Abstract
Purpose: Nail-Patella syndrome (MIM 161200) is a rare autosomal dominant disorder characterized by hypoplastic or absent patellae, dystrophic nails, dysplasia of the elbows, and iliac horn. In 40% of cases, a glomerular defect is present and, less frequently, ocular damage is observed. Inter- and intrafamilial variable expressivity of the clinical phenotype is a common finding. Mutations in the human LMX1B gene have been demonstrated to be responsible for Nail-Patella syndrome in around 80% of cases.
Methods: Standard polymerase chain reaction and sequencing methods were used for mutation and single nucleotide polymorphism identification and control of cloned sequences. Array-CGH (Agilent, 244A Kit) was used for detection of deletions. Standard cloning techniques and the Snapshot method were used for analysis of mosaicism.
Results: In this study, we present the results of LMX1B screening of 20 Nail-Patella syndrome patients. The molecular defect was found in 17 patients. We report five novel mutations and a ∼2 Mb deletion in chromosome 9q encompassing the entire LMX1B gene in a patient with a complex phenotype. We present evidence of somatic mosaicism in unaffected parents in two cases, which, to our knowledge, are the first reported cases of inheritance of a mutated LMX1B allele in Nail-Patella syndrome patients from a mosaic parent.
Conclusion: The study of the described case series provides some original observations in an “old” genetic disorder.
Similar content being viewed by others
Main
Nail-Patella syndrome (NPS), or hereditary onycho-osteodysplasia (MIM 161200), is a rare autosomal dominant disorder, first reported by Little1 in 1897, characterized by hypoplastic or absent patellae, dystrophic nails, dysplasia of the elbows, and iliac horn. In the skeletal system, tendons, ligaments, and muscles as well as bones can be affected.2 Ophthalmologic abnormalities include increased ocular pressure, glaucoma, and subsequent blindness. The most serious manifestation of NPS is nephropathy that can be found in 40% of patients.2,3 The earliest clinical findings are proteinuria and hematuria. Ten percent of NPS may progress to nephrotic syndrome and/or end-stage renal disease. Recent studies suggest that NPS phenotype may be more extensive than previously described including neurologic and neurobehavioral aspects.4
Most NPS cases are associated with heterozygous mutations in the LIM homeobox transcription factor 1 beta gene (LMX1B, MIM 602575),2 a member of the LIM-homeodomain family of transcription factors, that play a vital role during embryo development by determining body pattern in vertebrates and invertebrates.
The LMX1B gene is mapped on chromosome 9q34.1.5 It consists of eight exons spanning a region of ∼82 kb of genomic DNA and encodes about 372 amino acid residues of protein.2 The protein contains two zinc-binding LIM domains at the NH2-terminus and a DNA-binding homeodomain.2
During embryo development, LMX1B plays multiple roles.6 It is expressed in the dorsal mesenchyme of the limb bud, is responsible for the dorsal-ventral patterning, and is essential for the differentiation of metanephric precursor cells into podocytes and, possibly, for the maintenance of the differentiated status. Moreover, LMX1B expression has also been shown during the development of the central nervous system and seems to be essential for the development of serotonergic neurons. In accordance with the expression pattern, knock-out mice for targeted inactivation of Lmx1b showed a strongly resembling phenotype for NPS with absent nails and patellae and characteristic ultrastructural changes of the glomerular basement membrane in the kidneys.7
The incidence of the disease is estimated as 1 in 50,000 live births, with high penetrance and an extremely variable clinical presentation both within and among families. LMX1B reported mutations include a wide spectrum of substitutions, small insertions/deletions and splice site mutations, concentrated within the functional domains of the protein: LIM domains (LIM-A 44%, LIM-B 38%) and the homeodomain (18%).2,8 The most frequently recurring mutations have been found in the homeodomain (R198X, R200Q, R208X, A213P, and R223X), which comprises nearly 30% of all known LMX1B mutations.
So far, no evidence for locus heterogeneity has been reported. Recently, for the first time, deletions affecting the whole LMX1B gene or part of it were reported. Two deletions of the whole gene and another affecting exons 3 to 8 were identified in a series of eight unrelated families with classical features of NPS.9
Although it is possible that apparently negative cases actually carry mutations affecting regulatory regions essential for gene expression either at the 5′ end of the gene, or within introns, or in the 3′ untranslated regions, no such mutations have been so far reported as unequivocally causative.
