Abstract
Purpose: To examine the data from over 119,000 Fragile X Syndrome tests and 307 prenatal tests to detect unsuspected findings and obtain clinical data when indicated to optimize genetic counseling.
Methods: A proprietary database containing 119,232 consecutive postnatal and 307 prenatal FXS tests performed between November 2, 1992 and June 1, 2006 was queried.
Results: The distribution of normal FMR1 alleles was a bimodal distribution with a major peak at 30 repeats and a minor peak at 21 repeats. Of 59,707 tests performed for males, 1.4% had a fully expanded and methylated FMR1 allele. Of 59,525 tests performed for females, 0.61% had an affected FMR1 allele, and 1.7% had a premutation FMR1 allele for a total carrier frequency of 1.3%. When fetuses inherited an expanded maternal allele, the risk of expansion to a full affected allele was 0%, 5%, 30% and 100% for allele sizes of <50, 50–75, 76–100 and >100 repeats, respectively.
Conclusions: These figures can be used for genetic counseling of patients presenting for carrier detection and prenatal diagnosis for Fragile X Syndrome.
Similar content being viewed by others
Main
Fragile X Syndrome (FXS) is the most common inherited form of mental retardation and the second most frequent genetic cause of mental retardation. FXS is caused by mutations in the FMR1 gene coding for the protein Fragile X Mental Retardation Protein (FMRP). FXS is inherited as an X linked dominant disease exhibiting milder symptoms in females than in males. Males usually have mental retardation with an average IQ <50 in addition to stereotypic hand flapping behaviors, Attention Deficit Hyperactivity Disorder, and variable physical features such as postpubertal macro-orchidism and dysmorphic cranial features.1,2 The symptoms of FXS in females are milder than those in males and include Attention Deficit Disorder (with or without hyperactivity), learning disabilities and personality disorders. Almost all cases of FXS are due to an expansion of a CGG tandem repeat in the 3′ untranslated region of the FMR1 gene to more than 200 repeat units. Rarely, FXS is due to point mutations or complete deletions of the FMR1 gene.3–6
The inheritance patterns in FXS are complex. For the purposes of this article we will use our laboratory classification system that is based on the American College of Medical Genetics recommendations defining normal FMR1 alleles as CGG repeat numbers <45. Alleles of 45–55 repeats are defined as intermediate or “gray zone” alleles, premutation alleles are defined as 56–200 CGG repeats, and full mutation alleles are >200 repeats.7 A recent publication from the American College of Obstetricians and Gynecologists has slightly different definitions: normal alleles <40, intermediate alleles (gray zone) 41–60, premutation 61–200, and full mutation >200.8 Affected FMR1 alleles become highly methylated, thus reducing expression of FMR1 protein.1
Approximately 39% of males with premutation alleles will suffer from Fragile X Associated Tremor/Ataxia Syndrome (FXTAS) after the age of 50 years.9 When inherited through the female, premutation alleles may expand to larger premutation alleles or to full mutation alleles.10 Therefore, women who are carriers of either premutations or full mutation alleles are at risk for conceiving affected offspring. Female premutation carriers have no mental dysfunction due to their FMR1 alleles. Twenty percent experience premature ovarian failure defined as menopause younger than 40 years of age.11,12 Recently some premutation carrier females have been found to have some features of FXTAS.13 In contrast, premutation alleles when inherited through the male do not expand, but his daughters are at risk of having affecting children. Although “gray zone” alleles (45–55 CGG repeats) are considered above the normal range, there have been no reported instances of an allele below 56 repeats expanding to a full allele in a single meiosis.10
We have been performing FXS testing using a combination of PCR and Southern blot analysis for all patients since 1992. All result data are stored in a proprietary database. This article summarizes the results of this 14-year experience including 119,232 postnatal FMR1 tests and 307 prenatal diagnostic tests.
The impetus for undertaking this study is several recent developments and publications regarding FXS, namely the description of FXTAS in both males and females,9,13 premature ovarian failure in premutation carrier women,11,12 and the suggestion that carrier screening for FXS be offered to all pregnant women.14 Therefore, it is important to know the frequency of premutation and full mutation carriers in the US population in order to predict the prevalence of women who may have neurological symptoms or hormonal problems due to premutation FMR1 alleles. Due to the complex nature of the inheritance patterns in FXS, and the technical difficulties involved in the detection of fully expanded alleles, any carrier screening strategy will probably rely on a PCR based initial screen. In order to assess the ability of such screening programs to detect carriers of FXS, it is essential to know the expected number of noncarrier females who are homozygous for an unexpanded allele, as well as the expected number of heterozygous females for the full mutation and premutation.
