Abstract
Aims
To investigate relationships between retinal morphology and retinal function in patients with retinitis pigmentosa (RP) using optical coherence tomography (OCT) and multifocal electroretinography (mfERG).
Methods
In all, 14 patients with RP who had visual acuities of 0.2 logMAR or better and Humphrey central fields of 10° or larger participated in the study along with 16 normal control subjects. The amplitudes and timings of the mfERG responses were compared with spatially corresponding measures of retinal layer thickness from OCT within the macula region (central 12°).
Results
Eyes with RP showed thinning of the photoreceptor retinal (PR) layer and thickening of mid-inner retinal (MIR) layers beyond the fovea. mfERG amplitude was reduced in all regions, whereas mfERG timing was only significantly delayed at a retinal eccentricity of 6–12° and was otherwise preserved within the foveal and parafoveal retina (0–6°). PR layer thickness was correlated with mfERG amplitude across the macula region. mfERG timing was correlated with the total change in retinal thickness (combined PR thinning and MIR thickening) at an eccentricity of 6–12°.
Conclusions
The relationship between mfERG timing and retinal thickness in RP is dependent on the retinal eccentricity. Preserved timing in the central retina (0–6°), despite significant disruption to retinal laminar structure, could be suggestive of inner retinal remodelling or functional redundancy. Cone system activity derived from mfERG amplitude appears to be related to the thickness of the photoreceptor layer in the macula region.
Similar content being viewed by others
Introduction
Retinitis pigmentosa (RP) is an inherited disease causing degeneration of retinal photoreceptor cells. Currently, there are no treatments, which can recover lost vision or halt disease progression. However, there is optimism for the future with the development of novel treatments including gene replacement,1, 2 tissue transplantation,3, 4, 5 and retinal prosthesis.6, 7 Common among these approaches is their targeting of the subretinal and epiretinal layers. However, as it is known that retinal remodelling can occur during the course of retinal degeneration (rd) in RP,8, 9, 10 the success of any therapeutic approach could rely on our ability to form an accurate evaluation of the status of the structure and function of individual retina. Thus, a non-invasive assessment of the morphological and physiological changes of the retina in RP is likely to be essential in establishing the extent of treatable retina as well as being useful for patient selection and monitoring.
Optical coherence tomography (OCT) images of the human retina in RP demonstrate changes in retinal thickness, including thinning of the outer nuclear layer (ONL), thought to reflect the loss of photoreceptor outer segments and thickening of the inner retina, suggestive of progressive retinal remodelling.10, 11 Evidence exists to show that retinal thickness and the status of the inner and outer segment junction (IS/OS) of the photoreceptors can be associated with visual acuity (VA) in RP.12, 13, 14, 15, 16 Furthermore, OCT images of rd animal models have a predictable relationship with histology and demonstrate potential for monitoring structural progression of the degenerative retina.17, 18, 19
Multifocal electroretinography (mfERG) allows for the simultaneous recording of focal retinal responses and can be used to provide information about localised retinal function in RP.20, 21, 22, 23 In particular, mfERGs can be useful in monitoring macular cone system function in RP and indeed mfERG responses have been shown to be associated with the subjective visual field size.21, 24, 25, 26
To date, relatively few studies have combined OCT and electrophysiology techniques to investigate the relationship between retinal morphology and function in human RP,27, 28, 29, 30 and in particular, studies of structure–function changes at a local level are limited. The current study compares the spatial variation in mfERG with OCT changes in RP. The study of the functional consequences of changes to retinal structure in human RP aims to develop our understanding of retinal degeneration. Furthermore, improving the techniques used to characterise retinal status in vivo could provide valuable information for use in the evaluation of patients undergoing future potential treatment options.
