Abstract
The objective of this study was to estimate mean blood pressure (BP), prevalence of hypertension (defined as BP ⩾140/90 mm Hg) and its awareness, treatment and control in the Vietnamese adult population. This cross-sectional survey took place in eight Vietnamese provinces and cities. Multi-stage stratified sampling was used to select 9832 participants from the general population aged 25 years and over. Trained observers obtained two or three BP measurements from each person, using an automatic sphygmomanometer. Information on socio-geographical factors and anti-hypertensive medications was obtained using a standard questionnaire. The overall prevalence of hypertension was 25.1%, 28.3% in men and 23.1% in women. Among hypertensives, 48.4% were aware of their elevated BP, 29.6% had treatment and 10.7% achieved targeted BP control (<140/90 mm Hg). Among hypertensive aware, 61.1% had treatment, and among hypertensive treated, 36.3% had well control. Hypertension increased with age in both men and women. The hypertension was significantly higher in urban than in rural areas (32.7 vs 17.3%, P<0.001). Hypertension is a major and increasing public health problem in Vietnam. Prevalence among adults is high, whereas the proportions of hypertensives aware, treated and controlled were unacceptably low. These results imply an urgent need to develop national strategies to improve prevention and control of hypertension in Vietnam.
Similar content being viewed by others
Introduction
Of 58 million deaths in the world during 2005, non-communicable diseases were estimated to account for 35 million, twice the deaths from all communicable diseases. Cardiovascular diseases (CVD) were responsible for 30% of all deaths (17.5 million).1 Hypertension is the disorder most commonly associated with cardiovascular disease worldwide, and is the most important modifiable risk factor for cardiovascular mortality.2 According to World Health Organization (WHO),1 each year at least 7.1 million people die as a result of hypertension. The WHO Global Burden of Disease estimates for 2004 showed hypertension as the leading risk factor for mortality (12.7% of deaths attributable), followed by tobacco use (8.7%) and high blood glucose (5.8%).3
Vietnam, as an emerging economy in Western-Pacific region, is facing a double burden of infectious and chronic disease. In the past 10–20 years, in transforming from a planned economy to market forces, the Vietnamese economy has grown rapidly. Changing dietary patterns and lifestyles accompanying economic growth may have affected the prevalence and incidence of atherosclerotic diseases, and hypertension, is becoming an important public health problem in Vietnam. It was the fifth leading cause of hospital deaths and the sixth leading cause of disease in hospitals in 1998,4 and moved up to the third leading cause of death and the sixth leading cause of disease in hospitals in 2002.5 Intra-cerebral haemorrhage, hypertension and heart failure were among the ten leading causes of morbidity and mortality in hospitals in 2002.5 In 2003, the Vietnam National Neurology Institute showed that over a third of cerebrovascular accidents (intra-cerebral haemorrhage, cerebrovascular infarction or transient ischaemic attack) in hospitals were significantly associated with high blood pressure (BP).6, 7 In 2005, 46% of patients with acute myocardial infarction treated at the Vietnam National Heart Institute were directly associated with hypertension.8
Vietnam has a generally weak community-based health information system, focusing on hospital databases. Thus, there is little information on hypertension in Vietnam. Population-based data of use to policy makers and health managers are therefore scarce. There was no strategy or model for prevention, early detection and management of high BP at the community level in Vietnam by the time this study concluded in 2008. Hypertensive patients received consultations, treatment and some monitoring in public general hospitals or private polyclinics. Public health prevention activities for cardiovascular risk factors are weak. Any national strategy for prevention and control of hypertension would face double barriers: inadequate population-based databases for better understanding of the condition and deficiencies in evidence for developing effective community-based intervention models. The objective of this paper is to characterise the prevalence and distribution of hypertension, together with awareness, treatment, and control in the general adult population (25 years and over) in Vietnam, with a view to provide a better evidence base for health planning.