METHODS
Molecular testing
Molecular diagnostic testing was performed using both PCR and Southern blot analysis for all samples as described previously.15 The PCR reaction contains 2 primer sets, one flanking the CGG repeat area in the 5′ untranslated region of FMR1 and an internal control consisting of primers spanning a highly polymorphic region near the promoter of the androgen receptor gene.15 The PCR reaction is routinely capable of amplifying repeat sizes of up to 100 CGG repeats although sometimes larger repeat sizes will amplify and be detected. Larger repeat sizes will not reliably amplify in the PCR reaction. The only significant modification is that the original protocol used a polyacrylamide gel based automated sequencer to analyze the PCR products. Beginning in 2002, this analysis was converted to capillary electrophoresis on an ABI 3700 automated DNA sequencer. Prior to introduction of the capillary instrument, any fragment size over 100 repeats was simply scored as >100. Subsequently, the actual repeat size was determined and reported. This procedural advance was suggested in January, 2002.16 Southern blot analysis must be used to analyze larger repeat sizes as well as the methylation status of the FMR1 gene.15 The methods for Southern blot analysis have not been altered during the course of the study. For the purposes of this report, normal FMR1 alleles are defined as CGG repeat numbers <45. Premutation alleles consist of 55–200 CGG repeats without methylation, full mutation alleles are >200 repeats with methylation. Alleles between 45 and 55 are considered “gray zone” alleles.7
Our laboratory has participated in the CAP proficiency testing program for FMR1 testing since the introduction of the program, and subscribes to all CLIA guidelines for continuous quality improvement and quality assurance. The assay has been stable and other than the improvement noted with the change to capillary sequencing from gel base sequencing there are no significant differences in sensitivity and specificity during the 14 year history of our laboratory performing these analyses.
The Southern blot uses a specific restriction enzyme that will not cleave the DNA if the recognition contains a methylated cytidine residue. This allows differentiation between FMR1 alleles that are methylated and those that are not methylated. For the purposes of this article we will use the terms “unmethylated” for alleles that are sensitive to restriction digestion and “methylated” to describe alleles that are resistant to restriction digestion. Normal females will have one methylated and one unmethylated allele, whereas normal males will have a single unmethylated band. Samples of many patients with expanded alleles do not demonstrate an allele of a discrete size on Southern blot analysis but have a “smear” extending across a range of molecular weights. In such cases the allele sizing is given as a range between the upper and lower edge of the smear. Some patients with expanded alleles will have 2 discrete alleles indicating mosaicism. Such patients will be described as mosaic with an approximate percentage given to each band based on the intensity of each band on the autoradiogram.15
Alleles between 200 and 250 repeats represent a problem in diagnosis. Some alleles in this size range are unmethylated and therefore are classified as premutation alleles whereas others are highly methylated and must be classified as affected alleles. Therefore, the classification of alleles in the range of 200–250 is dependent not only on the extent of the expansion but on the assessment of the methylation status of the expanded allele.
Data analysis
All molecular testing data are maintained in a proprietary database called Mol Gen, written by one of the authors (BC). This database captures demographic information from our laboratory information systems (LIS) and analytic information from the automated sequencers. Southern blot data are entered manually and following Director review the results are uploaded back into the LIS. Thus, all reported patient results and demographics are captured in the database.
χ2 statistical analysis was performed using the PC based freeware program Epistat.
RESULTS
Postnatal testing
Table 1 is a summary of the data and results for the 119,232 postnatal FXS molecular tests performed at Quest Diagnostics in the 14-year period. There are nearly equal numbers of male and female patients. Since 1993, the first full year of testing, there has been a nearly 30-fold increase in FXS testing volumes. In the period between 1992 and 1999, twice as many tests were ordered for males than for females. Currently the gender ratio has reversed with 1.5 times as many females tested as males. The average age of tested males is 8.1 years; the average age of tested females is 28.3 years. We infer from the age patterns that testing for males is primarily for diagnostic purposes in boys with mental dysfunction whereas testing for females is primarily for carrier detection in women of reproductive age. The number of females and males tested because of a positive family history for FXS is <1% of all testing. Although we have no documentation available we infer that the bulk of the increase in testing is most likely due to physicians performing population based carrier detection despite the absence of recommendations from any professional organization. A full FXS mutation was found in 862 of 59,707 males tested (1.4%). Premutation alleles were found in 333 (0.56%), and gray zone alleles in 518 (0.87%). The incidence of 1.4% is well below the usual estimation of FXS prevalence in retarded males of 3–8%,17 but within the range of several reported incidence studies in MR populations.18
A full FXS mutation was discovered in 364/59,525 females tested (0.61%), 1,008 (1.69%) premutation carriers and 1,283 (2.16%) women had gray zone alleles. In all, 1:43 tested women were at risk for having children with FXS. This is higher than the observed FXS carrier frequencies in British, Israeli and French Canadian populations that vary from between 1:70 to 1:25919–21 and may be due to ascertainment bias since many positives could have been submitted because of a family history of FXS or a family history consistent with X-linked MR.
