Abstract
Purpose
Compare the efficacy and survival of trabeculectomy with intraoperative mitomycin-C (MMC) between Asian American and Caucasian patients in the same clinical setting.
Methods
In total, 29 Asian American patients (29 eyes) with trabeculectomies were matched case to case with 29 Caucasian patients (29 eyes) retrospectively. Matching criteria included age, glaucoma subtype, and preoperative intraocular pressure (IOP), gender, surgeon, ocular history, and glaucoma medications. Criteria of success included: (1) Final IOP >5 and <22 mmHg, (2) IOP reduction ≥20%, or final IOP ≤10 mmHg, and (3) without additional glaucoma surgery, loss of light perception, or complication.
Results
Mean follow-up durations of Asian American and Caucasian group were 40.11±22.5 months and 38.8±17.7 months, respectively (P=0.81). At the final visits, IOP decreased from 18.7±6.1 to 10.9±4.0 mmHg (P<0.0001) in the Asian American group, and from 19.0±5.5 to 11.0±3.8 mmHg (P<0.0001) in the Caucasian group. There were no significant differences between the two groups in IOP levels at 6 months, 1 year, and final visits. The probabilities of trabeculectomy survival (continuing to meet definition of success criteria) at 12 and 48 months were 75.9 and 56.6% in the Asian American group and 82.8 and 66.6% in the Caucasian group, respectively. (P=0.46) There were no significant differences for rates of surgical success, failure, complication, vision decrease, hypotony, and cataract development. Patients who had episodes of hypotony had a higher rate of diagnosis of low-tension glaucoma subtype (P=0.02).
Conclusions
In a case-controlled comparison of an intermediate-term follow-up of trabeculectomy with intraoperative MMC, Asian American patients have a similar efficacy and survival probability as Caucasian patients.
Similar content being viewed by others
Introduction
In the latest US census, Asian Americans make up 4.2% of the total US population and their 10-year population growth rate was five times the rate of the total population.1 Asian Americans in the United States are a diverse group of people, composed of different cultural and ethnic backgrounds. Although certain ethnic groups in East Asia, such as the Chinese, Japanese, Vietnamese, and Mongolian, were reported to have a difference in proportion of glaucoma subtypes,2, 3, 4 lower average intraocular pressure (IOP),5, 6, 7, 8, 9 and difference in response to glaucoma surgical management than the Caucasian,10, 11, 12 clinical studies on glaucoma of the American Asian population are few.13, 14
Based on the Medicare claims available in 1999, which categorized patients into different racial groups including Asian, white, and black, the rate of diagnosis of primary open angle glaucoma (POAG) among the Asian Medicare recipients (4.2%) was significantly lower than the rate among the white (5.1%) and black (8.6%) people.4 In addition, a high prevalence of low-tension glaucoma has been reported in the Japanese.2, 5, 15 A lower target IOP may need to be set to decrease the chance of progressive glaucomatous optic neuropathy. From the studies conducted on overseas Asians with POAG, the success rate of trabeculectomy without use of antimetabolite appears to be lower than the success rate in Caucasian.10, 11, 16 Wong et al reported a 3-year success rate of only 36% for trabeculectomy in Asians with POAG, but the rate was higher if antimetabolite was used and approached the rate observed in Caucasians reported in the western studies.12, 16, 17, 18, 19, 20 However, comparison of glaucoma surgical management in Asian and Caucasian populations is difficult because of the different surgical techniques, ophthalmic practice and medical care environments, and glaucoma managements in different countries.
The purpose of this study was to evaluate the efficacy of trabeculectomy with intraoperative application of mitomycin-C (MMC) in Asian American patients compared with Caucasian patients. We conducted a retrospective case-controlled comparison between Asian American and Caucasian glaucoma patients who had received a trabeculectomy with intraoperative MMC at the same clinic by the same surgeons. These patients were on maximal tolerated medical therapy and were judged to require additional IOP reduction to prevent further progression of functional visual loss.
Materials and methods
This study was approved by the Institutional Review Board of the University of California, Los Angeles. Trabeculectomies performed at our institute by two surgeons (SKL, JC) from July 1997 to April 2003 (69 months) were retrospectively reviewed. Patients who were Asian American in ethnicity, older than 30 years of age, and had at least 1 year of follow-up at our institute after the surgery were included. Patients' ethnicities were identified based on the ethnicity recorded in the medical records.
