Abstract
Summary of Recommendations: The Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group found that the evidence is currently insufficient to recommend for or against the routine use of UGT1A1 genotyping in patients with metastatic colorectal cancer who are to be treated with irinotecan, with the intent of modifying the dose as a way to avoid adverse drug reactions (severe neutropenia).
Rationale: The EGAPP Working Group (EWG) found no intervention trials showing that targeted dosing of irinotecan based on UGT1A1 genotyping could reduce the rates of two specific adverse drug events, severe (Grade 3–4) neutropenia or diarrhea. Observational studies indicate a significant association between UGT1A1 genotypes, particularly *28/*28 and *1/*28, and the occurrence of severe neutropenia. Observational studies also indicate a possible association between severe diarrhea and these UGT1A1 genotypes, but the association is not statistically significant. An additional finding was the suggestion that reducing irinotecan dose may result in patient harms due to diminished effectiveness of treatment in highest risk individuals (*28/*28 homozygotes), and that a higher dose might be warranted among individuals at lower risk of adverse drug events (*1/*1 and *1/*28 genotypes). This review did not consider higher risk patients (e.g., having previous adverse reactions to irinotecan or additional risk factors for neutropenia).
Analytic Validity: The EWG found adequate evidence to conclude that analytic sensitivity and specificity were high for the commonly tested alleles, but evidence was inadequate for rarer alleles.
Clinical Validity: The EWG found adequate evidence of a significant association between UGT1A1 genotype and the incidence of severe neutropenia at standard doses of irinotecan. The EWG found adequate evidence of a possible association between genotype and severe diarrhea, but the effect was smaller and not statistically significant. The EWG found adequate evidence of a significantly higher rate of tumor response to standard irinotecan dosing among individuals with the genotype at highest risk of adverse drug events (*28/*28).
Clinical Utility: The EWG found no evidence to support clinical utility in the proposed clinical scenario. Preliminary modeling suggests that, even if targeted dosing were to be highly effective, it is not clear that benefits (reduced adverse drug events) outweigh harms (unresponsive tumors).
Contextual Issues: Addressing patient preferences regarding risk of side effects and quality of life, versus aggressive treatment to potentially improve effectiveness, is expected practice. In addition, a recent study reported that risk for neutropenia was lower at lower irinotecan doses. For treatment regimens utilizing lower irinotecan doses, UGT1A1 genotype may not be a useful indicator of risk for adverse drug events. Further rigorous evaluation of UGT1A1 genotyping using current and promising irinotecan treatment protocols is warranted.
Similar content being viewed by others
CLINICAL CONSIDERATIONS
Patient population under consideration
Colorectal cancer (CRC) will be diagnosed in an estimated 150,000 individuals in 2007, resulting in 52,000 deaths. No direct estimate of irinotecan use is available, but about 15% of cases (22,500) have “distant” CRC and may be candidates for irinotecan therapy.
Testing (UGT1A1 genotyping)
Of the 60 or more UGT1A1 gene variants, two are responsible for 98–99% of the genotypes found in the US white population. These are named *1 (the “wild” sequence of (TA)6TAA) and *28 (with an extra TA repeat or (TA)7TAA).
-
44% of the US white population are homozygous for *1 (genotype *1/*1);
-
45% are heterozygous (genotype *1/*28); and
-
11% (about 1 in 10) are homozygous for *28 (genotype *28/*28).
Reliable UGT1A1 genotyping is available using the US Food and Drug Administration (FDA)-cleared kit or through a laboratory developed test. FDA clearance provides assurance that the test is analytically valid, and the results are related to an outcome of interest, but FDA does not evaluate clinical utility.
Clinical implications
When compared with individuals with the *1/*1 genotype, individuals with the *28/*28 genotype:
-
Metabolize the active form of irinotecan (SN-38) more slowly and, therefore, have a longer time-weighted exposure;
-
Have a significant 3.5-fold increase in the rate of severe (Grade 3/4) neutropenia (heterozygotes are intermediate with a nonsignificant 1.8-fold increase);
-
Have a nonsignificant 1.6-fold increase in the rate of severe (Grade 3/4) diarrhea (heterozygotes are intermediate with a nonsignificant 1.4-fold increase); and
-
Have a significant 1.7-fold increase in the tumor response rate to treatment (heterozygotes are similar to the reference category, with a nonsignificant 1.1-fold increase).
