The productions of TNF-α and IL-1β upon mitogen stimulation are diminished, and the production of IL-2 is enhanced during sleep.78 Sleep deprivation seems to affect catecholamine and IL-1 levels, the levels of IL-2 remained unchanged.79 For patients with schizophrenia, it was reported that reduced sleep is associated with increased serum levels of IL-1.80 Although there is no direct evidence for the lowered production of IL-2 and IFN-γ to be associated with sleep disturbances in patients with schizophrenia, such an effect could not be ruled out in this study. Future work in this field should regard the possible effects of sleep disturbances and diurnal variation.
In conclusion, in vitro production of IL-2 and IFN-γ is significantly reduced and also intercorrelated in acute schizophrenia. These results support the main body of published evidence. An aberrant production of these TH-1 cytokines is not only found on admission, but is also likely to be seen throughout early stages of remission. Lowered cytokine production might represent a biological state marker for acuteness of schizophrenia, however caution is recommended with respect to the fact that we investigated patients with chronic schizophrenia, a limited follow-up interval, and the possible influence of neuroleptic medication. Since there are ambiguous results with respect to possible associations between cytokine production and clinical features, more research is needed to clarify whether cytokine production abnormalities can act as markers for a certain, also clinically characterized, subtype of the disease. The involvement of immunological abnormalities in the pathophysiology of schizophrenia is still largely unclear and remains to be explored.
References
Lehmann-Facius H . Liquoruntersuchungen bei destruktiven Erkrankungen des Nervensystems, besonders bei Schizophrenien Neurol Psychiatrie 1937; 157: 109–115
Ganguli R, Brar JS, Chengappa KNR, Yang ZW, Nimgaonkar VL, Rabin BS . Autoimmunity in schizophrenia Ann Med 1993; 25: 489–496
Kroemer G, Martinez C . Cytokines and autoimmune disease Clin Immunol Immunopathol 1991; 61: 275–295
Ruschen S, Stellberg W, Warnatz H . Kinetics of cytokine secretion by mononuclear cells of the blood from rheumatoid patients are different from those of healthy controls Clin Exp Immunol 1992; 89: 32–37
Sanders ME, Makoba MW, Sharrow SO, Stephany D, Springer TA, Young HA et al. Human memory T-lymphocytes express increased levels of three cell adhesion molecules (LFA-3, CD2 and LFA-1) and three other molecules (UCHL-1, Cdw29 and Pgp-1) and have enhanced interferon-gamma production J Immunol 1988; 140: 1401–1407
Bruce LC, Peebles AMS . Clinical and experimental observations on catatonia J Ment Sci 1903; 49: 614–628
Kirch DG . Infection and autoimmunity as etiologic factors in schizophrenia: a review and reappraisal Schizophr Bull 1993; 19: 355–370
Villemain F, Chatenoud L, Guillibert E, Pelicier Y, Bach JF . Decreased production of interleukin-2 in schizophrenia Ann NY Acad Sci 1987; 469: 669–675
Kolyaskina GI, Morozov TP, Sekirina TP, Burbayeya GS . Immunological and Virological Studies in Schizophrenia. Presented at the Second World Congress on Viruses, Immunity, and Mental Health, October 6, 1988, Quebec
Villemain F, Chatenoud L, Galinowski A, Homo-Delarche F, Ginestet D, Loo H et al. Aberrant T-cell mediated immunity in untreated schizophrenic patients: deficient interleukin-2 production Am J Psychiatry 1989; 146: 609–616
