Abstract
Aim
To evaluate the success rate and complications associated with deep sclerectomy with mitomycin C (MMC) and a reticulated hyaluronic acid implant in previously failed trabeculectomy.
Methods
This prospective study included 20 eyes with a previously failed trabeculectomy, which were treated with deep sclerectomy with 0.2 mg/ml MMC application under the conjunctiva and superficial scleral flap. Intraocular pressure (IOP), glaucoma medications, visual acuity, and complications were recorded preoperatively and 1 day, 1 week, and 1, 3, 6, and 12 months postoperatively.
Results
The mean preoperative IOP was 25.8±7.3 mmHg; the IOP significantly decreased to 14.6±3.2 mmHg 1 year postoperative. At each interval, the mean IOP was significantly lower than preoperatively (P=0.000). At 1 year, the complete success rate (IOP≤21 mmHg untreated) was 65% and the qualified success rate (IOP≤21 mmHg with and without medication) was 100%. 12 patients (60%) achieved an IOP≤15 mmHg with and without medication. No shallow or flat anterior chamber, endophthalmitis, or leakage developed.
Conclusions
These data suggest that deep sclerectomy augmented with MMC is a safe surgical procedure that decreases IOP in eyes with a previously failed trabeculectomy.
Similar content being viewed by others
Introduction
Trabeculectomy is the most common surgery for glaucoma. However, the probability of successful control of intraocular pressure (IOP) and disease progression decreases over time despite an initially successful trabeculectomy.1, 2
When the first trabeculectomy fails, several surgical options are available, such as slit-lamp needle revision, repeat trabeculectomy with antimetabolites, or an aqueous shunt procedure. A previously failed filtering surgery is a known risk factor for surgical failure.
Mitomycin C (MMC) is a potent antineoplastic antibiotic agent used to prolong bleb survival in these high-risk eyes.3, 4, 5, 6, 7
As an initial surgery, deep sclerectomy may offer success rates comparable to trabeculectomy and minimize the risk of postoperative complications.8, 9, 10, 11, 12, 13
Recently, the adjunctive use of MMC in deep sclerectomy has been reported to be safe and to improve the surgical results.12, 14, 15, 16
Although studies have been performed on the efficacy of trabeculectomy with MMC in eyes that underwent previous filtering procedures,4, 5, 6, 7 to the best of our knowledge, no study has been published on the success rate and safety of deep sclerectomy augmented with MMC in these eyes.
We designed a prospective clinical study to evaluate the efficacy of deep sclerectomy with intraoperative 0.02% MMC application under the conjunctival and superficial scleral flap and a reticulated hyaluronic acid implant in eyes with a previously failed trabeculectomy.
Methods
Patients
We included 20 consecutive eyes of 20 patients who had undergone a previously failed trabeculectomy isolated or combined with an uneventful phacoemulsification and were admitted for planned deep sclerectomy with intraoperative MMC application between April 2003 and April 2004 at the Glaucoma Unit of Hospital Ramón y Cajal in Madrid. All patients had a previous failed trabeculectomy with no visible filtration bleb and uncontrolled IOP greater than 21 mmHg despite maximally tolerated medications.7
Patients were excluded if they had angle closure, neovascular, traumatic, uveitic, or juvenile glaucoma, had undergone a penetrating keratoplasty, or were aphakic. All patients had at least 12 months of follow-up after deep sclerectomy. Institutional Review Board Committee approval was obtained and all patients provided informed consent for surgery.
The data prospectively recorded were age at the time of deep sclerectomy, gender, eye, the time since the first trabeculectomy, IOP (measured by Goldmann tonometry at the visit performed 1 week before surgery), number of glaucoma medications used, and best-corrected visual acuity (VA) before surgery. Patients were examined 1 day, 1 week, and 1, 3, 6, and 12 months after surgery (and more often when necessary). The VA, biomicroscopic examination, IOP, postoperative complications, and the number of glaucoma medications were recorded at each follow-up visit.
The use of glaucoma medications was reported as the number of drugs taken, with no differentiation as to the type or the frequency of medication use. Fixed combinations of two drugs were considered to be two glaucoma medications.
A complete success was defined as an IOP of 21 mmHg or less without medications, whereas a qualified success meant that antiglaucoma medications were required to achieve an IOP of 21 mmHg or less.
