Key Points
-
When considering the future demand for dental services the effects of an ageing population need to be taken into account.
-
The impact of a growth both in numbers of older people, and especially the very old, are examined.
-
Account is taken of differences in gender and ethnic origin.
-
The likely effects of an ageing workforce and changes in attitudes, living conditions and technology are also considered.
-
They all lead to the conclusion that older people are currently disadvantaged and policy needs to take this into account.
Abstract
When considering the future demand for dental care and the consequent provision of services for the older population there are two key demographic issues that need to be discussed. The first concerns the older population itself and the second concerns the workforce. This paper focuses on the former but discusses the latter briefly.
Similar content being viewed by others
Main
The current focus of interest of the British Dental Association is the effect of an ageing population in twenty years time. Projections by the Government Actuary's Department (GAD) now go up to 2070 but this is in response to demand for such data and using current assumptions.1 The United Nations (UN) is prepared to make projections to 2050 However, any projections need a health warning because many factors could alter them. In particular assumptions about declining fertility rates may have to be revised in the light of increased migration. Similarly there is need for caution about medical advances. For example anything, such as the development of drugs, that would improve the position of people with dementia would reduce the burden of care. Nor do we know what resources older people will have in the future. At the moment the evidence is that the gap between the rich and poor is growing.2
Ageing in the United Kingdom — the older population
There are a number of elements when considering the older population. These include:
-
a
An increase in overall numbers and percentages of older people.
-
b
An increase in numbers and percentages of very old people.
-
c
A continued preponderance of older women.
-
d
An increase in numbers and percentages of older people from black and ethnic minority groups.
When drawing conclusions about these groups it is tempting to examine the position of older people in that group now and project it to the future. However, cohort differences are important. People who are 50 now and will be 70 in 20 years are likely to be substantially different from those who are 70 now.
a. An increase in overall numbers and percentages of older people
Table 1 shows that while the total population of the United Kingdom (UK) will grow from 588 million in 2001 to 622 million in 2020 a substantial number will be accounted for by the rise of those aged 65 and over from 94 million to 12 million. Even more striking is the rise in the percentage of those aged 65 and over in the population from 159% to 193%.
It is important to take account of short-term effects within these overall figures. For example 1920 saw the highest number of babies born in the last century. This large group, which experienced some deaths in World War 2, are now aged 82 Similarly there will be the short-term effect of the baby boomers of the 1940s who are now entering retirement. Another group are the baby boomers born in the mid 1960s which will lead to a further rise in numbers of older people in 30 years time.
The reasons for the increases in numbers of older people is partly that people are living longer and, in the developed world, mainly due to falls in mortality at older ages. But what must also be taken into account in looking at percentages of older people compared with other ages is the effect of the fall in the birth rate. Table 2 shows the dramatic drop in total live births per 1000 women aged 15-44 in the UK.3 From a rate of 91 per 1,000 in 1961 the rate fell to 55 in 2000.
What is relevant in looking at population figures is the likely effects. While generalisations are dangerous one of the obvious effects is on health and health services. For example there is a strong association between age and disability as Table 3 shows. This shows that for some indicators of self reported health this was worse at older ages. Figures from the 1998 General Household Survey (GHS) show that comparing those aged 65-74 with those aged 75 and over 37% of the former reported limiting long-standing illness compared with 48% of the latter and the former reported 52 days with acute sickness compared with 72 of the latter.4 In 1998 over half (58%) of people aged 75 and over had no natural teeth.5 But even in very old age there is evidence of good health (see the next section).
There is evidence that older people are disadvantaged in dentistry. Access to NHS Dentistry, the first report of the House of Commons Health Committee found that certain groups, including older people and those with dementia (one in five over the age of 80) suffer particular problems over access to dental services.6 They also argued that there should be greater clarity about the availability of NHS treatment.