Materials and methods
Participants
A prospective study examined 14 patients (six female (F), eight male (M), age range: 17–56 years, median 37 years) with a clinical diagnosis of RP. Diagnosis was based on full-field electroretinography (ffERG), fluorescein angiography, and family history. All patients had a VA of 0.2 logMAR or better (12 had 0.1 logMAR or better), functional visual fields of at least 10° using Humphrey field analyser, 24–2 threshold test (Carl Zeiss Meditec, Dublin, CA, USA) and reduced/delayed ISCEV standard ffERGs. None of the patients had clinically significant cataract or macula oedema. Sixteen normal control subjects (eight F, eight M, age range: 18–45 years, median 31 years) with VAs of 0.1 logMAR or better and no history of eye disease also participated. We can certify that all applicable institution and governmental regulations concerning the ethical use of human volunteers were followed during this research. Informed consent was obtained from all participants in the study.
Multifocal electroretinography
MfERG stimulation (VERIS 4.1, Electro-Diagnostic Imaging Inc., San Mateo, CA, USA) was performed with Dawson–Trick–Litzkow (DTL) corneal contact thread electrodes using a standard protocol.31 The right eye was fully dilated (1% tropicamide) and corrected for the test distance with large diameter (50 mm) lenses. The left eye was occluded. The subject fixated the centre of the stimulus, which consisted of a 61 hexagonal element pattern array, scaled with eccentricity and covering 30° of the central visual field. Each hexagon was modulated between black (<10 cd/m2) and white (450 cd/m2) according to a standard binary m-sequence. Total recording time was 4 min. The mfERG signals were sampled at 1 KHz, filtered between 10 and 300 Hz and amplified by 100 K. The first 80 ms of each signal from each stimulus element was analysed to yield the N1-P1 amplitude and P1 implicit timing (Figure 1). Zero amplitude values from undetectable responses were included in the analysis, although these contributed no corresponding latency value.
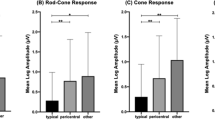
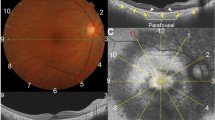
Photoreceptor retinal (PR) thickness and mid-inner retinal (MIR) thickness were measured from overlapping OCT line scans (a). A 61 Hexagonal element array (b) was used to generate localised mfERG responses from which N1–P1 amplitude, and P1 timing were measured. Colocalised structure–function data was determined and compared in the foveal region (F) and four quadrants within the macula (central 12°).
Retinal thickness
OCT (Stratus OCT 3.0, Carl Zeiss Meditec, Dublin, CA, USA) images of the retina were acquired from the right eye of each subject. Line scans were aligned with the stimulus elements of the mfERG pattern array and provided images of the retinal foveal region and each of the four retinal quadrants of 12° eccentricity (Figure 1). Overlapping 5-mm OCT line scan protocols consisting of 512 A-scans/image were used. Accurate central fixation was confirmed in each patient by observing the location of the foveal depression in each scan. Two measurements of retinal thickness were determined; photoreceptor retinal (PR) thickness was defined as the distance between the inner boundary of the highly reflective border (HRB) representing the retinal pigment epithelial (RPE; which was distinguished from the hyperreflective photoreceptor IS/OS17, 32) to the outer boundary of the low reflective band representing the outer plexiform layer (OPL). Mid-inner retinal (MIR) thickness was defined as the distance between the outer boundary of the OPL and the outer boundary of the HRB representing retinal nerve fibre layer (RNFL; 33Figure 1). Concerns exist regarding the accuracy of some automated analysis techniques.34, 35 Instead, manually placed electronic calipers were used for retinal thickness measurements, which were measured (at intervals of 125 μm along each scan) on two occasions, and an average value was calculated. All the measurements were performed by a single operator and repeatability of the manual thickness measurements was determined. Average retinal thickness values were calculated for retinal regions, which corresponded with the size and location of the mfERG stimulus elements. These included the central region 0–2° and measurements from each of the four quadrants at eccentricities of 2–6° and 6–12° (Figure 1). The absolute change in PR thickness was combined with the absolute change in MIR thickness to calculate the total change in retinal thickness.
