Abstract
Introduction:
Acute bleeding of different genesis can be a severe, life-threatening problem in neonatology. Recombinant factor seven (rFVIIa) is known to have unique hemostatic properties in adults and older children.
Case presentation:
Three cases of acute life-threatening peri- and postnatal hemorrhage were successfully controlled after the application of fFVIIa. All infants were first treated with vitamin K, fresh-frozen plasma and platelet transfusion.
Conclusion:
The cases substantiate other reports that rFVIIa is an effective treatment for acute, refractory and life-threatening bleeding in neonates and premature infants.
Similar content being viewed by others
Introduction
Recombinant activated factor VII (Novoseven, Novo Nordisk Pharma A/S, Bagsvaerd, Denmark; rFVIIa) was initially developed for the treatment of hemophiliacs with inhibitors to factor VIII and IX. Meanwhile, numerous case reports and studies give evidence that rFVIIa is efficient in treating acute bleeding in patients without preexisting hemophilia.1 In adults, rFVIIa was used to treat or prevent bleeding in patients with oral anticoagulation-therapy, heparin therapy, thrombocytopenia, impaired liver function, traumatic bleeding, gastrointestinal bleeding, cardiothoracic surgery, postoperative bleeding and intracerebral hemorrhage.2
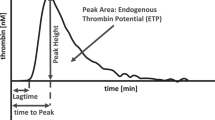
Recombinant FVIIa is unique because it does not have enzymatic activity without its cofactor, the tissue factor (TF). The hemostatic active complex VIIa/TF can only be formed in the presence of a tissue trauma. Thus, the effect of activated factor seven is mainly localized to the site of trauma – and general activation of coagulation does not usually occur. Factor VIIa binds to TF in the presence of endothelial damage. The Factor VIIa/TF complex activates factor X (FXa), which in turn leads to a formation of thrombin (activated factor II; FIIa). FII activates platelets at the site of the damage. In addition, FVIIa applied in high doses without TF is bound to activated platelets leading to activation of FX, FII and the formation of a localized fibrin clot.
The following is a report on three cases of acute, life-threatening peri- and post-natal hemorrhage with cardiovascular shock, which were successfully controlled after the application of rFVIIa.
Case 1
The female patient was born at 40 weeks’ gestation with a birth weight of 3800 g; Apgar score was 6, 5 and 5 at 1, 5 and 10 min, respectively, and the umbilical artery blood pH was 7.21. The infant was the second pregnancy of a 32-year-old mother. The actual pregnancy and delivery were uneventful except herpetiform blisters were present on the mother's lower back. Immediately after birth the infant had massive pulmonary bleeding and developed severe respiratory insufficiency. In the delivery room, the baby was intubated, manually ventilated and significant amounts of blood were suctioned from the endotracheal tube. Fresh-frozen plasma (20 ml/kg) and packed red blood cells (30 ml/kg) were transfused via venous umbilical catheter. The baby was transferred to the Children's Hospital of the University of Cologne. In the neonatal intensive care unit, the pulmonary bleeding persisted and the infant was put on high-frequency ventilation and vasopressors. After a single intravenous infusion of 90 μg/kg rFVIIa, the bleeding decreased significantly within a few minutes. The baby received a second bolus of 200 μg/kg rFVIIa 17 h later because of persisting blood-stained tracheal secretion (coagulation tests and platelet count see Table 1). The cause of the underlying consumption coagulopathy was most likely a perinatal Herpes-simplex virus type 1-infection demonstrated by positive polymerase chain reaction from anal and vaginal swabs and pleural effusion. The patient received acyclovir for 21 days. Elevated liver enzymes with peak alanine aminotransferase of 388 U/l and aspartate aminotransferase of 482 U/l on day of life (DOL) three gave evidence of hepatitis. The infant was ventilated for 9 days and required supplemental oxygen for 11 days. The now 16-month-old girl recovered and was dismissed from hospital on DOL 21. She survived without any neurologic sequelae.