When looking at these figures, differences between groups must always be taken into account. Gender and ethnic differences will be considered later but other likely variations should also be noted. Geographical variations will mean differences in the kinds of patients that dentists treat. For example in 1997 Conwy had the highest percentage of people over pension age with 25%.7 There are also clusters of areas around the south coast including Dorset, Isle of Wight and Sussex where there are above average percentages. London has a lower than average proportion.
Resources is another area where generalisations are dangerous. 'Pensioners' incomes have risen, but so has the gap between the richest and the poorest' is the conclusion of a recent study by Curry and O'Connell.7 These authors also found that a quarter of pensioners are in relative poverty and that 'The make up of pensioners' incomes will change but there are no signs that future pensioners will be relatively better off than the pensioners of today'.2 The ability to pay for health services will be severely jeopardised by evidence about low incomes. In NHS Dentistry: Options for Change, the Department of Health (DH) stated 'Fear of cost, made worse by lack of information on cost, is a major barrier to older people accessing care'.8
b. An increase in numbers and percentages of very old people
Decisions about how very old is defined is an ad hoc one. Looking at those aged 85 and over Table 4 shows that numbers and percentage of very old people is projected to increase in the next 20 years.1 Whereas there were 11 million people aged 85 and over by 2020 another half a million will have been added. As a percentage of the total population there will be a rise from 19% to 25% but as a percentage of those over the age of 65 it will rise from 21% to 129%.
On average very old people will experience worse health but many very old people are in relatively good health. In an analysis of those aged 80 and over compared with other older people it was found that about half of the former had no limiting long-standing illness and nearly half the men and one quarter of the women had no difficulty with any tasks (Table 5).9 In addition 17% of men and 9% of women had given regular help to someone outside the household.9
Looking specifically at those aged 85 and over one study Eighty Five Not Out, which was both quantitative and qualitative, contained findings which are relevant to health professions.10 One of the objectives was to look at differences in old age. A good example is over living conditions. While 5% of those aged 65 and over live in an institution the percentages change dramatically when the figures are disaggregated. As Table 6 shows only 1% of those aged 65-69 are in an institution while 48% of those aged 95 and over are.
The qualitative interviews showed the strong wish for 'independence' and the desire to live at home. Views about being very old can work both ways. Some of the older people interviewed thought that they were not old enough to move while others were too old. The importance of family support, the home and the role of primary care and basic services came out clearly. So did the timing and appropriateness of services and the personal qualities of service providers.
c. A continued preponderance of older women
Gender differences are important when considering older people. A higher percentage of the older population are women and this is predicted to continue (Table 7).1 Numbers of men aged 65-84 are expected to grow from 36 million in 2001 to 49 million in 2020 while those for women will rise from 46 million to 56 million. For those aged 85 and over both groups are expected to grow by about half a million. It should also be noted that a higher percentage of the female population is old/very old (Table 8).3
Women have higher rates of disability than men but differences in kinds of conditions eg women are more likely to have arthritis and less likely to have a stroke. Women are more likely to have muscoskeletal problems, to be more obese (markedly in very old age), less likely to participate in exercise, more likely to report increased anxiety and depression. But they have a higher expectation of life, are less likely to drink excessive amounts of alcohol and are likely to have stronger social networks.
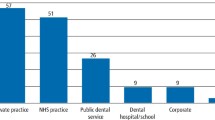
The special General Household Survey module in 1998 on people aged 65 and over showed that women were less likely to use a dentist than men (Table 9).11
d. An increase in numbers and proportions of older people from black and ethnic minority groups
It is difficult to project numbers and proportions of older people from black and ethnic minority groups without taking into account both those who may come into the country and those who may leave. Nationals from the European Union have the right to live in the UK provided they are working or are able to support themselves financially. This is in addition to those from other countries who need Home Office acceptance. With the widening of the EU to many countries in Eastern Europe it is inevitable that numbers will increase. Whether they will stay until old age is a debatable point.