A VA change was considered significant if a change of two or more lines or one low-vision category (ie, hand motion to light perception) was observed after deep sclerectomy.
Surgical technique
All surgical procedures were performed by one of the authors. In all cases, retrobulbar anaesthesia was used. We dissected a fornix-based conjunctival flap and avoided the old filtering site. A superior temporal or nasal filtration site was selected intraoperatively by testing the conjunctival mobility.
A one-third scleral thickness superficial flap (5.0 × 5.0 mm) was created at least 1.0 mm into the clear cornea. Several surgical sponges soaked with MMC (0.2 mg/ml) were used under the conjunctiva and scleral flaps for 2–3 min in eyes with one or two previously failed trabeculectomy, respectively.6 After the sponges were removed, the entire area was irrigated copiously with balanced salt solution. A second triangle of deep sclera was dissected, Schlemm's canal deroofed, and a trabeculo-Descemet membrane (TDM) was created.
The juxtacanalicular trabeculum and Schlemm's endothelium were removed using small blunt forceps (Huco Vision S.A., Saint-Blaise, Switzerland) (ab externo trabeculectomy) when it was possible, and a reticulated hyaluronic acid implant (SKGel 3.5, Corneal Laboratories, Paris, France) was placed in the scleral bed. A deep scleral flap was excised and the superficial scleral flap sutured with two to four interrupted nylon 10/0 buried sutures. No case had to be converted to a trabeculectomy because of perforation of the TDM.
The postoperative treatment included a combination of dexamethasone and tobramycin eight times daily for 2 weeks. The dosage was tapered by one drop weekly until discontinuation after 12 weeks. When the vessel density increased or flattening occurred, we intensified the postoperative anti-inflammatory treatment (prednisolone acetate every 1–2 h during waking hours).
When the filtration through the TDM was considered to be insufficient because of elevated IOP, a goniopuncture was performed with the neodymium (Nd):YAG laser in the anterior thinnest portion of the TDM.
Statistical analysis
The IOPs were compared longitudinally using the two-tailed Student's t-test. The number of glaucoma medications was compared using the Wilcoxon signed-rank test. A statistics program (SPSS 10.0 for Windows, SPSS Inc., Chicago, IL, USA) was used for all analyses. A P-value of 0.05 or less was considered the level of significance.
Results
20 eyes of 20 patients (10 men, 10 women) participated in this study. Table 1 shows the demographic data. Patient ages ranged from 56 to 99 years. The mean follow-up was 14.9±3.2 months.
The most frequent preoperative diagnosis was primary open-angle glaucoma. The time to failure from the first trabeculectomy ranged from 2 to 15 years (8.3±4.8). Most patients (70%) had only one previous failed filtering surgery. In six eyes (30%), a combined phacotrabeculectomy surgery with MMC had been performed after the first failed trabeculectomy.
Most eyes (90%) were pseudophakic with an acrylic foldable posterior chamber intraocular lens in the capsular bag.
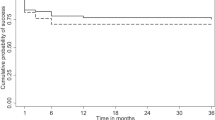
Figure 1 shows the mean IOPs before and after deep sclerectomy at each follow-up visit. The mean preoperative IOP was 25.8±7.3 mmHg. At 12 months, the mean IOP decreased to 14.6±3.2 mmHg (P=0.000).
At 12 months, the complete success rate, defined as an IOP of 21 mmHg or less without medications, was 65% and the qualified success rate, defined as an IOP <21 mmHg with and without medication, was 100%. Eight patients (40%) achieved an IOP≤15 mmHg without medication and 12 cases (60%) with or without medication.
At 1 year postoperatively, the mean IOP was 14.5±3.3 and 14.8±3.5 mmHg in eyes using MMC for 2 and 3 min, respectively (P=0.846).
The mean postoperative number of medications used decreased significantly from 2.3±0.8 to 0.4±0.50 postoperatively (Wilcoxon's signed-rank test, P=0.000) (Table 2). At 12 months, topical medical treatment was necessary in seven cases (35%) to obtain target IOP.
Postoperative Nd:YAG goniopuncture was performed in eight eyes (40%). The mean number of laser pulses used was 4.3 (range: 1–8) and the mean laser energy used was 3.2 mJ (range: 2–4 mJ). The mean time between deep sclerectomy and goniopuncture was 4.2±1.7 months. Four (50%) of them were performed early after surgery (1–3 months postoperatively). The mean IOP decrease was 6.4 mmHg immediately after laser treatment.