Ganguli R, Rabin BS, Belle SH . Decreased interleukin-2 production in schizophrenic patients Biol Psychiatry 1989; 26: 427–430
Sirota P, Fishman P, Elizur A, Djaldetty M . Lymphokine production in schizophrenic patients Biol Psychiatry 1990; 27: 173A
Bessler H, Levental Z, Karp L, Modai I, Djaldetti M, Weizman A . Cytokine production in drug-free and neuroleptic-treated schizophrenic patients Biol Psychiatry 1995; 38: 297–302
Hornberg M, Arolt V, Wilke I, Kruse A, Kirchner H . Lymphokine production in leukocyte cultures of patients with schizophrenia Schizophr Res 1995; 15: 237–242
Wilke I, Arolt V, Hornberg M, Kirchner H . Investigations of cytokine production in whole blood cultures of paranoid and residual schizophrenics Eur Arch Psychiatry Clin Neurosci 1996; 246: 279–284
Licinio J, Seibyl JP, Altemus M, Charney DS, Krystal JH . Elevated CSF levels of interleukin-2 in neuroleptic-free schizophrenic patients Am J Psychiatry 1993; 150: 1408–1410
McAllister CG, van Kammen DP, Rehn TJ, Miller AL, Gurklis J, Kelley ME et al. Increases in CSF levels of interleukin-2 in schizophrenia: effects of recurrence of psychosis and medication status Am J Psychiatry 1995; 152: 1291–1297
Ganguli R, Rabin BS . Increased serum interleukin-2 receptor in schizophrenic and brain damaged subjects Arch Gen Psychiatry 1989; 46: 292
Rapaport MH, McAllister CG, Pickar D, Nelson DL, Paul SM . Elevated levels of soluble interleukin-2 receptors in schizophrenia Arch Gen Psychiatry 1989; 46: 291–292
Preble OT, Torrey EF . Serum interferon in patients with psychosis Am J Psychiatry 1985; 142: 1184–1186
Schindler L, Leroux M, Beck J, Moises HW, Kirchner H . Studies of cellular immunity, serum interferon titers, and natural killer cell activity in schizophrenic patients Acta Psychiatr Scand 1986; 73: 651–657
Becker D, Kritschmann E, Floru S, Shlomo-David Y, Gotlieb-Stematsky T . Serum interferon in first psychotic attack Br J Psychiatry 1990; 157: 136–138
Gattaz WF, Dalgalarrondo P, Schröder HC . Abnormalities in serum concentrations of interleukin-2 and interferon-γ in schizophrenia not detected Schizophr Res 1992; 6: 237–241
Ahokas A, Rimon R, Koskemieni M, Vaheri A, Julkunen I, Sarna S . Viral antibodies and interferon in acute psychiatric disorders J Clin Psychiatry 1987; 48: 194–196
Katila H, Cantell K, Hirvonen S, Rimon R . Production of interferon alpha and gamma by lymphocytes from patients with schizophrenia Schizophr Res 1989; 2: 361–365
Cazzullo CL, Scarone S, Grassi B, Vismara C, Trabattoni D, Clerici M et al. Cytokines production in chronic schizophrenia patients with or without paranoid behaviour Prog Neuropsychopharmacol Biol Psychiatry 1998; 22: 947–957
Moises HW, Schindler L, Leroux M, Kirchner H . Decreased production of interferon-gamma in leucocyte cultures of schizophrenic patients Acta Psychiat Scand 1985; 72: 45–50
Kirchner H, Kleinicke C, Diegel W . A whole blood technique for testing production of human interferon by leukocytes Immunol Meth 1982; 48: 213–219
Rothermundt M, Arolt V, Weitzsch C, Eckhoff D, Kirchner H . Production of cytokines in acute schizophrenic psychosis Biol Psychiatry 1996; 40: 1294–1297
Arolt V, Weitzsch C, Wilke I, Nolte A, Pinnow M, Kirchner H . Production of interferon-gamma in families with multiple occurrence of schizophrenia Psychiatry Res 1997; 66: 145–151
Arolt V, Weitzsch C . Rothermundt M, Eckhoff D, Kirchner H. Interferon-gamma in schizophrenia Adv Biol Psychiatry 1997; 18: 57–66
Overall JE, Gorham DR . The Brief Psychiatric Rating Scale Psychol Rep 1962; 10: 799–812