Materials and methods
Sample design
Data for this study were obtained from population-based surveys on hypertension and its risk factors within the prevention and control of CVD Programme in Vietnam, collected between 2002 and 2008 by the Vietnam National Heart Institute. Multi-stage stratified sampling methods were used to select a nationally representative sample of the general population aged 25 years and over in Vietnam. Three provinces plus Hanoi city from northern Vietnam, and three provinces plus Ho Chi Minh city from southern Vietnam were selected at the first stage of sampling. Hanoi city and Ho Chi Minh city are the two major cities in Vietnam. They were intentionally included to enable a solely urban sample of subjects to be studied. Three selected provinces in each part of Vietnam were stratified by geographic areas (1) lowland areas: Thai Binh and Dong Thap provinces; (2) coastal areas: Nghe An and Khanh Hoa provinces; (3) highland areas: Thai Nguyen and Daklak provinces. At the second stage of sampling, three rural districts and one urban district were randomly selected from each selected province, and four districts each from Hanoi and Ho Chi Minh cities were randomly selected. Three communes were randomly selected from each selected district in the third stage of sampling. The final stage used a simple random sampling method to select individual participants from the list of all residents aged 25 years and over, both male and female. A total of 10 560 persons was randomly selected from 96 primary sampling units (communes) and invited to participate. Overall, 9823 persons (3853 men and 5970 women) completed the survey and examination. The general response rate was 93.0% (93.1% in men and 93.0% in women; and 93.0% in urban and 93.0% in rural areas). Blood samples were taken from a 1-in-5 sample of participants in Hanoi and Ho Chi Minh cities for laboratory analysis (fasting glucosaemia and lipidaemia profile).
Measurement
Data collection was conducted in local health stations in the participants’ areas of residence. The survey teams were medical doctors and nurses from local general district hospitals and from the Vietnam National Heart Institute. Two trained public health nurses performed anthropometry measurements. An interview and physical examination team of 10 doctors performed interviews and examinations using a standard questionnaire based on the WHO Stepwise approach (the surveillance of risk factors for non-communicable disease).9 Demographic data including age, gender, education, ethnicity and occupation were collected. The interview included questions related to personal and family medical histories of hypertension, smoking, alcohol consumption and salty dietary habits. Information on awareness and drug treatments for hypertension was also obtained. Body weight, height, waist circumference and BP were measured in two times. Anthropometric measurements were performed with the participants wearing light clothing and no footwear. Body weight was measured to the nearest 0.1 kg using a digital scale, and height recorded to the nearest 0.1 cm in the standing position using a portable stadiometer. Waist circumference was recorded to the nearest 0.1 cm, using a constant tension tape, directly over the skin, at the level of the midpoint between the inferior margin of the last rib and the iliac crest in the mid-axillary line. Body mass index was calculated as weight per height squared (kg m−2). Underweight, normal weight, overweight and obesity were defined as body mass index ranges of under 18, 18–23, 23–25 and over 25 kg m−2, respectively.10 Abdominal fat was defined as a waist circumference over 80 cm in women and over 90 cm in men.10 The concentrations of glucose, cholesterol, triglyceride, low-density lipoproteins and high-density lipoproteins were determined from blood samples.
All study investigators and staff members successfully completed a training programme that oriented them both to the aims of the study and to the specific tools and methodologies employed. At the training sessions, interviewers were given detailed instructions on administering the study questionnaire. All those recording BP, participated in a special training session on the use of a standardized protocol for measurement. Satisfactory performance during a written test on knowledge for preparing study participants for measuring BP, selecting a correct cuff size (small, medium or large) and using standard techniques for measurement was required.
BP measurements used a common protocol adapted from procedures recommended by WHO Stepwise approach (the Surveillance of risk factors for non-communicable disease)9 and the Vietnam National Cardiology Association.11 Automatic sphygmomanometers (OMRON, model SEM-2, Healthcare Inc., Bannockburn, IL, USA) with appropriately sized cuffs were used. BP was measured twice, 1 min apart, with participants in a sitting position after 5 min of rest, in one visit. A third measurement was performed if the difference between the first two was over 10 mm Hg for systolic or diastolic BP. The average of the second and the third BP measurements was used for analyses. In addition, participants were advised to avoid alcohol, cigarette smoking, coffee/tea and exercise for at least 30 min before their BP measurement.
The distribution of BP levels based on categories established in the Sixth Report of the Joint National Committee on detection, evaluation, and treatment of high blood pressure;12 1999 WHO-International Society of Hypertension Guidelines for the management of hypertension13 and Vietnam National Cardiology Association's guidelines11 for prevention, detection, diagnosis and treatment of hypertension are presented. These include six BP levels: optimal, normal, high normal, hypertensive grade 1, hypertensive grade 2 and hypertensive grade 3. Hypertension was defined as an average systolic BP (SBP) ⩾140 mm Hg and/or average diastolic BP (DBP) ⩾90 mm Hg, and/or self-reported previous diagnosis of hypertension by a health professional staff and/or self-reported current treatment for hypertension with antihypertensive medications in the previous 2 weeks. Awareness of hypertension was defined as self-report of any prior diagnosis of hypertension by a health care professional among the population defined as having hypertension. Treatment of hypertension was defined as use of a prescription medication for management of their high BP at the time of the interview. Prevalence estimates of treatment among aware hypertensives and among all hypertensives are presented. Control of hypertension was defined as pharmacological treatment of hypertension associated with an average SBP <140 mm Hg and an average DBP <90 mm Hg. Prevalence estimates of control among treated hypertensives and among all hypertensives are presented.
