Many regions of the world have experienced the pandemic in punishing waves, but Chennai in India endured a six-month flood, according to Bharath Kumar Tirupakuzhi Vijayaraghavan. The Apollo Main Hospital, where Vijayaraghavan works as an intensive-care specialist, was never overwhelmed, but it was relentlessly busy. And although the numbers of people with COVID-19 finally began to fall in mid-October, Vijayaraghavan worries about the possible impact of the festival season, which began on 20 October, and the public’s waning compliance with health measures. “Everybody is exhausted,” he says. “It’s become a never-ending health-care problem.”
One shining light that he can point to is his intensive-care unit’s dwindling fatality rate. In April, up to 35% of those in the unit with COVID-19 perished, and about 70% of those on ventilators died. Now, the intensive-care mortality rate for people with the illness is down to 30%, and for those on ventilators it is around 45–50%. “This itself was a relief,” says Vijayaraghavan.
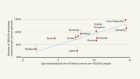
Around the world, similar stories are emerging. Charlotte Summers, an intensive-care physician at the University of Cambridge, UK, says that data collected by the country’s National Health Service (NHS) show a decline in death rates1 (see ‘Mortality falls’). Critical-care physician Derek Angus at the University of Pittsburgh in Pennsylvania says that his hospital’s statistics team also saw reductions over time. “Without question, we’ve noticed a drop in mortality,” says Angus. “All things being equal, patients have a better chance of getting out alive.”

Source: Ref. 1
The reasons are not entirely obvious. There have been no miracle drugs, no new technologies and no great advances in treatment strategies for the disease that has infected more than 50 million and killed more than 1.2 million around the world. Shifts in the demographics of those being treated might have contributed to perceived boosts in survival. And at many hospitals, it seems clear that physicians are getting incrementally better at treating COVID-19 — particularly as health-care systems become less overwhelmed. Still, those gains could be erased by increasing case loads around the world.
Vijayaraghavan credits the improvements in mortality at his institution to hard-earned experience, a better understanding of how to use steroids and a shift away from unproven drugs and procedures.
Marcus Schultz, an intensive-care specialist at Amsterdam University Medical Center in the Netherlands, agrees, adding that it took time to realize that standard treatments were among the most effective. “In just half a year, I think we repeated 20 years of research in acute respiratory distress,” he says. “Everything was done again, and everything came with the same result.”
Crunching the numbers
Researchers have struggled to work out whether the COVID-19 death rates are truly dropping. The calculations can be complex. Case-fatality rates depend on testing: a country that tests only people with severe symptoms, for example, will have an outsized case-fatality rate compared with one in which asymptomatic testing is widespread. And fatality rates in intensive-care units can mislead if the demographics of the people admitted change over time. For example, many hospitals reported high numbers of younger patients as the pandemic wore on.
Coronavirus blood-clot mystery intensifies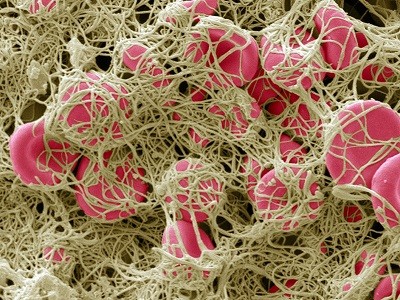
The detailed data that are needed to parse these differences have been hard to come by in many countries, and that frustrates Andrew Levin, an economist at Dartmouth College in Hanover, New Hampshire. “We still don’t have the data that scientists and public-health officials should have,” he says.
As a result, it has taken researchers some time to determine whether the number of deaths per SARS-CoV-2 infection is really falling, particularly for older people, says epidemiologist Ali Mokdad at the University of Washington in Seattle. Mokdad and his colleagues have been monitoring global data, with a focus on the United States and Europe. A provisional analysis, he says, which includes data from the American Hospital Association, now suggests that the number of fatalities per infection might have fallen by 20%.
Intensive-care physicians say that treatment has improved, but not always in ways that are easy to pinpoint. Vijayaraghavan and others credit a shift in mindset. In the early days of the pandemic, COVID-19 was viewed as something frightening and new — and worthy of resorting to unproven interventions in a desperate act to save patients. “Unfortunately, a lot of the initial discourse was complicated by noise about how this disease was entirely different or entirely new,” says Vijayaraghavan. “This distraction caused more harm — we were all probably poised to go off track.”
