Abstract
Background/Objectives:
This study explored the association between serum 25-hydroxyvitamin D (25(OH)D) or parathyroid hormone (PTH) concentrations and the risk of metabolic syndrome (MetS) in middle-aged and older Korean adults using the most recent, nationally representative survey data.
Subjects/Methods:
The study sample consisted of 2624 Korean adults (⩾50 years old) who participated in the fifth Korean National Health and Nutrition Examination Surveys. Serum 25(OH)D was measured by radioimmunoassay and serum PTH was measured using chemiluminescence assay. MetS was defined according to the joint interim statement of the International Diabetes Federation and the American Heart Association/National Heart, Lung, and Blood Institute.
Results:
Serum 25(OH)D concentrations were significantly lower in subjects with MetS than in subjects without MetS, and the prevalence of MetS significantly decreased according to quartiles of serum 25(OH)D concentration. Serum 25(OH)D concentrations were negatively associated with the risk of elevated blood pressure (P for trend= 0.039), hypertriglyceridemia (P for trend=0.0474) and reduced high-density lipoprotein cholesterol (P for trend= 0.0139), whereas serum PTH concentrations were positively associated with the risk of elevated blood pressure (P for trend=0.0002) after adjusting for age, gender, residential district, education level, income, smoking status, body mass index, alcohol intake and physical activity. Furthermore, serum 25(OH)D concentrations were inversely associated with the risk of MetS after adjusting for confounding factors (P for trend=0.0163). However, serum PTH concentrations were not associated with the risk of MetS.
Conclusion:
Serum 25(OH)D concentration may be an independent risk factor of MetS among middle-aged and older Korean adults.
Similar content being viewed by others
Introduction
Vitamin D is a fat-soluble vitamin that can be produced in the skin following sun exposure, or ingested through diet and supplementation. Evidence suggests that 25-hydroxyvitamin D (25(OH)D), a generally accepted indicator of vitamin D status, is associated with insulin resistance, obesity and dyslipidemia, along with its role in calcium homeostasis and bone metabolism.1,2 Some recent epidemiologic studies have suggested that 25(OH)D status is inversely associated with metabolic syndrome (MetS) or its components,3, 4, 5, 6, 7 whereas other studies have produced conflicting results.8,9 MetS is a cluster of metabolic risk factors including abdominal obesity, hypertension, dyslipidemia and hyperglycemia, all of which are associated with an increased risk of developing cardiovascular disease.10 Some studies have indicated that parathyroid hormone (PTH), an important calcium-regulating hormone, is positively correlated with MetS and its components;9,11 other studies reported no association between PTH and MetS.4,12
Although ethnic differences could affect vitamin D metabolism and levels,13 evidence of an association between 25(OH)D, PTH and MetS in Asian populations is very limited. The fourth Korean National Health Nutrition and Examination Survey (KNHANES IV-2), conducted in 2008, found that the prevalence of vitamin D deficiency (<50 nmol/l) was 56% in Korean adults aged >19 years. Furthermore, Koreans, especially adults and the elderly aged ⩾50 years, have low dietary intakes of dairy calcium and vitamin D compared with people from Western countries because Koreans have a high prevalence of lactose intolerance and traditionally do not consume dairy.10 The prevalence of MetS is rapidly increasing in Korean adults14 because of changes in dietary habits15 and a reduction in physical activity.
According to data from the KNHANES III, 33.1% of Korean men and 26.1% of Korean women aged ⩾30 years had MetS based on the National Cholesterol Education Program Adult Treatment Panel III criteria.10 We hypothesized that vitamin D deficiency and increased PTH level might be associated with MetS in the Korean adults. Thus, it is critical to identify the association between 25(OH)D, PTH and MetS in older Korean populations.
To the best of our knowledge, this is the first population-based study to explore the association of both serum 25(OH)D and PTH levels with MetS in a Korean population.
The present study investigated the association between serum 25(OH)D and PTH levels and MetS in middle-aged and older Korean adults using the most recent nationally representative survey data.
Materials and methods
Study population
The study was based on the fifth KNHANES (V-1), a cross-sectional and nationally representative survey carried out by the Korean Center for Disease Control and Prevention (CDC) from October to December 2010. The survey used a stratified multistage probability sampling design. Of the 8958 Koreans who participated in the original health examination study, 3273 adults aged ⩾50 years were selected for the present study. However, 649 were then excluded because socioeconomic, anthropometric or biochemical data were lacking. Ultimately, 2624 Korean adults (1172 men and 1452 women) were eligible for the analysis and constituted the study cohort. Informed written consent for participation was obtained from all study subjects. In addition, the study was approved by the Korea CDC Institutional Review Board.