No correlation in the range of severity of NPS symptoms has been reported among patients with missense, nonsense, frameshift, or splice mutations and those with large deletions of most or all the gene, strongly supporting haploinsufficiency for LMX1B as the mechanism underlying NPS.2,9
We describe here the results of LMX1B screening in a series of NPS patients. Besides mutations already reported in the literature, we describe five previously unreported mutations and a deletion in chromosome 9q that includes the entire LMX1B gene in a patient with a more complex phenotype. We describe somatic mosaicism in unaffected parents in two cases, which, to our knowledge, are the first reported cases of inheritance of a mutated LMX1B allele in NPS patients from a mosaic parent.
MATERIALS AND METHODS
Patients
This case series includes 20 patients with a clinical diagnosis of NPS, referred to our center. Peripheral blood samples were obtained from patients, in some cases from their parents also, and from control individuals, after obtaining informed consent.
DNA extraction, PCR, and sequencing reactions
Genomic DNA was extracted from peripheral blood samples with the Puregene Blood Kit (Gentra Systems, Minneapolis, MN) according to the manufacturer's procedure. Oligonucleotides and conditions used to amplify the LMX1B coding sequence were already described.10 Polymerase chain reactions (PCR) were performed in a total volume of 20 μL containing 1 × PCR Buffer (Applied Biosystems, Foster City, CA), 200 μM dNTPs mix, 1.5 mM MgCl2, 10 pmoles of each oligonucleotide, 1 U of AmpliTaq Gold Polymerase (Applied Biosystems).
PCR products were checked by standard agarose gel electrophoresis and purified by Exo/SAP-IT (USB Europe GmbH) digestion as suggested by the manufacturer's procedure. Sequencing reactions were set up with a Big Dye Terminator Cycle Sequencing Kit (Applied Biosystems) according to the provided protocol and run on a 3130xl Genetic Analyzer (Applied Biosytems).
Mosaicism analysis
After observing the presence of a low intensity mutated nucleotide in the sequencing electropherogram, PCR products of the LMX1B exon 4 obtained from the mosaic parent of patients 4 and 19 were subcloned using the TOPO-TA cloning Kit (Invitrogen, Carlsbad, CA) to verify the presence of two different alleles. Ten colonies were selected for each amplimer and grown overnight in Luria-Bertani medium. Plasmids were then recovered with the IllustraTM plasmid Prep Mini Spin Kit (GE Healthcare, Chalfont St. Giles, UK) according to the provided protocol. Plasmid DNA was sequenced by using the M13 Forward and Reverse vector primers included in the TOPO-TA cloning kit (Invitrogen) and the Big Dye Terminator Cycle Sequencing Kit (Applied Biosystems) as already described. The Snapshot method was used according to the instructions provided by the purchasing company (Applied Biosystems).
Single nucleotide polymorphisms genotyping
Three clusters (A, B, and C; Table 1) of single nucleotide polymorphisms (SNP) mapping in LMX1B introns 1, 3, and 6, respectively, were selected from the SNP database (dbSNP, www.ncbi.nlm.nih.gov). Genotyping by PCR amplification (see Table 1 for primers sequences) and direct sequencing of the purified product, as already described, was then performed.
CGH array analysis
The search for deletions in patient NPS5 was performed using the Agilent Human Genome CGH Microarray Kit 244A (Agilent Technologies, Santa Clara, CA). This platform is a 60-mer oligonucleotide-based microarray that allows genome-wide survey and molecular profiling of genomic aberrations with a resolution of ∼35 kb.
Labeling and hybridization were performed following the protocols provided by Agilent. Briefly, 1 μg of purified DNA of patient and a control (Promega Corporation, Madison, WI) were double digested with RSAI and AluI for 2 hours at 37° degrees. Each digested sample was then labeled by the Agilent random primers labeling kit for 2 hours using Cy5-dUTP for the patient DNA and Cy3-dUTP for the control DNA. Labeled products were column purified and prepared according to the Agilent protocol. After probe denaturation and preannealing with Cot-1 DNA, hybridization was performed at 65°C with rotation for 40 hours. After two washing steps, the arrays were analyzed with the Agilent scanner and the Feature Extraction software (v9.5.3.1; Agilent Technologies). Graphical overview was obtained using the CGH Analytics software (v3.4.40; Agilent Technologies).
