Abstract
High incidences of human herpesvirus (HHV)-6 encephalitis have recently been reported from several Japanese SCT centers. To evaluate the effect of low-dose foscarnet (PFA) in preventing HHV-6 infection among recipients of unrelated BM or cord blood (CB), we examined consecutive cohorts without prophylaxis against HHV-6 (Cohort 1, n=51) and with PFA prophylaxis (Cohort 2, PFA 50 mg/kg/day for 10 days after engraftment, n=67). Plasma real-time PCR assay was performed weekly. High-level reactivation defined as HHV-6 DNA⩾104 copies/mL by day 70 was the primary endpoint. No significant reduction of high-level reactivation was seen in Cohort 2 (19.4%) compared with Cohort 1 (33.8%, P=0.095). A trend was identified toward fewer high-level HHV-6 reactivations in Cohort 2 among recipients of unrelated BM (P=0.067), but no difference in incidence was observed among CB recipients (P=0.75). Breakthrough HHV-6 encephalitis occurred following PFA prophylaxis in three patients, and incidence of HHV-6 encephalitis did not differ between Cohort 1 (9.9%) and Cohort 2 (4.5%, P=0.24). In conclusion, 50 mg/kg/day of PFA does not effectively suppress HHV-6 reactivation and cannot prevent all cases of HHV-6 encephalitis. To effectively prevent HHV-6 encephalitis, alternative approaches based on the pathogenesis of HHV-6 encephalitis will probably be required.
Similar content being viewed by others
Introduction
Human herpesvirus (HHV)-6 reactivates early after hematopoietic SCT and is found in the blood in about half of allo-SCT recipients.1, 2, 3, 4 HHV-6 reactivation is potentially associated with various post-transplant complications, including those affecting the skin, lung, gastrointestinal tract and central nervous system (CNS).5, 6 In particular, HHV-6 encephalitis has been recognized as a life-threatening complication associated with HHV-6 reactivation.
HHV-6 encephalitis typically developed 3 weeks after SCT.7, 8 Memory disturbance is a typical initial symptom, and consciousness loss, disorientation and seizures can subsequently develop.3, 7, 8, 9 The limbic system is a target of HHV-6.3, 6, 7, 8, 9, 10 Recipients of unrelated transplants and cord blood (CB) display a high risk of HHV-6 encephalitis.3, 4, 7, 8 HHV-6 encephalitis develops concomitant to the appearance of a high-HHV-6 DNA load in plasma.3, 11, 12 This suggests that systemic high-level HHV-6 replication is a key factor in the development of HHV-6 encephalitis and that HHV-6 encephalitis is preventable as long as high-level HHV-6 reactivation can be suppressed.
Foscarnet (PFA), ganciclovir (GCV) and cidofovir (CDV) have been shown to display in vitro inhibitory effects against HHV-6,5 and most patients with reported HHV-6 encephalitis are treated with GCV and/or PFA.7, 8 However, more than half of the patients who developed HHV-6 encephalitis developed neurological sequelae such as memory disturbance, or died of encephalitis.3, 7, 8, 13, 14, 15 The efficacy of antiviral treatment after development of HHV-6 encephalitis thus appears insufficient.
The European Conference on Infections in Leukemia does not recommend antiviral prophylaxis against HHV-6, because of the low risk of HHV-6 disease and the toxicity of the available antiviral drugs.16 However, a high incidence of HHV-6 encephalitis has recently been reported from several Japanese SCT centers3, 4, 12, 13, 14, 15, 17, 18, 19 (Table 1). Several investigators have asserted that the establishment of methods to prevent HHV-6 encephalitis is needed for patients at high risk of this complication.6, 11, 14, 15, 20, 21
To prevent the development of HHV-6 encephalitis, we have attempted pre-emptive GCV therapy guided by plasma HHV-6 DNA load.11 However, dynamic kinetics of plasma HHV-6 viral load make pre-emptive therapy difficult. Prophylactic administration of active agents against HHV-6 may be useful to prevent HHV-6 encephalitis. The important issue is whether the benefits of preventing HHV-6 encephalitis outweigh the toxicities associated with the antiviral drug. HHV-6 reactivation concentrates during the first 10 days after engraftment,3 and prophylaxis using GCV during this period may be associated with prolonged neutropenia.22 While PFA may be more appropriate than GCV as a prophylactic agent, renal toxicity remains problematic for prophylactic use.21 The effects of PFA in preventing CMV infection have been studied previously,23, 24 but this agent is not currently in common used for prophylaxis due to its toxicity.