Measurements
Height and body weight were measured as part of the health examination. Body mass index (BMI) was calculated from measured height and weight. Waist circumference was measured to the nearest 0.1 cm at the narrowest point between the lowest rib and the uppermost lateral border of the right iliac crest. Blood pressure was measured with a Baumanometer mercury sphygmomanometer (WA Baum, Copiague, NY, USA) after subjects had rested for 5 min in a sitting position. Systolic and diastolic blood pressures (SBP and DBP) were measured at phase I and V Korotkoff sound,16 respectively. Three SBP and DBP readings were recorded, and the average of the last two readings was used for data analysis. The blood samples used to measure fasting plasma glucose, triglycerides (TGs), high-density lipoprotein cholesterol (HDL-C), insulin, 25(OH)D and PTH in serum were collected after an overnight fast. All biochemical analyses were carried out within 2 h of blood sampling. Fasting plasma glucose, TGs and HDL-C were measured enzymatically using a Hitachi automatic analyzer 7600 (Hitachi, Tokyo, Japan). Insulin was measured using a gamma-Counter (1470 WIZARD gamma-counter, PerkinElmer, Turku, Finland) with immunoradiometric assay (INS-IRMA, Biosource, Nivelles, Belgium). Serum 25(OH)D concentrations were measured using a gamma counter (1470 WIZARD gamma-counter, PerkinElmer) with a radioimmunoassay (25-Hydroxyvitamin D 125I RIA kit; DiaSorin, Stillwater, MN, USA).17 All intra- and interassay coefficients of variation for 25(OH)D were <12.5% and <11%, respectively. Serum PTH concentrations were measured using LIAISON (DiaSorin) and a chemiluminescence immunoassay (N-tact PTH assay; DiaSorin) measured intact PTH.18 All intra- and interassay coefficients of variation for PTH were <5.3% and <6.3%, respectively.
Definition of metabolic syndrome
MetS was defined according to the joint interim statement issued by the International Diabetes Federation and the American Heart Association/National Heart, Lung, and Blood Institute. This statement defines a person with MetS as an individual who meets three or more of the following criteria:19 abdominal obesity (waist circumference >90 cm for men or >80 cm for women); elevated blood pressure (SBP/ DBP ⩾130/85 mmHg) or daily use of antihypertensive medication; hyperglycemia (fasting plasma glucose ⩾5.5 mmol/l) or current use of insulin or oral hypoglycemia medication or a physician’s diagnosis of hypertriglyceridemia (TG ⩾1.7 mmol/l) or low HDL-C (HDL-C <1.04 mmol/l in men or <1.30 mmol/l in women).
Covariates
Information about lifestyle factors was obtained using a self-administered questionnaire and verified by personal interview. Subjects were categorized as living in either an urban or rural residential district. Seoul, its surrounding metropolitan area (Gyeonggi) and six other metropolitan cities (Busan, Daegu, Incheon, Gwangju, Daejeon and Ulsan) in South Korea were considered urban areas. The remaining regions (Gangwon, Chungbuk, Chungnam, Jeonbuk, Jeonnam, Gyeonbuk, Gyeongnam and Jeju) were considered rural areas. Education levels were categorized into three groups: ⩽6 years (elementary school level), 6–12 years (high school level) and ⩾12 years (college level). Smoking status was classified as nonsmoker, former smoker (for at least 1 year) or current smoker. Alcohol intake was assessed by a questionnaire regarding the frequency of alcohol use during the previous year; responses were then converted into alcohol intake per week. Alcohol intake was used to categorize the participants into three groups: nondrinker, light or moderate drinker (<2 times/week) and heavy drinker (⩾2 times/week). Physical activity was categorized two groups: regular physical activity group (hard exercise for ⩾20 min/session, ⩾5 sessions/week; moderate exercise for ⩾30 min/session ⩾5 sessions/week; or walking for ⩾30 min/sessions ⩾5 sessions/week) or nonregular physical activity group.
