Key Points
In brief
-
Levels of complexity of treatment were determined for endodontics, periodontics, fixed and removable prosthodontics.
-
Modifying factors relate to patient management.
-
Priority for specialised treatment was related to the complexity of providing care.
Abstract
The process undertaken to establish an initial pilot index for restorative dental treatment is described. Following consultation with a wide range of clinicians and others, an outline framework for the index was developed and comprised three main components: 1. Patient identified need for treatment: the data from the patient perceived need questionnaire were inconclusive; 2. Complexity of treatment (assessed by clinicians): this was found to be a practical tool capable of being used by a range of dentists. A booklet has been produced which describes the process of using the scoring system; 3. Priority for treatment (assessed by clinicians): three levels of priority were identified; the highest priority was assigned to patients with inherited or developmental defects that justify complex care (eg clefts of the lip and palate). The initial development of the index has had some success in a difficult area. The treatment complexity component is the most developed and may allow both referrers and commissioners of specialist restorative dentistry to determine appropriate use of skilled clinicians' expertise.
Similar content being viewed by others
Main
In the specialty of orthodontics an index of treatment need has been used for some years to categorise patients according to the severity of their malocclusion.1 The index allows informed choices to be made by service providers and purchasers regarding types of patients and treatment categories appropriate for inclusion in service contracts.
In the specialty of restorative dentistry no similar index of treatment need exists, although an index which measures oral health status with particular reference to the adequacy of dental restorations has been described.3 The Clinical Audit Committee of the Faculty of Dental Surgery, Royal College of Surgeons of England identified the requirement for such an index and obtained funds from the Department of Health to support a development project. The project was administered by the Audit Working Group for Restorative Dentistry and a research team was established following approval from the Department of Health. The aim of the project was to establish an initial pilot index that would allow need to be identified and ranked by complexity. The index would have to be simple to use, based on evidence, reproducible and produce patient-based data that would be amenable to statistical analysis. It was intended that the index, once developed might be used in a similar way to the orthodontic index, both to inform purchasers during contract negotiations and to audit referral and clinical activity.
This paper describes the process undertaken to establish an index of treatment need for restorative dentistry. It outlines the structure of the complexity component of the index, provides details of the codes agreed and summarises the progress in developing contributory components.
Background
Dental indices that measure need for treatment rather than dental health status are not widely used in the UK. The exceptions are the Index of Orthodontic Treatment Need1 and the Community Periodontal Index of Treatment Need.2 Each has been used as both a population based measurement and, with modification, as an individual treatment planning tool. They enable treatment complexity as well as past disease activity to be quantified. IOTN incorporates a patient-assessed component and records clinician assessed treatment need, but its scoring system does not give an indication of treatment complexity. Neither index addresses the aetiology of the condition but merely seeks to measure the need for intervention. Each index enables audit of patient selection and permits some limited analysis of treatment outcome.
It was decided to design a restorative dental index incorporating some of the features of these two well-used and evaluated examples.
Establishing and testing the framework of the index
Two researchers, (HF, PR) contacted and then visited eight restorative dental departments in teaching hospitals and one district general hospital within the UK. In addition, they met with senior representatives of the British Dental Association, Community Dental Service, Faculty of General Dental Practitioners, Dental Practice Board, Dental Protection Societies and Consultants in Dental Public Health. The aim was to establish an understanding of the key issues relating to referrals for restorative dental care and to ensure any resulting index took these views into account.
An outline framework for the index was developed and comprised three main components:
-
1
Patient identified need for treatment
-
2
Complexity of treatment (assessed by clinician)
-
3
Priority for treatment (assessed by clinician)
An outline of the proposed index, together with several clinical case reports to illustrate the index structure, was presented to the consultants in restorative dentistry group at an annual meeting. The aim was to seek co-operation and promote consensus prior to establishing draft codes and initial boundaries to rank priority and complexity. It was decided to achieve this initially with a series of questionnaires circulated to clinicians within the specialty. Nominees from the relevant specialist societies (British Society for Restorative Dentistry, British Society for the Study of Prosthetic Dentistry, British Endodontic Society, British Society for Periodontology) contributed to the questionnaire design and content. The questionnaires identified a range of treatment procedures undertaken in restorative dentistry and asked respondents to score each treatment process separately for priority and complexity.
A postal questionnaire was distributed to 141 members of the consultants in restorative dentistry group. The questionnaire was divided into sections relating to the so-called 'mono specialities' within restorative dentistry (periodontics, endodontics, fixed and removable prosthodontics). Some consultants, with a known mono-specialty interest, were sent only sections of the questionnaire that were relevant to their own clinical activity. A 66% return was achieved from those circulated.
