Abstract
Although it has long been known that the myeloproliferative neoplasms (MPN) polycythemia vera (PV), essential thrombocythemia (ET) and primary myelofibrosis (PMF) are clonal hematopoietic stem-cell disorders, for many years the genetic basis for these disorders was elusive. A new era in MPN biology began in 2005 with the discovery of a somatic point mutation in JAK2 tyrosine kinase (JAK2V617F), which was identified in a significant proportion of patients with PV, ET and PMF. Based on the hypothesis that JAK-STAT signaling is central to the pathogenesis of JAK2V617F-negative MPN, genomic studies have identified JAK2 exon 12 mutations in JAK2V617F-negative PV and activating mutations in MPL in patients with JAK2V617F-negative ET and PMF. In this review, we will discuss the role of these mutant alleles in the pathogenesis of PV, ET and PMF, the potential therapeutic implications of these discoveries, and the implications of these discoveries for genomic studies of hematopoietic malignancies.
Similar content being viewed by others
Introduction
The myeloproliferative neoplasms (MPN) were first described in a landmark editorial in 1951 by William Dameshek (1900–1969), an American hematologist.1 Dameshek recognized that the different MPN are characterized by pan-myeloid proliferation, which he suggested might result from an ‘undiscovered stimulus’. In subsequent years, the disorders classified as MPN have evolved to include chronic myeloid leukemia (CML), polycythemia vera (PV), essential thrombocythemia (ET), primary myelofibrosis (PMF), chronic eosinophilic leukemia (CEL), chronic myelomonocytic leukemia, and systemic mastocytosis.2 In the past half century, a series of seminal cytogenetic and molecular biologic studies led to the identification of disease-causing mutations in other MPNs, including BCR-ABL in CML,3 FIP1L1-PDGFRA in CEL,4 and PDGFRA/B translocations in chronic myelomonocytic leukemia,5 each of which has had diagnostic, biologic and therapeutic relevance for these disorders.
In contrast, our understanding of the molecular pathogenesis of PV, ET, and PMF was largely limited to the work of Fialkow, Adamson, and Axelrad and other investigators in the 1970s. Following up on Fialkow's earlier work demonstrating that CML is a clonal hematopoietic stem-cell disorder,6 Adamson and Fialkow identified a single G6PD isoform in PV red blood cells, granulocytes, and platelets, consistent with clonal multilineage expansion.7 Subsequent studies extended these findings to ET and PMF,8, 9 providing evidence that these disorders arise in a multipotent hematopoietic progenitor. At about the same time Jaroslav Prchal and Arthur Axelrad10 demonstrated that erythroid colonies could be grown from PV bone marrow cells, but not from normal cells, in the absence of erythropoietin; this has been termed endogenous erythroid colony formation, and can be demonstrated in some, but not all, patients with ET and PMF.10, 11 In subsequent years, our understanding of the molecular basis of PV, ET and PMF remained unchanged, with the notable exception of two papers in 1998; when Silva et al.12 noted overexpression of BCL-XL in PV erythroid progenitors, and Moliterno et al.13 noted downmodulation of thrombopoietin receptor expression on PV platelets.