Preoperative data were collected from the records of the patients within 3 months before the operation, and included age, gender, race, IOP, visual acuity, slit-lamp and fundus examination findings, specific diagnosis of glaucoma subtype, and other ocular history. The enrolled Asian American patients were matched case by case with Caucasian patients with trabeculectomy and intraoperative MMC application during the same study period. Primary matching criteria included age (difference within 20% of the age), glaucoma subtype, and preoperative IOP (difference within 20% of the IOP). Secondary matching criteria included gender, surgeon who performed the operation, ocular history, and preoperative number of glaucoma medications (difference within one medication).
To avoid a potential bias in abstracting the Caucasian patients to match the Asian American patients who had trabeculectomy and intraoperative MMC, two investigators (SKL, SM) were involved in the matching process. One investigator (SM) was responsible for abstracting the Caucasian patient cases based on the relevant matching criteria, and the other investigator (SKL) was responsible for selecting the best-matched control case when several cases were available.
The surgeries were performed by two surgeons (SKL, JC) using the same technique. A superior limbal-based conjunctival flap was created. A 4.0 × 3.0 mm scleral flap was outlined with a surgical blade at 12 : 00 position. Pieces of cut weck-cel soaked in MMC of concentration 0.3 mg/ml were placed under the Tenon capsule and conjunctiva on the sclera at the outlined flap area for 1 min. The weck-cel pieces were removed followed by thorough irrigation of the area exposed to MMC with 30 cc of balanced salt solution. Then, a partial-thickness 4.0 × 3.0 mm rectangular sclera flap was dissected. A block of trabecular section was removed anterior to the scleral spur by a Kelly punch or number 75-microsurgery blade, and a peripheral iridectomy was performed. The scleral flap was sutured at the two corners of the scleral flap with interrupted 10–0 nylon sutures to ensure a slight egression of aqueous yet maintain adequate anterior chamber's depth. Finally, the conjunctiva and Tenon capsule were sutured with a continuous 9–0 polyglactin suture (Vicryl®).
Postoperatively, patients received a 4-weeks tapering dose of 1% prednisolone acetate ophthalmic drop starting with four times daily. Suture lysis was performed with argon laser for inadequate IOP control or a low filtering bleb between 1 and 4 weeks after the surgery. The target IOP before laser suture lysis or the addition of ocular hypotensive therapy was low teens or less, with the goal of preventing further progression of functional visual loss. Subconjunctival injection or needling of the bleb with 5-fluorouracil (5-FU) was performed to maintain the function of the filtering bleb according to the discretion of surgeons.
Postoperative data were collected from the records for visits that fell into six different postoperative intervals. The six intervals were set as follows: Visit 1 as 0–2 days after operation, Visit 2 as 5–10 days after operation, Visit 3 as 20–40 days after operation, Visit 4 as 60–120 days after operation, Visit 5 as 121–240 days after operation, and Visit 6 as 241–480 days after operation. Postoperative data on patients who had follow-up beyond 1 year were also recorded up to 5 years. Postoperative data collected from the visits included vision, IOP, slit-lamp and fundus examination findings, number of glaucoma medications used, and surgical complications.
Criteria of success included: (1) IOP reduction at least 20% of the preoperative IOP, or final IOP equaled 10 mmHg or less, and (2) final IOP >5 mmHg and <22 mmHg, and (3) without additional glaucoma surgery, loss of light perception, or devastating complication. Devastating complications were defined as complications that might result in a significant decrease of vision or required surgical correction, including, but not limited to, large choroidal effusion, suprachoroidal haemorrhage, retinal detachment, vitreous haemorrhage, or endophthalmitis. A complete success required no glaucoma medication to achieve the final IOP control, and qualified success required the use of glaucoma medication(s).
Surgical failure was defined as IOP reduction less than 20% of the preoperative IOP, or final IOP ≤5 mmHg or ≥22 mmHg, progression to no light perception, a need for additional glaucoma surgery, or occurrence of a devastating complication. In those cases categorized as failures, the IOPs, visual acuities, and glaucoma medication used were recorded on the dates when further intervention was recommended or a devastating complication occurred. Hypotony was defined as IOP ≤5 mmHg beyond Visit 3 (1 month follow-up), development of hypotony maculopathy, or requirement of surgical intervention. Decrease of vision was defined as more than one line of decrease of best-corrected vision as measured with Snellen acuity 1 year after trabeculectomy. The 1-year follow-up visit was chosen as a reference for comparison because of unequal lengths of follow-up among patients.