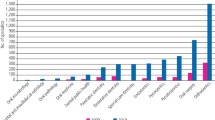
Looking at younger age groups it is not hard to see that numbers in the older age groups are likely to increase. Table 10 shows that currently 16% of the white population of the population are aged 65 and over but only 7% of the Indian, 5% of the black and 4% of the Pakistani/Bangladeshi population are.3 However, in younger age groups the position is reversed. Thus, while 20% of the white population are aged 16 and under the figures for the black population is 34%, for the Indian it is 23% and for the Pakistani/Bangladeshi is 37%.
The Acheson report on Inequalities in Health (1998) found that 'Overall people from minority ethnic groups are more likely to describe their health as 'fair' or 'poor' than the ethnic majority' although it is pointed out that there is danger in generalising about such a diverse group.12 It is already known from Modernising NHS Dentistry — implementing the NHS Plan that black and ethnic minority groups have poorer than average oral health.13
Ageing in the United Kingdom — an ageing workforce
It is projected that there will be a small drop in the percentage of people of working age (16-64) — from 64% in 2001 to 63% in 2020 (Table 11).1 The figures need careful interpretation, as some of those aged 16-64 will not necessarily be in work. Similarly the assumption is that a growing proportion of those aged 65 and over will be encouraged to remain in work. Looking further ahead, the United Nations forecast a halving of the potential support ratio (the number of people aged 15-64 per 1 older person aged 65 and over) in the UK.14 From four in 2002 it is projected to decline to two in 2050.
As in other professions the figures on the estimated decline in numbers of working age is likely to have repercussions. For example shortages of dentists may lead, as it has in other professions, to an increase in the role of those who are less qualified such as dental therapists and hygienists.15
Changes in attitudes, living conditions and technology: some effects on dentistry
It is worth touching briefly on a few other issues which may be relevant when considering other aspects of ageing.
a. Changing attitudes and growing expectations
Expectations are growing about the kinds of services to be provided. There is growing evidence that older people, in common with others, are also more likely to speak up for themselves in the future. The next generation are likely to demand more and to participate in decision making as other patients/consumers are. Initiatives such as the Better Government of Older People, Patients Forums and the use of older people as advisers are likely to grow. For example in planning services and in research it is becoming obligatory to include 'consumers' 'lay people' and 'champions' before funding is forthcoming.
b. Living conditions
As has already been seen most older people live in a home of their own rather than in an institution. In response to research which shows that most older people do not want to move to a hospital, nursing home or residential care home there is likely to be even more emphasis on staying at home solutions. The Department of Health state that 'Access to dental care can be particularly difficult for older people without access to their own transport'.8 However, while the focus of provision must be on older people in the community, and reaching people who live alone, different challenges are likely to be presented by those who live in an institution. The Department of Health admits that 'Older people in care homes do not receive uniformly high standards of oral health care'.8
Of those who live in the community a growing proportion live alone (Table 12).3 Whereas only 7% of households with one person over state pension age lived alone in 1961 that had grown to 15% in 20013 This increase mirrors the position for people of all ages where 14% of households were one person in 1961 and 29% in 2001 (Table 13).
c. The use of technology
Another factor, which is likely to have an impact on the dental care of older people, is developments in technology. This is not the place to discuss the impact of advances in technology such as telemedicine, but two developments should be mentioned. The first is the growing access that people have to information and communication. In 2000 17% of households where there were two adults, one or both aged 60 or over had access to the internet and 38% had access to a mobile phone (Table 14).4 For one adult aged 60 or over, the figures were 4% for access to the internet and 16% for a mobile phone.