The distribution of all alleles in unaffected patients is shown in Figure 1. This is combined data from females with 2 alleles in the normal range or males with a single allele in the normal range. In all, 171,734 alleles are represented. As expected, there were no apparent distribution differences between male and female alleles (data not shown). Although most of the alleles center around a distribution of 30 repeats, allele sizes of 18–24 have an increased frequency and there may be 1 or 2 shoulders of the distribution at the sizes of 36 repeats and 40 repeats. A similar finding was published of 492 alleles showing an increased frequency of alleles of 19–22 repeats and a second peak at 39 repeats.21 Our large data set makes it unlikely that these variances in prevalence are due to sampling error.
Figure 2 represents the distribution of 3,142 gray zone and premutation alleles observed in this cohort. The apparent spike at 100 repeats is an artifact of our prior gel-based sizing system when any band detected at 100 repeats or greater was scored as >100 repeats (see Methods). There are suggestions of 2 frequency peaks, one at 72–75 repeats, and a second at 93 repeats but since each data point represents <30 cases, this apparent bimodal distribution may be due to sampling artifact.
Sex chromosome aneuploidies
One of the advantages of our assay system is the ability to detect sex chromosome abnormalities.15 Sometimes on PCR, a male sample will be heterozygous at the androgen receptor locus and/or the FMR1 locus indicating the presence of 2 X-chromosomes. More frequently, the Southern blot for a male will demonstrate a methylated X-chromosome and an unmethylated X-chromosome indicating the presence of at least 2 X-chromosomes. In females, the PCR can demonstrate 3 androgen receptor alleles or FMR1 alleles indicating the presence of an additional X-chromosome and/or the methylated band on the Southern blot may be of a higher intensity than the unmethylated band also suggesting the presence of an additional X-chromosome. The presence of a single unmethylated band on a Southern blot of a female patient suggests the diagnosis of 45,X (Turner syndrome). All these observations can also be consistent with misidentified gender. Whenever the molecular testing suggests a sex chromosome aneuploidy or gender discrepancy and the patient has not previously had a karyotype analysis ordered, we contact the physician's office. If there has been no phenotypic gender misidentification by the physician's office we request an additional sample for karyotyping.
By far the most common suspected and confirmed sex chromosome aneuploidy was Klinefelter syndrome, with 59 confirmed diagnoses of 47,XXY and 13 suspected diagnoses in the 59,707 male patients. There were no cases where the FMR1 analysis indicated the presence of an additional X-chromosome that was not confirmed by karyotype. Karyotypes had not been performed prior to FMR1 analysis for any of these patients. There were also 9 confirmed cases 48,XXYY, 2 cases of 48,XXXY and 2 cases of 49,XXXXY. This leads to a calculated incidence of 1:702 male samples submitted for FXS molecular analysis with sex chromosome aneuploidies and supports the recommendation that all patients with MR have a karyotype analysis in addition to an FMR1 analysis.
The incidence of sex chromosome aneuploidies in females was 1:2,125 with 17 cases of 45,X Turner syndrome and 4 mosaic Turner syndrome patients. In this series of nearly 120,000 tests, there was not a single case of a patient who had both a sex chromosome aneuploidy and a premutation or full mutation allele. This observation has important implications for screening strategies that use the assumption that any female with 2 normal FMR1 alleles cannot be a carrier for FXS and that any male with a single normal FMR1 allele cannot be affected with FXS. This strategy could yield false negatives if there are additional X-chromosomes present. These data demonstrate that such false negatives will occur <1:120,000 tests.
