Abstract
Bone marrow DNA was screened for isocitrate dehydrogenase (IDH) mutations in 200 patients with chronic (n=166) or blast (n=34) phase myeloproliferative neoplasms (MPN). Included among the former were 77 patients with primary myelofibrosis (PMF), 47 essential thrombocythemia and 38 polycythemia vera (PV). Nine IDH mutations (5 IDH1 and 4 IDH2) were detected; mutational frequencies were ∼21% (7 of 34) for blast-phase MPN and ∼4% (3 of 77) for PMF. IDH mutations were seen in only 1 of 12 paired chronic-blast-phase samples and in none of 27 concurrently studied acute myeloid leukemia (AML) patients without antecedent MPN. IDH1 mutations included R132C (n=4; two post-PMF AML, one post-PV AML and one PMF) and R132S (n=1; post-PMF AML). IDH2 mutations included R140Q (n=3; one post-PMF AML, one post-PV AML and one PMF) and a novel R140W (n=1; mutation found in both chronic- and blast-phase samples). The entire study cohort was also screened for JAK2 and MPL mutations and JAK2V617F was found in three IDH-mutated cases (two PMF and one PV). This study shows a relatively high incidence of IDH mutations in blast-phase MPN, regardless of JAK2 mutational status, and the occurrence of similar mutations in chronic-phase PMF.
Similar content being viewed by others
Introduction
An initial genome-wide screen using glioblastoma multiforme tumor tissue identified point mutations within the isocitrate dehydrogenase 1 (IDH1) gene in 12% of cases.1 These findings were confirmed and extended in a subsequent study wherein 445 central nervous system and 494 non-central nervous system tumors were screened for mutations in exon 4 of IDH1 and, in noninformative cases, of IDH2.2 Mutations involving residue 132 of IDH1 were identified in more than 70% of World Health Organization grade II and III astrocytomas and oligodendrogliomas, and in glioblastomas developing from these lower-grade lesions. Tumors without mutations in IDH1 often had mutations affecting the analogous amino acid (R172) of the IDH2 gene. In this study, the median survival of adult patients with the aforementioned tumor types and mutated IDH1 or IDH2 was significantly longer than those with wild-type IDH genes. In contrast to gliomas, IDH mutations appear to be a rare occurrence in other solid tumors.2, 3, 4
Recently, mutations involving R132 of IDH1 (but not R172 of IDH2) were identified in 9% of primary acute myeloid leukemia (AML) patients, and were found to co-segregate with cytogenetically normal samples (16%).5 Similarly, in another study of 493 adult patients with de novo AML who were screened for R132 IDH1 mutations, 6% tested positive; these mutations co-segregated with normal karyotype or isolated trisomy 8, presence of NPM1 mutations and FAB M1 AML subtype.6 However, in another study of 78 AML patients, the prevalence of IDH1 and IDH2 mutations was 8 and 12%, respectively.7 Again, the mutations were restricted to normal karyotype AML, and the most frequent allele was R140Q IDH2, which did not co-segregate with FLT-3, NPM1 or ASXL1 mutations.
There is relatively scant data regarding the prevalence of IDH mutations in other hematological malignancies. In a recent small study of blast/leukemic phase of preexisting JAK2 mutation-positive myeloproliferative neoplasms (MPN), 5 of 16 patients (31%) were found to harbor IDH mutations.8 Of these, three patients harbored the previously described R132C IDH1 mutation, whereas two carried R140Q IDH2 mutation. In contrast, none of 180 other patients with chronic-phase polycythemia vera (PV) or essential thrombocythemia (ET) harbored IDH mutations. IDH mutation status during chronic-phase MPN was not reported for the patients whose leukemic blasts were IDH mutation positive; instead the identification of R140Q IDH2 in both erythroid colonies and leukemic blasts for one patient suggested that IDH mutations arise early during the disease course.
In this study, we report on IDH1 and IDH2 mutation analysis in a relatively large cohort of MPN patients, including a subset (n=12) for whom paired chronic- and blast-phase samples were available, with the following goals: (1) to describe the prevalence of IDH mutations in chronic-phase MPN, particularly primary myelofibrosis (PMF), which has hitherto not been studied; (2) to describe the clinical, cytogenetic, and JAK2 and MPL mutation correlates of IDH mutations and (3) to define the relationship of IDH mutation acquisition and leukemic transformation of MPN, through the study of paired sequential samples.
Materials and methods
This study was approved by the Mayo Clinic Institutional Review Board. All patients provided authorization for the use of their medical records for research purposes, and research was carried out according to the Declaration of Helsinki Principles. We used the Mayo Clinic database of adult MPN and AML patients (age ⩾18 years) to identify consecutive patients in whom stored peripheral blood or bone marrow cells were available for DNA extraction. Clinical data and bone marrow histology were reviewed and the hematological diagnosis confirmed to the 2008 World Health Organization proposal.9 DNA was extracted using DNA Mini Extraction Kit (Qiagen, Santa Clarita, CA, USA).