Kay SR, Fishbein A, Oppler LA . The Positive and Negative Syndrom Scale (PANSS) for schizophrenia Schizophr Bull 1987; 13: 261–276
Zier KS, Leo MM, Spielman RS, Baker L . Decreased synthesis of interleukin-2 (IL-2) in insulin-dependent diabetes mellitus Diabetes 1984; 33: 552–555
Roncarolo MG, Zoppo M, Bacchetta R, Gabbiano C, Sacchetti C, Cerutti F et al. Interleukin-2 production and interleukin-2 receptor expression in children with newly diagnosed diabetes Clin Immunol Immunopathol 1988; 49: 53–62
Kaye WA, Adri MN, Soeldner JS, Rabinowe SL, Kaldany A, Kahn CR et al. Aquired defect of interleukin-2 production in patients with type I diabetes mellitus N Engl J Med 1986; 315: 920–924
Catheley GB, Amor B, Fournier C . Defective IL-2 production in active rheumatoid arthritis: regulation by radiosensitive suppressor cells Clin Rheumatol 1986; 5: 482–492
Jokinen EI, Mottonen TT, Hannonen PJ, Arvilommi HS . Association of in vitro immune functions with the severity of the disease in rheumatoid arthritis Br J Rheumatol 1993; 32: 550–555
Steiner G, Studnicka-Benke A, Witzmann G, Hofler E, Smolen J . Soluble receptors for tumor necrosis factor and interleukin-2 in serum and synovial fluid of patients with rheumatoid arthritis, reactive arthritis and osteoarthritis J Rheumatol 1995; 22: 406–412
Cuadrado MJ, Marubayashi M, Ortega C, Fernandez-Arcas N, Garcia-Cozar F, Pena J et al. Relationship of IL-2, IL-2R (CD25+), soluble IL-2R, and IL-4 with disease activity in SLE patients Lupus 1993; 2: 257–260
Kucharz EJ, Sierakowski SJ, Goodwin JS . Lithium in vitro enhances interleukin-2 production by T cells from patients with systemic lupus erythematosus Immunopharmacol Immunotoxicol 1993; 15: 515–523
Samosonov MY, Tilz GP, Egorova O, Reibnegger G, Balabanova RM, Nassonov EL et al. Serum soluble markers of immune activation and disease activity in systemic lupus erythematosus Lupus 1995; 4: 29–32
Suzuki T, Suzuki N, Engleman EG, Mitsushima Y, Sakane T . Low serum levels of dehydroepiandrosterone may cause deficient IL-2 production by lymphocytes in patients with systemic lupus erythematosus Clin Exp Immunol 1995; 99: 251–255
Corrales JJ, Orfao A, Lopez A, Mories MT, Miralles JM, Ciudad J . Analysis of IL-2 and IL-6 binding to peripheral blood lymphocytes in Graves’ disease. Relationship with disease activity Cytometr 1997; 30: 118–123
Eisenstein Z, Engelsman E, Weiss M, Kalechman Y, Sredni B . Modulation of the IL-2 production defect in vitro in Graves’ disease Clin Exp Immunol 1994; 96: 323–328
Navikas V, Link H . Review: cytokines and the pathogenesis of multiple sclerosis J Neurosci Res 1996; 45: 322–333
Selmaj K, Nowak Z, Tchorzewski H . Interleukin-1 and interleukin-2 production by peripheral blood mononuclear cells in multiple sclerosis patients J Neurol Sci 1988; 85: 67–76
Wandinger KP, Wessel K, Neustock P, Siekhaus A, Kirchner H . Diminished production of type I interferon and interleukin-2 in patients with multiple sclerosis J Neurol Sci 1997; 149: 87–93
Hartung HP, Reiners K, Schmidt B, Stoll G, Toyka KV . Serum interleukin-2 concentrations in Guillain-Barré syndrome and chronic ideopathic demyelinating polyradiculoneuropathy: comparison with other neurological diseases of presumed immunopathogenesis Ann Neurol 1991; 30: 48–53
Zoukos Y, Kidd D, Woodroofe MN, Kendall BE, Thompsom AJ, Cuzner ML . Increased expression of high affinity IL-2 receptors and beta-adrenoreceptors on peripheral blood mononuclear cells is associated with clinical and MRI activity in multiple sclerosis Brain 1994; 117: 307–315