Gender discrepancies
The test requisition form for FMR1 testing requires the age and gender of the patient to be specified. Other data such as indication for testing, family history, and race is requested but inconsistently supplied and not captured in our database, and therefore unavailable for analysis. Because, in the absence of a sex chromosome aneuploidy, the gender of the patient sample can be inferred from the Southern blot results (a single hypomethylated band for a male and both a methylated and hypo-methylated band for a female), cases of discrepant gender are sometimes noted. In such cases the physician's office is contacted to determine the correct gender of each patient. In our series of 119,232 analyses, 530 patients were identified as female who are male and 227 patients were identified as male who are female. Almost all cases were due to misinterpretations of the patient's first name by medical office staff, but some were careless errors. This has important implications for any potential screening strategy that relies on accurate gender information for test interpretation. Because of this issue we have recently added an internal Amelogenin control22 to our multiplex PCR reaction that allows a molecular interpretation of gender. In the rare instances of sex chromosome aneuploidy, there could still be false negative results using this control, but as was mentioned above, there have been no instances of a patient with both a sex aneuploidy and an expanded FMR1 allele. This internal control would eliminate the 757 cases (1:229) of misidentified gender on the test requisition forms.
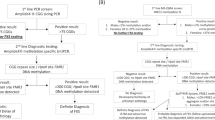
Prenatal diagnosis
We performed 307 prenatal diagnoses for FXS during this 14-year period. Karyotypes were also performed on all samples. The results are summarized in Table 2. Although there is a difference between the number of male fetuses (165) to female fetuses (142) this difference was not statistically significant. There were 22 affected fetuses (7.1%). We did not have a database field for maternal allele size in our database. This necessitated performing a text search and manual review to determine the maternal expanded allele size for the prenatal cases. No physical chart review could be performed for older cases whose records had been moved to long term storage or had been destroyed pursuant to regulatory compliance. We were able to determine the maternal allele size for 161 of the pregnancies. These data are summarized in Table 3. Prenatal diagnosis for FXS was ordered for 14 fetuses whose mothers had 2 normal FMR1 alleles. These were cases with a positive family history of MR consistent with X-linked inheritance in pregnancies undergoing an invasive diagnostic procedure for other indications. As expected, there were no expansions of any of the normal or gray zone alleles. If all premutation alleles are taken as a single group, 40% (21/52) expanded during meiosis, and 18% (9/52) expanded to full mutations. Given that the expanded chromosome will only be inherited half the time, the risk of a premutation carrier having an affected child is approximately 9%, a number that agrees with the 7% observed in the larger series of prenatal diagnosis shown in Table 2.
Table 4 is a breakdown of the prenatal diagnostic data for 98 prenatal diagnostic cases for which we have a complete data set and the fetus inherited the maternal expanded allele. As expected there were no expansions observed with repeat sizes <50. As the maternal premutation sizes increase there is a corresponding increase in the risk of expansion to affected alleles. Repeat size ranges of 50–75, 76–100 and >100 demonstrated a 5%, 30% and 100% rate of expansion to full mutation, respectively.
We observed a total of 23 expansions in our series of prenatal diagnoses for which we have a complete data set. These cases are listed in Table 4. The smallest allele observed to expand to an affected allele contained 64 repeats that expanded to a mosaic with 25% of the alleles having 76 repeats and 25% of the alleles having 200 repeats. The 200 repeat allele was methylated in this male fetus and the couple chose to terminate the pregnancy. The second smallest repeat observed to expand to a full mutation was an allele of 72 repeats that expanded to 350 repeats in the fetus. In this series, alleles of >90 repeats all expanded to full mutations and the largest premutation allele to expand to a larger premutation allele was an 84 repeat allele that expanded to a 94 repeat premutation allele.
DISCUSSION
Quest Diagnostics has been performing molecular FXS testing for 14 years. Despite the absence of recommendations for population based carrier screening, the number of tests ordered for this purpose continues to increase annually. This trend will likely continue as physicians and patients become increasingly aware of FXS and the possibility for carrier detection prior to the birth of an affected child.
Because of the nature of our assay, we would expect to detect all cases of Klinefelter syndrome (47,XXY) because these males will have both a methlyated and unmethylated FMR1 band. We observed a frequency of 1:702 that is midway between the prevalence of 1:1,000 seen in newborn surveys23 and the 1:500 reported in dysmorphology texts.24 Even though Klinefelter syndrome has been associated with mild mental dysfunction we did not see a concentration of cases in our FXS sample. This might be due to the fact that males with Klinefelter syndrome had already been diagnosed prior having FMR1 testing or that they are so mildly affected that FXS testing was not considered. The paucity of cases of 47,XXX is almost certainly due to fact that only a fraction of 47,XXX females will be detected by our assay and such females have a low incidence of mental dysfunction.