The second development is in assistive (AT) technology for older people. Research for the Royal Commission on Long Term Care identified a number of options which could enable older people to live at home and be an alternative to an institution.16 One of these was assistive technology which was defined as 'an umbrella term for any device or system that allows an individual to perform a task they would otherwise be unable to do or increases the ease and safety with which the task can be performed'.17 This can range from simple aids and adaptations to sophisticated telemedicine. A current piece of research is looking at the feasibility, acceptability, costs and outcomes of providing AT in older people's existing homes.18
d. Some other effects on dentistry
Since 1978 the proportion of adults who have lost all their natural teeth has shown a steady decline. If this trend continues this will have a great effect on the profession. Another trend is the growth in proportions of very old people visiting the dentist. In 1991 for people aged 85 and over it was 5% and this had doubled to 11% in 1998 (Table 15).10
Conclusion
What does an ageing population mean for dentistry? It means a larger percentage of the population will be old or very old with consequent problems. Most will live in homes of their own except in very old age. But it is dangerous to generalise. They are likely to be as different as other generations and to ignore that is to adopt attitudes that are inappropriate. Policy initiatives are beginning to acknowledge the need for better services. The National Service Framework in a section on health promotion, stresses the need for both dental treatment and advice on oral health.19 The Department of Health admits that 'There is no comprehensive strategy for oral health for older people so local services can be patchy'.8 Their recommendations include the need to provide both a surgery and domiciliary based service, for dental premises to be accessible to older patients with mobility, sensory and other difficulties and for information aimed at older people to be widely available on the cost of care and how to access it.8
References
Government Actuary's Department. Population Projections 2000-2070. London: GAD, 2002.
Curry C, O'Connell A . The Pensions Landscape. London: The Pensions Policy Institute, King's College London, 2003.
Office for National Statistics. Social Trends, Number 32. London: The Stationery Office, 2002.
Office for National Statistics. General Household Survey 1998. London: The Stationery Office, 2000.
Office for National Statistics. The 1998 Adult Dental Health Survey. London: The Stationery Office, 2000.
House of Commons, Health Committee. Access to NHS Dentistry: First report. London: The Stationery Office, 2001.
Office for National Statistics. Social Focus on Older People. London: The Stationery Office, 1999.
Department of Health. NHS Dentistry: Options for Change. London: DoH, 2002.
Jarvis C, Hancock R, Askham J, Tinker A . Getting Around After 60. London: HMSO, 1996.
Tinker A, Askham J, Hancock R, Mueller G, Stuchbury R . Eighty five not out. Oxford: Anchor Trust, 2000.
Bridgwood A . People aged 65 and over: General Household Survey 1998. London: Office for National Statistics, 2000.
Acheson D . Inequalities in Health. London: Department of Health: London, 1998.
Department of Health. Modernising NHS Dentistry: Implementing the NHS Plan. London: DoH, 2000.
United Nations. Population Ageing 2002. New York: United Nations, 2002.
Health Services Journal. 26.10.2000.
Tinker A, Wright F, McCreadie C, Askham J, Hancock R, Holmans A . Alternative models of care for older people, research volume 2 for the Royal Commission on long term care. London: The Stationery Office, 1999.
Cowan D, Turner-Smith A . The role of assistive technology in alternative models of care for elderly people. In Tinker A, Wright F, McCreadie C, Askham J, Hancock R, Holmans A Alternative Models of Care for Older People, Research Volume 2 for the Royal Commission on Long Term Care. London: The Stationery Office, 1999.
The RE(Reading University)/ KI (King's College London) Engineering and Physical Sciences Research Council funded project: Introducing assistive technology into older people's homes: feasibility, acceptability, costs and outcomes. (www.equal.ac.uk/AT).
Department of Health. National Service Framework for Older People. London: DoH, 2001.
Acknowledgements
This article is based on a presentation made to the British Dental Association conference: Dental Care for Older People in 2020 on 5122002
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tinker, A. Ageing in the United Kingdom — what does this mean for dentistry?. Br Dent J 194, 369–372 (2003). https://doi.org/10.1038/sj.bdj.4809996
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4809996
This article is cited by
-
Minimising barriers to dental care in older people
BMC Oral Health (2008)
-
Dentistry – a professional contained career in healthcare. A qualitative study of Vocational Dental Practitioners' professional expectations
BMC Oral Health (2007)
-
Special Care Dentistry: a professional challenge
British Dental Journal (2007)
-
The neutral zone impression revisited
British Dental Journal (2005)
-
Older patients
British Dental Journal (2003)