Abstract
Overexpression of the ecotropic virus integration-1 (EVI1) gene (EVI1+), localized at chromosome 3q26, is associated with adverse outcome in adult acute myeloid leukemia (AML). In pediatric AML, 3q26 abnormalities are rare, and the role of EVI1 is unknown. We studied 228 pediatric AML samples for EVI1+ using gene expression profiling and RQ-PCR. EVI1+ was found in 20/213 (9%) of children with de novo AML, and in 4/8 with secondary AML. It was predominantly found in MLL-rearranged AML (13/47), monosomy 7 (2/3), or FAB M6/7 (6/10), and mutually exclusive with core-binding factor AML, t(15;17), and NPM1 mutations. Fluorescent in situ hybridization (FISH) was performed to detect cryptic 3q26 abnormalities. However, none of the EVI1+ patients harbored structural 3q26 alterations. Although significant differences in 4 years pEFS for EVI1+ and EVI1− pediatric AML were observed (28%±11 vs 44%±4, P=0.04), multivariate analysis did not identify EVI1+ as an independent prognostic factor. We conclude that EVI1+ can be found in ∼10% of pediatric AML. Although EVI1+ was not an independent prognostic factor, it was predominantly found in subtypes of pediatric AML that are related with an intermediate to unfavorable prognosis. Further research should explain the role of EVI1+ in disease biology in these cases. Remarkably, no 3q26 abnormalities were identified in EVI1+ pediatric AML.
Similar content being viewed by others
Introduction
In various myeloid malignancies 3q26 rearrangements can be found.1 These abnormalities are often associated with overexpression of the ecotropic virus integration-1 (EVI1) gene, which is localized at 3q26.2 The EVI1 gene encodes for a DNA-binding protein with two zinc-finger domains.3 It has been shown to have an essential role in early development, as inactivation of EVI1 in mice embryos is lethal within 8 days after conception.4 More information on the role of EVI1 in leukemogenesis was gained in murine leukemia studies using retroviral insertion.5 Both in mouse and human myeloid progenitors, overexpression of EVI1 is suggested to impair granulocytic differentiation in hematopoietic stem cells, and hence to result in maturation arrest.2 Interestingly, myeloid malignancies associated with EVI1 overexpression often show dysplastic megakaryopoiesis.1, 6 Although the EVI1 function is not fully understood, recent studies suggest that this gene is involved in chromatin remodeling, through interactions with H3K9 methyltransferases7, 8
Five splice variants of EVI1 have been reported, that is EVI1-1A, -1B, -1C, -1D, and -3L, as well as the MDS1/EVI1 intergenic splice variant.9, 10 The MDS1 gene is located upstream of EVI1 and its function is currently unknown. In the MDS1/EVI1 transcripts, the first two exons of MDS1 have been fused to exon 2 of EVI1, resulting in a so-called PR domain containing the EVI1 protein.10 The PR domain is highly correlated to the SET domain, which has been shown to have a critical role in chromatin-mediated gene expression histone methyltransferases.11 In cells that express MDS1/EVI1 transcripts, the EVI1 transcripts are normally expressed as well.
In adult acute myeloid leukemia (AML) overexpression of EVI1 is found in particular in patients with a 3q26 rearrangement, such as inv(3)(q21q26) or t(3;3)(q21;q26). However, high EVI1 levels have also been discovered in a separate subgroup of AML patients without 3q26 rearrangements.12, 13 In clinical studies in adult AML, overexpression of EVI1 has shown to be an independent prognostic factor, irrespective of harboring typical 3q26 rearrangements. It was recently shown that high EVI1 expression can also occur in the absence of the MDS1/EVI1 transcript in patients with cryptic 3q26 rearrangements involving the EVI1 gene.13 In contrast, patients with high expression of both EVI1 and MDS1/EVI1 were frequently found in adult MLL-rearranged AML cases.13
In children with AML, 3q26 rearrangements have not been frequently described and the role of EVI1 is unknown.14 Therefore, we studied the occurrence and the role of EVI1 overexpression in a large cohort of 228 children with AML.
Materials and methods
Patients
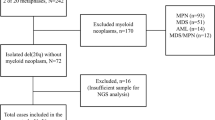
Viably frozen bone marrow or peripheral blood samples from 221 patients with newly diagnosed AML, comprising 213 with de novo and 8 with secondary-AML, were provided by the Dutch Childhood Oncology Group (DCOG), the ‘Berlin–Frankfurt–Münster’ AML Study Group (AML-BFM-SG), and the Czech Pediatric Hematology. In addition, 7 relapse samples (no paired samples were included) of AML patients were included. Informed consent was obtained from all patients, after Institutional Review Board approval according to national law and regulations. As a control for EVI1 expression, normal bone marrow of 2 children and 6 adults with informed consent was available at the Erasmus MC—Sophia Children's Hospital in Rotterdam, The Netherlands. Each study group performed central review of the morphology, according to the WHO/FAB (French-American-British) classification.15 They also provided data on the clinical follow-up of these patients. Survival analysis was restricted to a subset of 198 de novo AML patients who were treated using AML-BFM-98, AML BFM-2004, DCOG-BFM-87, DCOG 92/94, DCOG 97 protocols. Details of the treatment protocols included in the survival analysis and overall outcome data have been previously published, with the exception of study AML-BFM-2004, which is ongoing.16, 17, 18 Because of a selection based on material availability, the survival rates of this patient cohort studied for survival analysis (n=198) are slightly different from the studies published earlier.16, 17, 18 Treatment consisted of 4–5 blocks of intensive chemotherapy, using a standard cytarabine and anthracycline backbone.