Mutation nomenclature
All mutations are described according to the recommended nomenclature (http://www.genomic.unimelb.edu.au/mdi/mutnomen/). Nucleotide numbers, considering the A of the AUG start codon as number 1, are derived from cDNA LMX1B sequence (GeneBank accession no. NM_002316). The described mutations are defined by the same categories used in the Human Gene Mutation Database for the LMX1B gene (HGMD) (http://www.hgmd.cf.ac.uk).
RESULTS
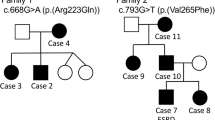
Twenty patients with a clinical diagnosis of NPS referred to our laboratory in the last 6 years have been examined. Most of the patients were Italian with the exception of two (NPS3 from Switzerland, NPS11 from Poland). Nine of them were sporadic cases, whereas 11 inherited the mutation from an affected parent. Patients NPS3 and NPS18 inherited the mutation from their unaffected fathers, for whom we are reporting evidence of somatic mosaicism.
This case series confirms variable clinical presentation, with cases showing a more common NPS phenotype and some more complex cases. Beyond the classical signs, a number of additional signs were observed: club feet in three cases; hypoacusia in one case; psychomotor delay in one case; macrocrania, left eye convergent strabismus, and fine hairs in one case; and frontal bossing and high hair line in one case. One case showed involvement of the central nervous system with cerebellar type tremor, mild cognitive deficit, diffuse periventricular white matter alteration observed by magnetic resonance imaging.
Patient NPS4, who carries a deletion that includes the entire LMX1B gene and other surrounding genes, showed a more complex phenotype. At physical examination, he showed triangular face, cloverleaf iris, low-set and prominent ears, thin lip, dorsal scoliosis, nail hypoplasia at the first and second right fingers and at the second left finger, elbow contractures, and small stature (height < third centile). He had psychomotor developmental delay and stereotypic movements. At birth, bilateral club feet were reported, which were treated with serial casting. Surgical intervention for recurvatum penis and right cryptorchidism was performed. Conduction defect and signs of right ventricular hypertrophy at electrocardiography were noticed; echocardiography was normal. Brain magnetic resonance imaging was normal.
Table 2 describes the molecular findings for the entire case series. LMX1B mutations were found in 16 patients of the 20 analyzed, and a deletion including the entire gene in one patient was found (85% of cases with LMX1B involvement). Most of the mutations had been already reported in the literature in association with NPS, whereas five of them have never been described so far.
A graphic representation of the LMX1B gene with all mutations detected in our case series is shown in Figure 1. Patient NPS1 carried a de novo duplication of 11 nucleotides in exon 4, which caused a frameshift and consequent introduction of a premature stop codon (Fig. 2).
Electropherogram of the mutation p.22fs (c.664_674 dupCGTCGAAGCCT) in patient NPS1. Upper panel: mutation c.664_674 dupCGTCGAAGCCT in patient NPS1. Mid panel: wild type allele, after separation by subcloning of the specific PCR product. Lower panel: allele with the 11 nucleotide duplication, after separation by subcloning of the specific PCR product. The circled nucleotide shows the synonymous rs13295990 polymorphism.
A single nucleotide deletion, c.488delC, affecting the following S164 codon, was found in both familial cases NPS12 and NPS13, for whom no apparent consanguinity was present (Fig. 3). This deletion caused a frameshift and the introduction of a premature stop codon. The mutation was inherited from the affected mother in patient NPS12 and from the affected father in patient NPS13.
Patient NPS4 resulted negative for mutations in the LMX1B coding sequence. However, the patient was homozygous for several SNPs included in the analyzed exons and adjacent intronic sequences, suggesting the possible presence of a deletion of the gene. The analysis of these SNPs in the patient's parents was not conclusive; therefore, it was extended to three clusters of SNPs located in introns 1, 3, and 6, respectively (Table 1). Only two of these SNPs, rs2235057 and rs3780332, were informative for our analysis showing a distorsion of allele segregation; indeed, only the maternal allele of the LMX1B gene was inherited by the patient (Fig. 4). After this indication, array-CGH analysis was performed, which detected a de novo 9q interstitial deletion of ∼2 Mb. The deletion extended between probe A_14_P111640 at 126.857.965 Mb (first deleted) and probe _14_P132586 at 129.081.374Mb (last deleted), flanked by probe A_14_P104324 at 126.820.885 Mb and probe A_14_P116197 at 129.122.002 Mb (both present) (according to UCSC Genome Browser, http://genome.ucsc.edu, March 2006) (Fig. 5). This region includes the entire LMX1B gene and 13 additional RefSeq genes. As assessed by SNPs segregation, the deletion occurred on the paternal allele and was not present in the patient's parents.