Clinical utility of UGT1A1 genotyping
The clinical utility of routine reduction of initial irinotecan dose in *28 homozygotes based on UGT1A1 genotyping is unknown. No study has prospectively documented the potential benefits (reduced adverse drug events) or harms (reduced proportion of responsive tumors).
Clinical caveats
-
Some evidence exists that when lower doses of irinotecan are routinely used, the lower rate of adverse drug events is not related to UGT1A1 genotype. However, the clinical effectiveness of lower dosing is not clear.
-
Selective genotyping based on patient preferences is possible. Among those individuals wanting aggressive treatment, genotyping might allow higher dosing among the *1/*1 and *1/*28 groups. Alternatively, individuals wanting to maximize quality of life may chose lower dosing if found to be *28/*28.
-
Alternate drug use is possible, based on patient preference (e.g., cetuximab or bevacizumab) without genotyping, or if a *28/*28 individual is identified.
-
The National Comprehensive Cancer Network recommends pretreatment with colony-stimulating factors for individuals with a 20% or greater risk of febrile neutropenia.1
-
The rate of severe neutropenia is as high as 36% among *28/*28 individuals, but the proportion with associated fever is unknown.
BACKGROUND AND CLINICAL CONTEXT FOR THE RECOMMENDATION
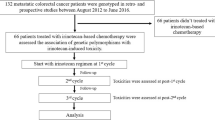
CRC is the third leading cause of new cancers in the United States, with nearly 150,000 cases diagnosed per year in 2007. More than 52,000 deaths from CRC were expected in 2007.2 In patients with newly diagnosed CRC, staging of tumors is performed to determine the extent and location of the tumor, to inform appropriate treatment strategies, and to provide information on prognosis.3 For the 70–80% of patients who present with “apparently resectable localized disease;” optimal treatment is usually considered to be surgery followed by adjuvant therapy for high risk cases.4–6 CRC patients with advanced disease at diagnosis may receive first-line systemic chemotherapy, or chemotherapy and radiation therapy, either followed by surgery or used palliatively if surgery is not indicated.5
Chemotherapy regimens using irinotecan in combination with 5-fluorouracil and leucovorin or other drugs are commonly prescribed for first-line and sequential therapy for metastatic CRC.5,7–9 In patients >50 years of age, about 15% have “distant” cancer and might be candidates for irinotecan therapy; however, no published data provide a direct estimate of potential irinotecan use. It seems likely that the number of patients who ultimately receive irinotecan will continue to increase as FDA approves other new chemotherapeutic agents that may be used with irinotecan in second-line therapy of CRC, and with the increase in the number of patients surviving to progress from first-line to second-line treatment.5,10
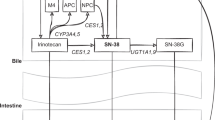
Irinotecan is a prodrug of the plant alkaloid camptothecin, a topoisomerase I inhibitor.11–13 Irinotecan is activated by the enzyme carboxylesterase to the active metabolite SN-38. Metabolism of this active form of irinotecan (SN-38) to an inactive form (SN-38G) is catalyzed by hepatic and extrahepatic UGT enzymes. The major isozyme involved is UGT1A1, but others also have some role (UGT1A 6, 7, 9, 10).14 One UGT1A1 polymorphism (*28) is most strongly associated with reduced clearance of the active form of irinotecan. Therefore, individuals with no copies of this polymorphism (UGT1A1 *1/*1) have average levels of the enzyme and will metabolize SN-38 more quickly than either heterozygotes (UGT1A1 *1/*28) or homozygotes (UGT1A1 *28/*28). Higher exposure of *28 homozygotes to the active form of the drug is thought to explain some of the adverse drug events (e.g., severe neutropenia and diarrhea) that increase morbidity and mortality directly or indirectly (e.g., delay chemotherapy).12,15
If the dosage of irinotecan in patients with metastatic CRC can be modified based on genotype while maintaining the effectiveness of cancer treatment, it is possible that some proportion of the severe adverse drug effects can be reduced. Whether this potential can be realized in practice, and whether reduction in dosage might negatively impact response to therapy, is unclear. In an attempt to answer this question, Evaluation of Genomic Applications in Practice and Prevention (EGAPP) commissioned an evidence-based review to address the following specific clinical scenario (overarching question):
Does testing for UGT1A1 mutations in patients with metastatic CRC treated with irinotecan lead to improvement in outcomes?