Statistical analysis
As four dependent variables (PR and MIR thickness, mfERG amplitude, and timing) were measured, a multivariate analysis of variance (MANOVA) was conducted to determine the effect of RP on the combination of these variables. When this was found to be statistically significant, the follow-up analyses of variances (ANOVA) on each dependent variable (at each retinal eccentricity) were conducted to evaluate the differences between RP patients and controls. The correlations between the measurable mfERG response parameters and OCT retinal thickness measurements were evaluated using linear regression analysis. The level of significance was 0.05 (Bonferroni adjusted for multiple comparisons).
Results
Statistically significant differences were found between RP patients and control subjects on the combined dependent variables at the different retinal eccentricities (0–2°, F (4,25)=29.4, P<0.001; 2–6°, F(4,113)=203.4, P<0.001; 6–12°, F (4,96)=446.0, P<0.001). Results from the follow-up analyses using ANOVAs are given in the sections below. Table 1 contains the median, 5th and 95th percentiles for the dependent variables for RP patients and controls at the different retinal eccentricities.
Retinal structure
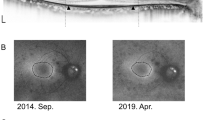
In general, OCT images from patients with RP show disruption of the retinal layers and reduced reflectivity in the extrafoveal regions of the retina (Figure 2). A loss of retinal laminar structure, including increased MIR thickness and a greater decline in PR thickness with increasing eccentricity was seen in patients with RP compared with controls (Figure 3). Average PR and MIR thicknesses in each retinal quadrant at eccentricities of 0–2, 2–6, and 6–12° were found to be significantly different in RP eyes compared with controls in all cases (F(1,27)=10.0–137.1, P<0.005). The coefficients of variance for manual OCT thickness measurements were between 2 and 6%. The line representing the photoreceptor IS/OS junction, was well-defined in all control subjects for the central 12° of the retina, however in eyes with RP the IS/OS signal was unclear and could often only be identified in the most central areas of the retina (0–4°). Eleven of the fourteen patients with RP had preserved foveal thickness consistent with their VA.
Examples of OCT images (0–6°) and mfERG responses (0–12°) from a control subject and three patients with RP. OCT shows disruption to the retinal laminar structure, including outer nuclear layer thinning and mid-inner retinal layer thickening. mfERGs in RP show reduced central responses and a greater decline in signal with increasing eccentricity.
Average (a) photoreceptor retinal (PR) thickness and (b) mid-inner retinal (MIR) thickness derived from OCT for 14 patients with RP for the central 0–12° of the retina. The 95% confidence limits of retinal thickness from 16 control eyes are shown in grey colour. RP patients exhibit reduced PR thickness and thickened MIR thickness beyond the foveal region compared with controls.
Retinal function
MfERGs from patients with RP showed normal to moderately reduced central responses and diminished/non-detectable extrafoveal responses (Figure 2). Only four patients with RP had any measurable responses in regions beyond 12° eccentricity. Grouped and averaged N1-P1 amplitudes for the central region of 0–2° and for the stimulus rings at eccentricities of 2–6° and 6–12° were significantly reduced in RP patients compared with controls (F (1,28)=47.1–76.5, P<0.001; Figure 4a). P1 implicit timings were significantly delayed in RP eyes compared with control eyes at an eccentricity of 6–12° (F (1,28)=33.02, P<0.001). However, for eccentricities of 0–2° and 2–6°, mfERG P1 timings in RP were not found to be significantly different from those in the control group (F (1,28)=0.53, P=0.47; F (1,28)=4.46, P=0.051; Figure 4b).
Structure and function
In patients with RP, significant correlation was found between mfERG amplitude and PR thickness at all retinal eccentricities (r (54)=0.56–0. 75, P<0.002) (Figure 5a). In addition, mfERG implicit timing was significantly correlated with MIR thickness and total change in retinal thickness at an eccentricity of 6–12° (r (35)=0.46, P=0.005; Figure 5b). No other significant correlations were measured.
(a) In RP, thinning of the PR layer is significantly correlated with the loss of mfERG amplitude at retinal eccentricities 0–2°, 2–6°, and 6–12°. (b) The total change in retinal thickness (combined PR thinning and MIR thickening) is only correlated with the timing of the mfERG responses at the retinal eccentricity of 6–12°. Dashed lines represent the lower 95% confidence limits of the control group.