Discovery of JAK2V617F: four different stories
The year 2005 was a watershed in our understanding of the molecular pathogenesis of PV, ET, and PMF with the identification of the JAK2V617F allele in a significant proportion of patients with PV, ET and PMF.14, 15, 16, 17 It is interesting to note that the different groups used disparate approaches to arrive at the same discovery, and these approaches are of value in considering current and future efforts in cancer gene discovery. The group led by William Vainchenker began by developing a liquid culture system to culture PV erythroid cells in the absence of exogenous cytokines;18 this important technical advancement allowed them to use small molecule inhibitors to interrogate the requirement for specific signaling pathways in PV erythroid cell proliferation. They first noted that small molecule inhibition of JAK2 inhibited PV erythroid proliferation, and then subsequently used siRNA to show that JAK2 expression was required for erythroid expansion in the absence of cytokines; this led them to sequence JAK2 in PV patient samples.15 This approach represents an important example of how functional genomics can be used to evaluate the role of specific genes and pathways in oncogenic transformation, and as small molecule and siRNA libraries continue to improve in size and in ease of use, these approaches will facilitate investigation into the pathogenesis of human malignancies on a much larger scale. Moreover, these approaches will complement the high-throughput genomic studies being used to discover cancer-associated mutations, and allow dissection of which mutations represent ‘drivers’ in oncogenesis and which are ‘passengers’ acquired by the transformed clone during clonal selection but with no relevance to tumorigenesis.19, 20
Robert Kralovics and Radek Skoda began their efforts by following up on the important discovery by Josef Prchal and Kralovics21 that loss of heterozygosity of chromosome 9p24 is a relatively common event in PV. In this important study, Prchal and coworkers showed that unlike most tumor suppressors, where LOH is commonly the result of deletion of the remaining wild-type copy of the gene, LOH at this locus in PV is the result of acquired uniparental disomy (UPD), such that patients are left either with two paternal or two maternal copies of this region of the genome after mitotic recombination. Skoda and coworkers sequenced the genes in the minimal region of UPD to identify the JAK2V617F allele.16 As with the functional approach undertaken by Vainchenker's group, this approach also has important general relevance to the investigation of the genetic basis of cancer. Recent studies have shown that UPD, resulting in homozygous gain-of-function alleles, is observed for other oncogenic alleles, including FLT3 in acute myeloid leukemia,22 and MPL in PMF (RLL and DG Gilliland, unpublished observation). The advent of high-resolution genomic platforms, most notably single nucleotide polymorphism arrays, will facilitate the identification of regions of UPD,23, 24 which can then be subjected to high-throughput DNA resequencing for somatic mutations.25, 26, 27
The remaining two groups used candidate gene approaches to discover the JAK2V617F allele. Anthony Green and coworkers used candidate resequencing of genes relevant to signaling pathways important in oncogenic transformation to identify the JAK2V617F allele in PV, ET and PMF.14 The group led by Gary Gilliland resequenced conserved domains of all tyrosine kinases on a large set of MPN patients who provided samples using an Internet-based collection protocol.17 This ‘tyrosine kinome’ resequencing strategy has been used to identify oncogenic alleles in a spectrum of human malignancies, including colorectal cancer,25 lung cancer,26 and more recently in acute myeloid leukemia.27 These candidate gene resequencing studies have become easier to perform as standard resequencing decreases in cost and as next-generation sequencing technologies become feasible for larger resequencing efforts; however, these approaches will likely lead to the identification of ‘driver’ and ‘passenger’ alleles, and as discussed above functional studies will be of paramount importance to elucidate those mutations that actually contribute to oncogenic transformation. Moreover, it will be important to assess whether candidate mutations are acquired or inherited through analysis of matched normal tissue, as was done to show JAK2V617F was somatic; therefore analysis of tumor and matched normal DNA is absolutely required for future high-throughput genomic studies.
The mutation at codon 617 of JAK2 is always the same, a guanine-to-thymidine transversion, which changes valine to phenylalanine. Given that substitution of tryptophan, methionine, isoleucine and leucine for valine at codon 617 constitutively activates JAK2,28 it is surprising that no other alleles have been identified at this position. Moreover, there are additional activating mutations in other domains of JAK2, including the T875N kinase domain mutation,29 the IREED deletion,30 and JAK2 exon 12 mutations.31 Why then do virtually all patients acquire the same mutation at codon 617? It is hoped that future genetic and functional studies will elucidate why JAK2V617F predominates in PV, ET and PMF.
A spectrum of in vitro and in vivo studies have been performed, which validate JAK2V617F as an oncogene; however, the most important studies performed to date are in vivo assays in which JAK2V617F is expressed in the murine bone marrow transplantation assay.32, 33, 34, 35 In this context, expression of Jak2V617F, but not wild-type Jak2, in recipient mice results in a short latency, fully penetrant MPN notable for marked polycythemia, strain-specific leukocytosis, extramedullary hematopoiesis and interestingly, an absence of thrombocytosis. Although these data do not allow us to elucidate how a single disease allele contributes to three distinct diseases, they provide in vivo evidence of hematopoietic transformation by this oncogene, and provide a platform for testing JAK2-directed therapies in an in vivo setting.36
JAK2V617F: a breakthrough discovery, but the beginning of the journey
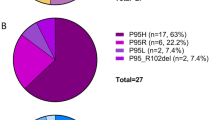
The discovery of the JAK2V617F allele was a landmark discovery; however, it represents the start of what is an important journey into the genetic basis of PV, ET and PMF. The first question, which has begun to be addressed, is the molecular etiology of JAK2V617F-negative PV, ET and PMF. Sensitive, allele-specific assays suggest that almost all patients with PV are JAK2V617F-positive;37 however, a subset of patients with PV (≈5%) are JAK2V617F-negative. This led Scott, Green and their coworkers to hypothesize that JAK-STAT signaling would be activated by novel mutations in this subset of PV, and led to the identification of somatic mutations in exon 12 of JAK2 in JAK2V617F-negative PV.31 To date at least eight different somatic missense, deletion and insertion mutations in JAK2 exon 12 have been identified in JAK2V617F-negative PV-involving residues 538–543.38, 39, 40, 41 In vitro studies demonstrated that these alleles transform hematopoietic cells to cytokine-independent growth, and expression of JAK2 Exon 12 alleles in vivo causes polycythemia and leukocytosis, as is observed for JAK2V617F.