Occupational status (main job of the participants) was classified into three groups: (1) experts and government staff (currently working in a state-run office or having retired from government work), (2) manual workers (farmers, building workers, unskilled workers and so on or having retired from those jobs because of old age) and (3) other jobs (housewives, small traders, housekeepers, handicraft makers and the jobless, and so on). Educational attainment was determined by years of schooling and level of graduates. For the purpose of this analysis, each subject was classified into one of three categories: (1) low level or less than primary school education level included people who were no more than graduates of primary school (<6 years of education); (2) medium level or primary and secondary educational level included attendees or graduates of primary and secondary school (⩾6 years but ⩽9 years of education); (3) high level or higher educational level included high school and university attendees or graduates (>9 years of education). Type of residence was determined according to the classification of regions and areas in Vietnam by the Vietnamese Government.
The prevention and control of CVD programme is a part of National Programme for Prevention and Control of Non-Communicable Diseases from the Vietnam Ministry of Health. The ethics committees and other relevant regulatory bodies in Vietnam approved this study. All participants were informing both the aims of the study and the personal interests and responsibilities. Informed consent was obtained from each participant before data collection. During the survey, the participants with untreated diseases or conditions identified during the examination were referred to their usual primary health care provider in local health stations.
Statistical analysis
The national survey of hypertension and its risk factors was designed to provide precise estimates of prevalence and mean levels of BP by age groups, gender, area of residence (urban vs rural) and region (lowland vs coastal, highland and city) among the adult population aged 25 years and over in Vietnam. The prevalences and mean levels of BP were weighted to represent the total Vietnamese adult population aged 25 years and over. For the analysis, study subjects were classified by gender, age, residence, education, occupation, any evidence of hypertension as previously defined, awareness of their condition, pharmaceutical therapy for it and effectiveness of treatment. Subsequently, odds ratios contrasting the indicated groups (those with hypertension vs normotension; among hypertensives, those with awareness of hypertension vs unawareness; among those aware, those treated vs untreated; among those treated, those effectively controlled vs uncontrolled) by gender, age, type of residence, educational level, occupation, marital status, family history of hypertension, regions, body mass index range and abdominal fat were estimated by modelling the data using multiple logistic regression in Stata 10 (Stata Corporation, College Station, TX, USA).
Results
Sample characteristics
Characteristics of the sample are summarised in Table 1. The sample comprised 9823 participants with 26.2, 24.6, 24.8 and 24.4% from lowland, coastal, highland areas and cities, respectively. A total of 50.8% were from urban areas and the remaining 49.2% from rural areas. The mean age was 42.7 (standard deviation 11.0 years) and ranged from 25 to 100 years. Almost all participants were married (81.7%), most had primary or secondary school education (49.8%) and the most common occupation was manual work (64.5%). Approximately one fifth of men and women reported family histories of hypertension. The overall weighted prevalence of overweight was 11.8%, and 9.2% of the participants were obese. Abdominal fat was observed in 19.7% women and 3.9% of men (a significant difference, P<0.001).
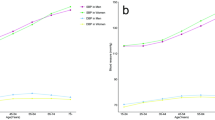
Mean BP values
The gender- and age-specific mean BP levels for the total sample and for three subgroups defined by hypertension status are shown in Table 2. Overall, the mean (± standard deviation) SBP was 121.0±19.1 mm Hg and the mean DBP was 75.8±11.5 mm Hg. Systolic and DBP increased progressively with age in males and females. Mean BP was slightly higher in males across all age groups. The mean SBP and DBP for normotensive participants were 34.6 and 14.8 mm Hg lower than the corresponding figures for those with treated hypertension, and 37.3 and 19.8 mm Hg lower than the corresponding figures for those with untreated hypertension. In contrast, individuals under anti-hypertensive treatment only showed SBP 2.7 mm Hg and DBP 5.0 mm Hg lower than corresponding values among individuals without anti-hypertensive treatment.
Distribution of BP
In Table 3, the percentages of BP levels by gender and age groups are given according to the international classification system outlined above. Overall, 57.3% of men and 68.8% of women had optimal and normal BP, whereas the prevalence of high normal BP was 16.6% in men and 11.8% in women. The prevalence of stage 1, 2 and 3 hypertension was 16.6, 5.9 and 3.7% in men and 11.7, 5.1 and 2.6% in women, respectively, and significantly increased with age for participants of both sexes.