REVIEW OF SCIENTIFIC EVIDENCE
This statement summarizes the supporting scientific evidence used by the EGAPP Working Group (EWG) to make recommendations regarding UGT1A1 genotyping in patients with CRC treated with irinotecan.
Methods
EGAPP is a project developed by the National Office of Public Health Genomics at the Centers for Disease Control and Prevention designed to support a rigorous, evidence-based process for evaluating genetic tests and other genomic applications that are in transition from research to clinical and public health practice in the United States.16 A key goal of the EWG is to develop conclusions and recommendations regarding clinical genomic applications and to establish clear linkage to the supporting scientific evidence. The EWG members are nonfederal multidisciplinary experts convened to establish methods and processes, set priorities for review topics, participate in technical expert panels for commissioned evidence reviews, and develop and publish recommendations.17
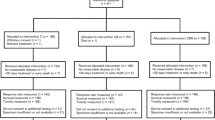
Evidence reviews are designed around specific clinical scenarios from which analytic frameworks and key questions are constructed that are then converted into explicit literature strategies. Standard methods are used to judge the quality of the evidence at the level of individual articles, and the certainty of the body of evidence around a particular question. The process considers the evidence and selected contextual factors before reaching one of three general conclusions: (1) EGAPP recommends use of the test; (2) EGAPP recommends against use of the test; or (3) EGAPP finds the evidence insufficient to recommend use of the test.18 Finally, EGAPP comments on key gaps in the evidence that might be addressed in future research.
The review focused on evaluation of UGT1A1*28 genotyping in whites. One technical contractor conducted an initial review of the literature on clinical validity and utility. A second review group completed the systematic review by searching literature on analytic validity and population allele/genotype frequencies, updating the previous searches, and performing summarization and statistical analyses before producing the final report. Methods followed in conducting this review are well described in the evidence report19 and the accompanying article summarizing the evidence.20 A Technical Expert Panel (including EWG members) advised the reviewers in designing the literature search strategies, defining study inclusion and exclusion criteria, extracting and evaluating the quality of evidence, developing evidence tables, and addressing various substantive questions as the review proceeded. The evidence report and this recommendation statement were each peer reviewed before being finalized. EWG members reviewed in the evidence report, examined other sources of information as needed to address specific gaps in the evidence, and considered contextual issues related to implementation of testing in clinical practice. The final recommendation was formulated based on magnitude of effect, certainty of evidence, and consideration of contextual factors.
Technology
When the UGT1A1 promoter has the wild-type sequence (TA)6TAA, levels of the UGT1A1 enzyme are normal. The insertion of an extra dinucleotide repeat in the promoter region of the gene—(TA)7TAA (UGT1A1*28 variant)—results in reduced gene expression. Resulting enzyme levels appear to vary substantially but are reduced by about 25% compared with normal in UGT1A1*28 heterozygotes, and by 50–70% compared with normal in UGT1A1*28 homozygotes.12,21 The homozygous UGT1A1*28 genotype is found in about 10% of the North American population; prevalence is variable depending on race.19,20,22
Several laboratories offer genetic testing for UGT1A1 variants using different test formats. Laboratories may develop and validate their own, in-house tests for UGT1A1 genotyping, known as laboratory developed tests. A significant development was the clearance by the FDA Center for Devices and Radiological Health (CDRH) of the Third Wave Invader® UGT1A1 Molecular Assay (testing for UGT1A1*28 and UGT1A1*1) under 510(k) rules for Drug Metabolizing Enzyme Genotyping Systems.23,24 In approving companion diagnostics for drugs, CDRH requires evidence to support the test's clinical validity; data on clinical utility are reported if available but are not required. A change to the Camptosar® (irinotecan) (Pfizer, New York) package insert prescribing information had been approved by the FDA Center for Drug Evaluation and Research in 2004 in order to alert clinicians that a reduction in starting dose of the drug should be considered for UGT1A1*28 homozygotes, who are at increased risk for neutropenia.22,25 However, the revised prescribing information includes the caution that “the precise dose reduction in this patient population is not known and subsequent dose modifications should be considered based on individual patient tolerance to treatment.”22