Case 2
A male newborn was delivered by caesarean section for shoulder dystocia at 42 weeks’ gestation. It was the first pregnancy of a 25-year-old mother, which had been uneventful. The birth weight of the infant was 4000 g. The baby had severe asphyxia with an umbilical artery blood pH of 6.84 and an Apgar score of 0, 0 and 2 at 1, 5 and 10 min, respectively. The infant was intubated, ventilated and resuscitated with epinephrine, sodium bicarbonate and infusion of normal saline. Dopamine and dobutamine were also begun. On DOL 1, the infant developed a massive subgaleal hemorrhage extending around the whole cranial circumference. Transfusions of packed red blood cells (28 ml/kg), fresh-frozen plasma (20 ml/kg) and platelets (20 ml/kg) were given. There was no intracranial hemorrhage. Despite these measures, the subgaleal bleeding persisted. The maximum vertical diameter of the bleeding measured by ultrasonography was 2.3 cm. After an intravenous bolus of 120 μg/kg rFVIIa, the progression of the bleeding was interrupted. International normalized ratio (INR) decreased immediately from 2.0 to 1.1 (coagulation tests see Table 1). During the first 72 h after birth, whole body hypothermia for neuroprotection was induced with a central body temperature of 33−34°C. Electroencephalogram on DOL 5 was suppressed with dissociated discharges. The infant was extubated on DOL 7. At hospital discharge on day 25, the neurologic condition was satisfactory, cranial ultrasounds showed no pathologic findings. At the age of 6 months, surgery was performed for persisting plexus paresis of the left arm. The neurological development of the now 12-month-old infant is appropriate for its age; no epilepsy or cerebral palsy has developed.
Case 3
A female premature infant was delivered by Caesarean section at 27 6/7 weeks’ gestation with a birth weight of 1100 g because of premature rupture of membranes, amnionitis and pathologic fetal heart rate in the cardiotocogram. The mother had received antenatal intravenous steroids on the day of delivery. Apgar scores were 8, 8 and 9 at 1, 5 and 10 min, respectively. Initially, the infant was stabilized using continuous positive airway pressure (CPAP) with low supplemental oxygen requirement of 0.25 FiO2. On DOL 4, respiration deteriorated and she was intubated and ventilated for 1 day. The underlying cause of the deterioration was most likely an obstruction of the upper airways. Indomethacin therapy (0.2 mg/kg; 4 times at 12-hour intervals) for persisting ductus arteriosus was started at the age of 20 h. On DOL 8, 3 days after completion of the indomethacin therapy, a large upper gastrointestinal tract hemorrhage developed that was considered to be life threatening. She was treated with a transfusion of fresh-frozen plasma (20 ml/kg), platelets (15 ml/kg) and packed red blood cells (38 ml/kg), vitamin K, ranitidine and gastric lavage with cold isotonic saline. Infusion of dopamine and dobutamine was started to support circulation. Despite these measures, the bleeding did not stop until a bolus of rFVIIa 110 μg/kg was given intravenously. INR immediately decreased from 8.9 to 0.9 and activated partial thromboplastin time (aPTT) decreased from 120 to 28 s. Bleeding did not recur. Cranial ultrasound showed intraventricular hemorrhage grade II immediately after the birth. There was no progression and the bleeding resolved. CPAP therapy was terminated on DOL 25. Before discharge, there was no gross pathological finding in cranial ultrasound and no evidence of periventricular leukomalacia. Electroencephalogram was appropriate for her age. The neurological development of the girl is satisfactory, at the age of 10 months she had a disturbance of the central motor-tone and coordination.
None of the three patients displayed adverse events related to rFVIIa such as thrombosis or increased bleeding and the infusions did not affect cardiopulmonary status. None of the children had an underlying hemorrhagic diathesis.
Search strategy
Medline and EMBASE databases were searched using the words novoseven, rFVIIa, recombinant factor VIIa, recombinant activated factor VII, recombinant activated factor seven and newborn, neonate and premature in combination.
Discussion
The above relates to three cases of life-threatening bleeding in the perinatal period of two term newborn and one premature infant. The hemorrhages were of different origin (pulmonary, gastrointestinal and subgaleal bleeding). None of the children were diagnosed as having genetic causes for the hemorrhagic diathesis. In all three cases, vitamin K, transfusion of fresh-frozen plasma and platelets had no effect on the extent of the bleeding. The administration of an intravenous bolus of rFVIIa in a dose range of 90 to 200 μg/kg in all cases led to a quick resolution of the bleeding. Except for one patient, a single infusion of rFVIIa was sufficient to stop the bleeding and no recurrence or progression of the bleeding occurred. In the case of one term newborn, a second dose was administered 17 h after the first because of apparent persisting pulmonary hemorrhage.