Prevalence of hypertension
The prevalence of hypertension according to gender, age groups, geographical regions and socio-physical determinants is presented in Table 4. The overall prevalence of hypertension in Vietnamese adults was 25.1%, slightly higher in men than in women (28.3 vs 23.1%, P<0.001). Hypertension prevalence progressively increased with age in both sexes, and was higher among men in age groups up to 64 years than among women. However, women aged 65 and over had higher prevalences than men (58.2 vs 53.4%; and 70.5 vs 68.8%, respectively). In term of socio-geographical factors, the highest hypertension prevalence was seen in men living in cities (37.8%) and the lowest in women living in highland areas (17.1%). Hypertension prevalence was significantly higher in urban areas than in rural areas (32.7 vs 17.3%, P<0.001).
Factors associated with hypertension prevalence
After adjustment for age, sex, geographical region (lowland/other regions and urban/rural) and other factors, the odds for hypertension increased with age and were statistically higher in all age groups compared with the 25–34 age group (Table 5). Multivariable logistic models were constructed to further analyse the association of hypertension and socio-geographical factors separately among men and women. As shown in Table 5, age; having family histories of hypertension, living in urban areas, being underweight, overweight, obesity and having abdominal fat were significantly associated with hypertension for both men and women.
Awareness, treatment and control of hypertension
Table 4 shows proportions of participants with hypertension who were aware of their hypertensive condition, who were being treated with anti-hypertensive drugs, and who were both treated and controlled. Among 2467 hypertensive individuals, 48.4% (1194 cases, 434 men (39.8%) and 760 women (55.2%)) were aware of their hypertensive status, only 29.6% (730 cases, 236 men (21.7%) and 494 women (35.9%)) were taking a treatment to lower their BP, and only 10.7% (265 cases, 66 men (6.1%) and 199 women (14.5%)) achieved targeted BP control (<140/90 mm Hg). These data are summarised in Figure 1, together with estimates extrapolated to the Vietnamese population. There were 1273 cases (51.6%) newly diagnosed (previously unaware) of their hypertension. More than one third (36.3%) of hypertensives that were being treated, successfully controlled their BP. More than half of women were aware of their hypertension, higher than the corresponding value in men (55.2 vs 39.8%, P<0.001). The prevalences of treatment and control were higher in women than in men (35.9 vs 21.7%, P<0.001 and 14.5 vs 6.1%, P<0.001, respectively). As shown in Table 6, the odds for hypertension awareness were higher among people at least 45-years-old, who had family histories of hypertension, lived in urban areas, and who were underweight or overweight or obese. In contrast, men were less likely to be aware of their elevated BP. In all hypertensives that were aware of their high BP, the odds for hypertension treatment were higher among people who had low educational levels, family histories of hypertension or lived in urban areas.
Prevalence of hypertension, with proportions aware, treated and controlled, among a national sample survey of 9832 Vietnamese adults aged 25 years and over, with extrapolations to the general population (in 2009)51 (44 million aged 25 years and over).
Discussion
This study gives an important overview of hypertension in Vietnam, on the basis of a national sample. We found that one quarter of Vietnamese adults aged 25 years or over, amounting to approximately 11 million people, were hypertensive. Despite high levels of hypertension, there were relatively low levels of awareness, treatment and control.
These results show higher prevalences than in previous studies (11.2% in 1992,14 16.3% in 2001,15 16.9% among subjects aged 24–64 years in 2002,16 14.1% in a rural community of Vietnam in 2002,17 and 18.3% in 2005.18 These findings indicate an increasing problem.
When comparing the prevalences of hypertension from this data with those from other studies, other factors that might contribute to any observed differences should be taken into consideration, such as differences in age structure between studied participants, geographical characteristics of the population, time of the study and standardisation of BP measurement instruments and procedures and so on Internationally, our findings are more similar to those from developed rather than developing countries.19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32
Other international investigations have studied factors associated with prevalence, awareness, treatment and control of hypertension.21, 22, 23, 28, 29, 30, 31, 33, 34, 35 Our results are consistent with several previous reports. The figure of awareness, treatment and control was lower than the average in high-income countries and similar to corresponding figures for low- and middle-income countries.20 An important key predictor of hypertension in many populations is age,36 as we also found. Prevalence of hypertension was more common in men, but awareness, treatment and control were higher in women. These findings were contrary to the studies in India in 199537 and in Greece in 2004,33 which showed that the prevalence of hypertension was as high among women as in men. Relationships between hypertension and educational level have been found in higher-income countries such as Canada, Netherlands, Sweden and United States of America38 as well as in low- and middle-income countries such as China,30 India,25 Iran39 and Mozambique.40
Having a family history of hypertension is a well-known risk factor for hypertension as we also found in this study, and it was also associated with greater awareness. The SUNSET study34 and one other study in rural China showed that family history of hypertension was significantly associated with awareness, treatment and control of hypertension.41
Hypertension prevalence among urban residents in this study was nearly twice that of those in rural areas. Similarly, cities and lowland regions had higher hypertension prevalences than coastal and highland regions. In Vietnam, lowland regions with provincial centres have experienced rapid industrialisation and modernisation in recent decades, leading to lifestyle changes towards western habits such as high-fat diets, smoking, alcohol consumption and work-related stress. These lifestyle changes may contribute to the development of high BP.