Leukemic cells were isolated and enriched from these samples as described earlier.19 All resulting samples contained ⩾80% leukemic cells, as determined morphologically by May–Grünwald–Giemsa (Merck, Darmstadt, Germany)-stained cytospins. A minimum of 5 × 106 purified leukemic cells were lysed in Trizol reagent (Gibco BRL, Life Technologies, Breda, The Netherlands) and stored at −80 °C. Genomic DNA and total cellular RNA were isolated as described earlier.20
Cytogenetic and molecular analysis
Leukemic samples were routinely investigated for cytogenetic abnormalities by standard chromosome-banding analysis, and screened for recurrent non-random genetic abnormalities characteristic for AML, including t(15;17), inv(16), t(8;21), and MLL rearrangements, using either real-time polymerase chain reaction (RT-PCR) and/or fluorescent in situ hybridization (FISH) by each study group. NPM1, CEBPA, MLL-PTD, NRAS, KRAS, PTPN11, C-KIT, FLT3 mutational screening was performed as described earlier.21, 22, 23, 24, 25, 26
Microarray-based gene expression profiling
Integrity of total RNA was checked using the Agilent 2100 Bio-analyzer (Agilent, Santa Clara, CA, USA). cDNA and biotinylated cRNA was synthesized hybridized and processed on the Affymetrix Human Genome U133 Plus 2.0 Array (Affymetrix, Santa Clara, CA, USA) according to the manufacturer's guidelines. Data-acquisition was performed using expresso (Bioconductor package Affy27) and probe-set intensities were normalized using the variance stabilization normalization (Bioconductor package VSN28) in the statistical data analysis environment R, version 2.2.0.29
Identification of EVI1 overexpression with gene expression profiling
Four probe sets are positioned within the EVI1 gene (Supplementary Figure 1). Normalized intensities of these probe sets were extracted from the complete data set and further clustering analysis was performed with Genemaths XT (Applied Maths, Austin, TX, USA). Of each probe set, the standard deviation using the median as cutoff was calculated for all patients. As the probe sets 243277_x_at and 215851_at were located in introns of the EVI1 gene, only the probe sets 221884_at and 226420_at were used for hierarchical clustering using the Euclidean distance. Samples were considered to have an abnormal EVI1 expression (EVI1+) based on the hierarchical clustering dendrogram.
Gene expression signatures for EVI1+ cases
To find gene expression signatures for EVI1, an empirical Bayes linear regression model was used (R package limma).30 Moderated T-statistics P-values were corrected for multiple testing using the false discovery rate (FDR) method defined by Benjamini and Hochberg.31 This was performed using models without and with correction for the different cytogenetic subgroups (MLL-rearranged AML, t(8;21), inv(16), t(15;17), normal-, remaining-, and unknown cytogenetics).30 In addition, gene expression signatures were generated for EVI1+ in specific subsets of AML (that is MLL-rearranged AML and non-MLL-rearranged AML).
RT quantitative PCR and FISH
In 179 samples, including 22 samples with EVI1 overexpression based on microarray analysis, the RNA expression could be validated by RT quantitative PCR (RQ-PCR). For the other 49 samples, no additional RNA was available to perform RQ-PCR. The relative expression of the EVI1 transcripts (EVI1-1A, -1B, -1D, and -3L) and MDS1/EVI1 transcript was calculated using the comparative cycle time (ΔCt) method, with GAPDH as the house-keeping gene.32 Primer en probe sequences are shown in Supplementary Table 1. A sample was considered EVI1+ with RQ-PCR, if the cumulative relative expression EVI1-1A, -1B, and -3L to GAPDH was above 1.5%. This showed the highest correlation with EVI1+ cases based on gene expression profiling and all normal bone marrow samples were below this threshold.
Interphase cytospins of cases with a high EVI1 expression were screened with FISH for cryptic 3q26 abnormalities with the Poseidon Repeat Free EVI t(3;3) inv(3) Break probe (Kreatech, Amsterdam, The Netherlands) according to the manufacture's protocol.