Ciampolillo A, Guastamachia E, Caragiulo L, Lollino G, DeRobertis O, Lattanzi V et al. In vitro secretion of interleukin-1 beta and interferon-gamma by peripheral blood lymphomononuclear cells in diabetic patients Diabetes Res Clin Prac 1993; 21: 87–93
Vonherrath MG, Oldstone MBA . Interferon gamma is essential for destruction of beta cells and development of insulin-dependent diabetes mellitus J Exp Med 1997; 185: 531–539
Baldeon ME, Neece DJ, Nandi D, Monaco JJ, Gaskins HR . Interferon gamma independently activates the MHC class I antigen processing pathway and diminishes glucose responsiveness in pancreatic cell lines Diabetes 1997; 46: 770–778
Zangerle PF, DeGroote D, Lopez M, Meuleman RJ, Vrindts Y, Fauchet F et al. Direct stimulation of cytokines (IL-1 beta, TNF-alpha, IL-6, IL-2, IFN-gamma, and GM-CSF) in whole blood: II. Application to rheumatoid arthritis and osteoarthritis Cytokine 1992; 4: 568–575
Gattorno M, Facchetti P, Ghiotto F, Vignola S, Buoncompagni A, Prigione I et al. Synovial fluid T cell clones from oligoarthricular juvenile arthritis patients display a prevalent TH1/TH0-type pattern of cytokine secretion irrespective of immunophenotype Clin Exp Immunol 1997; 109: 4–11
Dolhain RJEM, Vanderheiden AN, Terhaar NT, Breedveld FC, Miltenburg AMM . Shift towards T-lymphocytes with a T-helper1 cytokine secretion profile in the joints of patients with rheumatoid arthritis Arthritis Rheumatism 1996; 39: 1961–1969
Olsson T . Cytokine-producing cells in experimental autoimmune encephalomyelitis and multiple sclerosis Neurology 1995; 45: (suppl 6) 11–15
Beck J, Rondot P, Catinot L, Falcoff L, Kirchner H, Wietzerbin J . Increased production of interferon gamma and tumor necrosis factor precedes clinical manifestation in multiple sclerosis: do cytokines trigger off exacerbations? Acta Neurol Scand 1988; 78: 318–323
Merrill J, Jonakait GM . Interactions of the nervous and immune systems in development, normal brain homeostasis, and disease FASEB J 1995; 9: 611–618
Jonakait GM . Interferon-gamma promotes cholinergic differentiation of embrionic septal nuclei and adjacent basal forebrain Neuron 1995; 12: 1149–1159
Nistico G, DeSarro G . Is interleukin-2 a neuromodulator in the brain? Trends Neurosci 1991; 14: 146–150
Alonso R, Chaudieu I, Diorio J, Krishnamurthy A, Quirion R, Boksa P . Interleukin-2 modulates evoked release of 3H-dopamine in rat cultured mesencephalic cells J Neurochem 1993; 61: 1284–1290
Lapchak PA . A role for interleukin-2 in the regulation of striatal dopaminergic function Neuro Report 1992; 3: 165–168
Pasternak KI, Timo-Iara C, Rodrigues CJ, Maria DA, Duarte AJS, Paiva L et al. Circumscribed lesion of the medial forebrain bundle area causes structural impairment of lymphoid organs and severe depression of immune function in rats Mol Psychiatry 1998; 3: 397–404
Claret E, Renversez J-C, Zheng X, Bonnefoix T, Sotto J-J . Valid estimation of IL-2 secretion by PHA-stimulated T-cell clones absolutely requires the use of anti-CD25 monoclonal antibody to prevent IL-2 consumption Immunol Lett 1992; 33: 179–186
Rapaport MH, Torrey EF, McAllister CG, Nelson DL, Pickar D, Paul SM . Increased serum interleukin-2 receptors in schizophrenic monozygotic twins Eur Arch Psychiatr Clin Neurosci 1993; 242: 7–10
Ganguli R, Brar JS, Chengappa KNR, DeLeo M, Yang ZW, Shurin G et al. Mitogen-stimulated interleukin-2 production in never-medicated, first episode schizophrenic patients Arch Gen Psychiatry 1995; 52: 668–671