Summers points to the furore around hydroxychloroquine, a malaria drug that some initial studies suggested might help to treat COVID-19. The possibility set off a run on the drug, with some physicians and politicians advocating its use without strong evidence that it was effective. In June, a large study in the United Kingdom2 showed that the drug did not benefit people hospitalized with COVID-19. Meanwhile, that study and others suggested that hydroxychloroquine could be harming some patients, in particular by causing heart damage, and especially when combined with the antibiotic azithromycin3. Hundreds of hydroxychloroquine clinical trials were launched, wasting resources and effort that could have been directed elsewhere, says Summers. “In terms of hospitalized patients, hydroxychloroquine is dead,” says Summers. “That’s one less thing for us to worry about.”
Chasing miracles
Intensive-care physicians point to early concerns about the increased production of proteins called cytokines that can rev up immune responses in some people with severe COVID-19. This phenomenon, known as a ‘cytokine storm’, stimulated interest in using targeted therapies to dampen immune responses. Vijayaraghavan says that this prompted some physicians in India to treat COVID-19 with tocilizumab, an antibody that blocks the activity of the cytokine interleukin-6 (IL-6). But, he says, the treatment might have made patients more susceptible to other infections, a particular risk in regions where drug-resistant bacteria are common.
Chloroquine hype is derailing the search for coronavirus treatments
Since then, additional studies have shown that, although IL-6 levels are raised in some people with severe COVID-19 compared with healthy individuals or those with mild infections, they are not elevated when compared with others with acute respiratory distress4. Researchers have been looking — without success — at targeted ways to dampen immune responses in critically ill people for decades, says Angus. “And we have 20 to 30 years of failing to improve outcome with therapies that try to block the cytokine cascade.”
Some studies have borne out Angus’s pessimism. A test of another IL-6-blocking antibody called sarilumab in the United States was halted because it showed no benefit, and a study of tocilizumab also found no effect on COVID-19 death rates5. A large, randomized, controlled clinical trial of tocilizumab taking place in the United Kingdom should have a result before the end of December, says Summers.
In contrast to more-targeted drugs, blanket suppression of the immune system using steroids has been shown to cut death rates when used to treat severe COVID-19. On 16 June, the UK RECOVERY trial found that a common steroid called dexamethasone could reduce COVID-19 fatalities by as much as one-third when administered to patients who require supplemental oxygen or are on ventilators6. (However, Summers cautions that dexamethasone treatment has not been shown to carry a benefit for people with mild COVID-19 who do not need oxygen support, possibly because it weakens defences against the virus itself.)
Hopes rise for coronavirus drug remdesivir
Some intensive-care physicians were already giving low doses of dexamethasone to critically ill patients as part of their standard treatment for acute respiratory distress, but the safety of that approach was debated. The RECOVERY trial results encouraged more to use the drugs, and the doses were low enough that infections did not increase, says Vijayaraghavan.
Thus far, steroids are the only medicine that has been shown to have a dramatic effect on COVID-19 mortality. “Anyone who’s very sick should get steroids,” says Angus. “And everything else is a crapshoot.”
The antiviral drug remdesivir, developed by the biopharmaceutical company Gilead Sciences in Foster City, California, has been shown by a US National Institutes of Health study to shorten hospital stays7. A subsequent trial coordinated by the World Health Organization found that the drug had little, if any, effect on mortality, but the US Food and Drug Administration nevertheless approved it for treating COVID-19 on 22 October.

Many experimental treatments, such as blood plasma taken from those who have recovered from COVID-19, have not proved to be effective.Credit: Lindsey Wasson/Reuters
Hundreds of other therapies are being tested against COVID-19, but many of the ongoing trials are too small to yield convincing results soon. Among the furthest along are studies of antibodies against SARS-CoV-2 — either purified antibodies administered individually or in cocktails, or antibody-rich blood plasma taken from people recovering from the disease.
Convalescent plasma studies have been hampered in the United States by the widespread availability of the treatment outside clinical trials, but the UK RECOVERY trial hopes to have data on this approach from a large, randomized, controlled trial this year. Meanwhile, a 464-person, open-label study in India found that convalescent plasma did not prevent moderate COVID-19 from progressing to severe disease or reduce deaths8.
Tests of purified antibodies are also under way — such as those assessing the mixture of two antibodies produced by the biotechnology firm Regeneron Pharmaceuticals in Tarrytown, New York, that was administered to US President Donald Trump. These mainly target people who have mild COVID-19 symptoms. Despite Trump’s claims that the treatment was a “cure”, large trials of the cocktail have not yet been completed, and there is no evidence that it has an impact on death rates from COVID-19.