Perhaps the most interesting aspect of the discovery of JAK2 exon 12 mutations is the absence of the phenotypic pleiotropy associated with the canonical JAK2V617F allele. Studies have found these alleles in PV and not in ET/PMF, and the majority of patients with JAK2 exon 12 mutations exhibit a specific clinical phenotype, with polycythemia, variable leukocytosis, but not thrombocytosis. This suggests that different mutations in the same gene have different effects on signaling which result in distinct clinical phenotypes. From a clinical perspective, the identification of JAK2 exon 12 mutations provides a diagnostic test for JAK2V617F-negative patients who present with erythrocytosis, and the presence of JAK2 exon 12 mutations should be taken as evidence of a clonal MPN in this context.
As opposed to PV, where JAK2V617F and JAK2 exon 12 mutations account for virtually all patients, as many as half of ET and PMF are JAK2V617F-negative. No group has identified mutations in JAK2 in JAK2V617F-negative ET and PMF. Given the likelihood that JAK-STAT signaling would be involved in JAK2V617F-negative ET and PMF, Pikman et al.42 asked whether mutations in the type I cytokine receptors known to interact with JAK2 could be identified in these patients. This led to the identification of mutations of the thrombopoietin receptor (MPL) at codon 515. Unlike valine 617, substitution of leucine, lysine or alanine for tryptophan 515 have all been reported at codon 515, and these mutations are all transforming in vitro.42, 43, 44 These mutations occur in a subset of patients with JAK2V617F-negative ET and PMF, including 8.5% of JAK2V617F-negative ET patients,45 and approximately 10% of JAK2V617F-negative PMF patients.42, 43, 44 Three patients have also recently been described with somatic MPLS505N mutations,45 an allele which had previously been associated with inherited thrombocytosis.46 MPLW515-positive ET patients have higher platelet counts and lower hemoglobin levels than JAK2V617F-positive ET patients,45, 47 and MPLW515-positive PMF patients present with more severe anemia.48 Moreover, endogenous megakaryocyte colonies, but not endogenous erythroid colony, can be grown from MPLW515-positive patient cells. These data suggest that there are differences in signaling between JAK2V617F and MPLW515 mutations, which are of clinical relevance. The murine data supports this notion, as expression of MPLW515L causes a phenotype which is distinct from JAK2V617F in the murine BMT model, with thrombocytosis, leukocytosis and myelofibrosis, but not polycythemia, in recipient mice.
The most important aspect of the discovery of JAK2 exon 12 and MPL mutations in JAK2V617F-negative MPN is the demonstration that activation of JAK2 signaling is seen in both JAK2V617F-positive and JAK2V617F-negative disease, either through mutations in JAK2 itself or in cytokine receptors. The question remains, though as to whether patients with JAK2/MPL-negative MPN have evidence of JAK2 activation and dependence on this pathway for proliferation. A spectrum of in vitro and in vivo assays can be used to assess this possibility; however, the most convincing data will emerge from clinical trials of JAK2 inhibitors that will allow us to know whether patients with JAK2/MPL-negative MPN are sensitive to JAK2 inhibitors at similar doses to JAK2/MPL-positive patients.
Dilemma of one mutation and three phenotypes
The second unanswered question, which is perhaps the most important from a pathogenetic standpoint, is how does a single disease allele contribute to the pathogenesis of PV, ET and PMF, three distinct clinical disorders. A number of hypotheses have been posited to explain the phenotypic pleiotropy of these disorders.