Statistical analysis was performed with SPSS for Windows (SPSS, Chicago, IL, USA). Unpaired Student's t-test and χ2 analysis were performed to compare the demographic data and the IOPs of different visits between the Asian American group and Caucasian group. Paired Student's t-test was used to compare the preoperative and postoperative values of IOP of each of the two groups. Rates of surgical success and failure, visual acuity decrease, and hypotony were analysed with χ2 test. Kaplan–Meier survival analysis for success (complete and qualified success) was calculated with the Log rank test. A two-tailed P≤0.05 was considered statistically significant. The detectable differences of IOP level between the Asian American group and Caucasian group were calculated at a power of 80% with α=0.05.
Results
In all, 37 Asian American patients who had trabeculectomies with intraoperative MMC application were considered for participation in the study. Eight patients had less than 1 year of follow-up and so were excluded, thus allowing for 29 Asian American patients (29 eyes) to be enrolled. The 29 patients enrolled were successfully matched with 29 Caucasian patients with trabeculectomy and intraoperative MMC application on the basis of age, glaucoma subtype, and the preoperative IOP. Secondary matching criteria included gender, surgeon who performed the operation, and ocular history, with partial success on matching. In each group, 25 of 29 patients (86.2%) were diagnosed with POAG. Table 1 summarizes the demographic characteristics of the Asian American and Caucasian patients. There were 14 Chinese patients (48.3%), 10 Japanese patients (34.5%), four Korean patients (13.8%), and one Filipino patient (3.4%) in the Asian American group. The differences in age, sex, glaucoma subtype, previous ocular surgery, length of follow-up, preoperative IOP, and number of glaucoma medications were not statistically significant between the two groups.
There were statistically significant decreases of IOP for both the Asian American group and Caucasian group after a trabeculectomy with intraoperative MMC application. At 1 year after the surgery, IOP decreased from 18.7±6.1 to 10.9±3.9 mmHg (P<0.0001) in the Asian American group, and from 19.0±5.5 to 10.7±3.6 mmHg (P<0.0001) in the Caucasian group. At the final visits, IOP decreased to 10.9±4.0 mmHg in the Asian American group (P<0.0001) and 11.0±3.8 mmHg in the Caucasian group (P<0.0001). Table 2 and Figure 1 represents the comparison of the IOPs between the two groups in each follow-up visit. There was no significant difference between the two groups in postoperative IOP levels except for Visit 3 (20–40 days after trabeculectomy, P=0.05). The current study had an 80% power to detect a difference of 2.7 mmHg between the two groups at 1 year follow-up at a α=0.05.
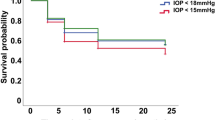
The probability of trabeculectomy survival (IOP reduction ≥20% or final IOP≤10 mmHg; and final IOP was >5 and <22 mmHg, without additional glaucoma surgery, loss of light perception, or devastating complication, with or without medication) at 12, 36, and 48 months was 75.9, 56.6, and 56.6%, respectively, in the Asian American group and 82.8, 74.9, and 66.6%, respectively, in the Caucasian group. (Figure 2, P=0.46 Log rank test) No significant difference were observed between the two groups in regards to the rates of complete surgical success, qualified surgical success, surgical failure, postoperative requirement of laser suture lysis or subconjunctival injection of 5-FU, decrease of best-corrected visual acuity, and hypotony (Table 3, Figure 3). The current study had an 80% power to detect a difference of 50% of survival rate (or relative risk of 0.33) between the two groups based on the survival rate of 75% at 36 months in the Caucasian group.
Results of Kaplan–Meier life-table analysis. (Log rank significance=0.54) Criteria of success: (1) IOP reduction at least 20% of the preoperative IOP, or final IOP 10 mmHg or less, (2) final IOP was greater than 5 mmHg and less then 22 mmHg, (3) without additional glaucoma surgery, loss of light perception, or devastating complication, (4) with or without antiglaucoma medication(s).