Our findings must be considered within the context of the investigation's limitations. Prevalence of hypertension may have been overestimated42 and the control of elevated BP condition underestimated42, because BP was measured only during a single visit. According to both WHO9, 13 and Vietnam National Association of Cardiology guidelines,11 hypertension should be defined based on the average of at least two or more BP readings taken at two or more visits after an initial screening. However, this should have minimal effects on within-sample comparisons and it is an inherent problem of large epidemiological investigations.43
Important strengths of the present study are the large sample study, its nationwide scope and its general population coverage. As such, the results of the current study can be extrapolated to the general population. Our study is considerably larger than previous studies in Vietnam that have targeted population groups in specific provinces or geographical areas. In addition, the advantages of the current investigation include use of a standard protocol with strong quality control procedures for measurement of BP and collection of a wide array of socio-geographical characteristics, which permitted to have a comprehensive analysis of factors associated with prevalence, awareness, treatment and control of hypertension in the general population in Vietnam.
The high prevalence of hypertension coupled with unacceptably low proportions of awareness, treatment and control has extremely important implications for public health staff, physicians, health care providers and health policy decision makers in Vietnam, particularly for initiatives such as the National Programme for Prevention and Control of Non-communicable Diseases, the National Targeted Programme for Prevention and Control of CVD. The high prevalence of hypertension in Vietnam mandates both a population-based strategy, to prevent this status and reduce mean BP, and a clinical strategy, to treat and manage those people with established hypertension or its complications such as stroke, myocardial infarction and heart failure. Such efforts include using the mass media to educate the general population, educating children and students, and providing leadership from social and professional organisations to promote healthy lifestyles. Traditionally, public health staff have focused their attention almost entirely on infectious and parasitic diseases, immunisation and vaccination programmes and on maternal and child health. The early detection and treatment of hypertension, especially salt reduction and tobacco control44 as well as other cardiovascular risk factors, must become a central focus of their health promotion and prevention efforts. It is not clear that pharmacotherapy is the most effective strategy for all, particularly at younger ages. However, wider use of cost-effective medications (low-price diuretics, low-price calcium-channel blockers, beta-blockers, aspirin and so on)45 has an important role. Scaling up the coverage of evidence-based interventions above current levels using a multi-drug regime limited to individuals accessing health services, is the only cost-effective clinical intervention that has been shown to be cost-effective in low- and middle-income countries. Treatment with off patent drugs of such individuals at high absolute risk of a CVD event (15% risk over 10 years) and based on the presence of easily measured risk factors (including, but not only, BP), has the potential to prevent 266 000 deaths in Vietnam over 10 years at a cost of 0.66 USD per person per year.46, 47 Voluntary salt reduction, combined with tobacco control, if widely applied could prevent a further 248 000 deaths in Vietnam over 10 years at a cost of 0.16 USD per person per year.44
Finally, health policy makers must be alerted to the clinical, public health and economic consequences of hypertension, as well as the risk factors associated with the emerging epidemic of cardiovascular disease in Vietnam, as a basis for developing policies and ensuring appropriate allocation of resources. Our extrapolations revealed an estimated 9.8 million Vietnamese aged 25 and over at a health disadvantage associated with elevated BP, including 5.7 million hypertensives unaware of their high BP status, 2.1 million people aware but untreated and 2.0 million treated but not controlled (Figure 1). Successfully changing this situation will require comprehensive public health actions, which combine preventions and interventions at the population and individual levels.1, 47 Like other low- and middle-income countries, Vietnam is facing a double burden of disease (communicable and non-communicable) and financial challenges. Successfully tackling the massive burden of disease associated with hypertension will be financially, logistically and organisationally challenging. However, given the future impact of hypertension on the health of the economically active adult population in a rapidly emerging economy, the country cannot afford to neglect this issue. Vietnam can benefit from the experiences of other countries1, 2, 44, 46, 48, 49, 50 that have designed and implemented successful programs leading to a reduction in hypertension as well as other cardiovascular risk factors. Further work is needed to guide strategies for preventing and managing hypertension in Vietnam in cost-effective and scientific ways for a low- and middle-income country, with rapid epidemiological and health transitions.