In the most central retinal area (0–2°), 10 of the 14 patients with RP had altered retinal layer structure (PR thinning and/or MIR thickening) and reduced mfERG amplitude when compared to controls, however none had abnormal mfERG timing (Figure 5). Likewise, between 2–6° eccentricity, 95% of the retinal thickness measurements and mfERG amplitudes were significantly altered in RP, although mfERG timings were delayed in fewer than 40% of cases. It is only at an eccentricity of 6–12° that mfERG timing delays were found to correlate with the altered retinal laminar structure (Figure 5b).
Discussion
This study examines colocalised measurements of OCT and mfERG from the macular region of the retina (0–12°) in patients with RP who retain good VA and central visual fields. The results show that although there is loss of mfERG amplitude, which is correlated to PR layer thinning, mfERG timing can be preserved (within 0–6°) despite significant disruption to retinal morphology (PR thinning and MIR thickening). At increased eccentricity of 6–12°, mfERG timings are delayed and correlated to retinal thickness changes, which include MIR thickening.
Several investigators have previously shown that patients with RP can have preserved mfERG timing in the central retina despite the loss of mfERG amplitude.20, 24 mfERG timing can also be preserved centrally in RP where there is reduced temporal contrast sensitivity function.36 A comparison of mfERGs with visual field testing suggests that the mfERG amplitude is not a good predictor of visual sensitivity, but that mfERG delays could provide an early indication of local retinal damage to the cone system.21 Indeed, it is suggested that the pattern of amplitude loss preceding timing changes often seen in mfERG testing in RP could reflect different disease mechanisms; where amplitude reflects losses in the number of cones, whereas timing could reflect the function of the residual receptors.21, 24 This being the case a fall in cell numbers would reduce retinal sensitivity, although stimulus detection and the temporal response would be mediated by the remaining ‘normal functioning’ cone cells.36
The morphological changes associated with these local functional changes have not been fully investigated. Earlier electrophysiology studies using focal macular ERGs (fmERG) show that the amplitude of the response can be related to OCT structural changes reflected in macular volume and the integrity of the photoreceptor IS/OS signal,29, 30 although it was also noted that preserved morphology on OCT did not always guarantee normal function.29 Using mfERG testing, we find that the response amplitudes are correlated with photoreceptor layer thickness in patients with RP suggesting that thinning of the photoreceptor layer can be directly related to a fall in the number of active cone pathways. This does not account for structural changes, which may result from the primary rod photoreceptor death. Nor does it fit particularly well with the understanding that the mfERG response is dominated by ON and OFF bipolar cell activity,37 although evidence of photoreceptor contribution to mfERGs,37 including an influence from the rod system pathway38 exists. No significant relationships were found between mfERG amplitude and MIR thickness. These findings raise the possibility that changes to macular PR layer morphology in rd are influenced to a greater extent by the time course of the secondary disorganisation (loss of pigment, shortening, and misalignment) of the cone cells. However, as previously mentioned, the role of central mfERG amplitudes in predicting visual function is still questionable given their reduced sensitivity and also their relatively high level of intersubject variability.20, 21, 39, 40
Timing of the mfERG response is related to MIR thickness and the total change in retinal thickness but only at an eccentricity of 6–12°. Altered retinal structure, including both thinning of the PR layer and thickening of the MIR layer, was not correlated with the preserved mfERG timing within the central retinal areas (0–6°). As the measurement of MIR thickness includes the bipolar cell structures, it was expected that a stronger association would have arisen between this parameter, and mfERG timing given that mfERG timing is thought to be a sensitive measure of local bipolar cell activity. This was not the case; instead we find a structure–function relationship that is dependent on retinal eccentricity, which itself raises several issues regarding the consequences of early retinal cell death. We speculate that laminar remodelling and/or functional redundancy could explain these findings. A process of neural remodelling (following rod photoreceptor death and secondary cone disorganisation), such as cell migration and a rewiring of the retinal circuits, as seen in animal studies,8 may partially protect retinal function, while possibly altering retinal structure. Although there may be a loss in the overall numbers of active cells and pathways, those, which remain may be ‘reorganised’ and functionally robust. The OCT changes that we have found are consistent with other recent human RP studies showing retinal laminar abnormalities, including thinning of the outer retina and thickening of the inner retina layers,10, 11 and several animal studies support the idea that ONL thinning reflects photoreceptor loss, and inner retinal thickening reflects a secondary process of structural remodelling, possibly neuronal–glial remodelling.8, 9, 41, 42 In addition, functional redundancy in the macula, possibly because of greater receptive field overlap (coverage factor) could enable the foveal and parafoveal retina to sustain a certain amount of structural change or cell loss before functional measures, such as mfERG timing and visual fields demonstrate significant changes. Cell loss because of rd is likely to have a greater effect on function in the peripheral retina where receptive field overlap is less.