Statistical analyses
Data are expressed as numbers and percentages, or as mean±s.d. Differences between subjects with MetS and those without MetS were evaluated using the Wilcoxon rank sum test or the χ2-test, as appropriate. Differences among the four groups according to quartiles of serum 25(OH)D level were determined using a generalized linear model (Duncan’s test of multiple comparisons). Multivariable-adjusted logistic regression analysis was conducted to determine odds ratios (ORs) and 95% confidence intervals (CIs) for the risk of MetS or its components across quartiles of serum 25(OH)D or PTH levels. Statistical analyses were performed with SAS version 8.2 (SAS Institute, Cary, NC, USA). The P-values of <0.05 were considered statistically significant.
Results
The characteristics of the study population according to the presence of MetS are shown in Table 1. Subjects with MetS were more likely to be older, to be women and less likely to be educated. Subjects with MetS were also more likely to have higher BMI, waist circumference, blood pressure, fasting plasma glucose and TG, and lower levels of HDL-C. Furthermore, subjects with MetS had lower levels of serum 25(OH)D. However, serum PTH did not differ between subjects with and without MetS.
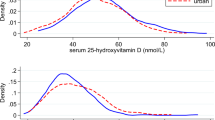
Characteristics of subjects according to quartiles of serum 25(OH)D concentration are provided in Table 2. Subjects with higher levels of serum 25(OH)D were more likely to be men, to drink alcohol and to exercise regularly, and were less likely to smoke and to live in a rural area. Higher serum 25(OH)D concentrations were significantly associated with lower BMI and SBP. Furthermore, MetS prevalence and serum PTH concentration decreased significantly according to quartiles of serum 25(OH)D.
ORs and 95% CIs for MetS components according to quartiles of serum 25(OH)D are summarized in Table 3. Adjusted ORs for elevated blood pressure (P for trend=0.039), hypertriglyceridemia (P for trend=0.047) and reduced HDL-C (P for trend=0.014) decreased with increasing serum 25(OH)D concentrations. Adjusted OR for elevated blood pressure (P for trend=0.0002) increased across the quartiles of serum PTH levels, whereas the adjusted OR for hypertriglyceridemia (P for trend=0.0032) tended to decrease across the quartiles of serum PTH levels.
The ORs and 95% CIs for MetS according to quartiles of serum 25(OH)D or PTH concentrations are summarized in Table 4. The unadjusted OR for MetS significantly decreased with increasing serum 25(OH)D (OR=0.71, 95% CI: 0.57–0.88 for comparisons of lowest vs highest quartile; P for trend=0.0003). This association remained unchanged after adjusting for potential confounders such as age, gender, residential district, education level, income, smoking status, BMI, alcohol intake and physical activity (OR=0.76, 95% CI: 0.59–0.98 for comparisons of lowest vs highest quartile; P for trend=0.016). However, serum PTH concentrations were not significantly associated with MetS risk.
Discussion
This study found a strong association between serum 25(OH)D concentrations and MetS in middle-aged and older Korean adults using the most recent nationally representative survey data. Serum 25(OH)D concentrations were significantly lower in subjects with MetS than those without MetS, and the prevalence of MetS decreased significantly according to quartiles of serum 25(OH)D. Serum 25(OH)D concentrations were negatively associated with the risk of elevated blood pressure, hypertriglyceridemia and reduced HDL-C after adjusting for potential risk factors such as age, gender, residential district, education level, income, smoking status, BMI, alcohol intake and physical activity. Furthermore, serum 25(OH)D concentrations were inversely associated with the risk of MetS after adjusting for confounders. However, serum PTH levels were not significantly associated with MetS risk, although they were significantly associated with the risk of elevated blood pressure and hypertriglyceridemia. These results suggest that serum 25(OH)D may be an independent risk factor of MetS among middle-aged and older Korean adults.
The present finding that serum 25(OH)D was strongly associated with the risk of MetS is consistent with previous studies. Among 8421 US subjects aged ⩾20 years, adjusted ORs for MetS, abdominal obesity, hypertriglyceridemia and hyperglycemia significantly decreased across increasing quintiles of serum 25(OH)D concentrations.3 Li et al.20 also reported that in 1390 Chinese adults aged 20–82 years, a 10 nmol/l increase in serum 25(OH)D was associated with a 10% lower risk of MetS. This same study found that serum 25(OH)D was negatively associated with high TG and reduced risk of HDL-C. In a prospective study of 4330 individuals aged 30–60 years, at 5-year follow-up, serum 25(OH)D levels were inversely associated with incidence rates of MetS and hypercholesterolemia.1 In contrast, George et al.21 showed a lack of association between serum 25(OH)D and MetS for Africans and Asian Indians. One previous study reported no association between serum 25(OH)D and MetS in Korean adults aged ⩾19 years.8 However, the two studies cannot be compared directly owing to differences on the age of participants and sample collection period (over four seasons) that might affect the relationship between serum 25(OH)D and MetS.