Although rFVIIa was effective in the treatment of life-threatening hemorrhage in our patients, experience is limited in this age group and sample size is too small to draw definite conclusions on efficacy. In this age group, the use of rFVIIa for acute bleeding without underlying hemorrhagic diathesis is off-label and has to be classified as an experimental therapy if other therapeutic efforts have failed.
A few other case reports on the use of rFVIIa in the neonatal period exist (Table 2), underlining our positive experience. These experiences include: intracranial hemorrhage in neonates with FVII deficiency,3, 4 intraventricular hemorrhage associated with coagulopathy caused by liver failure,5 infants during open heart surgery and extracorporeal membrane oxygenation (ECMO),6, 7, 8 resection of a giant sacrococcygeal teratoma,9 and with intraperitoneal and subcapsular liver bleeding.10 In premature infants, rFVIIa use was reported for treatment of bleeding from liver and spleen,11, 12 from pulmonary and intercostal arteries,11 from surgical wounds,12, 13 and from pulmonary hemorrhage.14 The 22 patients in these reports were born between 23 and 42 weeks gestation and they ranged in weight between 0.55 kg and 4.2 kg. The median day of rFVIIa therapy was DOL 8 (median; range: 1 to 83 days).
These case reports substantiate the efficacy of rFVIIa in controlling acute hemorrhage in the perinatal period. In 21 of the published 22 cases of neonatal hemorrhage, including our patients, rFVIIa led to a significant decrease of the bleeding within a few minutes after administration. In their case series of four premature infants with necrotizing enterocolitis (NEC), Filan et al.12 reported on one very immature infant of 24 weeks of gestation with NEC complicated by intra-abdominal abscesses who did not respond to rFVIIa. After operation on DOL 83 for abscess drainage, the infant bled from the surgical drains and received fluids, red packed cells, platelets, fresh-frozen plasma and two doses of rFVIIa with 400 μg/kg each dose. The underlying cause for the intractable bleeding was peritonitis with disseminated intravascular coagulopathy.
The most effective dosing regimen is uncertain. Dosage regimens in the above-mentioned cases differed from 15 to 400 μg/kg/bolus (the median dose was 95 μg/kg). The dosage intervals varied from the administration of a single dose, multiple doses given every 3 h and continuous infusion. The different administration techniques all induced a significant reduction of bleeding, except for the NEC patient reported above who received the high dose of 400 μg/kg.12 One patient with FVII deficiency with multiple intracranial hemorrhages was initially treated with 15 μg/kg rFVIIa.4 Here it is unclear if the bleeding was still in progress or if rFVIIa was administered with the intention to avoid the occurrence of further bleedings. In conclusion, rFVIIa doses of 40 to 300 μg/kg were sufficient to control acute hemorrhage in a variety of circumstances in newborn infants.
The recommended dose for the treatment of hemophiliac patients with inhibitors to factor VIII and IX is 90 μg/kg, repeated at 3 h intervals. Elimination half-life in adults is about 3 h. The pharmacokinetics of rFVIIa has been investigated in older children with hemophilia.15 In children (3 to 12 years), clearance of rFVIIa was significantly faster than in the adult population. Following the administration of 90 μg/kg, the clearance of FVIIa was 78 ml/kg/h in the pediatric population and 53 ml/kg/h in the adult population. The authors conclude that higher doses of rFVIIa may be appropriate for children to achieve the same plasma levels as adults. In the neonatal population, further investigation of population pharmacokinetics or controlled studies are required to establish age-dependant pharmakodynamic and pharmacokinetic data.
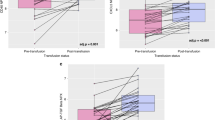
In our patients, we observed an immediate decrease in aPTT and especially in INR after administration of rFVIIa (see Table 1). Some of the case reports on infants with acute hemorrhage give further evidence for the effect of rFVIIa on clotting parameters. Though it is difficult to differentiate the effect of rFVIIa from the effect of fresh-frozen plasma or vitamin K, which in most cases were administered closely to rFVIIa, there is a consistent trend to improved prothrombin time (PT), INR and aPTT. Table 3 (electronic publication) shows the averaged values for INR, PT and aPTT before and after the administration of rFVIIa.
