Abstract
To investigate the relationship between clinical response and modification of BK viremia, we assessed retrospectively 32 cases of hemorrhagic cystitis (HC) after allogeneic hematopoietic SCT that were treated with i.v. cidofovir (CDV). They were 22 men (69%) and 10 women (31%) with a median age of 24 years, range 3–62. The median number of CDV doses was 3, range 1–8, and the treatment lasted for a median of 3 weeks, range 1–10. Clinical improvement of HC was observed in 27 patients (84%). In 12 of 32 episodes (37.5%), BK viremia was determined before every CDV administration and a complete clinical response was observed in 10 of 12 patients (83%), the reduction of BK viremia load being ⩾1 log by 2 weeks after starting CDV. Nephrotoxicity related to CDV was observed in nine patients. Among 26 patients with 100-day follow-up, 4 of 4 patients who had a complete clinical response by 30 days were alive vs 16 of 22 (73%) who did not have the resolution of HC in this time frame. We conclude that in patients with HC, the response to CDV treatment is usually associated with a significant reduction of BK viremia load.
Similar content being viewed by others
Introduction
In allogeneic hematopoietic SCT (HSCT), hemorrhagic cystitis (HC) is a serious complication of the early post-engraftment period with a variable incidence from 3 to 70%1, 2, 3 but in more recent reports it has occurred in 20–30% of patients.4, 5, 6 Generally, HC is a painful complication that additionally prolongs the hospital stay for supportive measures, increases the need for blood transfusions, and, in the severe form, may obstruct the urinary tract. Moreover, its occurrence has been associated with an increased mortality.3, 5, 7 From a pathogenic point of view, the uncontrolled replication of BK virus (BKV) in the bladder mucosa in the first weeks after transplant together with the immunological reaction of acute GVHD seems to have a key role in triggering sudden-onset hematuria.8, 9 Cidofovir (CDV) is an acyclic nucleoside analog with broad spectrum antiviral activity.9, 10 Despite its modest in vitro activity against BKV,11 CDV is the drug most frequently used clinically to block BKV replication as shown in previous case reports or retrospective studies.9, 10, 12, 13 In a study of the Infectious Disease Working Party (IDWP) of the European Group for Blood and Marrow Transplantation (EBMT),—the largest series published so far—a clinical improvement or resolution of HC was found in 45 of 57 patients with HC treated with CDV (79%).14 The main issue is whether clinical resolution of HC is really influenced by treatment with CDV, as resolution or improvement of HC can also be observed in patients who received only supportive care.6 Indeed, limited data are available on virological response during CDV treatment.13, 14 For these reasons, we decided to extend the data collection on CDV-treated HC among EBMT centers. The aim was to further investigate the relationship between clinical response and BK viremia in CDV-treated patients.
Patients and methods
The study was approved by the IDWP scientific committee and presented to centers at the IDWP session of 2008 EBMT meeting. The study was conducted from August 2008 to December 2010 and involved centers that routinely determine BKV load on blood by quantitative PCR. To be included in data collection the following criteria were required: (a) episodes of HC in allogeneic HSCT patients, (b) concurrent BK viremia documented by quantitative PCR and (c) treatment of HC episodes with i.v. CDV. Given that the main objective of the study was to describe the variation of BK viremia load during CDV treatment, the episodes of HC in which BKV load was determined only in the urine or episodes of HC treated with intrabladder instillation of CDV were excluded. HC was defined as the occurrence of symptomatic or asymptomatic frank hematuria and its severity was classified according standard criteria, that is, grade II, macroscopic hematuria only, grade III, hematuria with intrabladder clots and grade IV, macroscopic hematuria with renal or bladder dysfunction.15 Follow-up data were as of 30 October 2011.
HC prevention and management
Hyperhydration, forced diuresis and urine alkalinization were used in all patients during the conditioning regimen as general preventative measures for drug-related chemical cystitis, while mesna (mercaptoethanesodium sulfonate) was given to patients receiving CY as part of the conditioning ablative regimen.