A, Array-CGH profile of the ∼2Mb 9q33.3-q34.11 deletion in patient NPS4. B, Enlargement of the 9q33.3-q34.11 region from the UCSC genome browser showing a comparison between the two deleted segments (patient NPS4 black bar; Patient 1 from Schlaubitz et al.,13 red bar), cytogenetics bands and RefSeq genes.
The phenotype of this patient was rather complex and, as described previously, the diagnosis of NPS was not straightforward because of the presence of additional findings associated with classic NPS clinical signs. The child showed moderate mental retardation and stereotypic movements.
Interestingly, and to our knowledge for the first time in the literature, we found the presence of somatic mosaicism in unaffected fathers in two cases, NPS3 and NPS18. Patient NPS3 was a 9-year-old girl born from healthy parents. Since birth she presented absent patellae and lateral instability of knee-joints and elbow contractures with limited range of motion. She had normal psychomotor development. Diagnosis of NPS was formulated on the basis of the patient's clinical features at the age of 9 years. Karyotype analysis revealed a duplication in chromosome 22 (47,XX,+inv dup [22] [pter-q11]), absent in the mother whereas the apparently healthy father was not analyzed. However, no signs of cat eye syndrome, usually associated with such chromosome defect, were observed. Moreover, no association between NPS typical signs and acrocentric chromosomes (including chr22) has been reported so far.
In this patient, the LMX1B mutation screening (Table 1) showed a substitution in exon 4, c.599G>A, resulting in arginine to glutamine amino acid change at position 200 in the homeodomain of the protein (p.R200Q). This mutation was already reported in the literature as being associated to the NPS phenotype.11 Interestingly, after direct sequencing of specific PCR products from the parents, the mutation was also detected in the healthy father as a low height A peak superimposed to wild-type G nucleotide (see electropherogram in Fig. 6). On the contrary, the two peaks were at equal height in the patient, as expected in a heterozygote, and no trace of the G allele was found in the mother. The analysis was repeated several times, and it always confirmed the same result. This persistent low-peaked A superimposing the G strongly suggested the presence of a somatic mosaicism in the father, referred as unaffected on a clinical basis.
A similar situation was found in patient NPS18, a 2-year-old girl presenting with hypoplastic nails suggestive of the diagnosis of NPS. An ultrasound of the knees could not confirm with certainty the presence of the growing ossifying centers of the patellae. At the molecular level, she was heterozygous for a c.592C>T substitution in LMX1B exon 4, leading to the change of arginine 198 with a premature stop (p.R198X) (Fig. 6). This variation, already reported in the literature, is one of the most frequently recurring mutations in NPS.12 Also, in this case, the hypothesis of mosaicism in the healthy father was raised by the presence of the C and T peaks at a significantly different height, confirmed after three repeated sequencing reactions (Fig. 6).
In both cases, to verify the presence of the mutated alleles in the two fathers, we subcloned the specific PCR products using TA Cloning Kit (Invitrogen), and, after transformation in Escherichia coli, we picked colonies for DNA sequencing, as shown in Figure 6. As expected in the hypothesis of mosaicism, the wild-type allele-bearing colonies were significantly more represented than colonies with the mutated ones. In the case of patient NPS18, the father was also heterozygous for a C/G SNP located in exon 4, allowing us to confirm the cosegregation with the mutated allele and his transmission to the patient. The simultaneous presence of the C>T substitution and the SNP G allele transmitted from the father was clearly evident in the sequence of the mutated clones derived from the mosaic father.
In the case of the patient NPS18, we have also analyzed DNA extracted from saliva and hair bulbs of her mosaic father. The mosaicism was present in the saliva with the presence of the C and T peaks at a significantly different height similar to what was found in the DNA extracted from blood but not in the hair (not shown). For patient NPS3, DNA sources other than blood were unavailable.