Additional statistical analysis
Statistical analysis was performed with SPSS 11.0 (SPSS Inc. Chicago, IL, USA) and SAS (SAS-PC, version 9.1). Different variables were compared with the χ2 test or the Mann–Whitney U test. Probabilities of overall survival (pOS) and event-free survival (pEFS, events: no CR, relapse, secondary malignancy, death from any cause) were estimated by the method of Kaplan and Meier. Correlation between microarray gene expression and the RQ-PCR of the different transcript of EVI1 was measured with the Spearman correlation coefficient. The Cox Proportional hazards model analysis was applied to determine the association of EVI1+ with pOS, pEFS, adjusted for prognostic factors. All tests were two-tailed and a P-value of <0.05 was considered significant.
Results
EVI1 overexpression in pediatric AML as determined by gene expression profiling
Four probe sets on the Affymetrix Human Genome U133 Plus 2.0 Array were present within the EVI1 gene (Supplementary Figure 1). These probe sets were located in regions common for all isoforms of EVI1. However, 243277_x_at was found in intron 2–3 and 215851_at was found partly in intron.15, 16 As these short probe sets also showed more random variation of expression, they were not included in the hierarchical clustering analysis. By means of hierarchical clustering of the gene expression profiling data, three separate clusters could be identified: one cluster with high expression of EVI1 (cluster 1), one cluster with an intermediate-to-high expression of EVI1 (cluster 2), and one large cluster with low expression of EVI1. Therefore, 24 cases in the clusters with intermediate and high expression were considered EVI1+ based on the dendrogram (Figure 1). These cases included 19/213 (9%) patients with de novo AML, 4/8 (50%) patients with secondary AML, and one patient of whom only relapse material was available.
Hierarchical clustering using the gene expression of the three probe sets representing EVI1 in pediatric AML samples reveals a subclustering of 24 EVI1+ cases. Hierarchical clustering of 228 pediatric AML samples with probe sets 221884_at and 226420_at representing the EVI1 gene. Red represents high expression; black intermediate expression; and green low expression for the specific probe set.
Validation of EVI1 expression and 3q26 aberrations by real-time quantitative PCR and FISH
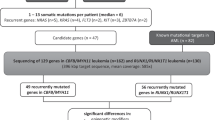
Of the 24 patients with a high-EVI1 expression, 22 could be investigated for the various EVI1 and the MDS1/EVI1 transcripts using RQ-PCR. Of two patients, the amount of available mRNA was not sufficient. In addition, RQ-PCR was also performed on 155 of the 197 remaining pediatric AML samples for which additional mRNA material was available (Figure 2). Normal bone marrow samples of eight individuals (six adults and two pediatric) were used as a control for normal expression of the different transcripts.
EVI1 expression in different cytogenetic subgroups. Cumulative mRNA expression levels of the EVI1-1A, -1B, -3L, relative to GAPDH (%) for 179 samples in different cytogenetic subgroups in pediatric AML and in 8 normal bone marrow (NBM) samples. A cumulative relative expression of 1.5% for one of the transcripts was considered positive.
Twenty-one of the 22 patients identified by gene expression profiling had a cumulative relative expression to GAPDH of at least 1.5% for one of the EVI1 transcripts (Table 1). The other patient (#20), whom lacked a cumulative relative expression of at least 1.5%, did show overexpression of EVI1-1D and MDS1/EVI1, and was considered EVI1+. In addition, one patient with FAB-M7 (#24), whom showed low expression of EVI1 on gene expression profiling, did show abnormal expression of EVI1 with RQ-PCR. All remaining samples did not show EVI1 overexpression (Figure 2). Although only 22/23 EVI1+ cases could be identified with gene expression profiling in comparison with RQ-PCR, still RQ-PCR for these four EVI1 isoforms showed high correlation with the gene expression data. Spearman correlation coefficients were 0.68 for EVI1-1A, 0.63 for EVI1-1B, 0.52 for EVI1-3L, and 0.78 for EVI1-1D. Moreover, microarray analysis showed a sensitivity of 95%, a specificity of 100%, a positive predictive value of 100%, and a negative predictive value of 99%.
On the basis of conventional cytogenetics, none of the patients harbored a 3q26 aberration. In addition, only three EVI1+ patients lacked the MDS1/EVI1 transcript, which has previously shown to be a marker to detect cryptic 3q26 aberrations.13 However, in all EVI1+ cases, cryptic 3q26 rearrangements were not detected by FISH (Table 1). Thus, combining data of the gene expression profiling and RQ-PCR, 25 EVI1+ cases were identified and none of them harbored a 3q26 aberration.