Neutrophil (polimorphonuclear) and platelet engraftment were defined as the first of 3 and 7 consecutive days on which neutrophil and platelet counts exceeded 0.5 × 109/L and 50 × 109/L, respectively.
Definition
The remission status of the underlying malignant disease was classified as controlled if the patient was in CR, PR, chronic phase (this last only for chronic myeloid leukemia patients) or who had a diagnosis of refractory anemia; in the remaining cases the underlying malignant disease was defined as uncontrolled. CR was defined as a complete clinical resolution of all symptoms of HC after CDV treatment, whereas PR was defined as a significant improvement of symptoms or of the grade of HC but hematuria persisted. Failure was considered as no improvement or worsening of HC. Standard criteria were used to define acute or chronic GVHD.16 Organ toxicity after CDV administration was graded according to World Health Organization toxicity scale. In particular, nephrotoxicity was scored according to serum creatinine level, as follows: grade I, <1.25, grade II, 1.26–2.5, grade III, 2.6–5 and grade IV, >5 of normal upper limit, respectively. Where appropriate, demographic, clinical and transplant characteristics were compared using χ2 or Fisher’s exact test for categorical variables. P significance was set at α=0.05.
Results
During the study period, 32 episodes of BKV–HC treated with CDV were recorded in 13 EBMT centers. None of these cases has previously been published. Twelve episodes (38%) occurred in patients <18 years of age. Table 1 shows the main transplant characteristics. The underlying disease was acute leukemia or myelodysplastic syndrome in 25 patients (78%), chronic malignancies such as multiple myeloma, chronic myeloid and/or lymphocytic leukemia in 3 patients (9%), Hodgkin lymphoma in 2 patients (6%) and non malignant diseases (beta-thalassemia, Chediak Higashi syndrome) in 2 patients (6%).
Table 2 shows the clinical and virological characteristics of 32 episodes of HC. Nineteen patients were treated with 5 mg/kg, 7 patients with 3 mg/kg and 6 patients with 0.5–1 mg/kg of CDV, respectively. Probenecid was associated to CDV in 23 patients, as follows: in 15 of 19 patients of 5 mg group, in 7 of 7 patients of 3 mg group, and in 1 of 6 patients of 0.5–1 mg group. The median number of CDV doses was 3, range 1–8, and the treatment lasted for a median of 3 weeks, range 1–10. Nephrotoxicity related to CDV was recorded in nine patients, as follows: grade I in four, grade II in three and grade III in two patients, respectively. Six patients received other treatment in addition to CDV, that is, ribavirin, 1 patient; ciprofloxacin, 1 patient; and hyperbaric oxygen therapy, 4 patients. Clinical improvement of HC was observed in 27 patients (84%).
In 12 of 32 episodes (37.5%), BKV load on blood was determined before every CDV dose. A complete clinical response was observed in 10 of them (83%). In these 10 patients the BKV load reduced by 1 log or more by 2 weeks from starting CDV. In the following weeks, the decrease in BKV load was continuous in five patients whereas transient rebounds were observed in five patients. Table 3 shows the main characteristics of 12 patients who were assessed for the clinical and virological response to CDV.
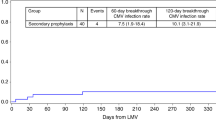
Among 26 patients followed-up to 100 days after HC, 4 of 4 patients who had a CR within 30 days from HC were alive at day 100 after HC vs 16 of 22 (73%) who did not have a resolution of HC in this time frame. After a median follow-up of 259 days, range 62–742, 22 patients (70%) were alive whereas 9 patients died of complications (4 multi-organ failure/acute respiratory distress syndrome, 3 infection and 2 GVHD) and 1 patient of disease progression.