The VA in each eye at the last follow-up visit was compared with the preoperative level. A VA change was considered significant if a change of two or more lines or one low-vision category (ie, hand motion to light perception) was observed. The VA was unchanged in 19 eyes (95%). One eye with very advanced visual field damage had a VA decrease from 20/400 to hand motion.
Postoperative complications included development of one postoperative hyphema and one choroidal detachment that resolved spontaneously. No shallow or flat anterior chamber, endophthalmitis, or leakage was observed.
Discussion
Since 1967, trabeculectomy has become the standard drainage procedure for most cases of uncontrolled primary glaucoma. However, surgical failure can occur over time.1, 2 The reported incidence of failure varies according to the length of the follow-up and the type of glaucoma being treated. The most common cause of filtration failure is scarring at the site of filtration bleb months or years after surgery.
Many variables affect the outcome of glaucoma filtering surgery. A prior failed trabeculectomy is one known risk factor for surgical failure. The introduction of antimetabolites has increased the success rate of repeat trabeculectomy. MMC decreases fibroblast replication both in vivo and in animal models, and it appears to be effective in reducing the relative risk of failure of trabeculectomy both in eyes at high risk of failure and those undergoing surgery for the first time.3, 4, 5, 6, 7
The presence of more than one preoperative ocular risk factor affects the surgical success of MMC-augmented trabeculectomy in high-risk cases.17 Considering this, eyes with other risk factors, such as neovascular, traumatic, juvenile, uveitic glaucoma, penetrating keratoplasty or aphakia, were excluded from this study.
Deep sclerectomy is a nonpenetrating filtering procedure that provides IOP control comparable to that of as trabeculectomy in the initial ocular surgery with fewer complications.8, 9, 10, 11, 12, 13
The use of intraoperative MMC during deep sclerectomy significantly reduced the postoperative IOP and increased the success rate of the procedure and the probability of achieving lower target IOPs.12, 14, 15, 16 However, to the best of our knowledge, no other study has reported data about deep sclerectomy augmented with MMC in eyes with a previously failed trabeculectomy.
Most surgeons individualize the MMC dosage according to the risk profile of each patient for surgical failure.5, 6 In this study, 0.2 mg/ml MMC was used for 2 min in patients with one previous failed trabeculectomy and for 3 min in eyes with two previously failed surgeries. In our study, we have not found any statistically significant difference in mean IOP between exposure time subgroups (P=0.846).
The site of MMC administration is a matter of considerable debate. In our study, we applied MMC under the conjunctiva and under the first scleral flap. Several studies have suggested that the application of MCC under both flaps during trabeculectomy provides the greatest IOP reduction.7, 18
The larger the bleb area is, the better is the prognosis for success. A large area prevents the development of a ring of scar tissue, which restricts flow and promotes the development of a raised avascular bleb and late leakage. To maintain that potential space, MMC was applied over the largest possible area with multiple sponges.19
A deep sclerectomy in eyes that underwent a previous surgery differs in several ways from primary deep sclerectomy. The superior quadrant is scarred, which makes it necessary to choose other locations. A superotemporal filtration site is better than a superonasal site, because the latter is more likely to cause symptoms. However, in our series, nine cases required a filtering site in the superonasal quadrant, because the temporal quadrant was scarred or the anterior chamber angle closed. In addition, scarring prevented us from performing a trabeculectomy ab externo in half of the cases (Table 1). No case of TDM macroperforation occurred. An intraoperative microperforation of the TDM without iris prolapse was observed in two eyes.
In our study, all patients achieved an IOP of 21 mmHg or less with or without medication, and 65% of these achieved this level without treatment 1 year postoperatively. Moreover, 35% achieved an IOP of 15 mmHg or less without medication.
Perkins et al5 analysed 68 patients who underwent trabeculectomy with MMC, including 57% of patients who had undergone a previous ocular surgery. In 59% of eyes, the IOP remained 21 mmHg or less after trabeculectomy without glaucoma medications at the 2-year follow-up examination.