Although further investigation is required to demonstrate these concepts, this study highlights the need for a localised analysis of both retinal structure and function to provide satisfactory information in the assessment and monitoring of patients with RP. It supports the previously held idea that the amplitude and timing of the mfERG response could represent different disease mechanisms. Furthermore, it suggests caution in exclusively using structural data, such as that from OCT retinal imaging to reflect the status of retinal function30 or to assess the feasibility of treatment, such as retinal prostheses in RP.15
Future studies could improve the matching between the mfERG stimulus and the OCT scans, which although colocalised represent different sized areas of the retina. In addition, it has been shown that the relationship between morphological changes detected by OCT and the ffERG in humans can depend on patient phenotype,27, 28 and this was not assessed in this study. Clearly, there remains a need to perform longitudinal studies using a combination of visual function measures and structural imaging to investigate in vivo the progression of rd in the human eye.
References
Bennett J . Gene therapy for retinitis pigmentosa. Curr Opin Mol Ther 2000; 2: 420–425.
Acland GM, Aguirre GD, Ray J, Zhang Q, Aleman TS, Cideciyan AV et al. Gene therapy restores vision in a canine model of childhood blindness. Nat Genet 2001; 28: 92–95.
Lund RD, Coffey PJ, Sauve Y, Lawrence JM . Intraretinal transplantation to prevent photoreceptor degeneration. Ophthalmic Res 1997; 29: 305–319.
Litchfield TM, Whiteley SJ, Lund RD . Transplantation of retinal pigment epithelial, photoreceptor and other cells as treatment for retinal degeneration. Exp Eye Res 1997; 64: 655–666.
Bartsch U, Oriyakhel W, Kenna PF, Linke S, Richard G, Petrowitz B et al. Retinal cells integrate into the outer nuclear layer and differentiate into mature photoreceptors after subretinal transplantation into adult mice. Exp Eye Res 2008; 86: 691–700.
Loewenstein JI, Montezuma SR, Rizzo III JF . Outer retinal degeneration: an electronic retinal prosthesis as a treatment strategy. Arch Ophthalmol 2004; 122: 587–596.
Hossain P, Seetho IW, Browning AC, Amoaku WM . Artificial means for restoring vision. BMJ 2005; 330: 30–33.
Marc RE, Jones BW, Watt CB, Strettoi E . Neural remodeling in retinal degeneration. Prog Retin Eye Res 2003; 22: 607–655.
Strettoi E, Pignatelli V, Rossi C, Porciatti V, Falsini B . Remodeling of second-order neurons in the retina of rd/rd mutant mice. Vision Res 2003; 43: 867–877.
Aleman TS, Cideciyan AV, Sumaroka A, Windsor EA, Herrera W, White DA et al. Retinal laminar architecture in human retinitis pigmentosa caused by rhodopsin gene mutations. Invest Ophthalmol Vis Sci 2008; 49: 1580–1590.
Aleman TS, Cideciyan AV, Sumaroka A, Schwartz SB, Roman AJ, Windsor EA et al. Inner retinal abnormalities in X-linked retinitis pigmentosa with RPGR mutations. Invest Ophthalmol Vis Sci 2007; 48: 4759–4765.