Although two studies evaluating the effects of prophylaxis to prevent HHV-6 reactivation have been reported,25, 26 those investigations were very small. The present study investigated whether prophylactic measures are effective for preventing high-level HHV-6 reactivation and HHV-6 encephalitis. Given the myelosuppressive effects of GCV, we chose PFA as a prophylactic agent. As PFA shows dose-dependent renal toxicity, a low dosage (50 mg/kg) and short-dosing period (10 days) were applied. Kinetics of plasma HHV-6 DNA among patients who received prophylactic PFA were compared with those of our historic controls.
Patients and methods
All study protocols were approved by the ethics committees of both the Oita University Faculty of Medicine and Oita Prefectural Hospital, and written informed consent was obtained from each patient before participation.
Patients
Cohort 1
This cohort comprised patients who received BMT from unrelated donor or CB transplantation (CBT) at Oita University Hospital or Oita Prefectural Hospital between November 1995 and February 2007. Eligibility criteria were as follows: age between 15 and 65 years; no severe concomitant disease; creatinine clearance >1 mL/min/kg bodyweight; and no prophylactic administration of GCV, PFA or CDV. Patients who received pre-emptive administration of GCV based on positive results for CMV antigenemia were not excluded. Patients in Cohort 1 were used as historical controls to evaluate the effects of PFA prophylaxis in Cohort 2. Cohort 1 included 31 patients who had participated in an earlier retrospective study linking plasma HHV-6 DNA with clinical manifestations3 and 20 patients treated subsequently.
Cohort 2
This cohort comprised patients who received BMT from unrelated donors or CBT at Oita University Hospital or Oita Prefectural Hospital between February 2007 and August 2011. Eligibility criteria were as follows: age between 15 and 65 years; no severe concomitant disease; and creatinine clearance >1 mL/min/kg bodyweight.
Patients in whom chromosomally integrated HHV-627 was suspected based on the findings of persistent-positive results for plasma HHV-6 DNA (⩾80% of plasma samples) were excluded from analysis.
Prophylactic PFA in Cohort 2
Patients in Cohort 2 were prospectively enrolled for this study and given i.v. PFA at 50 mg/kg/day, for 10 days from the day of neutrophil engraftment. If engraftment had not been achieved by 18 days after transplantation, PFA was started on the 18th day after SCT and continued for 10 days. Any patient showing ⩾grade 2 renal dysfunction (serum creatinine ⩾1.6 mg/dL) or severe concomitant organ dysfunction on the date of starting PFA was excluded from this study. During the dosing period, if a patient showed serum creatinine level of at least grade 2, non-hematological toxicity of at least grade 3 other than nausea or vomiting, or refusal to continue administration, PFA administration was interrupted. Patients who start to receive prophylactic PFA but interrupted administration at any time were still included in the analyses.