Table 3 summaries the reasons for surgical failure in each group. Five patients in the Asian American group and three patients in the Caucasian group required additional glaucoma surgery for glaucoma control. Of the total of eight patients of the two groups, four received Ahmed glaucoma valve implantation and four had repeated trabeculectomy with intraoperative MMC application. Additional glaucoma operations were performed at a mean of 18.8±8.8 months after the initial trabeculectomy.
Complication rates of trabeculectomy were relatively low in both the Asian American group (one bleb leakage) and Caucasian group (one bleb leakage, one hypotony maculopathy, and one large choroidal effusion). There was no significant difference in hypotony rates between the two groups, but the Caucasian group only had two patients that developed hypotony (IOP≤5 mmHg beyond 1-month follow-up). One of the two patients had a bleb leak and required a revision. The other patient had hypotony maculopathy and required revision. In the Asian group, five patients developed IOP<5 mmHg beyond 1-month follow-up. One patient required reformation of the anterior chamber with viscoelastic material. The intervention was successful and patient achieved good pressure control without glaucoma medication. Another patient had bleb leak and required a revision. The other three patients had episodes of IOP between 4–5 mmHg beyond 1-month follow-up but required no additional intervention. Of these seven patients from the two groups that had episodes of postoperative hypotony, three patients (42.9%) had POAG with possible low-tension glaucoma subtype. In the contrary, only three patients in the rest of the 51 patients (5.9%) without episode of postoperative hypotony had low-tension glaucoma subtype (P=0.02).
Sixteen (55.2%) of the 29 Asian American patients and 19 (65.5%) of the 29 Caucasian patients were phakic prior to the trabeculectomy. Of the 35 phakic patients with natural lens (both Asian American and Caucasian), 15 (42.9%) had development or increase of cataract, or required cataract surgery. Seven (43.8%) of the 16 Asian American patients and 8 (42.1%) of the 19 Caucasian patients had development or increase of cataract, or required cataract surgery. (P=0.81) Cataract operations were performed in an average of 11.7±6.6 months (range 4–24 months) after trabeculectomy.
Decrease of vision was defined as more than one line of decrease of best-corrected vision as measured with Snellen acuity 1 year after trabeculectomy. Among the four patients with decrease of best-corrected visual acuity more than one line in the Asian American group, three patients had pseudophakia and one patient was phakic. One Asian American patient developed a central retinal vein occlusion 5 weeks after trabeculectomy. The severe decrease of vision in this patient was thought to be unrelated to the trabeculectomy and this patient was not included in the analysis of visual acuity decrease. In the Caucasian group, three of the five patients with visual acuity decrease had pseudophakia and two patients had natural lens. One of the five patients had a large choroidal effusion that required surgical drainage and another patient had hypotony maculopathy that required a revision of the trabeculectomy.
Although 86.2% of patients included in our study had primary open angle and no history of previous glaucoma surgery, it is possible that the small proportion of patients with other glaucoma subtypes or a history of previous glaucoma surgery could affect the survival analysis. Thus, we reanalysed our data using only Asian Americans and Caucasians who had POAG and no previous history of glaucoma surgeries. Six patients in the Asian American group and seven patients in the Caucasian group had glaucoma subtypes other than POAG or a history of previous glaucoma surgeries (trabeculectomies) and thus were excluded from the reanalysis. The results of the comparison between the remaining 23 Asian American patients (eyes) and 22 Caucasian patients (eyes) were similar to those of the larger sample. At 1 year of follow-up, IOP decreased from 17.0±5.4 mmHg to 11.0±3.9 mmHg (P<0.0001) in the Asian American group and from 18.9±5.4 mmHg to 10.3±3.3 mmHg (P<0.0001) in the Caucasian group. At the final visit, IOP decreased to 10.7±3.6 mmHg in the Asian American group and 11.0±3.3 in the Caucasian group. There were no significant differences between the two groups in IOP levels at any follow-up visits. The probabilities of trabeculectomy survival at 12, 36, and 48 months were 73.9, 64.1, and 64.1% in the Asian American group and 81.8, 81.8, and 70.1% in the Caucasian group, respectively. (P=0.40) There were no significant differences for rates of surgical success, failure, complications, vision decrease, requirement of postoperative laser suture lysis or subconjunctival injection of 5-FU, and hypotony.