Data were analysed from the returned questionnaires and found to be sufficiently consistent to develop an initial series of codes and boundaries (low, moderate, high) for the complexity component of the index for dentate patients. The edentate were seen, from the questionnaires, to present a different complexity ranking task to the dentate. The data from the priority sections of the questionnaires were inconclusive.
Complexity component
The returned questionnaires allowed a draft complexity index to be compiled, listing a series of restorative procedures as either:
Complexity code 1 Able to be performed by any dental graduate
Complexity code 2 Able to be performed by any experienced dentist
Complexity code 3 Able to be performed by any dentist with skills developed following specialist training
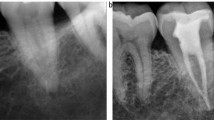
This first draft of the index was refined by a group of consultants and specialist trainees in a series of structured discussions. The subsequent draft was taken to a group of ten dentists from across the UK, consisting of vocational trainers, specialist practitioners and hospital consultants. The clinicians were involved in a facilitated discussion to further refine the components of the index. A final version of the complexity component was agreed and, in order to determine the feasibility of using the index, it was then applied by the same group of dentists to clinical data. These comprised clinical information, study models and radiographs. The index was found to be an appropriate and practical tool and feedback was obtained about layout, wording and presentation.
Reproducibility exercise
A training and reproducibility exercise was organised at the Dental Practice Board in Eastbourne. A group of 14 clinicians from general dental practice, community dental practice and the dental practice board took part in a training and reproducibility exercise to test the inter examiner variability of the complexity component of the index. Following an introductory training session, involving an explanation of the codes, presentation of clinical examples and a hands-on training exercise, each participant applied the index to 17 sets of clinical data. They were asked to assign a complexity score to each data set. The resultant data were analysed, comparing the codes assigned by each participant with the codes previously agreed by the research team. One set of clinical data was duplicated and unknowingly scored twice to measure intra examiner variation.
Results
The results showed no marked contrasts or trends between the three practitioner groups and so they were combined. The mean time for the assessment of each data set was 6.1 minutes. There was a mean conformity coefficient (a measure of the level of agreement of scores between participants) for the group of 80%. (Range 64%–96%). With 17 cases and four categories per case (periodontics, root canal treatment (RCT), fixed prosthodontics and removable prosthodontics), there were theoretically 68 possibilities for unanimous agreement. However, one participant omitted a RCT score for one patient, bringing the total possible number of recorded scores to 67. There were 31 out of 67 records of unanimous agreement among the 14 participating practitioners. A more detailed breakdown is shown in Table 1, where results are itemised according to category. This shows that there were two or fewer dissenters from a unanimous diagnosis in 40 out of 67 records (60%), and four or fewer dissenters in 53 out of 67 records (79%).
When the decisions reached by the participants were compared with those anticipated by the project team, in terms of grading (ie not applicable and grades 1–3), there was a unanimous or a majority agreement in 32 out of 32 instances of a 'not applicable' diagnosis, 7 out of 14 instances of a 'Grade 1' diagnosis, 2 out of 2 of a 'Grade 1-2', 5 out of 11 of a 'Grade 2', and 7 out of 8 of a 'Grade 3', giving a total of 53 out of 67 majority agreements. A more detailed breakdown is given in Table 2.
In terms of categories and cases there was majority agreement (over 50%) in 12 out of 17 periodontal categories, 14 out of 16 RCT categories, 13 out of 17 removable prosthodontics categories and 14 out of 17 fixed prosthodontics categories. Table 3 contains a more detailed breakdown.
The assessment process
A booklet was designed describing the process of applying the complexity assessment (Figs. 1, 2). The assessment process involves examining the patient and applying a complexity code (range 1–3) for each component of the examination that relates to restorative dentistry. The complexity codes are divided into four main components (Figs. 3456), involving a periodontal treatment assessment, a root canal treatment assessment, and separate assessments in fixed and removable prosthodontics. Each component of the assessment should be considered separately and may be the only relevant component for the complexity assessment for that patient. Each complexity component has a series of clinical descriptors that are ranked as low (code 1), moderate (code 2) or high complexity (code 3); to these a modifying factor may apply. The modifying factors (Fig. 7) are similar for each component of the index although there are small variations. They are predominantly related to patient management issues. Modifying factors only increase complexity by one code increment; they are not cumulative. The highest complexity is code 3.
How to use the complexity assessment tool
Step 1
Following a clinical examination and assessment of the patient's oral status, appropriate codes are selected which most closely describes the patient's condition or treatment requirement.