Assay
In both cohorts, collection of EDTA-treated peripheral blood was started within 1 week after SCT, and performed weekly during hospitalization. Samples collected until 100 days after SCT were used for analysis for both of cohort groups. HHV-6 DNA copy numbers in plasma samples were measured using real-time PCR methods, as described previously.3
Definitions
The primary endpoint was the incidence of high-level HHV-6 reactivation by day 70 after SCT. High-level HV-6 reactivation was defined as a plasma HHV-6 DNA ⩾104 copies/mL. The primary endpoint was set based on our findings that the threshold level for the development of HHV-6 encephalitis was 104 copies/mL plasma under our real-time PCR assay system.12 Secondary endpoints were the incidence of HHV-6 reactivation, adverse events during the PFA-dosing period and development of HHV-6 encephalitis or possible HHV-6 encephalitis. HHV-6 reactivation was defined as detection of HHV-6 DNA in plasma at any level. Toxicity was graded according to the Common Terminology Criteria for Adverse Events version 3.0 (National Cancer Institute, Bethesda, MD, USA). HHV-6 encephalitis was defined when patients satisfied all of the following criteria: (1) presence of CNS dysfunction; (2) a positive PCR result for HHV-6 in cerebrospinal fluid (CSF); and (3) the absence of other identified causes of CNS dysfunction. If no testing was performed to test for the presence of HHV-6 DNA in CSF, possible HHV-6 encephalitis was defined when patients satisfied all of the following criteria: (1) presence of CNS dysfunction; (2) demonstration of limbic encephalitis on magnetic resonance imaging (MRI); (3) positive plasma HHV-6 DNA; and (4) the absence of other identified causes of CNS dysfunction. Early stage was defined as acute leukemia during the first or second remission and CML during the first chronic phase, and myelodysplastic syndrome classified as refractory cytopenia with unilineage dysplasia, refractory cytopenia with multilineage dysplasia or refractory anemia with ringed sideroblasts; all other combinations were considered to represent non-early stage. Neutrophil engraftment was defined as an ANC of 0.5 × 109 neutrophils/L.
Statistical analysis
Comparisons of baseline characteristics between the two groups were made using Fisher’s exact test or the Mann–Whitney U-test. The P of first incidence of HHV-6 reactivation, high-level HHV-6 reactivation and HHV-6 encephalitis were estimated with Kaplan and Meier curves. The log-rank test was used to compare incidences between groups. Values of P<0.05 were considered statistically significant in all analyses. Prism for Macintosh version 5 software (GraphPad Software, San Diego, CA, USA) was used for all statistical analyses.
Results
Patient characteristics
Cohort 1 included a total of 51 consecutive patients who underwent BMT from unrelated donor or CBT. For Cohort 2, 73 patients were preliminarily enrolled before the start of preconditioning. Among these, a total of six patients withdrew or were judged as ineligible before starting PFA. The reasons for not receiving PFA were as follows: renal dysfunction (n=2); liver dysfunction (n=1); CNS complications of unknown origin (n=1); and death in the early phase because of sepsis (n=1) or heart failure (n=1). As a result, 67 patients received prophylactic PFA. Among these 67 patients who started to receive PFA, 11 patients were unable to complete 10 days of PFA administration. Reasons for not completing the full 10-day PFA administration were as follows: serum creatinine level reaching ⩾grade 2 (study termination rule) (n=3, all were grade (2); patient refusal to continue administration because of nausea (n=3, all were grade (3) or headache (n=1, grade 2); and discretion of the attending physician because of electrolyte loss (n=1, grade 2), graft failure (n=1) or liver dysfunction due to GVHD (n=2). Median duration of PFA administration in these 11 patients was 6 days (range, 2–9 days). These patients who received interrupted administration of PFA were included in the analyses.
Characteristics of the patients are listed in Table 2. Median age was significantly higher (P=0.0004) and P of receiving myeloablative conditioning was significantly lower (P<0.0001) in Cohort 2 than in Cohort 1.
HHV-6 reactivation
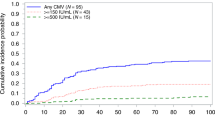
In both cohorts, no patient showed persisting positive plasma HHV-6 DNA suggestive of HHV-6 chromosomal integration. The P of first high-level HHV-6 reactivation (HHV-6 DNA ⩾104 copies/mL plasma) by day 70 after transplantation was the primary endpoint of the study. No significant reduction in high-level HHV-6 reactivation was seen in patients who received prophylactic PFA (33.8% and 19.4% in Cohorts 1 and 2, respectively; P=0.095) (Figure 1). Figure 2 shows the incidence of HHV-6 reactivation (left) and high-level HHV-6 reactivation (right) stratified by stem cell sources. Among unrelated BMT recipients (upper), a trend was seen toward fewer high-level HHV-6 reactivations in Cohort 2 (25.2 and 10.5% at day 70 after transplantation, in Cohorts 1, and 2, respectively, P=0.067). Among CBT recipients (bottom), no differences were identified in the incidence of either HHV-6 reactivation or high-level HHV-6 reactivation.