Rothermundt M, Arolt V, Weitzsch C, Eckhoff D, Kirchner H . Immunological dysfunction in schizophrenia: a systematic approach Neuropsychobiology 1998; 37: 186–193
McAllister CG . Rapaport MH, Pickar D, Paul SM. Effects of short-term administration of antipsychotic drugs on lymphocite subsets in schizophrenic patients Arch Gen Psychiatry 1989; 46: 956–957
Müller N, Ackenheil M, Hofschuster E, Mempel W, Eckstein R . Cellular immunity in schizophrenic patients before and during neuroleptic treatment Psychiatry Res 1991; 37: 147–160
Rapaport MH, Lohr JB . Serum soluble interleukin-2 receptors in neuroleptic naive schizophrenic subjects and in medicated subjects with and without tardive dyskinesia Psychiatr Scand 1994; 90: 311–315
Leykin I, Mayer R, Shinitzky M . Short and long-term immunosuppressive effects of clozapine and haloperidol Immunopharmacology 1997; 37: 75–86
Hinze-Selch D, Becker EW, Stein GM, Berg PA, Mullington J, Holsboer F et al. Effects of clozapine on in vitro immune parameters: a longitudinal study in clozapine-treated schizophrenic patients Neuropsychopharmacology 1998; 19: 114–122
Pollmächer T, Hinze-Selch D, Mullington J, Holsboer F . Clozapine-induced increase in plasma levels of soluble interleukin-2 receptors (letter) Arch Gen Psychiatry 1995; 52: 877
Ganguli R, Brar JS, Rabin BS . Clozapine-induced increase in plasma levels of soluble interleukin-2 receptors (comment) Arch Gen Psychiatry 1995; 52: 878
Sasaki T, Nanko S, Fukuda R, Kawate T, Kunugi H, Kazamatsuri H . Changes of immunological functions after acute exacerbation in schizophrenia Biol Psychiatry 1994; 35: 173–178
Gudewill S, Pollmacher T, Vedder H, Schreiber W, Fassbender K, Holsboer F . Nocturnal plasma levels of cytokines in healthy men Eur Arch Psychiatry Clin Neurosci 1992; 242: 53–56
Uthgenannt D, Schoolmann D, Pietrowsky R, Fehm HL, Born J . Effects of sleep on the production of cytokines in humans Psychosom Med 1995; 57: 97–104
Irwin M, Thompson J, Miller C, Gillin JC, Ziegler M . Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications J Clin Endocrinol Metab 1999; 84: 1979–1985
Appelberg B, Katila H, Rimon R . Plasma interleukin-1 beta and sleep architecture in schizophrenia and other nonaffective psychoses Psychosom Med 1997; 59: 529–532
Acknowledgements
This study was supported by the Stiftung Volkswagenwerk (Volkswagenwerk Science Foundation, No. I 71/998). We are grateful to Dörthe Eckhoff, MD and Christine Weitzsch, MD for their help with the patient recruitment and the laboratory work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arolt, V., Rothermundt, M., Wandinger, KP. et al. Decreased in vitro production of interferon-gamma and interleukin-2 in whole blood of patients with schizophrenia during treatment. Mol Psychiatry 5, 150–158 (2000). https://doi.org/10.1038/sj.mp.4000650
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.mp.4000650
Keywords
This article is cited by
-
Interferon-γ acutely augments inhibition of neocortical layer 5 pyramidal neurons
Journal of Neuroinflammation (2020)
-
Abnormal levels of vascular endothelial biomarkers in schizophrenia
European Archives of Psychiatry and Clinical Neuroscience (2018)
-
Relationship of Interferon-γ to Cognitive Function in Midlife Women with Schizophrenia
Psychiatric Quarterly (2018)
-
Serial Mitogen-Stimulated Cytokine Production from Continuously Ill Patients with Schizophrenia
Neuropsychopharmacology (2010)