Furthermore, preventive administration of rFVIIa in neonates with preexisting coagulopathy or acquired and congenital FVII deficiency seems to correct coagulation tests and thereby diminish the risk of bleeding with invasive procedures (see Table 2b; and references16, 17, 18, 19).
Finally, in our patients, we did not observe adverse events related to the administration of rFVIIa. Four of the 22 published cases describe adverse events possibly related to the adminstration of rFVIIa. In adults, arterial and venous thrombosis (e.g. myocardial infarction, bowel infarction rsp. deep vein thrombosis) are reported as rare complications with rFVIIa administration, mainly in patients with predisposing diseases as artherosclerosis, immobilization or additive risk factors for thrombosis formation. In the neonatal population, one report7 describes a thrombotic occlusion of the truncus brachiocephalicus in a term-neonate on ECMO support after cardiac surgery. The baby received 90 μg/kg rFVIIa for intractable bleeding from pulmonary left upper lobe fistulas. Initially, rFVIIa brought sufficient hemostasis but later the bleeding recurred. Autopsy revealed thrombotic occlusion of both subclavian arteries and the truncus brachiocephalicus. The authors recommend caution with the administration of rFVIIa to neonates supported by a circulatory assist device, especially when other coagulation products are administered. Other authors report good tolerance and efficacy of rFVIIa in acute hemorrhage in neonates on ECMO support.6 Filan et al.12 observed a transient digital ischemia in the presence of a radial artery line and the development of an arterial thrombus related to a brachial artery catheter in two of their premature infants treated with rFVIIa. The authors cannot exclude a relation to rFVIIa use. Tancabeli et al.5 report on a premature infant of 36 weeks of gestation with intracranial hemorrhage owing to a severe coagulopathy secondary to liver dysfunction. With progression of the bleeding, the baby received two bolus doses of 80 μg/kg rFVIIa followed by a continuous infusion of rFVIIa aimed to maintain a normal PT. On hospital day 38, with the rFVIIa infusion still continued, a thrombus related to a central venous line in the common left femoral vein was noted. The thrombus was treated with low molecular weight heparin and unfractionated heparin.
Thrombus formation in the presence of intravascular catheters is a common problem in neonatology. It is not possible to attribute the observed adverse events definitely to the administration of rFVIIa but an enhanced disposition to thrombus formation with rFVIIa in the presence of intravascular foreign material and especially in a systemic inflammation cannot be excluded.
To date, there is insufficient data to prove that rFVIIa is a safe therapy in neonates; but there is preliminary evidence that rFVIIa is not only effective, but also well-tolerated by patients.
Further confirmatory studies are required to determine pharmacokinetics and dynamics and to collect data on safety in premature infants and term neonates. In cases of acute bleeding not responsive to therapy with fresh-frozen plasma, cryoprecipitate and platelets, rFVIIa possibly is an effective treatment to control hemostasis. To date, it has to be regarded as an off-label use with curative intention in life-threatening situations. With increasing knowledge, rFVIIa may become an essential part in the therapy of refractory acute bleeding complications in neonatology.
References
Heuer L, Blumenberg D . Recombinant factor VIIa (NovoSeven®). A review of current and possible future indications. Anaesthesist 2002; 51: 388–399.
Mayer SA, Brun NC, Begtrup K, Broderick J, Davis S, Diringer MN et al. Recombinant activated factor VII for acute intracerebral hemorrhage. New Engl J Med 2005; 352: 777–785.
Chuansumrit A, Visanuyothin N, Puapunwattana S, Chaivisuth A, Rasmidat P, Charoenkwan P et al. Outcome of intracranial hemorrhage in infants with congenital factor VII deficiency. J Med Assoc Thai 2002; 85(S4): 1059–1064.
Wong WY, Huang WC, Miller R, McGinty K, Whisnat JK . Clinical efficacy and recovery levels of recombinant FVIIa (Novoseven) in the treatment of intracranial haemorrhage in severe neonatal FVII deficiency. Haemophilia 2000; 6: 50–54.
Tancabelic J, Haun SE . Management of coagulopathy with recombinant factor VIIa in a neonate with echovirus type 7. Pediatr Blood Cancer 2004; 43: 170–176.