Kaplan–Meier estimates of the P of high-level HHV-6 reactivation (plasma HHV-6 DNA⩾104 copies/mL) in Cohort 1 (without prophylaxis against HHV-6, n=51) and Cohort 2 (with PFA prophylaxis, n=67). At day 70 after transplantation, the rate of plasma HHV-6 DNA ⩾104 copies/mL was 33.8% in Cohort 1 and 19.4% in Cohort 2 (P=0.095).
Kaplan–Meier estimates of the P of HHV-6 reactivation (positive plasma HHV-6 DNA at any level, left side of the figure) and high-level HHV-6 reactivation (plasma HHV-6 DNA ⩾104 copies/mL, right side of the figure), stratified by stem cell source (top side, unrelated BM; bottom, CB). For recipients of unrelated BM (n=97), the rate of HHV-6 reactivation at day 70 was 62.5% in Cohort 1 and 51.6% in Cohort 2 (P=0.20) and the rate of high-level HHV-6 reactivation was 25.2% and 10.5% in the two cohorts (P=0.067), respectively. For recipients of CB (n=21), all patients in Cohort 1 and 90% of patients in Cohort 2 experienced HHV-6 reactivation by day 42 and day 53, respectively (P=0.71). Rate of HHV-6 DNA ⩾104 copies/mL was 65.9% (at day 70) and 70% (at day 53) in Cohorts 1 and 2, respectively (P=0.75).
Analysis of the kinetics of plasma HHV-6 DNA in patients who displayed positive results in Cohort 2 (Figure 3) revealed that HHV-6 DNA peaked outside of the dosing period for PFA in 18 patients (before the dosing period in 8 patients; after the dosing period in 10 patients) and during the dosing period in 21 patients.
Kinetics of plasma HHV-6 DNA among patients who displayed positive HHV-6 DNA despite receiving PFA prophylaxis (n=39). The shaded area indicates values below the threshold for detection (<50 copies/mL of plasma). Periods indicated by arrows represent the PFA-loading period. The upper figure shows kinetics of plasma HHV-6 DNA in patients for whom HHV-6 DNA peaked before starting PFA (n=8), the middle figure shows those in patients for whom HHV-6 DNA peaked during the PFA-dosing period (n=21) and the bottom figure shows those in patients for whom HHV-6 DNA peaked after finishing PFA prophylaxis (n=10).
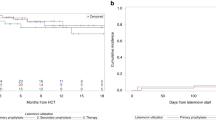
HHV-6 encephalitis
A total of five patients developed HHV-6 encephalitis (n=2) or possible HHV-6 encephalitis (n=3) in Cohort 1, while three patients developed HHV-6 encephalitis in Cohort 2. No significant difference in the incidence of HHV-6 encephalitis/possible HHV-6 encephalitis by day 70 was observed between cohorts (Kaplan and Meier analysis, 9.9% and 4.5% in Cohorts 1 and 2, respectively, P=0.24). Clinical courses and brain MRI findings of three patients who developed HHV-6 encephalitis despite receiving PFA prophylaxis are shown in Figures 4 and 5, respectively, and details are described below.
MRI of the brain for the three patients who developed HHV-6 encephalitis in Cohort 2, showing axial images at the level of the basal ganglia. Left side of figure shows T2-weighted fluid-attenuated inversion recovery imaging and right side shows diffusion-weighted imaging. Arrows indicate signal hyperintensities in limbic system. (a) For Patient 1 at 26 days after transplantation, 3 days after onset of neurological symptoms; (b) for Patient 2 at 28 days after SCT, on the day of onset of neurological symptoms; and (c) for Patient 3 at 43 days after SCT, 6 days after onset of neurological symptoms.