For example, a patient with a BPE score of 3 in one sextant, a non vital molar tooth with one root canal curvature greater than 40 degrees to the root long axis and requiring a mucosal born partial prosthesis would be scored
Periodontal complexity 1
Root canal treatment complexity 3
Prosthodontic complexity 1
Step 2
The highest code achieved in any of the individual components is the overall restorative dentistry complexity score
In the example given, there would be an overall restorative dentistry complexity code of 3.
Step 3
The complexity codes are then recorded on a data collection sheet, together with an indication of whether modifying factors apply. Application of a modifying factor increases the score by one increment, unless the maximum score has already been achieved. This is the final restorative dentistry complexity score.
In the example given the highest complexity score (3) has already been achieved and an additional modifying factor relating to the management of the patient would not change the level of complexity assessment.
Priority component
The questionnaires referred to in the first phase of the project failed to give any clear indication of priority for specialist treatment, either in relation to patient category, or dental procedure.
A workshop was held involving a group of 10 clinicians including general dental practitioners, community dentists, consultants in restorative dentistry and in dental public health. Prior to the group work all participants agreed some fundamental principles:
-
Any patient should have access to consultant services for advice or treatment planning guidance, following appropriate referral from a primary care practitioner.
-
Any patient should have equal access to specialist care irrespective of socio-economic group, gender, age or racial origin
-
Only those patients for whom treatment was of sufficient complexity to justify care from a trained specialist (assessed as part of the complexity coding) should receive care.
Participants were divided into two groups and asked to agree whether there were any categories of patients who should receive priority for restorative dentistry specialist treatment. Subsequent to this initial task the two groups were asked to debate and if possible agree whether there were any aspects of treatment or particular groups of teeth that should be considered a priority for specialist care. The two groups then shared their ideas and attempted to reach a consensus about the priorities raised.
Results – categories of patients
The two working groups considered that many of the patient groups that could be considered a priority category would already be scored as such via the modifying factors applied in the complexity assessment process.
The following patient categories were ranked as a priority for specialist restorative dental treatment:
Priority One
-
Patients with inherited or developmental defects that justify complex care (eg clefts of the lip and palate, hypodontia, amelogenesis imperfecta, etc.)
Priority Two
-
Those who have previously received complex care that requires maintenance or replacement (assessed as part of the complexity assessment process).
-
When tooth or tissue loss has occurred as the result of trauma.
-
People with special needs, including those with learning difficulties, physical disabilities, social impairment, mental illness or who are medically compromised.
-
When multi-specialty working is indicated.
-
Those receiving oncology treatment that has implications for oral and dental care, (to include those people requiring post surgical reconstruction with a fixed or removable prosthesis).
-
Those for whom a lack of specialist treatment may affect their livelihood (eg musicians).
-
Where specific facilities were required to enable treatment (eg in patient or day stay care requiring general anaesthetic facilities with specialist anaesthetist support).
Reduced priority
The working groups agreed that there were certain factors that would reduce priority for specialist care:
-
Lack of motivation or commitment to comply with preventive regimens, although it was acknowledged that certain patient groups may have difficulties complying and special consideration should be given to them.
-
Smokers in certain categories of care, eg periodontal therapy, implant treatment.
Results – types of treatment
Both the working groups agreed the following objectives when establishing priorities in restorative dentistry:
-
To maintain 20 functioning, aesthetic and predictably healthy teeth.
-
To maintain sufficient teeth in each dental sextant to provide a foundation for a fixed or removable prosthesis, where possible avoiding a free end saddle appliance.
Patient assessed need component
The Index of Orthodontic Treatment Need incorporates a patient assessment of need via an aesthetic component. This was designed following the construction of an illustrated 10-point scale using dental photographs of 12-year-old children and rated by six non-dental judges. In restorative dentistry there are other factors that affect patient assessed need including oral pain or discomfort, difficulties when eating or social embarrassment. An aesthetic assessment was considered and rejected, since it would only have reflected part of the patients' assessed component of need.
Other measures of patient assessed need have been developed, and largely focus on the impact of oral disorders on an individual, rather than an attempt to measure need for a particular intervention, since it is argued that most patients are not able to comment on the latter.5,6 One measure which has been adopted for measuring the impact of oral disorders with different groups of patients is the Oral Health Impact Profile (OHIP).7
It was decided to pilot a simplified version of the OHIP as a basis for the development of the patient assessed need component, since it contained a wide range of indicators relevant to restorative dentistry and had been widely tested.
A questionnaire based on the Oral Health Impact Profile was developed and used to conduct structured interviews at three dental teaching hospitals and one district general hospital across England.