To further analyze the degree of mosaicism in the NPS18 patient's father, a Snapshot assay was performed by allele specific extension and subsequent evaluation of peak signals obtained after separation on an automated sequencer. The two alleles in the heterozygous NPS18 patient were quantified in three different reactions, and the mean percent calculated from the peak area was 60% for the wild type allele and 40% for the mutant allele. The assay on the mosaic father's samples showed 86% for the wild type allele (wt) and 14% for the mutant (mut) in blood DNA, 89% wt versus 11% mut in saliva DNA and 96% wt versus 4% mut in hair bulb DNA. Controls with wt sequence yielded 100% wt allele. Results are shown in Figure 7. Considering the 1.5% apparent lower signal from the mutant allele in the theoretically expected 50% for the two alleles in the heterozygous patient, the above data could be corrected accordingly, providing a quantitative test of the degree of mosaicism in different tissues. We remark that, by this technique, we could appreciate the low percent of mutant allele in the hair sample, which had appeared always negative in the sequencing tracks.
DISCUSSION
The LMX1B gene mutational analysis we describe here confirms and extends previous clinical and molecular spectra. The first confirmation was the high percent of clinically diagnosed cases who carry LMX1B mutations or deletions that include all or part of the LMX1B gene. However, in 15% of our cases no mutations or deletions in the analyzed regions were found. This percent is similar to what has been found in other case series. In the majority of cases, we identified point mutations and, similar to other series, they occurred mostly in the homeodomain though some point mutations appeared in the LIM A and LIM B domains.
Deletions of the entire LMX1B or part of it have been recently reported.9 Compared with these, the deletion found in our case (NPS4) involves a large region, which includes a number of different genes. Also recently, a 3.07 Mb was identified by array-CGH in a phenotypically female individual with 46,XY sex reversal and clinical features of NPS and genitopatellar syndrome.13 This deletion, on chromosome 9q33.3-34.11 encompasses several genes, including LMX1B and NAR5A1. Our NPS4 patient showed disturbance in language and social interactions, combined with stereotypic behavior. We have compared the deleted regions in our case and the other, recently identified, even wider one13 (Fig. 5), in relationship to the clinical phenotype.
In the previously published case with genital anomalies,13 genes included in that deletion, in particular NR5A1 (that cooperates with WT1 in its regulation of the expression of anti-Mullerian hormone in men) and NR6A1 (that has a restricted expression in testis), may be responsible for genital anomalies. Our patient showed genital anomalies (recurvatum penis and right cryptorchidism) less serious than those reported in the previously published case, and the deleted region did not include NR5A1 and NR6A1. It is possible that another gene, deleted in both our patient and the previous case, could contribute to the etiopathogenesis of genital anomalies. Both patients had club feet, signs of NPS, and mental retardation. Regarding cardiac anomalies, a conduction defect was reported in our patient, whereas in the previously described patient, a heart murmur was signaled at birth, which later resolved spontaneously. We do not know of any genes included in the deletion that could be responsible for cardiac involvement. Other described deletions9 are much smaller and do not contribute to the understanding of the above discussed phenotypic features.
NPS9, NPS15, and NPS16 familial cases were homozygous for several SNPs included in the analyzed exons and flanking intronic sequences, suggesting the possibility of an LMX1B deletion. These three cases familial cases were also analyzed by array-CGH analysis at ∼35 kb resolution, with negative results. In a previous report,10 we described other cases, different from these more recent ones, in whom no mutation in the LMX1B gene was found, which highlights that, in a number of cases, the molecular basis remains up to now unexplained. Small deletions, undetectable at the resolution used in our CGH analysis, or mutations in regulatory elements, might still account for an LMX1B associated defect. However, locus heterogeneity has not been reported so far.
Somatic mosaicism is known to occur in unaffected parents of patients affected by autosomal dominant disorders, having significant implication for genetic counseling. NPS is a dominantly inherited condition and children of an affected person have a 50% chance of receiving the mutated allele responsible for the disorder. This risk is considerably lower, estimated to be <1%, if the disease is sporadic and the mutation has occurred de novo during gametogenesis in one of the unaffected, noncarrier parents. In case of suspected or demonstrated somatic mosaicism in a healthy parent, although the recurrence risk of the disease increases in proportion with the percent of mosaicism, it is difficult, in practical terms, to make a precise prediction. This fact is mainly because of the impossibility of estimating the percent of mosaicism at germline level. The sequencing technique usually used, as was the case in our patients and their parents, has a limit of detection of somatic mosaicism depending on the percent of mutated cells, suggesting that more cases might occur and be examined by other more sensitive techniques such as the Snapshot method.
In summary, this article describes clinical and molecular characteristics of 20 NPS cases from whom we highlight, as interesting features: 1. the novel mutations in the LMX1B gene; 2. a deletion in chromosome 9q encompassing not only the entire LMX1B gene but also some additional genes, that could explain a complex clinical phenotype; 3. evidence of somatic mosaicism in apparently healthy parents of two NPS patients.