Clinical characteristics of EVI1+ in pediatric AML
EVI1+ pediatric AML was not correlated with sex, white blood cell count, or age. When studying the relationship between EVI1+ and conventional classification criteria such as morphology (FAB classification) and cytogenetic data (Table 2), a higher frequency of EVI1 overexpression was detected in patients with (1) MLL rearrangements (n=13/47 cases), including all t(6;11) cases (n=4); (2) acute megakaryoblastic leukemia (AML-M7) (n=4/7 cases); (3) acute erythroblastic leukemia (AML-M6) (n=2/3 cases); and (4) monosomy 7 (n=2/3 cases). The six remaining cases were patients with normal karyotype (n=1), other cytogenetics (n=4), or unknown karyotype (n=1), but none of them harbored a 3q26 rearrangement (Tables 1 and 2). Overexpression of EVI1 was not found in the prognostically favorable types of AML, that is t(8;21), inv(16), and t(15;17).
We also studied EVI1+ in relation to single-gene mutations. Of interest, three patients (#14, #15, and #22) showed a mutation in the RAS gene. In addition, one EVI1+ patient (#8) had a CEBPA mutation. One EVI1+ patient (#10) had a FLT3-ITD, whereas 40/203 EVI1− patients had a FLT3-ITD (respectively, 4.0% vs 19.7%, P=0.05). EVI1+ was not found in patients with NPM1, MLL-PTD, and CKIT mutations.
Gene expression signature differences within EVI1+ cases
To get insight into the biology of EVI1+, we analyzed our data set to identify a specific gene expression signature for EVI1+ pediatric AML. Using an empirical Bayes linear regression model,30 2103 discriminative probe sets for EVI1+ were identified. However, within the MLL-rearranged AML subtype, a different gene expression signature was observed compared with the EVI1+ cases in other AML subtypes (Supplementary Figure 2). After applying correction for cytogenetic subtype, the amount of discriminating probe sets decreased drastically from 2103 to 253 and only 88 of these 253 probe sets were detected to be strongly significant in both groups, that is MLL-rearranged AML and other AML subtypes. Therefore, these 88 probe sets were considered to be highly discriminative for EVI1+ (FDR corrected P<0.001) independent of their cytogenetic background. The top four probe sets represented overexpression of the EVI1 and MDS1 gene themselves. Interestingly, some other probe sets represented genes that have been reported to have a role in hematopoiesis and/or the development of leukemias, for example PBX1 and RUNX233, 34 (Supplementary Table 2).
Survival analysis and prognosis of EVI1+ in pediatric AML
Survival data were available for 198 patients, including 18 EVI1+ cases. Patients with EVI1 overexpression had a significantly worse 4 years pEFS (28%±11 vs 44%±4, P=0.04) as compared with patients without EVI1 overexpression. However, the OS was not significantly different between both groups (56±12% vs 64±4%, P=0.34) (Figures 3a and b). Within the MLL-rearranged AML group (n=40), no significant difference for 4 years pEFS (20±13% vs 40±9%, P=0.44) nor for 4 years pOS (50±16% vs 47±9%, P=0.68) between EVI1+ and EVI1− patient was found (Figures 3c and d). The fact that EVI1 overexpression did not influence outcome in pediatric AML was confirmed with multivariate analysis, including favorable karyotype, age and WBC, and showed that EVI1+ lacked independent prognostic significance for pEFS (hazard ratio (HR), 1.2; P=0.67) and for pOS (HR, 1.0; P=0.97) (Table 3).
Survival outcome for high EVI1 expression in pediatric AML. (a) Kaplan–Meier estimates for pEFS in the total cohort between EVI1+ and EVI1− patients. (b) Kaplan–Meier estimates for pOS in the total cohort between EVI1+ and EVI1− patients. (c) Kaplan–Meier estimates for pEFS in the cohort of MLL-rearranged AML between EVI1+ and EVI1− patients. (d) Kaplan–Meier estimates for pOS in the cohort of MLL-rearranged AML between EVI1+ and EVI1− patients.
Discussion
Evi1 was detected by Morishita et al.5 as a common integration site by retroviral insertion in a murine model system, leading to Evi1 overexpression and leukemia, which suggests a role for EVI1 as an oncogene. Subsequently, the human EVI1 gene was detected in the breakpoint region of chromosome 3q26 rearrangements in different myeloid malignancies.1 Additional evidence that EVI1 may act as an oncogene comes from studies by Laricchia-Robbio and Nucifora35 and Kilbey et al.36 who showed that aberrant overexpression of EVI1 results in loss of cell-cycle control and increased self-renewal. Moreover, adult AML patients with high EVI1 expression, irrespective of harboring a 3q26 abnormality, have a poor prognosis.13
Until now, no information was available on the role of the EVI1 gene in pediatric AML, in which cytogenetically detectable 3q26 abnormalities do not seem to occur frequently.14 In this study cohort, without cytogenetically detectable 3q26 abnormalities, we discovered EVI1 overexpression in 20/213 (9%) of the children with de novo AML, and in 4/8 (50%) patients with secondary AML. Moreover, we showed a strong association between EVI1 overexpression and specific genetic and morphologic subtypes of AML. In contrast to adult AML, we did not find any evidence for chromosome 3q26 aberrations, nor for cryptic 3q26 rearrangements in EVI1+ cases. However, we did identify EVI1+ in FAB-M6/M7 cases, which has not been reported in adults so far. In addition, we identified EVI1+ in subgroups that are considered to have an intermediate or poor prognosis, that is pediatric AML with MLL rearrangements and monosomy 7, which included three of the four secondary-AML cases. Overexpression of EVI1 was also identified in MLL rearrangements and monosomy 7 in adult AML.14, 37, 38 Interestingly, EVI1 expression was mutually exclusive with CBF-AML, t(15;17), and NPM1 mutations, which represent favorable types of pediatric AML.