Gene dosage
As discussed above, homozygosity for JAK2V617F is the result of UPD at chromosome 9p24, and the initial studies noted that homozygosity for JAK2V617F was much more common in PV than in ET.14, 15, 16, 17 The gene dosage hypothesis is also supported by clonogenic colony data, as Scott et al.49 showed that homozygous JAK2V617F mutant erythroid colonies are observed in most patients with PV but are rare in ET. Therefore we can surmise that 9p24 UPD and JAK2V617F homozygosity is common, and early, in the development of PV, but not ET, suggesting that a high level of JAK2 signaling favors an erythroid phenotype and a low JAK2 state favors a megakaryocyte phenotype. In vivo studies are consistent with this hypothesis, as overexpression of Jak2V617F in the hematopoietic compartment results in polycythemia and leukocytosis without associated thrombocytosis,32, 33, 34, 35 and transgenic expression of JAK2V617F at a much lower level results in thrombocytosis.50, 51, 52 It is likely there are differences in constitutive signaling in cells heterozygous and homozygous for JAK2V617F that are relevant to MPN phenotype. Future studies are needed to elucidate the mechanism by which JAK2V617F gene dosage affects MPN pathogenesis.
Germ line modifiers
Pardanani et al.53 asked whether single nucleotide polymorphisms in JAK2, MPL, EPOR and GCSFR influence phenotype. Analysis of 32 single nucleotide polymorphisms in 179 patients with MPN allowed them to determine that specific single nucleotide polymorphisms were associated with PV or with ET. Although these data are from a single cohort, they provide evidence that host genetic variation is relevant to MPN phenotype. Nonetheless, these data provide evidence that host genetic variation is important to the phenotypic diversity of these diseases and sets the stage for future efforts aimed at elucidating the role of germ line variation in phenotype, response to specific therapies and MPN-associated complications.
Predisposition alleles
In families with a predisposition to the development of MPN,54 JAK2V617F is acquired as a somatic allele.55, 56 This suggests that there are MPN predisposition alleles, which provide a specific selective advantage to the development of mutations in the JAK2-signaling pathway. We would predict these alleles are relevant to signaling in this pathway, given that kindreds have been described with JAK2V617F-positive and JAK2 exon 12 positive MPN,39 and there are patients with JAK2V617F-positive, MPLW515L-positive disease,43 suggesting that there is extremely strong selection for JAK2-activating alleles in this context. Moreover, a recent study noted an increased risk of MPN for first-degree relatives of MPN patients,57 suggesting there are common MPN susceptibility alleles which might be relevant to presumed sporadic MPN.
Additional somatic mutations
Cytogenetic abnormalities have been observed in patients with MPN, most notably including deletion in chromosome 20q.58 In addition, patients have been observed where all hematopoietic cells had deletions of 20q loss and only a subset were positive for JAK2V617F.59 These data suggest there are ‘pre-JAK2 alleles’ which arise before the acquisition of the JAK2V617F allele in some patients. The most intriguing data comes from patients with a JAK2V617F-positive MPN transform to a JAK2V617F-negative acute leukemia,60, 61 suggesting there is a ‘pre-JAK2’-transformed hematopoietic progenitor. The identity of these alleles remains a mystery.
JAK2/MPL mutations and signaling
The relevance of specific-signaling pathways in JAK2V617F-mediated hematopoietic transformation has not been fully uncovered. Many groups have focused on the STAT family of transcription factors, including STAT5A and STAT5B,62, 63 based on previous studies showing that STAT5A and STAT5B are necessary for TEL-JAK2-mediated myeloproliferation.64 Additional studies are needed to ascertain the relevance of specific STAT transcription factors, the MAP kinase signaling pathway, PI3 kinase and other signaling pathways activated by JAK2V617F to MPN pathogenesis. Moreover, it remains to be seen whether there are differences in activation of signaling by JAK2V617F, JAK2 exon 12 mutations and by MPL mutations, and whether these differences are of clinical and/or pathogenic relevance.