References
Little EM . Congenital absence or delayed development of the patella. Lancet 1897; 3865: 781–784.
McIntosh I, Dunston JA, Liu L, Hoover-Fong JE, Sweeney E . Nail patella syndrome revisited: 50 years after linkage. Ann Hum Genet 2005; 69( Pt 4): 349–363.
Bongers EM, Huysmans FT, Levtchenko E, et al. Genotype-phenotype studies in nail-patella syndrome show that LMX1B mutation location is involved in the risk of developing nephropathy. Eur J Hum Genet 2005; 13: 935–946.
Dunston JA, Reimschisel T, Ding YQ, et al. A neurological phenotype in nail patella syndrome (NPS) patients illuminated by studies of murine Lmx1b expression. Eur J Hum Genet 2005; 13: 330–335.
McIntosh I, Clough MV, Schäffer AA, et al. Fine mapping of the nail-patella syndrome locus at 9q34. Am J Hum Genet 1997; 60: 133–142.
Dai J-X, Johnson RL, Ding YQ . Manifold functions of the Nail-Patella Syndrome gene Lmx1b in vertebrate development. Dev Growth Differ 2009; 51: 241–250.
Chen H, Lun Y, Ovchinnikov D, et al. Limb and kidney defects in Lmx1b mutant mice suggest an involvement of LMX1B in human nail patella syndrome. Nat Genet 1998; 19: 51–55.
Bongers EM, Gubler MC, Knoers NV . Nail-patella syndrome. Overview on clinical and molecular findings. Pediatr Nephrol 2002; 17: 703–712.
Bongers EM, de Wijs IJ, Marcelis C, Hoefsloot LH, Knoers NV . Identification of entire LMXB gene deletions in nail patella syndrome: evidence for haploinsufficiency as the main pathogenic mechanism underlying dominant inheritance in man. Eur J Hum Genet 2008; 16: 1240–1244.
Seri M, Melchionda S, Dreyer S, et al. Identification of LMX1B gene point mutations in italian patients affected with Nail-Patella syndrome. Int J Mol Med 1999; 4: 285–290.
McIntosh I, Dreyer SD, Clough MV, et al. Mutation analysis of LMX1B gene in nail-patella syndrome patients. Am J Hum Genet 1998; 63: 1651–1658.
Dreyer SD, Zhou G, Baldini A, et al. Mutations in LMX1B cause abnormal skeletal patterning and renal dysplasia in nail patella syndrome. Nat Genet 1998; 19: 47–50.
Schlaubitz S, Yatsenko SA, Smith LD, et al. Ovotestes and XY sex reversal in a female with an interstitial 9q33.3-q34.1 deletion encompassing NR5A1 and LMX1B causing features of Genitopatellar syndrome. Am J Med Genet A 2007; 143: 1071–1081.
Vollrath D, Jaramillo-Babb VL, Clough MV, et al. Loss-of-function mutations in the LIM-homeodomain gene, LMX1B, in nail-patella syndrome. Hum Mol Genet 1998; 7: 1091–1098.
Szczałuba K, Obersztyn E, Kozłowski K, Ravazzolo R, Gołabek B, Mazurczak T . Clinical picture and molecular analysis in a familial case of Nail-Patella Syndrome–identification of a new mutation in LMX1B gene. Med Wieku Rozwoj 2005; 9: 195–203.
Dunston JA, Hamlington JD, Zaveri J, et al. The human LMX1B gene: transcription unit, promoter, and pathogenic mutations. Genomics 2004; 84: 565–576.
Acknowledgements
Supported by the Italian Ministry of Health, Strategic Program, RFPS-4-631972 “Genetic bases of Birth Defects.”
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Marini, M., Bocciardi, R., Gimelli, S. et al. A spectrum of LMX1B mutations in Nail-Patella syndrome: New point mutations, deletion, and evidence of mosaicism in unaffected parents. Genet Med 12, 431–439 (2010). https://doi.org/10.1097/GIM.0b013e3181e21afa
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181e21afa
Keywords
This article is cited by
-
Inherited glomerular diseases in the gilded age of genomic advancements
Pediatric Nephrology (2020)
-
A novel small deletion of LMX1B in a large Chinese family with nail-patella syndrome
BMC Medical Genetics (2019)
-
Nail-patella syndrome
Pflügers Archiv - European Journal of Physiology (2017)