Gilliland et al. hypothesized that the initial development of AML results from both type I and type II mutations. Type I mutations induce enhanced proliferation of the hematopoietic cells, whereas type II mutations lead to impaired differentiation and maturation arrest.39 Non-random associations between specific mutations have been shown for various other subtypes in AML, such as t(8;21) or inv(16) and c-KIT, supporting the Gilliland hypothesis.40 We found that EVI1 was overexpressed in various morphologic and genetic subtypes of childhood AML, and even in homogeneous subgroups, EVI1 overexpression was often only detectable in a subset of patients. Therefore, we assume that EVI1 overexpression is a secondary and not an initiating event that may occur later in leukemogenesis. Moreover, it is not clear whether EVI1 is a driver rather than a bystander effect in our cases with EVI1+.
Several findings, however, may support a role for EVI1+ in leukemogenesis in these specific cases. For instance, all MLL-AF6 and a significant proportion of monosomy 7 cases are clearly associated with EVI1+, not only in pediatric but also in adult AML.13 Moreover, in vivo studies with an MLL-AF9 mouse model showed overexpression of Evi1 after the leukemic transformation.41 In addition, a recent report in pediatric AML patients with monosomy 7 showed a higher incidence of 3q26 rearrangements, and a role for EVI1 was already suggested by these investigators.37 We know from Fanconi anemia that patients with 3q26 aberrations have a higher risk of developing AML and if monosomy 7 develops, this occurs in the 3q26 aberrant clone as a second event.42 Therefore, as both MLL-AF6 and monosomy 7 are associated with poor outcome in pediatric AML,37, 38, 43 this may underscore that EVI1 has a role in these leukemias. However, direct evidence demonstrating an oncogenic effect of EVI1+ overexpression in these types of leukemia could not be derived from our study and further evidence is currently lacking. Clearly, further studies need to be performed to unravel the exact biological role of EVI1+ in these leukemias.
There is also supporting evidence for a role of EVI1+ in the development of AML FAB-M6 and -M7. For instance, adult myeloid malignancies with 3q26 abnormalities show increased numbers of dysplastic megakaryocytes. Other in vitro studies show that EVI1 overexpression leads to impaired erythroid and megakaryocytic differentiation by GATA-1 inactivation.44, 45, 46 However, in vivo, no abnormalities of erythroid cells were observed in Evi1 transgenic mice, although they did show a significant reduction in the number of erythroid colony-forming units, implying a defect of erythroid hematopoiesis affecting erythroid progenitor cells.47 Therefore, overexpression of EVI1 might be involved in the development of AML of both acute erythroid and megakaryoblastic leukemia.
Unsupervised cluster analyses (data not shown) did not identify a specific cluster for EVI1+ cases, as previously reported in adult AML. These cases were often split among different clusters harboring MLL-rearranged AML (adult and pediatric AML), monosomy 7/3q26 aberrations (adult AML), or FAB-M6/M7 (pediatric AML).48 However, by supervised clustering, we found that within the subgroup of MLL-rearranged AML, EVI1+ pediatric patients revealed a different gene expression signature as compared with the EVI1+ patients in the other cytogenetic subtypes. Interestingly, methylation array profiles in adult AML identified different subgroups within EVI1+ patients, indicating the heterogeneity of this subgroup.49
Although these data strongly suggest differences in biology between subgroups of EVI1+, still probe sets were identified to be discriminative for EVI1+, independent of their cytogenetic or morphologic background after multivariate analysis. This could indicate a specific role for EVI1 overexpression in the development of leukemia in these cases, especially as some of these probe sets included genes that have previously been reported to have a role in hematopoiesis and/or the development of leukemias, for example PBX1 and RUNX2.33, 34 Moreover, recent analysis of the Pbx1 promoter region in mice revealed that Evi-1 upregulates Pbx1 transcription.50 This emphasizes that PBX1 is a possible target gene of EVI1 involved in the leukemogenesis of EVI1+ patients.
Although differences in EFS and OS for EVI1+ and EVI1− pediatric AML were observed in our study, we showed that EVI1+ has no independent prognostic value for pediatric AML, which is in contrast to adult AML.12, 13 The latter may mainly be caused by differences in the frequency of 3q26 abnormalities, but also by differences in therapy and prognosis between adults and children.