Targeted therapy for MPNs
We are all hopeful that inhibitors of JAK2 will be safe and effective, and specific inhibitors of JAK2 kinase activity have entered the clinic in phase I/II trials in PMF and post-PV/ET myelofibrosis.65 It is important to consider there may be significant toxicities associated with JAK2 inhibition, making it likely that JAK2 inhibitors will have to demonstrate safety in patients with PMF or post-PV/ET-PMF before being tested in PV and ET. Colony assays suggest that JAK2 inhibitors will be of value for patients with JAK2 exon 12 or MPL mutations,41 and JAK2 inhibitor treatment in patients with JAK2/MPL-negative MPN would allow a direct test of the hypothesis that JAK-STAT signaling is central to the pathogenesis of PV, ET and PMF. Although there is considerable enthusiasm for JAK2 inhibitor development in these disorders, we must keep in mind a number of important concerns about these agents as they enter the clinical arena. First, resistance is likely to emerge in some patients treated with JAK2 inhibitors, which should be studied using in vitro systems. Moreover, the data showing that JAK2V617F-negative acute myeloid leukemia occurs frequently in patients with a JAK2V617F-positive MPN,60, 61 raises the troubling possibility that JAK2 inhibitor therapy might increase the risk of leukemic transformation. As we move forward into the clinic with these agents, it will be important to ask clinically and biologically relevant questions, and to ascertain the potential limitations of these agents to derive the most benefit for patients with the different MPN.
Future directions
Although the recent discovery of JAK2V617F and MPL mutations have provided important insight into the biology of PV, ET and PMF, there is much more to be done to unravel the mystery of these MPN. The identity of the causative alleles in JAK2/MPL-negative MPN are a mystery, and the biologic differences between JAK2V617F, JAK2 exon 12 alleles and MPL alleles are not known. Moreover, the basis of the phenotypic pleiotropy in JAK2V617F-positive MPN, and the role of additional inherited and acquired disease alleles remains to be delineated. We can truly say that the post-JAK2V617F era is an exciting era in MPN biology and therapy, and the best is yet to come!
References
Dameshek W . Some speculations on the myeloproliferative syndromes. Blood 1951; 6: 372–375.
Tefferi A, Thiele J, Orazi A, Kvasnicka HM, Barbui T, Hanson CA et al. Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood 2007; 110: 1092–1097.
Heisterkamp N, Stephenson JR, Groffen J, Hansen PF, de Klein A, Bartram CR et al. Localization of the c-ab1 oncogene adjacent to a translocation break point in chronic myelocytic leukaemia. Nature 1983; 306: 239–242.
Cools J, DeAngelo DJ, Gotlib J, Stover EH, Legare RD, Cortes J et al. A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med 2003; 348: 1201–1214.
Golub T, Barker G, Lovett M, Gilliland D . Fusion of PDGF receptor beta to a novel ets-like gene, tel, in chronic myelomonocytic leukemia with t(5;12) chromosomal translocation. Cell 1994; 77: 307–316.
Fialkow P, Gartler SM, Yoshida A . Clonal origin of chronic myelocytic leukemia in man. Proc Natl Acad Sci USA 1967; 58: 1468–1471.
Adamson JW, Fialkow PJ, Murphy S, Prchal JF, Steinmann L . Polycythemia vera: stem-cell and probable clonal origin of the disease. N Engl J Med 1976; 295: 913–916.
Tsukamoto N, Morita K, Maehara T, Okamoto K, Sakai H, Karasawa M et al. Clonality in chronic myeloproliferative disorders defined by X-chromosome linked probes: demonstration of heterogeneity in lineage involvement. British Journal of Haematology 1994; 86: 253–258.
El Kassar N, Hetet G, Li Y, Briere J, Grandchamp B . Clonal analysis of haemopoietic cells in essential thrombocythaemia. Br J Haem 1995; 90: 131–137.
Prchal JF, Axelrad AA . Letter: Bone-marrow responses in polycythemia vera. N Engl J Med 1974; 290: 1382.
Lutton JD, Levere RD . Endogenous erythroid colony formation by peripheral blood mononuclear cells from patients with myelofibrosis and polycythemia vera. Acta Haematol 1979; 62: 94–99.
Silva M, Richard C, Benito A, Sanz C, Olalla I, Fernandez-Luna JL . Expression of Bcl-x in erythroid precursors from patients with polycythemia vera. N Engl J Med 1998; 338: 564–571.
Moliterno AR, Hankins WD, Spivak JL . Impaired expression of the thrombopoietin receptor by platelets from patients with polycythemia vera. N Engl J Med 1998; 338: 572–580.
Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 2005; 365: 1054–1061.
James C, Ugo V, Le Couedic JP, Staerk J, Delhommeau F, Lacout C et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 2005; 434: 1144–1148.
Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 2005; 352: 1779–1790.
Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJ et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 2005; 7: 387–397.
Ugo V, Marzac C, Teyssandier I, Larbret F, Lecluse Y, Debili N et al. Multiple signaling pathways are involved in erythropoietin-independent differentiation of erythroid progenitors in polycythemia vera. Exp Hematol 2004; 32: 179–187.