Vitamin D may affect the risk of developing MetS and its components through several mechanisms. The present findings show that vitamin D seems to be related to lipid profiles and blood pressure. Vitamin D might influence serum TG through an increase of intestinal calcium absorption that may ultimately reduce hepatic TG formation and/or secretion via an effect on hepatocellular calcium.17,22 In addition, vitamin D could modulate lipid levels via suppression of PTH secretion, as elevated PTH concentrations reportedly reduce lipolysis.23 Jorde et al.24 found a significant increase in serum HDL-C levels and a significant decrease in serum TG levels across increasing serum 25(OH)D quartiles. In a longitudinal analysis, an increase in serum 25(OH)D over 14 years was associated with a significant decrease in serum TG.24 Similarly, Skaaby et al.1 reported that a 10 nmol/l increase in serum 25(OH) D was associated with a 48% decrease in TG and a 37% decrease in very-low-density lipoprotein levels, in a prospective study of 4330 subjects with a 5-year follow-up.
Interestingly, serum 25(OH)D levels were negatively associated with the risk of elevated blood pressure in this study. A recent epidemiologic study of a large normotensive population in the United States found an inverse association between serum 25(OH)D levels and blood pressure.25 Moreover, in a clinical trial, supplementation with vitamin D3 and calcium for 8 weeks increased serum 25(OH)D by 72% and decreased SBP by 9.3%. This same study found that the effect of short-term supplementation was greater than calcium alone in elderly women aged ⩾70 years.26 Vitamin D may influence blood pressure by regulating the renin–angiotensin system, an important regulator of blood pressure.27, 28, 29 The treatment of 1,25(OH)2D3, an active form of vitamin D, suppressed renin expression in 1-α-hydroxylase knockout mice independent of calcium or phosphorus.29 The suppression of renin likely inhibits formation of angiotensin II that increases salt retention and blood pressure by stimulating aldosterone secretion and increasing vasoconstriction. Resnick et al.28 showed that serum 1,25(OH)2D3 levels were inversely associated with blood pressure in normotensive and hypertensive subjects and inversely correlated with plasma renin activity in patients with essential hypertension.
In contrast, the present study found that serum PTH levels were positively associated with the risk of elevated blood pressure. This association is consistent with results from other studies.11,30,31 In 1205 Dutch subjects aged ⩾65 years, serum PTH levels were positively associated with blood pressure.31 Moreover, chronic intravenous PTH infusion for 12 days resulted in hypercalcemia and hypertension in healthy subjects.30 The underlying mechanism is not yet clear. It may be because of the prosclerotic effect of PTH on the vascular smooth muscle cells of blood vessels32that may contribute to vessel wall thickening and consequently result in higher blood pressure. In addition, PTH activates renal 1-α-hydroxylase that increases 1,25(OH)2D3. An increase in serum 1,25(OH)2D3 stimulates calcium influx in a variety of cells, including vascular smooth muscle cells that results in contraction and increased peripheral vascular resistance.33 Although there is a positive association between serum PTH and elevated blood pressure, serum PTH levels were not associated with MetS risk in the present study. These results are inconsistent with findings from previous studies.4,7,9 Given the present inconsistencies in the literature, further study in this area is warranted.
This study has several limitations. First, it was not possible to prove a causal relationship because the study was designed cross-sectionally. Second, sunlight exposure and vitamin D intake were not measured, and both of these may affect serum 25(OH)D levels. Third, this study did not consider seasonal variations, although this is unlikely to affect the results because blood samples were all collected within a 3-month period. Despite these limitations, to the best of our knowledge, this is the first study to investigate the association of both serum 25(OH)D and PTH levels with MetS in a Korean population from representative survey data.
