Abstract
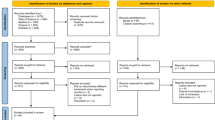
Data sources
PubMed/Medline, Embase and The Cochrane Library databases.
Study selection
Clinical studies with a minimum sample size of 20 teeth and six months follow-up period, providing clinical and radiographic assessment of success/failure were considered.
Data extraction and synthesis
Three reviewers selected the studies and assessed study quality. Weighted pooled success rates and 95% confidence interval (CI) estimates of the outcome were calculated and a random-effects meta-analysis was carried out.
Results
Eighteen studies involving 2373 patients were included. Eleven studies (1175 patients) considered microsurgery; four of these were RCTs, three prospective studies and four retrospective. Seven studies (1198 patients) addressed endodontic retreatment; six of these were prospective studies and one retrospective. There was a statistically significant difference between the weighted pooled success rates for the microsurgery group and retreatment group. This was apparent in all follow-up periods except those greater than four years.
Conclusions
The authors concluded that based on this study, endodontic microsurgery was confirmed as a reliable treatment option with favourable initial healing and a predictable outcome. Further long-term clinical studies investigating endodontic microsurgery and retreatment are needed in the future.
Similar content being viewed by others
Commentary
Root canal therapy constitutes a large number of treatments provided every year, with success rates reported to be in the range of 90% or above.1 However in a small percentage, failure often poses the dilemma of re-treating in the hope of saving the tooth. It is well acknowledged that the primary reason for failure of root canal treatment is a lack of sufficient disinfection and the inability to prevent re-colonisation of residual microorganisms.2,3 Nonsurgical retreatment is often considered the treatment of choice if a previously treated tooth has persistent apical periodontitis. However, a clinical judgment to retreat surgically or nonsurgically is based on a number of factors such as, the presence and size of the apical lesion, the root end filling material, type and quality of the coronal restoration, the status of previous root canal treatment etc.4,5,6,7,8,9. Root end microsurgery looks to provide a significantly enhanced direct access to that part of the root/s that affect the overall prognosis of the tooth.
The purpose of this study was to evaluate the outcomes of nonsurgical endodontic retreatment and endodontic microsurgery by meta-analysing all available literature from 1970 to 2012. The DerSimonian-Laird pooling method was used for this random-effects meta-analysis. The study reported that the micro-endodontic surgery had a significantly higher success rate than the retreatment group.
The authors have indicated that the results of a meta-analysis are significantly affected by the quality of the included studies; they reckon that the inadequate assessment of study qualities might be less meaningful or misleading. In this meta-analysis, the authors have tried to remove all confounding factors, however, the study analysis is still plagued by a general lack of standardisation. Factors such as the skill level of the operators, difficulty in standardisation of types of failures and the variability in the selection criteria for opting for nonsurgical vs endo-microsurgical treatment, could have a bearing on the final study outcome.10,11,12,13
This study uses pooled data of the included studies and categorises them into three, based on a quality assessment criterion. It's interesting to note that a substantially larger number of studies with quality ‘A’ were in the endo-microsurgery group (seven vs two). Further, the pooled success rate for this group was 90% and 74% (micro-endodontic vs nonsurgical retreatment). The respective pooled success rates for quality ‘B’ studies were 95% and 80%. This indicates that as the quality of the study decreased there was an increase in pooled success rates. This could be a concern as variability in reporting clinical findings could make interpretation of data difficult or, worse, misleading.
Farzaneh et al. (2004), indicated that the predictors for retreatment success were primarily dependent on the quality of root filling, the quality of post-operative restoration and the absence of pre-operative perforations. Apical periodontitis was a strong predictor, however this was only secondary to other factors.14 Nonsurgical retreatment outcomes are reported to be better in teeth that have failed due to inadequate previous filling and in teeth with no perforation or peri-apical radiolucencies.15 It is important to note that though the indications and skill levels for both the procedures may differ, the final objective is similar. This study reports that when the two treatment procedures were followed up over a four year period, no significant differences were observed. The study however does not indicate the potential causes of failure in the two groups. It should be questioned if the failures were due to a lack of proper case selection, skills level of operator, or other factors. Von arx et al. (2012) reported that five-year prognosis after apical microsurgery was 8% poorer than when assessed at one year following surgery. The study also reported that the interproximal bone levels could also affect the prognosis.16
When analysing the results of this study and others it becomes clear that for assessing the success of either treatments, there is a need for assessing factors or predictors that could affect prognosis and longer follow-up periods.