Discussion
Glaucoma surgery has been reported to have a lower success rate in black patients who had advanced glaucoma uncontrolled with medical therapy compared to Caucasian patients.20, 21, 22, 23 Studies on Asian patients in South East Asia have also reported a lower success rate of trabeculectomy than the success rate reported on Caucasian populations in the western literature.10, 11, 16 However, the survival of trabeculectomy improved with use of intraoperative antimetabolite as adjuvant, and the more liberal use of intraoperative antimetabolites was advocated in the Asian population.11, 12 Comparisons of survival of trabeculectomy performed in different populations were limited by the different clinical settings in various countries, such as surgical techniques, length of follow-up, and criteria for success. In the present study, the efficacy of trabeculectomy with intraoperative MMC application in Asian American patients and Caucasian patients was case-matched and compared in the same clinical setting, with surgery and follow-up performed by the same surgeons, and using the same criteria for surgical success. There were no significant differences between the Asian American and Caucasian groups in regards to the cumulative survival, and rates of surgical success, failure, complication, hypotony, and vision decrease. The probabilities of trabeculectomy survival at 1 year and 4 years were 75.9 and 56.6% for the Asian American group and 82.8 and 66.6% for the Caucasian group, respectively. When the comparison was limited to eyes with POAG and without previous glaucoma surgery, the probability of trabeculectomy survival at 4 years improved to 64.1% for the Asian American group and 70.1% in the Caucasian group.
The survival probabilities of trabeculectomy of Asian American patients in the present study were similar to the survival probabilities reported in some studies on the Asian population in the literature.12, 24 Wong et al12 reported the trabeculectomy survival with intraoperative 5-FU application to be 75.8% at 1 year and 65.8% at 3 years for the Asian patients in Singapore. The definition of success of that study was IOP<22 mmHg without additional medication or surgery. In the present study, additional reduction of IOP by 20% from preoperative IOP was required to qualify a success. This criterion was used because the patients in our tertiary centre had moderate or advanced stage of glaucoma and their IOPs might already be less than 22 mmHg on medical therapy. Both groups had a mean preoperative IOP in the high teens (18.7±6.1 mmHg in the Asian American group and 19.0±5.5 mmHg in the Caucasian group), but an aggressive lowering of IOP to prevent vision loss was required. In addition, 48% of the Asian American patients and 41% of the Caucasian patients in the present study had previous intraocular surgery, which may have an adverse effect on the survival of trabeculectomy. The Asian American group of the present study consisted largely of Chinese and Japanese Americans. In a sample of Japanese patients with a mean follow-up of 6 years after trabeculectomy with intraoperative and postoperative subconjunctival injection of 5-FU, Uchida et al24 reported a 6-year survival rate of 51.6% with the definition of IOP<16 mmHg regardless of medications plus 30% or more reduction of IOP. That study has a longer follow-up than the present study. From the Kaplan–Meier life-table analysis curve presented in that study, the 1-year and 3-years survival rates were approximately 75 and 55%, respectively. The rates were similar to those of the present study. The consistency is reasonable since 24 of the 29 Asian American patients (82.8%) of the present study were either Chinese American patients or Japanese American patients, and there was a similarity of criteria used to define a surgical success. Although a history of previous intraocular surgery may render the survival of trabeculectomy lower, the use of intraoperative application of a stronger antimetabolite, such as MMC, may have increased the survival rate compared to 5-FU.25, 26, 27
In the present study, mean IOP reduction achieved after trabeculectomy with intraoperative MMC application was more than 40% at 1 year and 4 years in both the Asian American group and Caucasian group. Patients in the combined Asian American and Caucasian group that had episodes of hypotony had a higher rate of diagnosis of low-tension glaucoma subtype then the rest of the patients that did not have episode of hypotony. In an unmasked study, those patients with low-tension glaucoma subtype that required a very low IOP (for instance, 10 mmHg or lower) to preserve the visual function might be surgically managed more aggressively and result in a higher rate of hypotony. Possible surgical and postsurgical steps that can provide a lower postoperative IOP include looser suturing of the scleral flap to allow higher filtration, higher concentration and longer duration of antimetabolite application on the area of the scleral flap, and earlier argon suture lysis. Although the same concentration of 0.3 mg/ml of MMC and duration of 1 min of application, same surgical technique and suture tightness in closing the scleral flap, and same criteria and timing of suture lysis were used in all patients, the biological response varies individually. In addition, the crossover effect of antiglaucoma medications required for the contralateral eyes cannot be controlled for.