Analytic validity
Analytic validity refers to the test's ability to accurately and reliably measure the genotype of interest and includes measures of analytic sensitivity and specificity, reproducibility, assay robustness, and quality control. Four studies were identified that addressed analytic validity of genetic tests for UGT1A1 variants against the reference standard of sequencing.24,26–28 One describes a methodology not likely to be used in current practice (radioactive polymerase chain reaction [PCR]),27 one provides data on denaturing high performance liquid chromatography (DHPLC),28 and two report on tests using the Invader technology.24,26
Despite the heterogeneity in methods, the overall estimate of analytic sensitivity was 100% for UGT1A1 genotypes containing the *28 allele (referent test: sequencing; 95% confidence interval [CI] 98–100%) and genotypes containing the less common*6 allele (referent test: PCR-RFLP [polymerase chain reaction-restriction fragment length polymorphism-based methodology]; 95% CI 98–100%). Few data are available to support estimates of analytic sensitivity for other promoter (*36, *37) and exon 1 variants (*6, *27).26 The overall estimate of analytic specificity was 100% (referent method: sequencing; 95% CI 97–100%). A subsequent study supported these earlier findings, comparing sequencing, the Invader in vitro device (IVD), and PCR/capillary electrophoresis.29 A three-center study of assay reproducibility for the Invader IVD test is available as part of the FDA summary, and reported an overall correct call rate of 98.8%.24
Estimates of first run failure rates in UGT1A1*1 and *28 were 5.0% for sequencing, 1.7% for PCR/capillary electrophoresis,29 and 6.7% for an Invader research use only assay26; all were resolved on repeat testing. The Invader IVD test had initial failure rate of 5.4% (95% CI 4.1–7.1%), most resolved by retesting,24 but a more recent study reported the Invader test failed on first and second runs in 7.6% of samples (95% CI 3.5–13.9%).29
An external proficiency testing program is available through the College of American Pathologists Pharmacogenetics Survey, cosponsored by College of American Pathologists and the American College of Medical Genetics.30
Analytic validity conclusions
The quality of evidence for the analytic validity of current UGT1A1 genetic testing methods is adequate, and available data indicate that both analytic sensitivity and specificity for the common genotypes (*1 and *28) are high. Estimates for rarer alleles were less reliable because of small numbers.
Clinical validity
The clinical validity of a genetic test defines how well test results correlate with the intermediate or final outcomes of interest.
Association of genotype with phenotypic markers (e.g., increased plasma SN-38 levels) and associated adverse drug reactions (e.g., severe neutropenia or diarrhea)
There is a clear association between UGT1A1 genotype and the ratio of the area under the curve (AUC) for SN-38G (inactive form) to the AUC for SN-38 (active form). Homozygotes (*28/*28) have about twice the exposure to the active form, due to slower metabolism of the drug compared with the wild genotype.19 However, there is significant overlap in these ratios between the three main genotypes.
Association of genotype with adverse drug reactions in observational studies
Table 1 provides the rates of severe neutropenia and diarrhea and clinical response stratified by genotype.
These results indicate a significant association between genotype and severe neutropenia at standard doses of irinotecan. There is a positive dose response between genotype and severe diarrhea, but this association is not statistically significant.
Association of genotype with tumor response in observational studies
At standard doses of irinotecan, the tumor response rates were 41% for wild type, 45% for *28 heterozygotes, and 70% for *28 homozygotes (Table 1). The risk ratio for *28 homozygotes versus wild-type individuals is 1.70 (95% CI 1.24–2.33), which is statistically significant. This suggests that wild-type individuals may be relatively under dosed, meaning that they are receiving a less-effective dose than *28 homozygotes at the same dose administered. That is, the higher serum levels of irinotecan in *28 homozygous individuals are associated with improved tumor response, compared with wild-type individuals.
Modeling
Modeling based on evidence to date suggests a tradeoff between the harms and benefits of dose reduction of irinotecan, based on UGT1A1 genotyping.19,20 If the reduction in dosage is highly effective in reducing or eliminating cases of severe neutropenia (70–100% effective) then the avoidance of one case of neutropenia is associated with one additional unresponsive tumor. At lower rates of effectiveness (20–50%), there are likely to be 2–5 times as many nonresponsive tumors as avoided cases of severe neutropenia.