Patient 1 was a 31-year-old man who received CBT for the treatment of refractory EBV-positive lymphoma. Plasma HHV-6 DNA level continued increasing despite prophylactic administration of 50 mg/kg PFA. Short-term memory loss developed concomitant to peak plasma HHV-6 DNA (23 080 copies/mL), and neurological status changed with loss of consciousness and seizures. The patient died of pneumonia 43 days after SCT. Patient 2 was a 61-year-old man who received BMT from an HLA Ag-mismatched unrelated donor for the treatment of myelodysplastic syndrome. Plasma HHV-6 DNA turned positive 2 days after finishing prophylactic PFA, and disturbance of memory appeared. After treatment with 180 mg/kg of PFA, neurological symptoms gradually improved but memory difficulties remained until his death (due to GVHD) on day 152 after transplantation. Patient 3 was a 42-year-old man who received BMT from an HLA-matched unrelated donor for the treatment of refractory adult T-cell leukemia. Plasma HHV-6 DNA became positive (85 033 copies/mL) 9 days after finishing PFA. Although 50 mg/kg PFA was restarted, plasma HHV-6 DNA copy number increased to 190 236 copies/mL, and memory loss and mental confusion developed. After treatment with 180 mg/kg of PFA, the patient showed good cognitive recovery. The patient did not have neurological sequelae but died of GVHD 6 months after SCT.
In each patient with HHV-6 encephalitis, positive HHV-6 DNA in CSF was demonstrated at the time of developing HHV-6 encephalitis (54 305 copies/mL, 209 678 copies/mL and 262 447 copies/mL in Patients 1, 2 and 3, respectively). MRI showed signal abnormalities in the region of the hippocampus in each patient (Figure 5). HHV-6 DNA copy number in both plasma and CSF decreased rapidly after initiating administration of PFA at 180 mg/kg.
Risk factor analysis for high-level HHV-6 reactivation and HHV-6 encephalitis
The important risk factors for high-level HHV-6 reactivation were CBT and HLA-mismatched donor status (Table 3). Among recipients of unrelated BMT, HLA mismatch was not significantly associated with high-level HHV-6 reactivation (HLA allelic match vs mismatch, P=0.30; HLA Ag match vs mismatch, P=0.39). For HHV-6 encephalitis, high-level HHV-6 reactivation was the only significant risk factor. The treatment group (Cohort 1 vs Cohort 2) was not significantly associated with incidence of either high-level HHV-6 reactivation or HHV-6 encephalitis.
Toxicity
Adverse events during the period of PFA administration in Cohort 2 are shown in Table 4. Nausea and vomiting were common adverse events. No patients developed grade 3–5 adverse events of electrolyte (magnesium, calcium or potassium) loss or increased serum creatinine levels.
Discussion
This study showed that in the setting of allo-SCT from unrelated donors or CB, PFA given at 50 mg/kg once daily for 10 days in the early phase after allo-SCT is a safe but relatively ineffective strategy for preventing either high-level HHV-6 reactivation or HHV-6 encephalitis compared with a historical control cohort. PFA was suggested to suppress high-level HHV-6 reactivation in recipients of unrelated BM, but no benefit was observed among CBT recipients. Unexpectedly, breakthrough HHV-6 encephalitis developed in 3 of the 67 patients receiving prophylactic PFA.
One possible reason for this disappointing result is that the dose of PFA was insufficient. Analysis of the timing of peak plasma HHV-6 DNA in relation to the dosing period for PFA (Figure 3) showed that plasma HHV-6 DNA peaked during the PFA-dosing period in more than half of the patients. Among the three patients who developed HHV-6 encephalitis in Cohort 2, plasma HHV-6 DNA in two patients increased during the period in which PFA was given at 50 mg/kg/day (Patient 1, during dosing period of planned prophylactic PFA; Patient 3, during dosing period of repeated PFA) and HHV-6 encephalitis developed concomitant to peak plasma HHV-6 DNA. The effect of PFA at 50 mg/kg/day appears, at least with a short-dosing period before the detection of positive plasma HHV-6 DNA, insufficient to suppress the replication of HHV-6.