The detection of several patients with more than 1 additional X-chromosome is not unexpected, as the greater the aneuploidy, from XXY to XXXXY, the more severe the mental deficiency.24 Although only 13 individuals were detected with these phenotypes it emphasizes the need for a karyotype as part of the complete work up for a male with mental retardation. Our assay cannot replace a karyotype as translocations and autosomal abnormalities will not be detected by our assay. No 47,XYY males were detected because our assay is not capable of detecting that abnormality.
Our assay should detect all cases of Turner Syndrome (45, X). Our observed frequency of 1:19,800 is far less than the reported incidence of 1:2,000.24 This is almost certainly due to the fact that testing for females is primarily for carrier detection; most Turner Syndrome patients are diagnosed well before age 28 and are infertile. The lower than expected observed frequency of 47,XXX is likely due to the assay design which will only detect a fraction of the 47,XXX females tested. The fact that 757 test requisition forms incorrectly noted the gender of the patient sample emphasizes the need to confirm phenotypic gender in any large scale screening program for FXS that relies on correct gender assignment for test interpretation.
The distribution of more than 170,000 normal FMR1 alleles revealed interesting patterns. Although there is a distribution around the modal size of 30 repeats, there are other repeat sizes of increased frequency, in particular 19–24, 36, 37, and 39–41. A similar observation was made previously with only 492 normal alleles.21 There have been suggestions that the presence or absence of interspersed CGG repeats might modify the stability of FMR1 alleles. Since our data are due to size alone, we have no way of knowing which alleles, if any, have interspersed CGG repeats. It will require further investigation to determine whether the allele sizes we observe in greater than expected numbers are more stable or if the allele sizes we observe in less than expected numbers are more unstable than the usual FMR1 allele.
Our analyses of 161 pregnancies confirmed that the instability of premutation alleles increases with increasing size of the alleles. We observed no allele of <59 repeats that expanded through a single meiosis to either a larger premutation allele or to a full mutation allele. This suggests the “gray zone” might be expanded from the current 45–55 repeat range to 45–59 repeat range. Premutation alleles of 59–75 repeats expanded to a larger premutation allele or full mutation allele at a rate of 17% and 5%, respectively. Premutation alleles of 76–100 expanded to larger full mutation alleles and full mutation alleles at the rate of 50% and 30%, respectively. Alleles of ≥90 repeats expanded to full alleles 100% of the time. These figures can be used for genetic counseling purposes.
References
Hagerman RJ . Physical and Behavioral Phenotype. In: Hagerman RJ, Cronister A, editors. Fragile X Syndrome, 2nd edition. Baltimore: Johns Hopkins University Press, 1996: 3–87.
Crawford DC, Meadows KL, Newman JL, Taft LF, et al. Prevalence and phenotype consequence of FRAXA and FRAXE alleles in a large, ethnically diverse, special education-needs population. Am J Hum Genet 1999; 64: 495–507.
Moore SJ, Strain L, Cole GF, Miedzybrodzka Z, et al. Fragile X syndrome with FMR1 and FMR2 deletion. J Med Genet 1999; 36: 565–566.
Parvari R, Mumm S, Galil A, Manor E, et al. Deletion of 8.5 Mb, including the FMR1 gene, in a male with the fragile X syndrome phenotype and overgrowth. Am J Med Genet 1999; 83: 302–307.
Wolff DJ, Gustashaw KM, Zurcher V, Ko L, et al. Deletions in Xq26.3-q27.3 including FMR1 result in a severe phenotype in a male and variable phenotypes in females depending upon the X inactivation pattern. Hum Genet 1997; 100: 256–262.
Grønskov K, Hallberg A, Brøndom-Nielsen K . Mutational analysis of the FMR1 gene in 118 mentally retarded males suspected of fragile X syndrome: absence of prevalent mutations. Am J Hum Genet 1998; 102: 440–445.
Maddalena A, Richard CS, McGinniss MJ, Brothman A, et al. Technical standards and guidelines for Fragile X. Genet Med 2001; 3: 200–205.
American College of Obstetricians and Gynecologists Committee on Genetics, Screening for Fragile X Syndrome. Obstet Gynecol 2006; 107: 1483–1485.