A total sample of 171 patients attending for their first out patient appointment were asked a series of questions about the problems they experienced with function (eg eating, painful mouth), specific tooth-related issues (eg food impaction, sharp or broken teeth) and psycho-social issues (eg embarrassment, sleep disturbance). Before the initial consultation, the participants were asked to quantify their problem using a visual analogue (Likert) scale. All patients attending the participating specialist clinics on the selected days were invited to take part. The questionnaires were administered by one of the project team (HF) or a trained member of clinical audit staff. Analysis of both the initial questionnaires and when they were repeated, indicated inconsistent results that would require a further study with a larger patient sample to establish whether this form of self reported profile analysis could yield an appropriate measurement tool.
Discussion
This initial development of an index of treatment need for restorative dentistry has had some success in a difficult area. The development of the complexity component of this index will help to initiate a debate concerning treatment complexity and as the only complexity index for restorative dentistry currently, may find sufficient support to be used both to inform the referrer, provider and purchaser about specialty care. There is potential for it to be used as a quality monitoring indicator and it may have a role in clinical governance for specialist restorative dental care. The process involved in designing the complexity component and the reproducibility exercise would suggest that it is a practical, easy to use complexity assessment tool. Its validity has been demonstrated in ideal conditions with a small representative group of clinicians, but will need to be extensively tested with a much larger patient group, using live clinical examinations and a greater number of clinicians from diverse backgrounds. It is likely that it could be a useful tool for assessing individual adults requiring restorative treatment, but would need to be tested on a whole population sample before recommendations could be made about its applicability in general epidemiological surveys. The individual criteria used are relatively simple and easily understandable. Where possible they have been based on accepted and validated measures, for example CPITN; but the grades of complexity are based on collective clinical opinion, taken from both the questionnaire and subsequent modification by the working groups. Further studies are needed on clinical outcomes for restorative procedures carried out by clinicians with differing experience and training, and these should inform the complexity bandings, which currently are subjective.
Whilst restorative dental treatment is largely mechanistic, patient management also involves both bio-medical and psychological assessment. An attempt has been made to address this through the modifying factors.
When taken as a whole, the final complexity score can only represent an indicative, broadly based measure of complexity, but the individual elements of the composite index offer a more precise measure, although with the same caveats as before.
The priority working group proposed a number of groups of patients for specialist care and described those who were either more vulnerable or who more frequently appeared to need help from specialist advice, treatment or facilities. They largely reflected current priorities in NHS specialist practice.
The use of the Oral Health Impact Profile has promise in developing a patient initiated measure of perceived need. Patients perceive their needs to be related to comfort, function and appearance. Dentists use similar criteria but place more emphasis on the presence of disease to prioritise need. The highest values in the scoring of treatment need will therefore always be attributable to conditions causing pain or difficulties with eating or speaking, in addition to an unacceptable dental appearance. Frequently such problems can be resolved within primary dental care without requiring specialist help. The need for specialist help becomes apparent when the care that is required is outside the experience, abilities or facilities available to the referring primary care dentist. The need for specialist care is therefore more often related to issues of complexity of care, giving an element of priority to those patients who have more complex management requirements.
A booklet outlining the complexity component of the index is available from the authors.
References
Brook P H, Shaw W C . The development of an index of orthodontic treatment priority. Eur J Orthod 1989; 11: 309–320.
Ainamo J, Barmes D, Beagrie G, Cuttress T, Martin J, Sardo-Infirri J . Development of the World Health Organization (WHO) community periodontal index of treatment need (CPITN). Int Dent J 1982; 32: 281–291.
Burke F J T, Wilson N H F . Measuring Oral health: an historical view and details of a contemporary oral health index (OHX). Int Dent J 1995; 45: 358–370.
Cushing A M, Sheiham A, Maizels J . Developing sociodental indicators – the social impact of dental disease. Community Dent Health 1986; 3: 3–17.
Atchison K A, Dolan T A . Development of the geriatric oral health assessment index. J Dent Educ 1990; 54: 680–687.
Locker D . Measuring oral health: a conceptual framework. Community Dent Health 1988; 5: 3–18.
Slade G D, Spencer J . Development and evaluation of the oral health impact profile. Community Dent Health 1994; 11: 3–11.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Falcon, H., Richardson, P., Shaw, M. et al. Developing an index of restorative dental treatment need. Br Dent J 190, 479–486 (2001). https://doi.org/10.1038/sj.bdj.4801010
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4801010
This article is cited by
-
A practitioner's guide to gutta-percha removal during endodontic retreatment
British Dental Journal (2017)
-
Evaluation of a system for grading the complexity of root canal treatment
British Dental Journal (2007)
-
Conscious sedation training received by specialist registrars in restorative dentistry in the UK: a survey
British Dental Journal (2006)
-
A survey of demand for specialist restorative dental services
British Dental Journal (2005)
-
Conscious sedation services provided in secondary care for restorative dentistry in the UK: a survey
British Dental Journal (2005)