Greenman C, Stephens P, Smith R, Dalgliesh GL, Hunter C, Bignell G et al. Patterns of somatic mutation in human cancer genomes. Nature 2007; 446: 153–158.
Frohling S, Scholl C, Levine RL, Loriaux M, Boggon TJ, Bernard OA et al. Identification of driver and passenger mutations of FLT3 by high-throughput DNA sequence analysis and functional assessment of candidate alleles. Cancer Cell 2007; 12: 501–513.
Kralovics R, Guan Y, Prchal JT . Acquired uniparental disomy of chromosome 9p is a frequent stem cell defect in polycythemia vera. Exp Hematol 2002; 30: 229–236.
Frohling S, Schlenk RF, Breitruck J, Benner A, Kreitmeier S, Tobis K et al. Prognostic significance of activating FLT3 mutations in younger adults (16 to 60 years) with acute myeloid leukemia and normal cytogenetics: a study of the AML Study Group Ulm. Blood 2002; 100: 4372–4380.
Gondek LP, Dunbar AJ, Szpurka H, McDevitt MA, Maciejewski JP . SNP array karyotyping allows for the detection of uniparental disomy and cryptic chromosomal abnormalities in MDS/MPD-U and MPD. PLoS ONE 2007; 2: e1225.
Raghavan M, Smith LL, Lillington DM, Chaplin T, Kakkas I, Molloy G et al. Segmental uniparental disomy is a commonly acquired genetic event in relapsed acute myeloid leukemia. Blood 2008; 112: 814–821.
Bardelli A, Parsons DW, Silliman N, Ptak J, Szabo S, Saha S et al. Mutational analysis of the tyrosine kinome in colorectal cancers. Science 2003; 300: 949.
Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 2004; 304: 1497–1500.
Loriaux MM, Levine RL, Tyner JW, Frohling S, Scholl C, Stoffregen EP et al. High-throughput sequence analysis of the tyrosine kinome in acute myeloid leukemia. Blood 2008; 111: 4788–4796.
Dusa A, Staerk J, Elliott J, Pecquet C, Poirel HA, Johnston JA et al. Substitution of pseudokinase domain residue Val-617 by large non-polar amino acids causes activation of JAK2. J Biol Chem 2008; 283: 12941–12948.
Mercher T, Wernig G, Moore SA, Levine RL, Gu TL, Frohling S et al. JAK2T875N is a novel activating mutation that results in myeloproliferative disease with features of megakaryoblastic leukemia in a murine bone marrow transplantation model. Blood 2006; 108: 2770–2779.
Malinge S, Ben-Abdelali R, Settegrana C, Radford-Weiss I, Debre M, Beldjord K et al. Novel activating JAK2 mutation in a patient with Down syndrome and B-cell precursor acute lymphoblastic leukemia. Blood 2007; 109: 2202–2204.
Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR et al. JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med 2007; 356: 459–468.
Lacout C, Pisani DF, Tulliez M, Gachelin FM, Vainchenker W, Villeval JL . JAK2V617F expression in murine hematopoietic cells leads to MPD mimicking human PV with secondary myelofibrosis. Blood 2006; 108: 1652–1660.
Wernig G, Mercher T, Okabe R, Levine RL, Lee BH, Gilliland DG . Expression of Jak2V617F causes a polycythemia vera-like disease with associated myelofibrosis in a murine bone marrow transplant model. Blood 2006; 107: 4274–4281.
Zaleskas VM, Krause DS, Lazarides K, Patel N, Hu Y, Li S et al. Molecular pathogenesis and therapy of polycythemia induced in mice by JAK2 V617F. PLoS ONE 2006; 1: e18.
Bumm TG, Elsea C, Corbin AS, Loriaux M, Sherbenou D, Wood L et al. Characterization of murine JAK2V617F-positive myeloproliferative disease. Cancer Res 2006; 66: 11156–11165.
Wernig G, Kharas MG, Okabe R, Moore SA, Leeman DS, Cullen DE et al. Efficacy of TG101348, a selective JAK2 inhibitor, in treatment of a murine model of JAK2V617F-induced polycythemia vera. Cancer Cell 2008; 13: 311–320.