Limitations
In general, evaluation of clinical validity was limited by the small number of studies. Further, some of the included studies did not focus exclusively on CRC patients. The majority of studies reported patients with Grade 3 and Grade 4 neutropenia as one group, making individual analysis for Grade 4 neutropenia not feasible. The clinical validity of UGT1A1 variants other than that of *28 in whites was not assessed.
Clinical validity conclusions
The EWG found convincing evidence for a significant association between UGT1A1*28 genotypes and the incidence of severe neutropenia at standard doses of irinotecan. The association between genotype and severe diarrhea is not as strong. There is a significantly higher tumor response rate in *28 homozygous individuals, suggesting that the standard dose of irinotecan may not be optimal for wild genotype individuals in terms of tumor response.
Clinical utility
The clinical utility of a genetic test is the likelihood that using the test to guide drug choice or dose will significantly improve health-related patient outcomes, such as fewer adverse events and/or reduced mortality. No studies addressed the influence of UGT1A1 genotyping results on irinotecan prescribing decisions. No studies used UGT1A1 genotyping to guide irinotecan choice or dose, and documented subsequent patient outcomes.
Observational studies in which individuals with all three genotypes were treated at standard doses show that *28 homozygotes are significantly more likely to have a responsive tumor than those with no copies.31,37 Heterozygotes have intermediate tumor response rates that are not significantly higher. Several, but not all, studies have shown longer survival among *28 homozygotes.33,36–38 These data suggest that reducing the dose of irinotecan (as would occur with personalized dosing) may result in patient harms due to the treatment being less effective. Further, it suggests that a higher dose might be warranted among individuals with one or no copies. Modeling suggests that even with high efficacy for targeted dosing to reduce adverse drug events, a reduced dose may lead to more cases of unresponsive tumors than adverse drug events avoided. A recent meta-analysis showed a statistically significant association between UGT1A1 genotype and severe neutropenia at medium and high doses of irinotecan (≥150 mg/m2) but did not find the association at doses <150 mg/m2.39 These findings support an earlier suggestion that, unless patients receive irinotecan at a dose greater than150 mg/m2, either alone or in combination with a myelotoxic drug, or irinotecan at 100 mg/m2 in combination with another marrow-toxic agent (e.g., oxaliplatin), the increase in risk for toxicity is “neither statistically nor clinically significant” and testing may not be warranted.40 Additional research is necessary to better define the clinical utility of UGT1A1 testing.
Clinical utility conclusions
The EWG found no prospective trials showing that targeted dosing of irinotecan based on UGT1A1 genotyping could reduce the rates of adverse drug events. No evidence exists to support clinical utility for this clinical scenario.
Research gaps
The EWG found the literature insufficient in many respects, and examining the deficiencies can be helpful in describing studies that could fill the gaps and help to set a research agenda.
-
Prospective studies of UGT1A1 genotyping and clinical decision making and clinical outcomes (benefits and harms) are needed to answer the over-arching question of clinical utility. Best evidence would come from adequately powered, controlled clinical trials that compare patient outcomes when treatment is informed by genotyping tests versus empirical treatment. Such trials will be important to determine best management practices with respect to UGT1A1 testing.
-
Alternatively, prospective studies could address more limited clinical scenarios, such as the potential value of using UGT1A1 testing to manage the subset of patients who have experienced serious adverse drug reactions with irinotecan, or who are already at increased risk for neutropenia based on other factors.
-
Additional data and similar analyses are needed for other UGT1A1 polymorphisms, including distribution and allele frequencies in different racial/ethnic groups and their phenotypic effects.
-
The association between UGT1A1 genotype and severe diarrhea is weaker and more variable than the association of UGT1A1 genotype and neutropenia. Additional well-designed studies are warranted to help explain the heterogeneity in the literature and to more confidently estimate the true effect.
-
Data to date suggest that the higher exposures to the active form of irinotecan (SN-38) experienced by *28 homozygotes may be associated with improved tumor response compared with individuals with one or no *28 alleles. Therefore, research should determine whether increases in irinotecan dose above current standard doses in individuals with one *28 allele or the wild genotype can safely increase drug level and improve tumor response.
-
Prospective studies of patient outcomes, including modification of dosage based on genotyping results, are needed to determine and assess the magnitudes of benefits and harms.
-
Introduction of tests should be accompanied by key measurements supporting the analytic sensitivity and specificity, reproducibility and robustness of the proposed method.