Hamada S, Yoshida K, Chihara E . Optical coherence tomography images of retinitis pigmentosa. Ophthalmic Surg Lasers 2000; 31: 253–256.
Witkin AJ, Ko TH, Fujimoto JG, Chan A, Drexler W, Schuman JS et al. Ultra-high resolution optical coherence tomography assessment of photoreceptors in retinitis pigmentosa and related diseases. Am J Ophthalmol 2006; 142: 945–952.
Sandberg MA, Brockhurst RJ, Gaudio AR, Berson EL . The association between visual acuity and central retinal thickness in retinitis pigmentosa. Invest Ophthalmol Vis Sci 2005; 46: 3349–3354.
Matsuo T, Morimoto N . Visual acuity and perimacular retinal layers detected by optical coherence tomography in patients with retinitis pigmentosa. Br J Ophthalmol 2007; 91: 888–890.
Aizawa S, Mitamura Y, Baba T, Hagiwara A, Ogata K, Yamamoto S . Correlation between visual function and photoreceptor inner/outer segment junction in patients with retinitis pigmentosa. Eye 2008; e-pub ahead of print.
Huang Y, Cideciyan AV, Papastergiou GI, Banin E, Semple-Rowland SL, Milam AH et al. Relation of optical coherence tomography to microanatomy in normal and rd chickens. Invest Ophthalmol Vis Sci 1998; 39: 2405–2416.
Li Q, Timmers AM, Hunter K, Gonzalez-Pola C, Lewin AS, Reitze DH et al. Noninvasive imaging by optical coherence tomography to monitor retinal degeneration in the mouse. Invest Ophthalmol Vis Sci 2001; 42: 2981–2989.
Horio N, Kachi S, Hori K, Okamoto Y, Yamamoto E, Terasaki H et al. Progressive change of optical coherence tomography scans in retinal degeneration slow mice. Arch Ophthalmol 2001; 119: 1329–1332.
Seeliger M, Kretschmann U, Apfelstedt-Sylla E, Ruther K, Zrenner E . Multifocal electroretinography in retinitis pigmentosa. Am J Ophthalmol 1998; 125: 214–226.
Hood DC, Holopigian K, Greenstein V, Seiple W, Li J, Sutter EE et al. Assessment of local retinal function in patients with retinitis pigmentosa using the multi-focal ERG technique. Vision Res 1998; 38: 163–179.
Chan HL, Brown B . Investigation of retinitis pigmentosa using the multifocal electroretinogram. Ophthalmic Physiol Opt 1998; 18: 335–350.
Dolan FM, Parks S, Hammer H, Keating D . The wide field multifocal electroretinogram reveals retinal dysfunction in early retinitis pigmentosa. Br J Ophthalmol 2002; 86: 480–481.
Holopigian K, Seiple W, Greenstein VC, Hood DC, Carr RE . Local cone and rod system function in patients with retinitis pigmentosa. Invest Ophthalmol Vis Sci 2001; 42: 779–788.
Sandberg MA, Weigel-DiFranco C, Rosner B, Berson EL . The relationship between visual field size and electroretinogram amplitude in retinitis pigmentosa. Invest Ophthalmol Vis Sci 1996; 37: 1693–1698.
Birch DG, Herman WK, deFaller JM, Disbrow DT, Birch EE . The relationship between rod perimetric thresholds and full-field rod ERGs in retinitis pigmentosa. Invest Ophthalmol Vis Sci 1987; 28: 954–965.
Jacobson SG, Cideciyan AV, Huang Y, Hanna DB, Freund CL, Affatigato LM et al. Retinal degenerations with truncation mutations in the cone-rod homeobox (CRX) gene. Invest Ophthalmol Vis Sci 1998; 39: 2417–2426.
Jacobson SG, Cideciyan AV, Iannaccone A, Weleber RG, Fishman GA, Maguire AM et al. Disease expression of RP1 mutations causing autosomal dominant retinitis pigmentosa. Invest Ophthalmol Vis Sci 2000; 41: 1898–1908.