The major complications experienced in the Asian American and Caucasian patients of the present study were two patients with bleb leakage, one with hypotony maculopathy, and one with a large choroidal effusion. The lower rate of complication of the present study may be explained by the inclusion of only visually significant complications in the analysis. Although a very small amount of hyphaema or small peripheral choroidal effusions were occasionally present in some eyes after trabeculectomy, they resolved spontaneously and were not considered a surgical complication in the present study.
Cataract development or progression is a common cause of visual acuity decrease after trabeculectomy. There was an increased risk of 78% of cataract formation reported by the Advanced Glaucoma Intervention Study.28 The rate of cataract formation or progression varies in different studies. In Japanese patients who had undergone a trabeculectomy, a rate of 20% of cataract progression in a mean follow-up of 6 years was reported.24 The current study had an overall rate of 25.9% of cataract formation, progression, or cataract operation required. However, if only phakic patients were considered, the rate increased to 42.9%, which falls within the range of cataract formation or progression reported in the literature.28, 29 There was no significant difference between the rates of cataract development, progression, or cataract operation after trabeculectomy between the Asian American and Caucasian groups. It is possible that both the Asian Americans and Caucasian patients in our tertiary care setting were more receptive to the option of cataract surgery.
A limitation of the current study is that we were unable to detect differences of IOP<2.7 mmHg or survival rate of smaller than 50% between the two groups at a power of 80%, and the retrospective design of the study that unknown differences between the two groups may exist. However, the case-controlled study design did allow us to control for confounding factors, such as clinical setting, clinical indication for surgery, and surgical technique, in comparing the efficacy of trabeculectomy in two populations. In an intermediate period of follow-up, trabeculectomy with intraoperative MMC application in Asian American patients appeared to have similar efficacy and probability of survival as Caucasian patients.
References
Barnes JS, Bennett CE . The Asian population: 2000, Census 2000 brief. United States Census 2000, US Department of Commerce, Economics and Statistic Administration. US Census Bureau: Washington, DC, February 2000.
Congdon N, Wang F, Tielsch JM . Issues in the epidemiology and population-based screening of primary angle-closure glaucoma. Surv Ophthalmol 1992; 36 (6): 411–423.
Foster PJ, Johnson GJ . Glaucoma in China: how big is the problem? Br J Ophthalmol 2001; 85 (11): 1277–1282.
Law SK . Asian Americans: glaucoma. Int Ophthalmol Clin 2003; 43 (4): 133–149.
Shiose Y, Kitazawa Y, Tsukahara S, Akamatsu T, Mizokami K, Futa R et al. Epidemiology of glaucoma in Japan—a nationwide glaucoma survey. Jpn J Ophthalmol 1991; 35 (2): 133–155.
Congdon NG, Quigley HA, Hung PT, Wang TH, Ho TC . Screening techniques for angle-closure glaucoma in rural Taiwan. Acta Ophthalmol Scand 1996; 74 (2): 113–119.
Hu CN . An epidemiologic study of glaucoma in Shunyi County, Beijing. Zhonghua Yan Ke Za Zhi. (Chin J Ophthalmol) 1989; 25: 115–119.
Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ . Glaucoma in Mongolia. A population-based survey in Hovsgol province, northern Mongolia. Arch Ophthalmol 1996; 114 (10): 1235–1241.
Foster PJ, Wong JS, Wong E, Chen FG, Machin D, Chew PT . Accuracy of clinical estimates of intraocular pressure in Chinese eyes. Ophthalmology 2000; 107 (10): 1816–1821.
Tan C, Chew PT, Lum WL, Chee C . Trabeculectomy—success rates in a Singapore hospital. Singapore Med J 1996; 37 (5): 505–507.
Hooi ST, Hooi SH . Trabeculectomy outcomes in a Malaysian general hospital. Med J Malaysia 2003; 58 (4): 565–578.
Wong JS, Yip L, Tan C, Chew P . Trabeculectomy survival with and without intra-operative 5-fluorouracil application in an Asian population. Aust N Z J Ophthalmol 1998; 26 (4): 283–288.
Nguyen N, Mora JS, Gaffney MM, Ma AS, Wong PC, Iwach AG et al. A high prevalence of occludable angles in a Vietnamese population. Ophthalmology 1996; 103 (9): 1426–1431.