Stone et al6 published a retrospective review of 57 patients who underwent trabeculectomy using MMC with exposure times titrated from 1 to 5 min based on risk factors for trabeculectomy failure. They included 14 cases (24.6%) with a previously failed trabeculectomy. An overall surgical success rate (IOP≤21 mmHg with or without medications) of 84.2% was achieved at a mean follow-up of 12 months. Other authors have reported a similar success rate with the use of adjuvant MMC in eyes with a high risk for failure.3
You et al7 reported a complete success rate of 95.5% for repeat trabeculectomy with simultaneous subconjunctival and subscleral MMC 1 year postoperatively and confirmed that MMC application under both flaps resulted in a higher success rate than when MMC was applied subconjunctivally. This success rate compares favourably with our results.
In deep sclerectomy, the use of Nd:YAG goniopuncture in the follow-up can change the values of IOP control. It is an efficient and safe treatment to re-establish a useful filtration of aqueous humour through the TDM. The rate of goniopunctures varies between studies and it increases with the follow-up. Shaarawy et al8 reported an Nd:YAG goniopuncture rate of 51% with a mean follow-up of 64 months and a mean time of goniopuncture performance of 21 months. Previous filtering surgery could accelerate fibrosis of the TDM, explaining why we had to use more commonly and early TDM goniopuncture.
Other surgical options when the primary trabeculectomy fails are slit-lamp needle revision with antimetabolites20 or an aqueous shunt procedure.
However, bled needle revision is not indicated in eyes with thick scarring, an immobile conjunctiva or an unidentifiable trabeculectomy flap.
Practice patterns vary in the surgical management of glaucoma, and there are differing opinions among glaucoma surgeons regarding the preferred surgical approach in patients who have undergone failed filtering surgery. Although the use of glaucoma drainage devices has increased in cases with poor prognosis, trabeculectomy and MMC continue to be preferably used for surgical management.21 The tube vs trabeculectomy (TVT) study is a multicentre randomized clinical trial that will compare the safety and efficacy of nonvalved tube shunt surgery to trabeculectomy with MMC in patients with previous intraocular surgery. Forthcoming data from the TVT study should provide valuable information comparing both surgical procedures.22
The advantage of deep sclerectomy over trabeculectomy is the development of fewer postoperative complications, which can in some instances precipitate or accelerate surgical failure. In fact, hypotony results in increased breakdown of the blood–aqueous barrier and increased inflammatory mediator release and it has been associated with decreased survival time of blebs.23 In our study, no flat or shallow anterior chamber developed. Moreover, trabeculectomy is associated with subsequent cataract formation, and cataract extraction has an important effect on the rate of failure of previous trabeculectomy.24, 25 In our study, most patients (90%) had had cataract surgery several years after the primary trabeculectomy alone or combined with a new trabeculectomy with MMC (Table 1).
We found that simultaneous MMC administration under the conjunctival and superficial scleral flaps in deep sclerectomy is associated with a high success rate and a lower incidence of postoperative complications in eyes with a previously failed trabeculectomy.
This pilot study is limited by its noncomparative nature, short follow-up, and small number of cases. Further studies are needed to compare deep sclerectomy and trabeculectomy in eyes with a failed trabeculectomy. Considering these limitations, our results are encouraging and should be reproducible by other glaucoma surgeons using similar techniques.
References
Chen TC, Wilensky JT, Viana MAG . Long-term follow-up of initially successful trabeculectomy. Ophthalmology 1997; 104: 1120–1125.
Molteno ACB, Bosma NJ, Kittelson JM . Otago glaucoma surgery outcome study. Long-term results of trabeculectomy—1976–1995. Ophthalmology 1999; 106: 1742–1750.
Palmer SS . Mitomycin as adjunct chemotherapy with trabeculectomy. Ophthalmology 1991; 98: 317–321.
Cohen JS, Novack GD, Li Z . The role of mitomycin treatment duration and previous intraocular surgery in the success of trabeculectomy surgery. J Glaucoma 1997; 6: 3–9.
Perkins TW, Gangnon R, Ladd W, Kaufman PL, Heatley GA . Trabeculectomy with mitomycin C; intermediate-term results. J Glaucoma 1998; 7: 230–236.
Stone RT, Herndon LW, Allingham RR, Shields MB . Results of trabeculectomy with 0.3 mg/ml mitomycin C titrating exposure times based on risk factors for failure. J Glaucoma 1998; 7: 39–43.
You YA, Gu YS, Fang CT, Ma XQ . Long-term effects of simultaneous subconjunctival and subscleral mitomycin C application in repeat trabeculectomy. J Glaucoma 2002; 111: 110–118.