In conclusion, the national survey on hypertension and its risk factors indicated that hypertension is a major and increasing public health problem in Vietnam. Effective national targeted programs to improve the prevention, early detection and comprehensive treatment of hypertension and other cardiovascular risk factors are urgently needed in Vietnam.

References
World-Health-Organization. World Health Organization Global Report: Preventing Chronic Diseases—A Vital Investment. World Health Organization: Geneva, 2005.
World-Health-Organization. Report of World Health Organization Expert Commitee. Hypertension Control: Geneva, 1996.
World-Health-Organization. Global Health Risks Summary Tables. Health Statistics and Informatics Department. World Health Organization: Geneva, Switzerland, 2009 ( http://www.who.int/evidence/bod).
Ministry-of-Health-of-Vietnam. Vietnam Health Statistics Yearbook 1998. Vietnam Ministry of Health: Hanoi, 1999.
Ministry-of-Health-of-Vietnam. Vietnam Health Statistics Yearbook 2002. Vietnam Ministry of Health: Hanoi, 2003.
Vietnam-National-Neurology-Institute. Preparatory Document for the VIIth National Congress: Situation of Nerology Diseases. Vietnam Ministry of Health: Hanoi, 1996.
Ministry-of-Health-of-Vietnam. Vietnam Health Statistics Yearbook 2003. Vietnam Ministry of Health: Hanoi, 2004.
Ministry-of-Health-of-Vietnam. Vietnam Health Statistics Yearbook 2005. Vietnam Ministry of Health: Hanoi, 2006.
Bonita R, De Counter MDT, Jamrozi K, Winkelmann R . Surveillance of Risk Factors for Non-Communicable Disease: The WHO STEPwise Approach. World Health Organization: Geneva, 2001 ( http://www.who.int/chp/steps).
World-Health-Organization/International-Association-for-the-Study-of-Obesity/International-Obesity-TaskForce. The Asia-Pacific Perspective: Redefining Obesity and its Treatment. Health Communications Australia: Melbourne, 2000. (ISBN 0-9577082-1-1).
Vietnam-Association-of-Cardiology. Guidelines for Prevention, Detection, Diagnosis and Treatment of Hypertension in Vietnam. Medical Publisher: Hanoi, 2008.
The sixth Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med 1997; 157 (21): 2413–2446.
1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens 1999; 17 (2): 151–183.
Vietnam-National-Heart-Institue. Survey on Hypertension in Vietnamese Adult Population. Vietnam National Heart Institute: Hanoi, 1992.
Vietnam-National-Heart-Institue. Epidemiologycal Survey of Hypertension and its Risk Factors Including Diatetes Mellitus in Northern Vietnam. Vietnam National Heart Institute: Hanoi, 2001.
Ministry-of-Health-of-Vietnam. Vietnam National Health Survey 2001-2002. Vietnam Ministry of Health: Hanoi, 2003.
Minh HV, Byass P, Chuc NT, Wall S . Gender differences in prevalence and socioeconomic determinants of hypertension: findings from the WHO STEPs survey in a rural community of Vietnam. J Hum Hypertens 2006; 20 (2): 109–115.
Van Minh H, Soonthornthada K, Ng N, Juvekar S, Razzaque A, Ashraf A et al. Blood pressure in adult rural INDEPTH population in Asia. Glob Health Action 2009; 2.
Kearney PM, Whelton M, Reynolds K, Whelton PK, He J . Worldwide prevalence of hypertension: a systematic review. J Hypertens 2004; 22 (1): 11–19.
Pereira M, Lunet N, Azevedo A, Barros H . Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens 2009; 27 (5): 963–975.
Ong KL, Cheung BM, Man YB, Lau CP, Lam KS . Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension 2007; 49 (1): 69–75.
Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension 2004; 43 (1): 10–17.
Banegas JR, Rodriguez-Artalejo F, de la Cruz Troca JJ, Guallar-Castillon P, del Rey Calero J . Blood pressure in Spain: distribution, awareness, control, and benefits of a reduction in average pressure. Hypertension 1998; 32 (6): 998–1002.
Ordunez-Garcia PO, Espinosa-Brito AD, Cooper RS, Kaufman JS, Nieto FJ . Hypertension in Cuba: evidence of a narrow black-white difference. J Hum Hypertens 1998; 12 (2): 111–116.