What is an appropriate strategy to prevent HHV-6 encephalitis? The kinetics of HHV-6 DNA in patients who developed HHV-6 encephalitis following PFA prophylaxis (Figure 3) showed that HHV-6 DNA from either plasma or CSF disappeared rapidly and CNS symptoms in two of these three patients started to improve immediately after starting PFA at 180 mg/kg/day. These observations suggest that PFA at 180 mg/kg is sufficient to suppress HHV-6 replication. PFA at higher doses may be recommended not only for the treatment of HHV-6 encephalitis, but also for prophylaxis against HHV-6 reactivation. However, adverse effects of PFA including dose-dependent renal toxicity, electrolyte loss and frequent gastrointestinal toxicities make it difficult to recommend prophylactic administration of high-dose PFA in the wider SCT recipient population. Clinical trials using an increased dose of prophylactic PFA for a longer period may be warranted in patients at higher risk of HHV-6 encephalitis. Furthermore, efforts must be made to establish measures other than PFA prophylaxis to prevent HHV-6 encephalitis.
Several questions remain regarding the pathogenic mechanisms underlying HHV-6 encephalitis. Elucidation of these questions may contribute to the establishment of preventative strategies for HHV-6 encephalitis. First, many cases of HHV-6 encephalitis appear to develop after episodes of pre-engraftment immune reaction, engraftment syndrome or GVHD.3, 12, 14, 18 In patients who developed HHV-6 encephalitis, an IL 6 surge was observed 1 week before development of CNS dysfunction.12 If a hypercytokinemic state around the time of engraftment has a causative role in the development of HHV-6 encephalitis, intensive control of immune reactions around this period may reduce the incidence of HHV-6 encephalitis. Second, little is known about the pathogenesis of HHV-6 encephalitis after SCT. Whether HHV-6 reactivates within the CNS,21 and the primary region of HHV-6 reactivation in patients who progress to HHV-6 encephalitis have yet to be clarified. If HHV-6 reactivates primarily in peripheral blood or parotid gland and enters the CNS, CDV, the drug with the strongest in vitro activity against HHV-6,28 but poor CNS penetration, may be effective for preventing HHV-6 encephalitis. A lipid-ester derivative of CDV, hexadecyloxypropylcidofovir, may represent an alternative drug for HHV-6 prophylaxis.21 Third, the role of HHV-6 in the development of HHV-6 encephalitis has not been defined fully. MRI of patients with HHV-6 encephalitis commonly shows bilateral findings in the region of the limbic system. Such symmetrical findings suggest the existence of systemic processes rather than local infection. Furthermore, HHV-6-negative post-transplant acute limbic encephalitis has been reported.10 Such findings suggest the existence of multiple pathogenic mechanisms, including immune attack, underlying the CNS manifestations of HHV-6 encephalitis.
One could ask whether the incidence of HHV-6 encephalitis is really high among Japanese SCT recipients. In fact, all reports on the incidence of HHV-6 encephalitis (Table 1) have been retrospective studies. To clarify this issue, we are now undertaking a prospective multicenter study to evaluate the incidence of and risk factors underlying HHV-6 reactivation and HHV-6 encephalitis in Japan.
In conclusion, these data indicate that PFA given at 50 mg/kg in the early phase after allo-SCT is relatively ineffective strategy for preventing HHV-6 encephalitis. The pathogenesis of HHV-6 encephalitis deserves future investigation to establish safe and effective prophylactic measures against HHV-6 encephalitis. We hope the present results will be useful for future medical practice to prevent HHV-6 encephalitis.
References
Yoshikawa T, Asano Y, Ihira M, Suzuki K, Ohashi M, Suga S et al. Human herpesvirus 6 viremia in bone marrow transplant recipients: clinical features and risk factors. J Infect Dis 2002; 185: 847–853.
Zerr DM, Corey L, Kim HW, Huang ML, Nguy L, Boeckh M . Clinical outcomes of human herpesvirus 6 reactivation after hematopoietic stem cell transplantation. Clin Infect Dis 2005; 40: 932–940.