In this first study on the relevance of EVI1 overexpression in pediatric AML, we conclude that EVI1+ is found in 9% of de novo pediatric AML. EVI1 is overexpressed in specific cytogenetic (MLL rearrangements and monosomy 7) and morphologic (FAB-M6/7) subtypes. However, the typical EVI1+ associated 3q26 aberrations reported in adult AML were not identified, indicating that there may be a difference for the role of EVI1+ in adult AML as compared with pediatric AML. Although EVI1+ was not an independent prognostic factor, it was predominantly found in types of pediatric AML that are related with an intermediate to unfavorable prognosis, for example MLL-AF6 and monosomy 7. This underscores the need for further studies to identify the biological role of EVI1 in the pathogenesis of childhood leukemia.
References
Wieser R . The oncogene and developmental regulator EVI1: expression, biochemical properties, and biological functions. Gene 2007; 396: 346–357.
Morishita K, Parganas E, William CL, Whittaker MH, Drabkin H, Oval J et al. Activation of EVI1 gene expression in human acute myelogenous leukemias by translocations spanning 300-400 kilobases on chromosome band 3q26. Proc Natl Acad Sci USA 1992; 89: 3937–3941.
Matsugi T, Morishita K, Ihle JN . Identification, nuclear localization, and DNA-binding activity of the zinc finger protein encoded by the Evi-1 myeloid transforming gene. Mol Cell Biol 1990; 10: 1259–1264.
Hoyt PR, Bartholomew C, Davis AJ, Yutzey K, Gamer LW, Potter SS et al. The Evi1 proto-oncogene is required at midgestation for neural, heart, and paraxial mesenchyme development. Mech Dev 1997; 65: 55–70.
Morishita K, Parker DS, Mucenski ML, Jenkins NA, Copeland NG, Ihle JN . Retroviral activation of a novel gene encoding a zinc finger protein in IL-3-dependent myeloid leukemia cell lines. Cell 1988; 54: 831–840.
Nucifora G, Laricchia-Robbio L, Senyuk V . EVI1 and hematopoietic disorders: history and perspectives. Gene 2006; 368: 1–11.
Spensberger D, Delwel R . A novel interaction between the proto-oncogene Evi1 and histone methyltransferases, SUV39H1 and G9a. FEBS Lett 2008; 582: 2761–2767.
Cattaneo F, Nucifora G . EVI1 recruits the histone methyltransferase SUV39H1 for transcription repression. J Cell Biochem 2008; 105: 344–352.
Aytekin M, Vinatzer U, Musteanu M, Raynaud S, Wieser R . Regulation of the expression of the oncogene EVI1 through the use of alternative mRNA 5′-ends. Gene 2005; 356: 160–168.
Fears S, Mathieu C, Zeleznik-Le N, Huang S, Rowley JD, Nucifora G . Intergenic splicing of MDS1 and EVI1 occurs in normal tissues as well as in myeloid leukemia and produces a new member of the PR domain family. Proc Natl Acad Sci USA 1996; 93: 1642–1647.
Huang S, Shao G, Liu L . The PR domain of the Rb-binding zinc finger protein RIZ1 is a protein binding interface and is related to the SET domain functioning in chromatin-mediated gene expression. J Biol Chem 1998; 273: 15933–15939.
Barjesteh van Waalwijk van Doorn-Khosrovani S, Erpelinck C, van Putten WL, Valk PJ, van der Poel-van de Luytgaarde S, Hack R et al. High EVI1 expression predicts poor survival in acute myeloid leukemia: a study of 319 de novo AML patients. Blood 2003; 101: 837–845.
Lugthart S, van Drunen E, van Norden Y, van Hoven A, Erpelinck CA, Valk PJ et al. High EVI1 levels predict adverse outcome in acute myeloid leukemia: prevalence of EVI1 overexpression and chromosome 3q26 abnormalities underestimated. Blood 2008; 111: 4329–4337.
Raimondi SC, Chang MN, Ravindranath Y, Behm FG, Gresik MV, Steuber CP et al. Chromosomal abnormalities in 478 children with acute myeloid leukemia: clinical characteristics and treatment outcome in a cooperative pediatric oncology group study-POG 8821. Blood 1999; 94: 3707–3716.
Vardiman JW, Harris NL, Brunning RD . The World Health Organization (WHO) classification of the myeloid neoplasms. Blood 2002; 100: 2292–2302.
Kardos G, Zwaan CM, Kaspers GJ, de-Graaf SS, de Bont ES, Postma A et al. Treatment strategy and results in children treated on three Dutch Childhood Oncology Group acute myeloid leukemia trials. Leukemia 2005; 19: 2063–2071.
Gibson BE, Wheatley K, Hann IM, Stevens RF, Webb D, Hills RK et al. Treatment strategy and long-term results in paediatric patients treated in consecutive UK AML trials. Leukemia 2005; 19: 2130–2138.