Discussion
There is no clear consensus on how to treat HC after HSCT because several therapeutic measures (CDV, ribavirin, hyperbaric oxygen treatment, others) are still regarded as experimental.10 In most studies, the efficacy of CDV was based on the observation of clinical improvement or resolution of HC but, considering the uncontrolled nature of these studies, a spontaneous resolution of HC cannot be excluded. In a previous study, nearly all adult patients treated with CDV had a clinical response (16/19, 84%) but only 9 of 19 patients (47%) had a measurable viral load virological response defined by a reduction >1 log of BKV load on urine.13 The same results were found by other authors in pediatric patients, a clinical response and a virological response, determined by quantitative PCR on urine, being observed in 15 of 19 (79%) and in 6 of 19 patients (32%) of patients treated with CDV, respectively.4 Monitoring of BKV virological response on urine is difficult because both urine volume and viral excretion can vary over 24 h and BK load viruria can be higher than the upper limit of detection of the assay.13 Moreover, BK viruria in patients with HC is usually long lasting.5, 6 In a previous retrospective study, resolution of HC was associated with the complete clearance of BK viremia in 21 (81%) of 27 patients who had at least 1 BKV load determination after starting CDV in a median time of 37 days, while BK viruria became negative in only 20% of patients in a median time of 161 days.14 Although the determination of BKV load on blood is less sensitive than BKV load on urine, some data suggest that BK viremia load is more specific than BK viruria load.5, 17 In our study, the determination of BKV load on blood during CDV was reported in 12 of 32 patients with HC and a reduction of ⩾1 log by 2 weeks was found in all 10 patients with CR of HC, whereas no modification of BKV load was observed in the 2 non-responding patients. The parallel reduction of BKV load viremia ⩾2 logs was also reported previously in 7 of 10 patients with complete resolution of HC after CDV treatment, whereas in 3 patients the improvement was independent from the modification of BK load viremia.14 Despite the multifactorial pathogenesis of HC in allogeneic HSCT patients, these observations highlight the role of controlling BKV replication in the process of recovery from HC. Interestingly, the resolution of HC by day +30 from its beginning was associated with a better OS. In general, post transplant bleeding complications, including HC, have been reported as negative predictors for survival.18 In a single-center study on pediatric patients and in a retrospective study on adult and pediatric patients, the lack of recovery from HC has been associated with both a higher transplant-related mortality (72% vs 40%), and lower survival (43% vs 52%).3, 14 One issue still debated is the optimal dosage of CDV. Bernhoff et al.19 assessed the anti-viral effect of CDV in primary human renal proximal tubule epithelial cells and found that a concentration of CDV of 40 μg/mL reduced the BKV load by an average of 90%. At the same concentration, CDV determined a measurable host cell toxicity by reducing DNA replication and metabolic activity of 30% to 40% and of 20% to 30%, respectively. Therefore, the use of CDV has an intrinsic weakness because, at conventional or higher dosages, from 1 to 10 mg/kg, the peak plasma concentration of CDV is inferior to the effective concentration against BKV in vitro.19, 20 Moreover, to reduce the risk of renal tubular toxicity, probenecid is generally associated with CDV when it is used at dosage of 3–5 mg/kg every 1–2 weeks while lower doses of 1 mg/kg 1–3 times a week without probenecid was shown to be efficacious and safe in single-center series.13, 21 Esterification of CDV with lipid ester derivative (hexadecyoxypropil, octadecyloxyethil and oleyloxyethil) has been shown to increase the efficacy of antiviral therapy against CMV and other vaccinia viruses and to decrease the effective concentration for BKV.12, 22 Rinaldo et al.23 demonstrated that the lipid conjugate 1-O-hexadecyloxypropyl CDV (CMX001) had a higher BKV-inhibitory potency compared with that of the parent compound CDV. This compound, orally administrable, showed the capacity to reduce the BKV replication by 90% at about 400-times lower concentration than CDV with a more rapid ad enduring effect and fewer side effects on host cells. In a recent small series, CMX001, the hexadecyloxypropyl ester-derivative of CDV, was administered, on a compassionate basis, to 12 transplanted patients affected by severe adenovirus infection after failure of i.v. CDV. By week 8 of treatment, nine patients (69%) had a significant virological response without any serious adverse event recorded during treatment. This result was associated with a better survival.24
In conclusion, in patients with HC, clinical response to CDV is associated with a significant reduction of BK viremia load. This may contribute to the recovery of HC although the role of other factors in this process, such as type and grade of immunosuppression, the level of recipient and donor BKV-specific immunity, earlier time of intervention, remains a matter of investigation. Prospective studies are needed to reduce the uncertainty on this topic and give more solid evidence of the role of CDV in the treatment of BKV–HC beyond its off-label, compassionate use.