In conclusion, serum 25(OH)D concentrations were inversely associated with the risk of elevated blood pressure, hypertriglyceridemia, reduced HDL-C and MetS after adjusting for potential risk factors in middle-aged and older Korean adults. Serum PTH levels were associated with reduced abdominal obesity, elevated blood pressure and low TGs, but were not associated with MetS in Korean adults. Further prospective studies should be conducted to explore potential causal relationships between serum 25(OH)D, PTH and risk of MetS.
References
Skaaby T, Husemoen LL, Pisinger C, Jorgensen T, Thuesen BH, Fenger M et al. Vitamin D status and changes in cardiovascular risk factors: a prospective study of a general population. Cardiology 2012; 123: 62–70.
Vilarrasa N, Vendrell J, Maravall J, Elio I, Solano E, San Jose P et al. Is plasma 25(OH) D related to adipokines, inflammatory cytokines and insulin resistance in both a healthy and morbidly obese population? Endocrine 2010; 38: 235–242.
Ford ES, Ajani UA, McGuire LC, Liu S . Concentrations of serum vitamin D and the metabolic syndrome among U.S. adults. Diabetes Care 2005; 28: 1228–1230.
Ford ES, Zhao G, Li C, Pearson WS . Serum concentrations of vitamin D and parathyroid hormone and prevalent metabolic syndrome among adults in the United States. J Diabetes 2009; 1: 296–303.
Gagnon C, Lu ZX, Magliano DJ, Dunstan DW, Shaw JE, Zimmet PZ et al. Low serum 25-hydroxyvitamin D is associated with increased risk of the development of the metabolic syndrome at five years: results from a national, population-based prospective study (The Australian Diabetes, Obesity and Lifestyle Study: AusDiab). J Clin Endocrinol Metabol 2012; 97: 1953–1961.
Kim MK, Il Kang M, Won OhK, Kwon HS, Lee JH, Lee WC et al. The association of serum vitamin D level with presence of metabolic syndrome and hypertension in middle-aged Korean subjects. Clin Endocrinol 2010; 73: 330–338.
Reis JP, von Muhlen D, Miller ER 3rd . Relation of 25-hydroxyvitamin D and parathyroid hormone levels with metabolic syndrome among US adults. Eur J Endocrinol 2008; 159: 41–48.
Kim S, Lim J, Kye S, Joung H . Association between vitamin D status and metabolic syndrome risk among Korean population: based on the Korean National Health and Nutrition Examination Survey IV-2, 2008. Diabetes Res Clin Pract 2012; 96: 230–236.
Reis JP, von Muhlen D, Kritz-Silverstein D, Wingard DL, Barrett-Connor E . Vitamin D, parathyroid hormone levels, and the prevalence of metabolic syndrome in community-dwelling older adults. Diabetes Care 2007; 30: 1549–1555.
Kim J . Dairy food consumption is inversely associated with the risk of the metabolic syndrome in Korean adults. J Hum Nutr Diet 2013; 26 (Suppl 1): 171–179.
Jorde R, Svartberg J, Sundsfjord J . Serum parathyroid hormone as a predictor of increase in systolic blood pressure in men. J Hypertens 2005; 23: 1639–1644.
Lee DM, Rutter MK, O'Neill TW, Boonen S, Vanderschueren D, Bouillon R et al. Vitamin D, parathyroid hormone and the metabolic syndrome in middle-aged and older European men. Eur J Endocrinol 2009; 161: 947–954.
Awumey EM, Mitra DA, Hollis BW, Kumar R, Bell NH . Vitamin D metabolism is altered in Asian Indians in the southern United States: a clinical research center study. J Clin Endocrinol Metabol 1998; 83: 169–173.
Ministry of Health and Welfare. National Health And Nutrition Examination Survey Report 2005. Ministry of Health and Welfare: Seoul, 2005.
Kim J, I Jo . Grains, vegetables, and fish dietary pattern is inversely associated with the risk of metabolic syndrome in South korean adults. J Ame Diet Assoc 2011; 111: 1141–1149.
The American Society of Hypertension. Recommendations for routine blood pressure measurement by indirect cuff sphygmomanometry. American Society of Hypertension. Am J Hypertens 1992; 5 (4 Pt 1): 207–209.
Zittermann A, Frisch S, Berthold HK, Gotting C, Kuhn J, Kleesiek K et al. Vitamin D supplementation enhances the beneficial effects of weight loss on cardiovascular disease risk markers. Am J Clin Nutr 2009; 89: 1321–1327.