Sugita T, Kondo M, Piao CH, Ito Y, Terasaki H . Correlation between macular volume and focal macular electroretinogram in patients with retinitis pigmentosa. Invest Ophthalmol Vis Sci 2008; 49: 3551–3558.
Oishi A, Nakamura H, Tatsumi I, Sasahara M, Kojima H, Kurimoto M et al. Optical coherence tomographic pattern and focal electroretinogram in patients with retinitis pigmentosa. Eye 2008; e-pub ahead of print.
Marmor MF, Hood DC, Keating D, Kondo M, Seeliger MW, Miyake Y et al. Guidelines for basic multifocal electroretinography (mfERG). Doc Ophthalmol 2003; 106: 105–115.
Pons ME, Garcia-Valenzuela E . Redefining the limit of the outer retina in optical coherence tomography scans. Ophthalmology 2005; 112: 1079–1085.
Shahidi M, Wang Z, Zelkha R . Quantitative thickness measurement of retinal layers imaged by optical coherence tomography. Am J Ophthalmol 2005; 139: 1056–1061.
Costa RA, Calucci D, Skaf M, Cardillo JA, Castro JC, Melo Jr LA et al. Optical coherence tomography 3: automatic delineation of the outer neural retinal boundary and its influence on retinal thickness measurements. Invest Ophthalmol Vis Sci 2004; 45: 2399–2406.
Sadda SR, Wu Z, Walsh AC, Richine L, Dougall J, Cortez R et al. Errors in retinal thickness measurements obtained by optical coherence tomography. Ophthalmology 2006; 113: 285–293.
Felius J, Swanson WH . Photopic temporal processing in retinitis pigmentosa. Invest Ophthalmol Vis Sci 1999; 40: 2932–2944.
Hood DC, Frishman LJ, Saszik S, Viswanathan S . Retinal origins of the primate multifocal ERG: implications for the human response. Invest Ophthalmol Vis Sci 2002; 43: 1673–1685.
Dolan FM, Sandinha T, Purdy A, Parks S, Keating D . Vitamin A deficiency modifies the mfERG: a case study of rod influence on the mfERG. Doc Ophthalmol 2006; 112: 31–34.
Janaky M, Palffy A, Deak A, Szilagyi M, Benedek G . Multifocal ERG reveals several patterns of cone degeneration in retinitis pigmentosa with concentric narrowing of the visual field. Invest Ophthalmol Vis Sci 2007; 48: 383–389.
Gerth C, Wright T, Heon E, Westall CA . Assessment of central retinal function in patients with advanced retinitis pigmentosa. Invest Ophthalmol Vis Sci 2007; 48: 1312–1318.
Gargini C, Terzibasi E, Mazzoni F, Strettoi E . Retinal organization in the retinal degeneration 10 (rd10) mutant mouse: a morphological and ERG study. J Comp Neurol 2007; 500: 222–238.
Milam AH, Li ZY, Fariss RN . Histopathology of the human retina in retinitis pigmentosa. Prog Retin Eye Res 1998; 17: 175–205.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded by the Northern Ireland Research and Development Office
Rights and permissions
About this article
Cite this article
Wolsley, C., Silvestri, G., O'Neill, J. et al. The association between multifocal electroretinograms and OCT retinal thickness in retinitis pigmentosa patients with good visual acuity. Eye 23, 1524–1531 (2009). https://doi.org/10.1038/eye.2008.318
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.318
Keywords
This article is cited by
-
The association between cone density and visual function in the macula of patients with retinitis pigmentosa
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)
-
The assessment of macular electrophysiology and macular morphology in patients with vitiligo
International Ophthalmology (2017)
-
Association between multifocal electroretinograms, optical coherence tomography and central visual sensitivity in advanced retinitis pigmentosa
Documenta Ophthalmologica (2012)
-
Effects of luminance combinations on the characteristics of the global flash multifocal electroretinogram (mfERG)
Graefe's Archive for Clinical and Experimental Ophthalmology (2010)