Levine RL, Belisle C, Wadleigh M, Zahrieh D, Lee S, Chagnon P et al. X-inactivation-based clonality analysis and quantitative JAK2V617F assessment reveal a strong association between clonality and JAK2V617F in PV but not ET/MMM, and identifies a subset of JAK2V617F-negative ET and MMM patients with clonal hematopoiesis. Blood 2006; 107: 4139–4141.
Kiladjian JJ, Cervantes F, Leebeek FW, Marzac C, Cassinat B, Chevret S et al. The impact of JAK2 and MPL mutations on diagnosis and prognosis of splanchnic vein thrombosis: a report on 241 cases. Blood 2008; 111: 4922–4929.
Pietra D, Li S, Brisci A, Passamonti F, Rumi E, Theocharides A et al. Somatic mutations of JAK2 exon 12 in patients with JAK2 (V617F)-negative myeloproliferative disorders. Blood 2008; 111: 1686–1689.
Williams DM, Kim AH, Rogers O, Spivak JL, Moliterno AR . Phenotypic variations and new mutations in JAK2 V617F-negative polycythemia vera, erythrocytosis, and idiopathic myelofibrosis. Exp Hematol 2007; 35: 1641–1646.
Lasho TL, Tefferi A, Hood JD, Verstovsek S, Gilliland DG, Pardanani A . TG101348, a JAK2-selective antagonist, inhibits primary hematopoietic cells derived from myeloproliferative disorder patients with JAK2V617F, MPLW515K or JAK2 exon 12 mutations as well as mutation negative patients. Leukemia 2008: published online.
Pikman Y, Lee BH, Mercher T, McDowell E, Ebert BL, Gozo M et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med 2006; 3: e270.
Pardanani AD, Levine RL, Lasho T, Pikman Y, Mesa RA, Wadleigh M et al. MPL515 mutations in myeloproliferative and other myeloid disorders: a study of 1182 patients. Blood 2006; 108: 3472–3476.
Chaligne R, Tonetti C, Besancenot R, Roy L, Marty C, Mossuz P et al. New mutations of MPL in primitive myelofibrosis: only the MPL W515 mutations promote a G(1)/S-phase transition. Leukemia 2008: published online.
Beer PA, Campbell PJ, Scott LM, Bench AJ, Erber WN, Bareford D et al. MPL mutations in myeloproliferative disorders: analysis of the PT-1 cohort. Blood 2008; 112: 141–149.
Ding J, Komatsu H, Wakita A, Kato-Uranishi M, Ito M, Satoh A et al. Familial essential thrombocythemia associated with a dominant-positive activating mutation of the c-MPL gene, which encodes for the receptor for thrombopoietin. Blood 2004; 103: 4198–4200.
Vannucchi AM, Antonioli E, Guglielmelli P, Pancrazzi A, Guerini V, Barosi G et al. Characteristics and clinical correlates of MPL 515W>L/K mutation in essential thrombocythemia. Blood 2008; 112: 844–847.
Guglielmelli P, Pancrazzi A, Bergamaschi G, Rosti V, Villani L, Antonioli E et al. Anaemia characterises patients with myelofibrosis harbouring Mpl mutation. Br J Haematol 2007; 137: 244–247.
Scott LM, Scott MA, Campbell PJ, Green AR . Progenitors homozygous for the V617F mutation occur in most patients with polycythemia vera, but not essential thrombocythemia. Blood 2006; 108: 2435–2437.
Tiedt R, Hao-Shen H, Sobas MA, Looser R, Dirnhofer S, Schwaller J et al. Ratio of mutant JAK2-V617F to wild-type Jak2 determines the MPD phenotypes in transgenic mice. Blood 2008; 111: 3931–3940.
Xing S, Wanting TH, Zhao W, Ma J, Wang S, Xu X et al. Transgenic expression of JAK2V617F causes myeloproliferative disorders in mice. Blood 2008; 111: 5109–5117.
Shide K, Shimoda HK, Kumano T, Karube K, Kameda T, Takenaka K et al. Development of ET, primary myelofibrosis and PV in mice expressing JAK2 V617F. Leukemia 2008; 22: 87–95.
Pardanani A, Fridley BL, Lasho TL, Gilliland DG, Tefferi A . Host genetic variation contributes to phenotypic diversity in myeloproliferative disorders. Blood 2008; 111: 2785–2789.
Kralovics R, Stockton DW, Prchal JT . Clonal hematopoiesis in familial polycythemia vera suggests the involvement of multiple mutational events in the early pathogenesis of the disease. Blood 2003; 102: 3793–3796.