Shaarawy T, Mansouri K, Schnyder C, Ravinet E, Achache F, Mermoud A . Long-term results of deep sclerectomy with collagen implant. J Cataract Refract Surg 2004; 30: 1225–1231.
El Sayyad F, Helal M, El-Kholify H, Khalil M, El-Maghraby A . Nonpenetrating deep sclerectomy versus trabeculectomy in bilateral primary open-angle glaucoma. Ophthalmology 2000; 107: 1671–1674.
Cheng JW, Ma XY, Wei RL . Efficacy of non-penetrating trabecular surgery for open angle glaucoma: a meta-analysis. Chin Med J 2004; 117: 1006–1010.
Egrilmez S, Ates H, Nalcaci S, Andac K, Yagci A . Surgically induced corneal refractive change following glaucoma surgery: nonpenetrating trabecular surgeries versus trabeculectomy. J Cataract Refract Surg 2004; 30: 1232–1239.
Schwenn O, Springer C, Troost A, Yun SH, Pfeiffer N . Deep sclerectomy using a hyaluronate implant versus trabeculectomy. A comparison of two glaucoma operations using mitomycin C. Ophthalmologe 2004; 101: 696–704.
Ambresin A, Shaarawy T, Mermoud A . Deep sclerectomy with collagen implant in one eye compared with trabeculectomy in the other eye of the same patient. J Glaucoma 2002; 11: 214–220.
Kozobolis VP, Christodoulakis EV, Tzanakis N, Zacharopoulos I, Pallikaris IG . Primary deep sclerectomy versus primary deep sclerectomy with the use of mitomycin C in primary open-angle glaucoma. J Glaucoma 2002; 11: 287–293.
Neudorfer N, Sadetzki S, Anisimova S, Geyer O . Nonpenetrating deep sclerectomy with the use of adjunctive mitomycin C. Ophthalmic Surg Lasers Imaging 2004; 35: 6–12.
Anand N, Atherley C . Deep sclerectomy augmented with mitomycin C. Eye 2005; 19: 442–450.
Agarwal HC, Sharma TK, Sihota R, Gulati V . Cumulative effect of risk factors on short-term surgical success of mitomycin augmented trabeculectomy. J Postgrad Med 2002; 48: 92–96.
El Sayyad FE, Belmekki M, Helal M, Khalil M, El-Hamzawey H, Hisham M . Simultaneous subconjunctival and subscleral mitomycin C application in trabeculectomy. Ophthalmology 2000; 107: 298–301.
Khaw PT, Chang L, Wong TL, Mead A, Daniels JT and Cordeiro MF . Modulation of wound healing after glaucoma surgery. Curr Opin Ophthalmology 2001; 12: 143–148.
Shetty RK, Wartluft L, Moster MR . Slit-lamp needle revision of failed filtering blebs using high-dose mitomycin C. J Glaucoma 2005; 14: 52–56.
Joshi AB, Parrish II RK, Feuer WF . 2002 survey of the American Glaucoma Society: practice preferences for glaucoma surgery and antifibrotic use. J Glaucoma 2005; 14: 172–174.
Gedde SJ, Schiffman JC, Feuer WJ, Parrish II RK, Heuer DK and Brandt JD . The tube versus trabeculectomy study: design and baseline characteristics of study patients. Am J Ophthalmol 2005; 140: 275–287.
Benson SE, Mandal K, Bunce CV, Fraser SG . Is post-trabeculectomy hypotony a risk factor for subsequent failure? A case–control study. BMC Ophthalmol 2005; 5: 5–7.
Rebolleda G, Muñoz-Negrete FJ . Phacoemulsification in eyes with functioning filtering blebs: a prospective study. Ophthalmology 2002; 109: 2248–2255.
Klink J, Schmitz B, Lieb WE, Klink T, Grein HJ, Sold-Darseff J et al. Filtering bleb function alter clear cornea phacoemulsification: a prospective study. Br J Ophthalmol 2005; 89: 597–601.
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors has a financial or proprietary interest in any material or method mentioned
Rights and permissions
About this article
Cite this article
Rebolleda, G., Muñoz-Negrete, F. Deep sclerectomy with mitomycin C in failed trabeculectomy. Eye 21, 23–28 (2007). https://doi.org/10.1038/sj.eye.6702183
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702183