Gupta PC, Gupta R, Pednekar MS . Hypertension prevalence and blood pressure trends in 88 653 subjects in Mumbai, India. J Hum Hypertens 2004; 18 (12): 907–910.
Ibrahim MM, Rizk H, Appel LJ, el Aroussy W, Helmy S, Sharaf Y et al. Hypertension prevalence, awareness, treatment, and control in Egypt. Results from the Egyptian National Hypertension Project (NHP). NHP Investigative Team. Hypertension 1995; 26 (6 Part 1): 886–890.
Steyn K, Gaziano TA, Bradshaw D, Laubscher R, Fourie J . Hypertension in South African adults: results from the Demographic and Health Survey, 1998. J Hypertens 2001; 19 (10): 1717–1725.
Kamadjeu RM, Edwards R, Atanga JS, Unwin N, Kiawi EC, Mbanya JC . Prevalence, awareness and management of hypertension in Cameroon: findings of the 2003 Cameroon Burden of Diabetes Baseline Survey. J Hum Hypertens 2006; 20 (1): 91–92.
Edwards R, Unwin N, Mugusi F, Whiting D, Rashid S, Kissima J et al. Hypertension prevalence and care in an urban and rural area of Tanzania. J Hypertens 2000; 18 (2): 145–152.
Muntner P, Gu D, Wu X, Duan X, Wenqi G, Whelton PK et al. Factors associated with hypertension awareness, treatment, and control in a representative sample of the chinese population. Hypertension 2004; 43 (3): 578–585.
Chongsuvivatwong V, Yipintsoi T, Suriyawongpaisal P, Cheepudomwit S, Aekplakorn W, Faramnuayphol P et al. Comparison of cardiovascular risk factors in five regions of Thailand: InterASIA data. J Med Assoc Thai 2010; 93 (1): 17–26.
Cutter J, Tan BY, Chew SK . Levels of cardiovascular disease risk factors in Singapore following a national intervention programme. Bull World Health Organ 2001; 79 (10): 908–915.
Psaltopoulou T, Orfanos P, Naska A, Lenas D, Trichopoulos D, Trichopoulou A . Prevalence, awareness, treatment and control of hypertension in a general population sample of 26 913 adults in the Greek EPIC study. Int J Epidemiol 2004; 33 (6): 1345–1352.
Agyemang C, van Valkengoed I, Koopmans R, Stronks K . Factors associated with hypertension awareness, treatment and control among ethnic groups in Amsterdam, the Netherlands: the SUNSET study. J Hum Hypertens 2006; 20 (11): 874–881.
Degli Esposti E, Di Martino M, Sturani A, Russo P, Dradi C, Falcinelli S et al. Risk factors for uncontrolled hypertension in Italy. J Hum Hypertens 2004; 18 (3): 207–213.
Whelton PK . Epidemiology of hypertension. Lancet 1994; 344 (8915): 101–106.
Malhotra P, Kumari S, Kumar R, Jain S, Sharma BK . Prevalence and determinants of hypertension in an un-industrialised rural population of North India. J Hum Hypertens 1999; 13 (7): 467–472.
Colhoun HM, Hemingway H, Poulter NR . Socio-economic status and blood pressure: an overview analysis. J Hum Hypertens 1998; 12 (2): 91–110.
Esteghamati A, Abbasi M, Alikhani S, Gouya MM, Delavari A, Shishehbor MH et al. Prevalence, awareness, treatment, and risk factors associated with hypertension in the Iranian population: the national survey of risk factors for noncommunicable diseases of Iran. Am J Hypertens 2008; 21 (6): 620–626.
Damasceno A, Azevedo A, Silva-Matos C, Prista A, Diogo D, Lunet N . Hypertension prevalence, awareness, treatment, and control in Mozambique: urban/rural gap during epidemiological transition. Hypertension 2009; 54 (1): 77–83.
Dong G, Sun Z, Zheng L, Li J, Zhang X, Xu C et al. Factors associated with hypertension awareness, treatment and control in rural Chinese. J Hum Hypertens 2008; 22 (5): 366–369.
Bovet P, Gervasoni JP, Ross AG, Mkamba M, Mtasiwa DM, Lengeler C et al. Assessing the prevalence of hypertension in populations: are we doing it right? J Hypertens 2003; 21 (3): 509–517.
Klungel OH, de Boer A, Paes AH, Nagelkerke NJ, Seidell JC, Bakker A . Estimating the prevalence of hypertension corrected for the effect of within-person variability in blood pressure. J Clin Epidemiol 2000; 53 (11): 1158–1163.
Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R . Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet 2007; 370 (9604): 2044–2053.
Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation 2002; 106 (3): 388–391.
Lim SS, Gaziano TA, Gakidou E, Reddy KS, Farzadfar F, Lozano R et al. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet 2007; 370 (9604): 2054–2062.
Van Minh H, Lan Huong D, Bao Giang K, Byass P . Economic aspects of chronic diseases in Vietnam. Glob Health Action 2009; 2.
Tian HG, Guo ZY, Hu G, Yu SJ, Sun W, Pietinen P et al. Changes in sodium intake and blood pressure in a community-based intervention project in China. J Hum Hypertens 1995; 9 (12): 959–968.
Nissinen A, Berrios X, Puska P . Community-based noncommunicable disease interventions: lessons from developed countries for developing ones. Bull World Health Organ 2001; 79 (10): 963–970.
Isaakidis P, Raguenaud ME, Say C, De Clerck H, Khim C, Pottier R et al. Treatment of hypertension in rural Cambodia: results from a 6-year programme. J Hum Hypertens 2011; 25 (4): 241–249.
General-Statistics-Office-of-Vietnam. The 2009 Vietnam Population and Housing Census: Major Findings. General Statistics Office of Vietnam: Hanoi, 2010 (http://www.gso.gov.vn/default_en.aspx?tabid=515&idmid=5&ItemID=9813).
Acknowledgements
Technical and financial support for this study was made available by the Vietnamese Ministry of Health and the World Health Organization (WHO) Western Pacific Region. We would like to thank Professor Leigh Blizzard, a WHO expert, Menzies Research Institute, University of Tasmania, Hobart, Australia for his valuable and helpful insights in the design of this study. The survey participants, principal staff, the host institutions and all those involved in the survey data collection at eight provinces in this study are greatly acknowledged. We would specifically like to recognise the contributions of the following staff:
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Vietnam National Heart Institute: Do Doan Loi, Do Quoc Hung, Nguyen Thi Bach Yen, Pham Thi Tuyet Nga, Nguyen Thi Thu Hoai, Nguyen Quoc Thai, Khong Nam Huong, Pham Tran Linh, Nguyen Cong Ha, Tran Thi An, Do Kim Bang, Nguyen Minh Hung, Do Phuong Anh, Dao Ngoc Thuy, Pham Nhu Hung, Hoang Van, Tran Hai Yen, Le Thanh Binh, Do Thuy Can, Nguyen Xuan Tu, Nguyen Thi Hai Yen.
National Hospital of Endocrinology: Ta Van Binh, Pham Thi Lan, Nguyen Hong Loan, Ho Khai Hoan, Nguyen Thu Hien, Le Thi Viet Ha, Ha Quang Thanh.
Vienam-Poland General Hospital, Nghe An: Pham Hong Phuong.
Thai Binh Service of Health, Thai Binh: Le Xuan Dieu.
Khanh Hoa Service of Health, Khanh Hoa: Tran Van Minh.
Daklak Service of Health, Daklak: Nay Nguyen, Tran Van Tiet.
Nguyen Trai General Hospital, Ho Chi Minh city: Pham Thi Nga.
Dong Thap Service of Health, Dong Thap province: Nguyen Van Thuyen.
This study was supported from the Umeå Centre for Global Health Research, funded from FAS, the Swedish Council for Working Life and Social Research (grant no. 2006-1512) and through the SIDA Health Systems Research Programme is appreciated.
Rights and permissions
About this article
Cite this article
Son, P., Quang, N., Viet, N. et al. Prevalence, awareness, treatment and control of hypertension in Vietnam—results from a national survey. J Hum Hypertens 26, 268–280 (2012). https://doi.org/10.1038/jhh.2011.18
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2011.18
Keywords
This article is cited by
-
Management of Hypertension in the Asia-Pacific Region: A Structured Review
American Journal of Cardiovascular Drugs (2024)
-
Uncontrolled blood pressure and associated factors in adult hypertensive patients undergoing follow-up at public health facility ambulatory clinics in Bishoftu town, Ethiopia: a multi-center study
BMC Cardiovascular Disorders (2023)
-
Assessment of availability, readiness, and challenges for scaling-up hypertension management services at primary healthcare facilities, Central Highland region, Vietnam, 2020
BMC Primary Care (2023)
-
Prevalence, awareness, and control of hypertension and associated factors among Royal Thai Army personnel in Thailand from 2017 to 2021
Scientific Reports (2023)
-
Prevalence of undetected hypertension and its association with socio-demographic and non-communicable diseases risk factors in Brunei Darussalam
Journal of Public Health (2023)