References
Arthur RR, Shah KV, Baust SJ, Santos GW, Saral R . Association of BK viruria with hemorrhagic cystitis in recipients of bone marrow transplants. New Engl J Med 1986; 315: 230–234.
Vose JM, Reed EC, Pippert GC, Anderson JR, Bierman PJ, Kessinger A et al. Mesna compared with continuous bladder irrigation as uroprotection during high-dose chemotherapy and transplantation: a randomized trial. J Clin Oncol 1993; 11: 1306–1310.
Cesaro S, Brugiolo A, Faraci M, Uderzo C, Rondelli R, Favre C et al. Incidence and treatment of hemorrhagic cystitis in children given hematopoietic stem cell transplantation: a survey from the Italian Association of Pediatric Hematology Oncology-Bone marrow Transplantation Group. Bone Marrow Transplant 2003; 32: 925–931.
Gorczynska E, Turkiewicz D, Rybka K, Toporski J, Kalwak K, Dyla A et al. Incidence, clinical outcome, and management of virus-induced hemorrhagic cystitis in children and adolescents after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2005; 11: 797–804.
Cesaro S, Facchin C, Tridello G, Messina C, Calore E, Biasolo MA et al. A prospective study of BK-virus-associated haemorrhagic cystitis in paediatric patients undergoing allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2008; 41: 363–370.
Gaziev J, Paba P, Miano R, Germani S, Sodani P, Bove P et al. Late-onset hemorrhagic cystitis in children after hematopoietic stem cell transplantation for thalassemia and sickle cell anemia: a prospective evaluation of polyoma (BK) virus infection and treatment with cidofovir. Biol Blood Marrow Transplant 2010; 16: 662–671.
Cheuk DK, Lee TL, Chiang AK, Ha SY, Lau YL, Chan GC . Risk factors and treatment of hemorrhagic cystitis in children who underwent hematopoietic stem cell transplantation. Transpl Int 2007; 20: 73–81.
Leung AY, Yuen KY, Kwong YL . Polyma BK virus and hemorrhagic cystitis in hematopoietic stem cell transplantation: a changing paradigm. Bone Marrow Transplant 2005; 36: 929–937.
Hirsch HH . BK virus: opportunity makes a pathogen. Clin Infect Dis 2005; 41: 354–360.
Hassan Z . Management of refractory hemorrhagic cystitis following hematopoietic stem cell transplantation in children. Pediatr Transplant 2011; 15: 348–361.
Farasati NA, Shapiro R, Vats A, Randhawa P . Effect of leflunomide and cidofovir on replication of BK virus in an in vitro culture system. Transplantation 2005; 79: 116–118.
Rinaldo Hanssen C, Hirsch HH . Antivirial for the treatment of polyomavirus BK replication. Expert Rev Anti Infect Ther 2007; 5: 105–115.
Savona MR, Newton D, Frame D, Levine JE, Mineishi S, Kail DR . Low-dose cidofovir treatment of BK virus associated hemorrhagic cystitis in recipients of hematopoiietic stem cell transplant. Bone Marrow Transplant 2007; 39: 783–787.