-
General studies are needed to address the acceptability of pharmacogenetic testing to clinicians and to individuals with metastatic CRC. The possibilities of harm from stigma, discrimination or adverse family impacts from UGT1A1 genotyping in this context are low. Nevertheless, attitudes and subjective experiences with testing would be valuable to ascertain.
Recommendations of other groups
EGAPP did not find recommendations from other groups regarding UGT1A1 testing in patients treated with irinotecan.
Contextual issues important to the recommendation
There is insufficient evidence to support a recommendation for or against use of UGT1A1 testing in adults with metastatic CRC treated with irinotecan. In the absence of evidence supporting clinical utility, additional contextual issues were taken into account in formulating the final EWG recommendation.
Contextual issues that suggest the potential benefits of UGT1A1 genotyping
-
CRC is a major public health problem in the United States, causing substantial morbidity and mortality.
-
Irinotecan is a commonly used chemotherapeutic agent that appears to be effective as a first-line or second-line agent.
-
Potentially avoidable irinotecan-related adverse reactions, such as severe neutropenia and diarrhea, are relatively common. Depending on severity, these adverse reactions can reduce overall quality of life and, in some cases, be life threatening.
-
A number of therapeutic regimens are available for the treatment of CRC, including regimens that do not involve irinotecan. Therefore, individuals identified to be at increased risk for serious adverse reactions related to irinotecan may have alternative treatment options.
-
UGT1A1 genetic testing may be of benefit in individual cases when used by knowledgeable practitioners who are informed about the potential benefits and harms of genotyping in this context.
-
Considering patient preferences may be reasonable on a case by case basis to address patient preferences about risk factors and quality of life versus aggressive treatment to potentially improve effectiveness.
-
Limited evidence for improved survival among *28 homozygotes suggests the possibility that wild genotype individuals are being under dosed.
Contextual issues that suggest the potential harms of UGT1A1 genotyping
-
Utilization of UGT1A1 testing in this clinical scenario and impact on physician decision making is not known.
-
Reductions in irinotecan dosage resulting from information gained through UGT1A1 genotyping may reduce tumor response and survival.
Other contextual issues regarding UGT1A1 genotyping
-
Although the cost of UGT1A1 genotyping on an individual level may be relatively low in the context of cancer treatment, the potential for increased cost of widespread use may not be justifiable without evidence supporting clinical utility and improved outcomes.
-
Other options may be considered for individuals who are homozygous for UGT1A1*28. For example, the National Comprehensive Cancer Network recommends pretreatment with colony stimulating factor for individuals at a 20% or higher risk of febrile neutropenia.1
REFERENCES
NCCN Myeloid Growth Factors Panel Members. Myeloid Growth Factors V. 1.2008–NCCN clinical practice guidelines in oncology. Available at: http://www.nccn.org/professionals/physician_gls/PDF/myeloid_growth.pdf. Accessed January 25, 2008.
Cancer Facts & Figures 2007. American Cancer Society. Available at: http://www.cancer.org/downloads/STT/CAFF2007PWSecured.pdf. Accessed June 11, 2008.
American Joint Committee on Cancer AJCC cancer staging manual, 6th ed. New York: Springer, 2002.
Pessino A, Sobrero A . Optimal treatment of metastatic colorectal cancer. Expert Rev Anticancer Ther 2006; 6: 801–812.
Saunders M, Iveson T . Management of advanced colorectal cancer: state of the art. Br J Cancer 2006; 95: 131–138.
Van Cutsem E, Verslype C, Demedts I . The treatment of advanced colorectal cancer: where are we now and where do we go?. Best Pract Res Clin Gastroenterol 2002; 16: 319–330.
Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin 2006; 56: 106–130.
Kelly H, Goldberg RM . Systemic therapy for metastatic colorectal cancer: current options, current evidence. J Clin Oncol 2005; 23: 4553–4560.
Wolpin BM, Meyerhardt JA, Mamon HJ, Mayer RJ . Adjuvant treatment of colorectal cancer. CA Cancer J Clin 2007; 57: 168–185.
Goldberg RM, Sargent DJ, Morton RF, et al. Randomized controlled trial of reduced-dose bolus fluorouracil plus leucovorin and irinotecan or infused fluorouracil plus leucovorin and oxaliplatin in patients with previously untreated metastatic colorectal cancer: a North American Intergroup Trial. J Clin Oncol 2006; 24: 3347–3353.