Cavalier E, Delanaye P, Carlisi A, Krzesinski JM, Chapelle JP . Analytical validation of the new version of the Liaison N-Tact PTH assay. Clin Chem Lab Med 2007; 45: 105–107.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009; 120: 1640–1645.
Li LH, Yin XY, Yao CY, Zhu XC, Wu XH . Serum 25-hydroxyvitamin D, parathyroid hormone, and their association with metabolic syndrome in Chinese. Endocrine 2013; 44: 465–472.
George JA, Norris SA, van Deventer HE, Crowther NJ . The association of 25 hydroxyvitamin D and parathyroid hormone with metabolic syndrome in two ethnic groups in South Africa. PLoS One 2013; 8: e61282.
Cho HJ, Kang HC, Choi SA, Ju YC, Lee HS, Park HJ . The possible role of Ca2+ on the activation of microsomal triglyceride transfer protein in rat hepatocytes. Biol Pharm Bull 2005; 28: 1418–1423.
Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC . Regulation of adiposity by dietary calcium. FASEB J 2000; 14: 1132–1138.
Jorde R, Figenschau Y, Hutchinson M, Emaus N, Grimnes G . High serum 25-hydroxyvitamin D concentrations are associated with a favorable serum lipid profile. Eur J Clin Nutr 2010; 64: 1457–1464.
Scragg R, Sowers M, Bell C . Serum 25-hydroxyvitamin D, ethnicity, and blood pressure in the Third National Health and Nutrition Examination Survey. Am J Hypertens 2007; 20: 713–719.
Pfeifer M, Begerow B, Minne HW, Nachtigall D, Hansen C . Effects of a short-term vitamin D(3) and calcium supplementation on blood pressure and parathyroid hormone levels in elderly women. J Clin Endocrinol Metabol 2001; 86: 1633–1637.
Kimura Y, Kawamura M, Owada M, Oshima T, Murooka M, Fujiwara T et al. Effectiveness of 1,25-dihydroxyvitamin D supplementation on blood pressure reduction in a pseudohypoparathyroidism patient with high renin activity. Intern Med 1999; 38: 31–35.
Resnick LM, Muller FB, Laragh JH . Calcium-regulating hormones in essential hypertension. Relation to plasma renin activity and sodium metabolism. Ann Intern Med 1986; 105: 649–654.
Zhou C, Lu F, Cao K, Xu D, Goltzman D, D. Miao . Calcium-independent and 1,25(OH)2D3-dependent regulation of the renin-angiotensin system in 1alpha-hydroxylase knockout mice. Kidney Int 2008; 74: 170–179.
Hulter HN, Melby JC, Peterson JC, Cooke CR . Chronic continuous PTH infusion results in hypertension in normal subjects. J Clin Hypertens 1986; 2: 360–370.
Snijder MB, Lips P, Seidell JC, Visser M, Deeg DJ, Dekker JM et al. Vitamin D status and parathyroid hormone levels in relation to blood pressure: a population-based study in older men and women. J Intern Med 2007; 261: 558–565.
Perkovic V, Hewitson TD, Kelynack KJ, Martic M, Tait MG, Becker GJ . Parathyroid hormone has a prosclerotic effect on vascular smooth muscle cells. Kidney Blood Press Res 2003; 26: 27–33.
Zemel MB . Calcium modulation of hypertension and obesity: mechanisms and implications. J Am Coll Nutr 2001; 20 (5 Suppl): 428S–435S. discussion 440S-442S.
Acknowledgements
This work was supported by a grant from the Kyung Hee University in 2013 (KHU-20130690).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, J. Association between serum vitamin D, parathyroid hormone and metabolic syndrome in middle-aged and older Korean adults. Eur J Clin Nutr 69, 425–430 (2015). https://doi.org/10.1038/ejcn.2014.192
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.192
This article is cited by
-
Gender specific association of parathyroid hormone and vitamin D with metabolic syndrome in population with preserved renal function
Scientific Reports (2018)
-
Vitamin D and parathyroid hormone in relation to bone health in Croatian women
Archives of Osteoporosis (2018)
-
Age and sex differences in the relationship between serum 25-hydroxyvitamin D and hypertension in the general Korean population
European Journal of Clinical Nutrition (2016)
-
Higher visceral fat area increases the risk of vitamin D insufficiency and deficiency in Chinese adults
Nutrition & Metabolism (2015)