Creutzig U, Zimmermann M, Ritter J, Reinhardt D, Hermann J, Henze G et al. Treatment strategies and long-term results in paediatric patients treated in four consecutive AML-BFM trials. Leukemia 2005; 19: 2030–2042.
Den Boer ML, Harms DO, Pieters R, Kazemier KM, Gobel U, Korholz D et al. Patient stratification based on prednisolone-vincristine-asparaginase resistance profiles in children with acute lymphoblastic leukemia. J Clin Oncol 2003; 21: 3262–3268.
Van Vlierberghe P, van Grotel M, Beverloo HB, Lee C, Helgason T, Buijs-Gladdines J et al. The cryptic chromosomal deletion del(11)(p12p13) as a new activation mechanism of LMO2 in pediatric T-cell acute lymphoblastic leukemia. Blood 2006; 108: 3520–3529.
Balgobind BV, Van Vlierberghe P, van den Ouweland AM, Beverloo HB, Terlouw-Kromosoeto JN, van Wering ER et al. Leukemia-associated NF1 inactivation in patients with pediatric T-ALL and AML lacking evidence for neurofibromatosis. Blood 2008; 111: 4322–4328.
Yamamoto Y, Kiyoi H, Nakano Y, Suzuki R, Kodera Y, Miyawaki S et al. Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies. Blood 2001; 97: 2434–2439.
Kiyoi H, Naoe T, Yokota S, Nakao M, Minami S, Kuriyama K et al. Internal tandem duplication of FLT3 associated with leukocytosis in acute promyelocytic leukemia. Leukemia Study Group of the Ministry of Health and Welfare (Kohseisho). Leukemia 1997; 11: 1447–1452.
Barjesteh van Waalwijk van Doorn-Khosrovani S, Erpelinck C, Meijer J, van Oosterhoud S, van Putten WL, Valk PJ et al. Biallelic mutations in the CEBPA gene and low CEBPA expression levels as prognostic markers in intermediate-risk AML. Hematol J 2003; 4: 31–40.
Hollink IH, Zwaan CM, Zimmermann M, Arentsen-Peters TC, Pieters R, Cloos J et al. Favorable prognostic impact of NPM1 gene mutations in childhood acute myeloid leukemia, with emphasis on cytogenetically normal AML. Leukemia 2009; 23: 262–270.
Balgobind BV, Hollink IHIM, Reinhardt D, van Wering ER, de Graaf SSN, Baruchel A et al. Low frequency of MLL-PTD detected in pediatric acute myeloid leukemia using MLPA screening. ASH Annual Meet Abstr 2008; 112: 1512.
Irizarry RA, Gautier L, Bolstad BM, Miller C, Astrand M, Cope LM et al. Affy: methods for affymetrix oligonucleotide arrays. Part of Bioconducter, http://www.bioconducter.org.
Huber W, von Heydebreck A, Sultmann H, Poustka A, Vingron M . Variance stabilization applied to microarray data calibration and to the quantification of differential expression. Bioinformatics (Oxford, England) 2002; 18 (Suppl 1): S96–S104.
Team RDC. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2007.
Smyth G . Linear models and empirical Bayes methods for assessing differential expression in microarray experiments. Stat Appl Genet Mol Biol 2004; 3: 1.
Benjamini Y, Hochberg Y . Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc B Met 1995; 57: 289–300.
Meijerink J, Mandigers C, van de Locht L, Tonnissen E, Goodsaid F, Raemaekers J . A novel method to compensate for different amplification efficiencies between patient DNA samples in quantitative real-time PCR. J Mol Diagn 2001; 3: 55–61.
Lu Q, Wright DD, Kamps MP . Fusion with E2A converts the Pbx1 homeodomain protein into a constitutive transcriptional activator in human leukemias carrying the t(1;19) translocation. Mol Cell Biol 1994; 14: 3938–3948.
Kuo YH, Zaidi SK, Gornostaeva S, Komori T, Stein GS, Castilla LH . Runx2 induces acute myeloid leukemia in cooperation with Cbfbeta-SMMHC in mice. Blood 2009; 113: 3323–3332.
Laricchia-Robbio L, Nucifora G . Significant increase of self-renewal in hematopoietic cells after forced expression of EVI1. Blood Cells Mol Dis 2008; 40: 141–147.
Kilbey A, Stephens V, Bartholomew C . Loss of cell cycle control by deregulation of cyclin-dependent kinase 2 kinase activity in Evi-1 transformed fibroblasts. Cell Growth Differ 1999; 10: 601–610.
Hasle H, Alonzo TA, Auvrignon A, Behar C, Chang M, Creutzig U et al. Monosomy 7 and deletion 7q in children and adolescents with acute myeloid leukemia: an international retrospective study. Blood 2007; 109: 4641–4647.
Barnard DR, Alonzo TA, Gerbing RB, Lange B, Woods WG . Comparison of childhood myelodysplastic syndrome, AML FAB M6 or M7, CCG 2891: report from the Children's Oncology Group. Pediatr Blood Cancer 2007; 49: 17–22.