References
Salehrabi R, Rotstein I . Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod 2004; 30: 846–850.
Peak JD, Hayes SJ, Bryant ST, Dummer PM . The outcome of root canal treatment. A retrospective study within the armed forces (Royal Air Force). Br Dent J 2001; 190: 140–144.
Nair PN, Sjogren U, Krey G, Kahnberg KE, Sundqvist G . Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. J Endod 1990; 16: 580–588.
Ng YL, Mann V, Gulabivala K . Outcome of secondary root canal treatment: a systematic review of the literature. Int Endod J 2008; 41: 1026–1046.
Caliskan MK . Nonsurgical retreatment of teeth with periapical lesions previously managed by either endodontic or surgical intervention. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100: 242–248.
Song M, Jung IY, Lee SJ, Lee CY, Kim E . Prognostic factors for clinical outcomes in endodontic microsurgery: a retrospective study. J Endod 2011; 37: 927–933.
Chong BS, Pitt Ford TR, Hudson MB . A prospective clinical study of Mineral Trioxide Aggregate and IRM when used as root-end filling materials in endodontic surgery. Int Endod J 2003; 36: 520–526.
Dorn SO, Gartner AH . Retrograde filling materials: a retrospective success-failure study of amalgam, EBA, and IRM. J Endod 1990; 16: 391–393.
Ng YL, Mann V, Gulabivala K . A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J 2011; 44: 583–609.
Smith CS, Setchell DJ, Harty FJ . Factors influencing the success of conventional root canal therapy--a five-year retrospective study. Int Endod J 1993; 26: 321–333.
Molven O, Halse A . Success rates for gutta-percha and Kloroperka N-0 root fillings made by undergraduate students: radiographic findings after 10-17 years. Int Endod J 1988; 21: 243–250.
Barbakow FH, Cleaton-Jones P, Friedman D . An evaluation of 566 cases of root canal therapy in general dental practice. 1. Diagnostic criteria and treatment details. J Endod 1980; 6: 456–460.
Barbakow FH, Cleaton-Jones P, Friedman D . An evaluation of 566 cases of root canal therapy in general dental practice. 2. Postoperative observations. J Endod 1980; 6: 485–489.
Farzaneh M, Abitbol S, Friedman S . Treatment outcome in endodontics: the Toronto study. Phases I and II: Orthograde retreatment. J Endod 2004; 30: 627–633.
de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, et al. Treatment outcome in endodontics: the Toronto study--phases 3 and 4: orthograde retreatment. J Endod 2008; 34: 131–137.
von Arx T, Jensen SS, Hanni S, Friedman S . Five-year longitudinal assessment of the prognosis of apical microsurgery. J Endod 2012; 38: 570–579.
Author information
Authors and Affiliations
Additional information
Address for correspondence: E Kim, Microscope Center, Department of Conservative Dentistry and Oral Science Research Center, College of Dentistry, Yonsei University, 50 Yonsei-Ro, Seodaemun-Gu, Seoul 120-752, Korea. E-mail: ANDYENDO@yuhs.ac
Kang M, In Jung H, Song M, Kim SY, Kim HC, Kim E. Outcome of nonsurgical retreatment and endodontic microsurgery: a meta-analysis. Clin Oral Investig 2015; 19: 569–582
Rights and permissions
About this article
Cite this article
George, R. Nonsurgical retreatment vs. endodontic microsurgery: assessing success. Evid Based Dent 16, 82–83 (2015). https://doi.org/10.1038/sj.ebd.6401116
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401116