Toffoli G, Cecchin E, Corona G, Boiocchi M . Pharmacogenetics of irinotecan. Curr Med Chem Anticancer Agents 2003; 3: 225–237.
Miners JO, McKinnon RA, Mackenzie PI . Genetic polymorphisms of UDP-glucuronosyltransferases and their functional significance. Toxicology 2002; 181-182: 453–456.
Mathijssen RH, van Alphen RJ, Verweij J, et al. Clinical pharmacokinetics and metabolism of irinotecan (CPT-11). Clin Cancer Res 2001; 7: 2182–2194.
Nagar S, Blanchard RL . Pharmacogenetics of uridine diphosphoglucuronosyltransferase (UGT)1A family members and its role in patient response to irinotecan. Drug Metab Rev 2006; 38: 393–409.
Innocenti F, Undevia SD, Iyer L, et al. Genetic variants in the UDP-glucuronosyltransferase 1A1 gene predict the risk of severe neutropenia of irinotecan. J Clin Oncol 2004; 22: 1382–1388.
Centers for Disease Control and Prevention: Evaluation of Genomic Applications in Practice and Prevention (EGAPP). Available at: http://www.cdc.gov/genomics/gtesting/EGAPP/about.htm. Accessed June 6, 2008.
Evaluation of Genomic Applications in Practice and Prevention (EGAPP): implementation and evaluation of a model approach. Available at: http://www.egappreviews.org/. Accessed June 6, 2008.
Teutsch SM, Bradley LA, Palomaki GE, et al. The Evaluation of Genomic Applications in Practice and Prevention (EGAPP) initiative: methods of the EGAPP working group. Genet Med 2009; 11: 3–14.
Bradley LA, Palomaki GE, Dotson WD, et al. Evidence report: can UGT1A1 genotyping reduce morbidity and mortality in patients with metastatic colorectal cancer treated with irinotecan. Available at: http://www.egappreviews.org.
Palomaki GE, Bradley LA, Douglas MP, et al. Can UGT1A1 genotyping reduce morbidity and mortality in patients with metastatic colorectal cancer treated with irinotecan: an evidence-based review. Genet Med 2009; 11: 21–34.
Iyer L, King CD, Whitington PF, et al. Genetic predisposition to the metabolism of irinotecan (CPT-11). Role of uridine diphosphate glucuronosyltransferase isoform 1A1 in the glucuronidation of its active metabolite (SN-38) in human liver microsomes. J Clin Invest 1998; 101: 847–854.
Camptosar Full Prescribing Information. Available at: http://www.pfizer-.com/files/products/uspi_camptosar.pdf. Accessed June 5, 2008.
US Food and Drug Administration. FDA News. FDA clears genetic test that advances personalized medicine: test helps determine safety of drug therapy. Available at: http://www.fda.gov/bbs/topics/NEWS/2005/NEW01220.html. Accessed July 17, 2008.
Invader®UGT1A1 Molecular Assay 510K Summary. Available at: http://www.fda.gov/cdrh/pdf5/K051824.pdf#search=%22Invader%C2%AE%20UGT1A1%20Molecular%20Assay%20%20510k%20summary%22. Accessed July 17, 2008.
Ramchandani RP, Wang Y, Booth BP, et al. The role of SN-38 exposure, UGT1A1*28 polymorphism, and baseline bilirubin level in predicting severe irinotecan toxicity. J Clin Pharmacol 2007; 47: 78–86.
Hasegawa Y, Sarashina T, Ando M, et al. Rapid detection of UGT1A1 gene polymorphisms by newly developed Invader assay. Clin Chem 2004; 50: 1479–1480.
Monaghan G, Ryan M, Seddon R, et al. Genetic variation in bilirubin UPD-glucuronosyltransferase gene promoter and Gilbert's syndrome. Lancet 1996; 347: 578–581.
Pirulli D, Giordano M, Puzzer D, et al. Rapid method for detection of extra (TA) in the promoter of the bilirubin-UDP-glucuronosyl transferase 1 gene associated with Gilbert syndrome. Clin Chem 2000; 46: 129–131.