Ogata M, Kikuchi H, Satou T, Kawano R, Ikewaki J, Kohno K et al. Human herpesvirus 6 DNA load in plasma after allogeneic stem cell transplantation: incidence and clinical significance. J Infect Dis 2006; 193: 68–79.
Yamane A, Mori T, Suzuki S, Mihara A, Yamazaki R, Aisa Y et al. Risk factors for developing human herpesvirus 6 (HHV-6) reactivation after allogeneic hematopoietic stem cell transplantation and its association with central nervous system disorders. Biol Blood Marrow Transplant 2007; 13: 100–106.
De Bolle L, Naesens L, De Clercq E . Update on human herpesvirus 6 biology, clinical features, and therapy. Clin Microbiol Rev 2005; 18: 217–245.
Ogata M . Human herpesvirus 6 in hematological malignancies. J Clin Exp Hematop 2009; 49: 57–67.
Zerr DM . Human herpesvirus 6 and central nervous system disease in hematopoietic cell transplantation. J Clin Virol 2006; 37: 52–56.
Muta T, Fukuda T, Harada M . Human herpesvirus-6 encephalitis in hematopoietic SCT recipients in Japan: a retrospective multicenter study. Bone Marrow Transplant 2008; 43: 583–585.
Wainwright MS, Martin PL, Morse RP, Lacaze M, Provenzale JM, Coleman RE et al. Human herpesvirus 6 limbic encephalitis after stem cell transplantation. Ann Neurol 2001; 50: 612–619.
Seeley WW, Marty FM, Holmes TM, Upchurch K, Soiffer RJ, Antin JH et al. Post-transplant acute limbic encephalitis: clinical features and relationship to HHV-6. Neurology 2007; 69: 156–165.
Ogata M, Satou T, Kawano R, Goto K, Ikewaki J, Kohno K et al. Plasma HHV-6 viral load-guided preemptive therapy against HHV-6 encephalopathy after allogeneic stem cell transplantation: a prospective evaluation. Bone Marrow Transplant 2008; 41: 279–285.
Ogata M, Satou T, Kawano R, Takakura S, Goto K, Ikewaki J et al. Correlations of HHV-6 viral load and plasma IL-6 concentration with HHV-6 encephalitis in allogeneic stem cell transplant recipients. Bone Marrow Transplant 2010; 45: 129–136.
Fujimaki K, Mori T, Kida A, Tanaka M, Kawai N, Matsushima T et al. Human herpesvirus 6 meningoencephalitis in allogeneic hematopoietic stem cell transplant recipients. Int J Hematol 2006; 84: 432–437.
Mori Y, Miyamoto T, Nagafuji K, Kamezaki K, Yamamoto A, Saito N et al. High incidence of human herpes virus 6-associated encephalitis/myelitis following a second unrelated cord blood transplantation. Biol Blood Marrow Transplant 2010; 16: 1596–1602.
Sakai R, Kanamori H, Motohashi K, Yamamoto W, Matsuura S, Fujita A et al. Long-term outcome of human herpesvirus-6 encephalitis after allogeneic stem cell transplantation. Biol Blood Marrow Transplant 2011; 17: 1389–1394.
Ljungman P, de la Camara R, Cordonnier C, Einsele H, Engelhard D, Reusser P et al. European Conference on Infections in Leukemia. Management of CMV, HHV-6, HHV-7 and Kaposi-sarcoma herpesvirus (HHV-8) infections in patients with hematological malignancies and after SCT. Bone Marrow Transplant 2008; 42: 227–240.
Ishiwata K, Kato D, Uchida N, Tsuji M, Yamamoto H, Araoka H et al. HHV-6-associated limbic encephalitis after umbilical cord blood transplantation. Jpn J Clin Hematol 2009; 50: 209 (Abstr. OS1-45) (in Japanese).
Ueki T, Satou K, Shimizu I, Akahane D, Ueno M, Ichikawa N et al. Five cases of post-CBT myelitis presenting with severe pain and clinical signs of dysautonomia. Jpn J Clin Hematol 2010; 51: 234 (Abstr. OS-1-108).