Cario H, Goerttler PS, Steimle C, Levine RL, Pahl HL . The JAK2V617F mutation is acquired secondary to the predisposing alteration in familial polycythaemia vera. Br J Haematol 2005; 130: 800–801.
Bellanne-Chantelot C, Chaumarel I, Labopin M, Bellanger F, Barbu V, De Toma C et al. Genetic and clinical implications of the Val617Phe JAK2 mutation in 72 families with myeloproliferative disorders. Blood 2006; 108: 346–352.
Landgren O, Goldin LR, Kristinsson SY, Helgadottir EA, Samuelsson J, Bjorkholm M . Increased risks of polycythemia vera, essential thrombocythemia, and myelofibrosis among 24577 first-degree relatives of 11039 patients with myeloproliferative neoplasms in Sweden. Blood 2008: published online.
Asimakopoulos FA, White NJ, Nacheva E, Green AR . Molecular analysis of chromosome 20q deletions associated with myeloproliferative disorders and myelodysplastic syndromes. Blood 1994; 84: 3086–3094.
Kralovics R, Teo SS, Li S, Theocharides A, Buser AS, Tichelli A et al. Acquisition of the V617F mutation of JAK2 is a late genetic event in a subset of patients with myeloproliferative disorders. Blood 2006; 108: 1377–1380.
Campbell PJ, Baxter EJ, Beer PA, Scott LM, Bench AJ, Huntly BJ et al. Mutation of JAK2 in the myeloproliferative disorders: timing, clonality studies, cytogenetic associations, and role in leukemic transformation. Blood 2006; 108: 3548–3555.
Theocharides A, Boissinot M, Girodon F, Garand R, Teo SS, Lippert E et al. Leukemic blasts in transformed JAK2-V617F-positive myeloproliferative disorders are frequently negative for the JAK2-V617F mutation. Blood 2007; 110: 375–379.
Lu X, Levine R, Tong W, Wernig G, Pikman Y, Zarnegar S et al. Expression of a homodimeric type I cytokine receptor is required for JAK2V617F-mediated transformation. Proc Natl Acad Sci USA 2005; 102: 18962–18967.
Garcon L, Rivat C, James C, Lacout C, Camara-Clayette V, Ugo V et al. Constitutive activation of STAT5 and Bcl-xL overexpression can induce endogenous erythroid colony formation in human primary cells. Blood 2006; 108: 1551–1554.
Schwaller J, Parganas E, Wang D, Cain D, Aster JC, Williams IR et al. Stat5 is essential for the myelo- and lymphoproliferative disease induced by TEL/JAK2. Mol Cell 2000; 6: 693–704.
Verstovek S, Kantarjian H, Pardanani A, Thomas D, Cortes J, Mesa R et al. A phase I/II study of ICNB018424, an oral, selective JAK inhibitor, in patients with primary myelofibrosis and postPV/ET myelofibrosis. American Socierty of Clincial Oncology Annual Meeting 2008, Abstract 7004.
Acknowledgements
We acknowledge the patients, physicians, and investigators who have contributed to our understanding of these disorders. The Levine Laboratory is supported by the US National Institutes of Health, the Howard Hughes Medical Institute Early Career Award Program, the American Society of Hematology, and the Doris Duke Charitable Foundation Clinical Scientist Development Award program. RLL is an American Society of Hematology Basic Research Fellow and is the Geoffrey Beene Junior Chair at Memorial Sloan Kettering Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kilpivaara, O., Levine, R. JAK2 and MPL mutations in myeloproliferative neoplasms: discovery and science. Leukemia 22, 1813–1817 (2008). https://doi.org/10.1038/leu.2008.229
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2008.229
Keywords
This article is cited by
-
Medicinal chemistry perspective of JAK inhibitors: synthesis, biological profile, selectivity, and structure activity relationship
Molecular Diversity (2024)
-
The Role of Caspase Genes Polymorphisms in Genetic Susceptibility to Philadelphia-Negative Myeloproliferative Neoplasms in a Portuguese Population
Pathology & Oncology Research (2019)
-
Activating JAK2 mutants reveal cytokine receptor coupling differences that impact outcomes in myeloproliferative neoplasm
Leukemia (2017)
-
Targeted next-generation sequencing identified novel mutations in triple-negative myeloproliferative neoplasms
Medical Oncology (2017)
-
Genetic–pathologic characterization of myeloproliferative neoplasms
Experimental & Molecular Medicine (2016)