Rosman M, Aung T, Ang LP, Chew PT, Liebmann JM, Ritch R . Chronic angle-closure with glaucomatous damage: long-term clinical course in a North American population and comparison with an Asian population. Ophthalmology 2002; 109 (12): 2227–2231.
Kitazawa Y . Open-angle glaucoma in Japan. J Glaucoma 2001; 10 (5 Suppl 1): S5–S6.
Ehrnrooth P, Lehto I, Puska P, Laatikainen L . Long-term outcome of trabeculectomy in terms of intraocular pressure. Acta Ophthalmol Scand 2002; 80 (3): 267–271.
Suzuki R, Dickens CJ, Iwach AG, Hoskins Jr HD, Hetherington Jr J, Juster RP et al. Long-term follow-up of initially successful trabeculectomy with 5-fluorouracil injections. Ophthalmology 2002; 109 (10): 1921–1924.
Costa VP, Comegno PE, Vasconcelos JP, Malta RF, Jose NK . Low-dose mitomycin C trabeculectomy in patients with advanced glaucoma. J Glaucoma 1996; 5 (3): 193–199.
Casson R, Rahman R, Salmon JF . Long term results and complications of trabeculectomy augmented with low dose mitomycin C in patients at risk for filtration failure. Br J Ophthalmol 2001; 85 (6): 686–688.
Scott IU, Greenfield DS, Schiffman J et al. Outcomes of primary trabeculectomy with the use of adjunctive mitomycin. Arch Ophthalmol 1998; 116 (3): 286–291.
AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 4. Comparison of treatment outcomes within race. Seven-year results. Ophthalmology 1998; 105 (7): 1146–1164.
AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 9. Comparison of glaucoma outcomes in black and white patients within treatment groups. Am J Ophthalmol 2001; 132 (3): 311–320.
Ederer F, Gaasterland DA, Dally LG, Kim J, VanVeldhuisen PC, Blackwell B et al. AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 13. Comparison of treatment outcomes within race: 10-year results. Ophthalmology 2004; 111 (4): 651–664.
Uchida S, Suzuki Y, Araie M, Shigeeda T, Hara T, Shirato S . Long-term follow-up of initial 5-fluorouracil trabeculectomy in primary open-angle glaucoma in Japanese patients. J Glaucoma 2001; 10 (6): 458–465.
Kitazawa Y, Kawase K, Matsushita H, Minobe M . Trabeculectomy with mitomycin. A comparative study with fluorouracil. Arch Ophthalmol 1991; 109 (12): 1693–1698.
Skuta GL, Beeson CC, Higginbotham EJ, Lichter PR, Musch DC, Bergstrom TJ et al. Intraoperative mitomycin vs postoperative 5-fluorouracil in high-risk glaucoma filtering surgery. Ophthalmology 1992; 99 (3): 438–444.
Katz GJ, Higginbotham EJ, Lichter PR, Skuta GL, Musch DC, Bergstrom TJ et al. Mitomycin C vs 5-fluorouracil in high-risk glaucoma filtering surgery. Extended follow-up. Ophthalmology 1995; 102 (9): 1263–1269.
AGIS (Advanced Glaucoma Intervention Study) Investigators. The Advanced Glaucoma Intervention Study: 8. Risk of cataract formation after trabeculectomy. Arch Ophthalmol 2001; 119 (12): 1771–1779.
Parc CE, Johnson DH, Oliver JE, Hattenhauer MG, Hodge DO . The long-term outcome of glaucoma filtration surgery. Am J Ophthalmol 2001; 132 (1): 27–35.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr SK Law has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis No author has a commercial or proprietary interest in the development or marketing of any of the products or devices mentioned in the study
Rights and permissions
About this article
Cite this article
Law, S., Modjtahedi, S., Mansury, A. et al. Intermediate-term comparison of trabeculectomy with intraoperative mitomycin-C between Asian American and Caucasian glaucoma patients: a case-controlled comparison. Eye 21, 71–78 (2007). https://doi.org/10.1038/sj.eye.6702128
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702128
Keywords
This article is cited by
-
The Japan Glaucoma Society guidelines for glaucoma 5th edition
Japanese Journal of Ophthalmology (2023)
-
Does TRABECULECTOMY meet the 10-10-10 challenge in PACG, POAG, JOAG and Secondary glaucomas?
International Ophthalmology (2020)