Cesaro S, Hirsch HH, Faraci M, Owoc-Lempach J, Beltrame A, Tendas A et al. Cidofovir for BK virus associated hemorrhagic cystitis: a retrospective study. Clin Infect Dis 2009; 49: 233–240.
Droller MJ, Saral R, Santos G . Prevention of cyclophoshamide-induced hemorrhagic cystitis. Urology 1982; 20: 256–258.
Apperley J, Carreras E, Gluckman E, Gratwohl A, Masszi T . Hematopoietic stem cell transplantation. In:. The EBMT Handbook 5th edn. EBMT and ESH. Forum Service Editore: Genova, Italy, 2008.
Erard V, Kim HW, Corey L, Limaye A, Huang ML, Myerson D et al. BK DNA viral load in plasma: evidence for an association with hemorrhagic cystitis in allogeneic hematopoietic cell transplant recipients. Blood 2005; 106: 1130–1132.
Nevo S, Enger C, Swan V, Wojno KJ, Fuller AK, Altomonte V et al. Acute bleeding after allogeneic bone marrow transplantation: association with graft versus host disease and effect on survival. Transplantation 1999; 67: 681–689.
Bernhoff E, Gutteberg TJ, Sandvik K, Hirsch HH, Rinaldo HC . Cidofovir inhibits polyomavirus BK replication in human renal tubular cells downstream of viral early gene expression. Am J Trasplant 2008; 8: 1413–1422.
Cundy KC, Petty BG, Flaherty J, Fisher PE, Polis MA, Wachsman M et al. Clinical pharmacokinetics of cidofovir in human immunodeficiency virus-infected patients. Antimicrob Agents Chemother 1995; 39: 1247–1252.
Faraci M, Cuzzubbo D, Lanino E, Di Marco E, Cirillo C, Dallorso S et al. Low dosage cidofovir without probenecid as treatment for BK virus hamorrhagic cystitis after hemopoietic stem cell transplant. Pediatr Infect Dis J 2009; 28: 55–57.
Randhawa P, Farasati NA, Shapiro R, Hostetler KY . Ether lipid ester derivatives of cidofovir inhibit polyomavirus BK replication in vitro. Antimicrob Agents Chemother 2006; 50: 1564–1566.
Rinaldo CH, Gosert R, Bernhoff E, Finstad S, Hirsch HH . 1-O-hexadecyloxypropyl cidofovir (CMX001) effectively inhibits polyomavirus BK replication in primary human renal tubular epithelial cells. Antimicrob Agents Chemother 2010; 54: 4714–4722.
Florescu DF, Pergam SA, Neely MN, Qiu F, Johnston C, Way S et al. Safety and efficacy of CMX001 as salvage therapy for severe adenovirus infections in immunocompromised patients. Biol Blood Marrow Transplant 2012; 18: 731–738.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cesaro, S., Pillon, M., Tridello, G. et al. Relationship between clinical and BK virological response in patients with late hemorrhagic cystitis treated with cidofovir: a retrospective study from the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant 48, 809–813 (2013). https://doi.org/10.1038/bmt.2012.247
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2012.247
Keywords
This article is cited by
-
Intravesical application of platelet-rich plasma in patients with persistent haemorrhagic cystitis after hematopoietic stem cell transplantation: a single-centre preliminary experience
International Urology and Nephrology (2019)
-
Single-agent GvHD prophylaxis with tacrolimus after post-transplant high-dose cyclophosphamide is a valid option for haploidentical transplantation in adults with hematological malignancies
Bone Marrow Transplantation (2017)
-
Patterns of infection and infection-related mortality in patients with steroid-refractory acute graft versus host disease
Bone Marrow Transplantation (2017)
-
Fulminating Hemorrhagic Cystitis: New Trends from Etiology to Treatment
Current Bladder Dysfunction Reports (2015)