Baudhuin LM, Highsmith WE, Skierka J, et al. Comparison of three methods for genotyping the UGT1A1 (TA)n repeat polymorphism. Clin Biochem 2007; 40: 710–717.
College of American Pathologists. 2008 Surveys & Anatomic Pathology Education Programs. Biochemical and molecular genetics–pharmacogenetics (PGx). Available at: http://www.cap.org/apps/docs/proficiency_testing/surveys_catalog/2008_full_catalog.pdf. Accessed June 6, 2008.
Carlini LE, Meropol NJ, Bever J, et al. UGT1A7 and UGT1A9 polymorphisms predict response and toxicity in colorectal cancer patients treated with capecitabine/irinotecan. Clin Cancer Res 2005; 11: 1226–1236.
Iyer L, Das S, Janisch L, et al. UGT1A1*28 polymorphism as a determinant of irinotecan disposition and toxicity. Pharmacogenomics J 2002; 2: 43–47.
Marcuello E, Altes A, Menoyo A, et al. UGT1A1 gene variations and irinotecan treatment in patients with metastatic colorectal cancer. Br J Cancer 2004; 91: 678–682.
Massacesi C, Terrazzino S, Marcucci F, et al. Uridine diphosphate glucuronosyl transferase 1A1 promoter polymorphism predicts the risk of gastrointestinal toxicity and fatigue induced by irinotecan-based chemotherapy. Cancer 2006; 106: 1007–1016.
Rouits E, Boisdron-Celle M, Dumont A, et al. Relevance of different UGT1A1 polymorphisms in irinotecan-induced toxicity: a molecular and clinical study of 75 patients. Clin Cancer Res 2004; 10: 5151–5159.
Font A, Sanchez JM, Taron M, et al. Weekly regimen of irinotecan/docetaxel in previously treated non-small cell lung cancer patients and correlation with uridine diphosphate glucuronosyltransferase 1A1 (UGT1A1) polymorphism. Invest New Drugs 2003; 21: 435–443.
Toffoli G, Cecchin E, Corona G, et al. The role of UGT1A1*28 polymorphism in the pharmacodynamics and pharmacokinetics of irinotecan in patients with metastatic colorectal cancer. J Clin Oncol 2006; 24: 3061–3068.
Côté JF, Kirzin S, Kramar A, et al. UGT1A1 polymorphism can predict hematologic toxicity in patients treated with irinotecan. Clin Cancer Res 2007; 13: 3269–3275.
Hoskins JM, Goldberg RM, Qu P, et al. UGT1A1*28 genotype and irinotecan-induced neutropenia: dose matters. J Natl Cancer Inst 2007; 99: 1290–1295.
McLeod H . To test or not to test: an update on UGT1A1 testing. Oncol Issues 2006; 21: 20–22.
Author information
Authors and Affiliations
Consortia
Additional information
Disclaimer: This recommendation statement is a product of the independent EGAPP Working Group. Although the Centers for Disease Control and Prevention (CDC) provides support to the EGAPP Working Group, including staff support in the preparation of this document, recommendations made by the EGAPP Working Group should not be construed as official positions of the CDC or the US Department of Health and Human Services.E-mail: egappinfo@egappreviews.org.Disclosure: Steven Teutsch is an employee, option and stock holder in Merck & Co., Inc.
Rights and permissions
About this article
Cite this article
Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group. Recommendations from the EGAPP Working Group: can UGT1A1 genotyping reduce morbidity and mortality in patients with metastatic colorectal cancer treated with irinotecan?. Genet Med 11, 15–20 (2009). https://doi.org/10.1097/GIM.0b013e31818efd9d
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31818efd9d
Keywords
This article is cited by
-
Collaborative Group of the Americas on Inherited Gastrointestinal Cancer Position statement on multigene panel testing for patients with colorectal cancer and/or polyposis
Familial Cancer (2020)
-
Individualization of Irinotecan Treatment: A Review of Pharmacokinetics, Pharmacodynamics, and Pharmacogenetics
Clinical Pharmacokinetics (2018)
-
The Routine Clinical use of Pharmacogenetic Tests: What it Will Require?
Pharmaceutical Research (2017)
-
A Single Institution Experience in Compliance with Universal Screening for Lynch Syndrome in Colorectal Cancer
Journal of Gastrointestinal Surgery (2015)
-
The EGAPP initiative: lessons learned
Genetics in Medicine (2014)