Wittenstein B, Ng C, Ravn H, Goldmann A . Recombinant factor VII for severe bleeding during extracorporeal membrane oxygenation following open heart surgery. Pediatr Crit Care Med 2005; 6: 473–476.
Velik-Salchner C, Sergi C, Fries D, Moser P, Streif W, Kolbitsch C . Use of recombinant factor VIIa (Novoseven) in combination with other products led to a thrombotic occlusion of the truncus brachiocephalicus in a neonate supported by exracorporal membrane oxygenation. Anesth Analg 2005; 101: 924.
Razon Y, Erez E, Vidne B, Birk E, Katz J, Tamari H et al. Recombinant factor VIIa (NovoSeven®) as a hemostatic agent after surgery for congenital heart disease. Pediatric Anesth 2005; 15: 235–240.
Girisch M, Rauch R, Carbon R, Habash T, Hofbeck M . Refractory bleeding following major surgery of a giant teratoma in a premature infant: succesful use of recombinant factor VIIa. Eur J Pediatr 2004; 163: 118–119.
Millar CG, Stringer MD, Sugarman I, Richards M . The use of recombinant factor VIIa for bleeding in paediatric practice. Haemophilia 2005; 11: 171–174.
Veldman A, Fischer D, Voigt B, Beyer PA, Schlösser R, Allendorf A et al. Life-threatening hemorrhage in neonates management with recombinant activated factor VII. Intens Care Med 2002; 28: 1635–1637.
Filan PM, Mills JF, Clarnette TD, Ekert H, Ekert P . Spontaneous liver hemorrhage during laparotomy for necrotizing enterocolitis: a potential role for recombinant factor VIIa. J Pediatr 2005; 147: 857–859.
Chuansumrit A, Nuntnarumit P, Okascharoen C, Teerakatkul S, Suwansingh S, Supapannachart S . The use of recombinant activated factor VII to control bleeding in a preterm infant undergoing exploratory laparotomy. Pediatrics 2002; 107: 169–170.
Olomu N, Kulkarni N, Manco-Johnson M . Treatment of severe pulmonary hemorrhage with activated recombinant factor VII (rFVIIa) in very low birth weight infants. J Perinatol 2002; 22: 672–674.
Villar A, Aronis S, Morfini M, Santagostino E, Auerswald G, Thomsen HF et al. Pharmacokinetics of activated recombinant coagulation factor VII (NovoSeven) in children vs adults with haemophilia A. Haemophilia 2004; 10: 352–359.
Fontaine MJ, Lazarchick J, Taylor S, Annibale D . Use of recombinant factor VIIa in Infants with severe coagulopathy. J Perinatol 2004; 24: 310–311.
Greisen G, Andreasen RB . Recombinant factor VIIa in preterm neonates with prolonged prothrombin time. Blood Coagul Fibrinolysis 2003; 14: 117–120.
Maimon M, Bernstein T, Kenet G, Kapelushnik J . Recombinant factor VIIa for treatment of a child with severe factor VII deficiency and coarctation of the aorta. J Pediatr Hematol Oncol 2003; 25: 591.
Tokunaga C, Hiramatsu Y, Horigome H, Takahashi-Igari M, Noma M, Sakakibara Y . Palliative open heart surgery in an infant with factor VII deficiency. Ann Thorac Surg 2003; 76: 2093–2094.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hünseler, C., Kribs, A., Eifinger, F. et al. Recombinant activated factor seven in acute life-threatening bleeding in neonates: report on three cases and review of literature. J Perinatol 26, 706–713 (2006). https://doi.org/10.1038/sj.jp.7211588
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211588
Keywords
This article is cited by
-
Neonatal subgaleal hemorrhage: twenty years of trends in incidence, associations, and outcomes
Journal of Perinatology (2023)
-
Recombinant Activated Factor VIIa (rFVIIa) Treatment in Very-Low-Birth-Weight (VLBW) Premature Infants with Acute Pulmonary Hemorrhage: A Single-Center, Retrospective Study
Pediatric Drugs (2017)
-
Recombinant activated factor VIIa treatment for refractory hemorrhage in infants
Journal of Perinatology (2011)
-
The neonatal coagulation system and the vitamin K deficiency bleeding – a mini review
Wiener Medizinische Wochenschrift (2008)