Gilliland DG, Griffin JD . The roles of FLT3 in hematopoiesis and leukemia. Blood 2002; 100: 1532–1542.
Goemans BF, Zwaan CM, Miller M, Zimmermann M, Harlow A, Meshinchi S et al. Mutations in KIT and RAS are frequent events in pediatric core-binding factor acute myeloid leukemia. Leukemia 2005; 19: 1536–1542.
Chen W, Kumar AR, Hudson WA, Li Q, Wu B, Staggs RA et al. Malignant transformation initiated by Mll-AF9: gene dosage and critical target cells. Cancer Cell 2008; 13: 432–440.
Tonnies H, Huber S, Kuhl JS, Gerlach A, Ebell W, Neitzel H . Clonal chromosomal aberrations in bone marrow cells of Fanconi anemia patients: gains of the chromosomal segment 3q26q29 as an adverse risk factor. Blood 2003; 101: 3872–3874.
Balgobind BV, Raimondi SC, Harbott J, Zimmermann M, Alonzo TA, Auvrignon A et al. Novel prognostic subgroups in childhood 11q23/MLL-rearranged acute myeloid leukemia: results of an international retrospective study. Blood 2009; 114: 2489–2496.
Laricchia-Robbio L, Fazzina R, Li D, Rinaldi CR, Sinha KK, Chakraborty S et al. Point mutations in two EVI1 Zn fingers abolish EVI1-GATA1 interaction and allow erythroid differentiation of murine bone marrow cells. Mol Cell Biol 2006; 26: 7658–7666.
Kreider BL, Orkin SH, Ihle JN . Loss of erythropoietin responsiveness in erythroid progenitors due to expression of the Evi-1 myeloid-transforming gene. Proc Natl Acad Sci USA 1993; 90: 6454–6458.
Shimizu S, Nagasawa T, Katoh O, Komatsu N, Yokota J, Morishita K . EVI1 is expressed in megakaryocyte cell lineage and enforced expression of EVI1 in UT-7/GM cells induces megakaryocyte differentiation. Biochem Biophys Res Commun 2002; 292: 609–616.
Louz D, van den Broek M, Verbakel S, Vankan Y, van Lom K, Joosten M et al. Erythroid defects and increased retrovirally-induced tumor formation in Evi1 transgenic mice. Leukemia 2000; 14: 1876–1884.
Valk PJ, Verhaak RG, Beijen MA, Erpelinck CA, Barjesteh van Waalwijk van Doorn-Khosrovani S, Boer JM et al. Prognostically useful gene-expression profiles in acute myeloid leukemia. N Engl J Med 2004; 350: 1617–1628.
Lugthart S, Figueroa ME, Valk PJM, Li Y, Erpelinck-Verschueren C, Greally J et al. Two different EVI1 expressing poor-risk AML subgroups with Distinct epigenetic signatures uncovered by genome wide DNA methylation profiling. ASH Annual Meet Abstr 2008; 112: 757.
Shimabe M, Goyama S, Watanabe-Okochi N, Yoshimi A, Ichikawa M, Imai Y et al. Pbx1 is a downstream target of Evi-1 in hematopoietic stem/progenitors and leukemic cells. Oncogene 2009; 28: 4364–4374.
Acknowledgements
This work was funded by the NWO ‘Netherlands Organization for Scientific Research’ (BVB), KOCR ‘Kinder-Oncologisch Centrum Rotterdam’ (BVB and IHH) and EHA (SL).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contribution
BVB designed and performed research and wrote the paper. SL and RD designed research. IHH designed and performed research. HBB performed FISH analysis. EW, SSNG, GJK, DR, UC, JS, and JT made this research possible by collecting patient samples and characteristics in their own study groups and providing additional information. MMH-E, CMZ, and RP designed and supervised research and wrote the paper.
Supplementary Information accompanies the paper on the Leukemia website
Rights and permissions
About this article
Cite this article
Balgobind, B., Lugthart, S., Hollink, I. et al. EVI1 overexpression in distinct subtypes of pediatric acute myeloid leukemia. Leukemia 24, 942–949 (2010). https://doi.org/10.1038/leu.2010.47
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2010.47
Keywords
This article is cited by
-
EVI1 expression in early-stage breast cancer patients treated with neoadjuvant chemotherapy
BMC Cancer (2022)
-
Myeloid leukemia with high EVI1 expression is sensitive to 5-aza-2′-deoxycytidine by targeting miR-9
Clinical and Translational Oncology (2020)
-
A critical role of epigenetic inactivation of miR-9 in EVI1high pediatric AML
Molecular Cancer (2019)
-
High expression of EVI1 and MEL1 is a compelling poor prognostic marker of pediatric AML
Leukemia (2015)
-
−7/7q− syndrome in myeloid-lineage hematopoietic malignancies: attempts to understand this complex disease entity
Oncogene (2015)