Numata A, Tanaka M, Tachibana T, Ozawa E, Ishigatsubo Y, Maruyama I et al. Risk factors for developing human herpes virus-6 encephalitis and clinical significance of antiviral therapy in early phase after allogeneic hematopoietic stem cell transplantation. Program Book for the 33rd Annual Meeting of the Japan Society for Hematopoietic Cell Transplantation 2011 P291 (Abstr. WS2-12-2) (in Japanese).
Zerr DM, Fann JR, Breiger D, Boeckh M, Adler AL, Xie H et al. HHV-6 reactivation and its effect on delirium and cognitive functioning in hematopoietic cell transplantation recipients. Blood 2011; 117: 5243–5249.
Caserta MT, Dewhurst S . Dazed and confused by HHV-6. Blood 2011; 117: 5016–5018.
Salzberger B, Bowden RA, Hackman RC, Davis C, Boeckh M . Neutropenia in allogeneic marrow transplant recipients receiving ganciclovir for prevention of cytomegalovirus disease: risk factors and outcome. Blood 1997; 90: 2502–2508.
Reusser P, Gambertoglio JG, Lilleby K, Meyers JD, Phase . I-II trial of foscarnet for prevention of cytomegalovirus infection in autologous and allogeneic marrow transplant recipients. J Infect Dis 1992; 166: 473–479.
Bacigalupo A, Tedone E, Van Lint MT, Trespi G, Lonngren M, Sanna MA et al. CMV prophylaxis with foscarnet in allogeneic bone marrow transplant recipients at high risk of developing CMV infections. Bone Marrow Transplant 1994; 13: 783–788.
Rapaport D, Engelhard D, Tagger G, Or R, Frenkel N . Antiviral prophylaxis may prevent human herpesvirus-6 reactivation in bone marrow transplant recipients. Transpl Infect Dis 2002; 4: 10–16.
Tokimasa S, Hara J, Osugi Y, Ohta H, Matsuda Y, Fujisaki H et al. Ganciclovir is effective for prophylaxis and treatment of human herpesvirus-6 in allogeneic stem cell transplantation. Bone Marrow Transplant 2002; 29: 595–598.
Pellett PE, Ablashi DV, Ambros PF, Agut H, Caserta MT, Descamps V et al. Chromosomally integrated human herpesvirus 6: questions and answers. Rev Med Virol 2012; 22: 144–155.
De Clercq E, Naesens L, De Bolle L, Schols D, Zhang Y, Neyts J . Antiviral agents active against human herpesviruses HHV-6, HHV-7 and HHV-8. Rev Med Virol 2001; 11: 381–395.
Acknowledgements
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest or financial conflict with the subject matter or materials discussed in the manuscript. No writing assistance was utilized in the production of this manuscript. This work was supported in part by grants from the Japanese Ministry of Health, Labor and Welfare and a non-profit organization, the Infection Control Oita Network.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ogata, M., Satou, T., Inoue, Y. et al. Foscarnet against human herpesvirus (HHV)-6 reactivation after allo-SCT: breakthrough HHV-6 encephalitis following antiviral prophylaxis. Bone Marrow Transplant 48, 257–264 (2013). https://doi.org/10.1038/bmt.2012.121
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2012.121
Keywords
This article is cited by
-
Analysis of five cases of human herpesvirus-6 myelitis among 121 cord blood transplantations
International Journal of Hematology (2018)
-
Hyponatremia associated with human herpesvirus-6 (HHV-6) encephalitis after allogeneic hematopoietic stem cell transplantation: A presentation different from HHV-6 myelitis
International Journal of Hematology (2017)
-
Roseolovirus-associated encephalitis in immunocompetent and immunocompromised individuals
Journal of NeuroVirology (2017)
-
Human herpesvirus-6 encephalitis after allogeneic hematopoietic cell transplantation: What we do and do not know
Bone Marrow Transplantation (2015)
-
Human herpesvirus 6B reactivation and delirium are frequent and associated events after cord blood transplantation
Bone Marrow Transplantation (2015)