Some studies in people with mild disease have shown that treatment with these antibodies can reduce hospitalizations. However, in October, the US National Institutes of Health halted a trial of an antibody produced by the pharmaceutical company Eli Lilly in Indianapolis, Indiana, in people hospitalized with COVID-19 after finding no benefit from the treatment. Regeneron has also stopped enrolment in a trial of its antibody cocktail for people with severe symptoms.
Researchers are also looking to find out whether drugs that prevent blood clots — an unexpected hallmark of COVID-19 — could be given at higher doses or earlier during infection.
Angus would like to see studies that test combinations of these treatments. He is an investigator for REMAP-CAP (Randomised, Embedded, Multi-factorial, Adaptive Platform Trial for Community-Acquired Pneumonia), a trial that spans more than 260 sites in 19 countries and is designed to allow treatments to be added or dropped. “For example, remdesivir might be better in the presence of steroids,” he says. “We need trials that simultaneously randomize several choices.”
Back to basics
Some intensive-care researchers are sceptical of the chances that a highly effective medicine will be found, citing decades of failed attempts to find a ‘magic bullet’ for acute respiratory distress. “Apart from a vaccine, I think the differences in outcome will be driven by things like other ways to supply oxygen or help patients in their gas exchange,” says Schultz.
In the early days of the pandemic, physicians were alarmed by the rapid deterioration of some people with COVID-19, says Eddy Fan, an intensive-care physician at University Health Network in Toronto, Canada. “There were a lot of unknowns about the best way to manage this,” he says. “Because the patient could deteriorate very quickly, the thought was to put them on a ventilator and breathing tube quickly to prevent deterioration.”
But, in retrospect, clinicians might have been overzealous at times. Schultz recalls asking patients to get off of their mobile phones so he could put them on a ventilator, but a candidate for a ventilator normally wouldn’t be well enough to hold a telephone conversation. As physicians became more comfortable treating people with COVID-19, many realized that early ventilation was not necessary, says Fan.
Evidence lags behind excitement over blood plasma as a coronavirus treatment
Unfortunately, the public began to become concerned that ventilators themselves were causing harm, says Summers. Now, she says, families are upset when physicians recommend that their loved ones be put on a ventilator — even when there are no other suitable ways of providing oxygen. “The narrative you’ve heard is that ventilators kill people,” she says. “That’s been particularly unhelpful.” The NHS health-care centres with the lowest mortality rates during the pandemic used ventilators, but not too early. They followed standard protocols for when to use the devices, says Summers.
Ultimately, Summers and others attribute possible drops in death rates more to shoring up standard health-care practices than to medical advances. “It’s the little subtle things,” says Angus.
This might mean that keeping death rates low could hinge on measures to reduce transmission. In Singapore, where COVID-19 death rates are among the lowest in the world, intensive-care physician Jason Phua at Alexandra Hospital says the key to the country’s success has been suppressing transmission, so that hospitals were never overwhelmed. Early reports of mortality from Wuhan approached 97% for people with COVID-19 who were on ventilators, he says. In Singapore, mortality rates in intensive-care units have been less than 15%. “I don’t think it’s because we are using the correct drugs,” he says. “I think what’s happening is that the others are overwhelmed.”
In response to the pandemic, many hospitals rapidly expanded their numbers of intensive-care beds, but that meant bringing in extra staff from other departments. Over time, those staff members have become more familiar with intensive care, learning to recognize the patterns that can signal when a patient is about to deteriorate. And hospitals have learnt to triage those who have risk factors for more severe disease, placing them under more careful observation.
Ultimately, reducing the COVID-19 death rate by 10–20% would feel like a huge win in an intensive-care ward, says Levin. But that would still leave the number of deaths relatively high, particularly among older people, in whom the case-fatality rate approaches 30% for those more than 80 years old. Instead, he says, suppressing transmission is the best way to reduce COVID-19 deaths: “In the grand scheme of things, from a public-policy angle, we need to say, ‘Let’s make sure that people in their 70s and 80s don’t get infected.’”


 Hopes rise for coronavirus drug remdesivir
Hopes rise for coronavirus drug remdesivir
 Chloroquine hype is derailing the search for coronavirus treatments
Chloroquine hype is derailing the search for coronavirus treatments
 Evidence lags behind excitement over blood plasma as a coronavirus treatment
Evidence lags behind excitement over blood plasma as a coronavirus treatment
 Coronavirus blood-clot mystery intensifies
Coronavirus blood-clot mystery intensifies