Jacquemont S, Hagerman RJ, Leehey MA, Hall DA, et al. Penetrance of the Fragile X-Associated Tremor/Ataxia Syndrome in a Premutation Carrier Population. JAMA 2004; 291: 460–469.
Nolin SL, Brown WT, Glicksman A, Houck GE Jr, et al. Expansion of the fragile X CGG repeat in females with permutation or intermediate alleles. Am J Hum Genet 2003; 72: 454–464.
Sullivan AK, Marcus M, Epstein MP, Allen EG, et al. Association of FMR1 repeat size with ovarian dysfunction. Hum Reprod 2005; 20: 402–412.
Bretherick KL, Fluker MR, Robinson WP . FMR1 repeat sizes in the gray zone and high end of the normal range are associated with premature ovarian failure. Hum Gen 2005; 117: 376–382.
Hagerman RJ, Leavitt BR, Farzin F, Jacquemont S, et al. Fragile-X-Associated Tremor/Ataxia Syndrome (FXTAS) in females with the FMR1 premutation. Am J Hum Genet 2004; 74: 1051–1056.
Pesso R, Berkenstadt M, Cuckle H, Gak E, et al. Screening for fragile X syndrome in women of reproductive age. Prenatal Diagnosis 2000; 20: 611–614.
White BJ, Ayad M, Fraser A, Entwistle T, et al. A 6-year experience demonstrates the utility of screening for both cytogenetic and FMR-1 abnormalities in patients with mental retardation. Genet Testing 1999; 3: 291–296.
O'Connell CD, Atha DH, Jakupciak JP, Amos JA, et al. Standardization of PCR amplification for Fragile X trinucleotide repeat measurements. Clin Genet 2002; 61: 13–20.
Southerland GR, Geez J, Mulley JC, et al. Fragile X Syndrome and other causes of X-linked mental retardation. In: Rimoin D, Connor JM, Pyeritz R, Korf B, editors. Emery and Rimoin's Principals and Practice of Medical Genetics, 4th edition. London: Churchill Livingston, 2002: 2804.
Crawford DC, Acuna JM, Sherman SL . FMR1 and the Fragile X syndrome: Human genome epidemiology review. Genet Med 2006; 3: 359–371.
Toledano-Alhadef H, Basel-Vanagaite L, Magal N, Davidov B, et al. Fragile-X carrier screening and the prevalence of premutation and full-mutation carriers in Israel. Am J Hum Genet 2001; 69: 351–360.
Rousseau F, Rouillard P, Morel ML, Khandijan EW, et al. Prevalence of carriers of premutation-size alleles of the FMR1 gene—and implications for the population genetics of the fragile X syndrome. Am J Hum Genet 1995; 57: 1006–1018.
Fu Y-H, Kuhl DPA, Pizzuti A, Pieretti M, Sutcliffe JS, et al. Variation of the CGG repeat at the Fragile X site results in Genetic Instability: Resolution of the Sherman Paradox. Cell 1991; 67: 1047–1058.
Strom CM, Rechitsky L, Verlinsky Y . Reliability of gender determination using the polylmerase chain reaction (PCR) for single cells. J In Vitro Fert Embryo Transfer 1991; 8: 225–229.
Hook EB, Hamerton JL . The frequency of chromosomal abnormalities detected in consecutive newborn studies–results by sex and by severity of phenotypic involvement. In: Hook EB, Porter IH, editors. Population Cytogenetics, Studies in Humans. New York: Academic Press, 1977: 63–79.
Jones KL . Smith's Recognizable Patterns of Human Malformation, 5th edition. Philadelphia: WB Saunders, 1997.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strom, C., Crossley, B., Redman, J. et al. Molecular testing for Fragile X Syndrome: Lessons learned from 119,232 tests performed in a clinical laboratory. Genet Med 9, 46–51 (2007). https://doi.org/10.1097/GIM.0b013e31802d833c
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31802d833c
Keywords
This article is cited by
-
The prevalence of CGG repeat expansion mutation in FMR1 gene in the northern Chinese women of reproductive age
BMC Medical Genetics (2019)
-
Fragile X syndrome screening in Chinese children with unknown intellectual developmental disorder
BMC Pediatrics (2015)
-
Fragile X syndrome due to a missense mutation
European Journal of Human Genetics (2014)
-
An improved Diagnostic PCR Assay for identification of Cryptic Heterozygosity for CGG Triplet Repeat Alleles in the Fragile X Gene (FMR1)
Molecular Cytogenetics (2008)