The primer sequences used to amplify IDH1 exon 4 were: 5′-CGGTCTTCAGAGAAGCCATT-3′ (sense), and 5′-CACATTATTGCCAACATGAC-3′ (anti-sense) as previously described.10 IDH2 exon 4 was amplified using 5′-CCACTATTATCTCTGTCCTC-3′ (sense) and 5′-GCTAGGCGAGGAGCTCCAGT-3′ (anti-sense).11 Briefly, both reactions were performed in 25 μl volume containing 100 ng of DNA, 0.25 U Taq polymerase, 0.3 mM each of dATP, dCTP, dGTP and dTTP, 5 μL of a 10 × PCR Buffer (Roche Diagnostics, Indianapolis, IN, USA), and 0.2 μM each of sense and anti-sense primers. The reaction was denatured at 94 °C for 3 min followed by 35 cycles of denaturing at 94 °C for 30 s, annealing at 57 °C for 30 s and extension at 72 °C for 40 s. After a final extension at 72 °C for 2 min the products were confirmed by 1.3% agarose gel and purified using PCR Quick Purification Kit (Qiagen). The product was sequenced using the ABI PRISM 3730xl Analyzer (Applied Biosystems Inc., Foster City, CA, USA) to screen for the presence of mutations. The LightCycler 480 Real-Time PCR System (Roche Diagnostics) and its high-resolution melting master reagents were used to perform LightCycler PCR and high-resolution melting (HRM) analysis to explore its use in detecting IDH1 mutations using the above-mentioned primers, as per manufacturer's instructions.
Primers and probes for MPL analysis were used as previously described.12 Briefly, two qPCR master mixes were created each containing 200 ng DNA, 1 × TaqMan Universal PCR Master Mix (Applied Biosystems, Framingham, MA, USA), 400 nM forward and reverse primers, W515WT-MGB-Probe (100 nM) and one of either W515L-MGB-Probe (200 nM) or W515K-MGB-Probe (300 nM). The reactions were set up in triplicate and qPCR was performed by standard quantification protocol using ABI PRISM 7900HT real-time instrumentation. The mean of the cycle threshold fluorescent determinants was calculated (Ct W515L/K – Ct W515WT) and the percent of mutant allele burden was compared with a reference standard curve of either heterozygous mutant W515L or W515K spiked with normal DNA. The mean of the Ct determinants (Ct MPL W515L/K – Ct MPL WT) was calculated and positively flagged samples were sequenced for confirmation. Assay sensitivity using this standard curve was accurate to 1:16 of spiked HET W515L and 1:8 of spiked HET W515K.
The JAK2V617F allele burden assay was performed using DNA from bone-marrow-derived cells according to previously reported methods.13
Results
We studied 227 patients for mutations in exons 4 of IDH1 and IDH2, including 81 with myelofibrosis (PMF=77, post-PV MF=2, post-ET MF=2), 47 ET, 38 PV and 34 with blast-phase MPN. Our data set also included 27 patients with AML without history of MPN (AML with myelodysplasia-related changes=9; AML, not otherwise specified=18). In other words, among the 61 AML patients studied, 34 had antecedent MPN including 20 post-PMF, 7 post-ET, 6 post-PV and 1 post-MPN-unclassified AML (Tables 1 and 2). In addition, paired serial samples from chronic- and blast-phase MPN were available for 12 patients (Table 1).
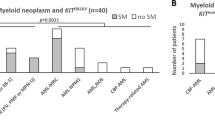
In the overall cohort of 227 patients, 9 (4%) harbored a mutation in exon 4 of either IDH1 (n=5) or IDH2 (n=4) (Figure 1). Mutational frequencies were ∼21% (7 of 34) for blast-phase MPN, ∼4% (3 of 77) for PMF and no mutations were detected in the other disease categories. Furthermore, among the seven IDH-mutated cases of blast-phase MPN, the antecedent MPN was PMF in five cases and PV in two. All the IDH1 mutations were previously described missense mutations involving R132 (R132C=4 and R132S=1). The four IDH2 mutations were missense mutations that were restricted to R140; three cases carried the previously described R140Q whereas one harbored a novel R140W mutation.
(A) DNA sequence traces showing nucleotide substitutions in the IDH1 gene and consequent amino-acid changes in the IDH1 protein, in patients with post-primary myelofibrosis acute myeloid leukemia (post-PMF AML; panels a, c and e), post-polycythemia AML (post-PV AML; panel d) and PMF (panel b). (B) DNA sequence traces showing nucleotide substitutions in the IDH2 gene and consequent amino-acid changes in the IDH2 protein, in patients with post-PMF AML (panels a and c), post-PV AML (panel b) and PMF (panel d). For the patient shown in a, samples were available at chronic phase and leukemic phase; both samples were found to harbor the IDH2R140W mutation.
In terms of clinical and molecular correlates of IDH1 mutations, three patients with R132C mutations (B13, B14 and B19; Table 2) had blast-phase MPN (two and one each with antecedent PMF and PV, respectively) and one had PMF; patient B19 (with antecedent PV) expectedly carried the JAK2V617F mutation; none of the patients harbored an MPL exon 10 mutation. The only patient with R132S had blast-phase MPN with antecedent PMF and concurrently harbored the JAK2V617F mutation at high allele burden (JAK2 mutant/wild-type ratio 96%). As to IDH2 mutations, three patients had blast-phase MPN, one with R140W (antecedent PMF; A4 Table 1), two with R140Q (antecedent PV and PMF for B3 and B22, respectively; Table 2). The remaining patient harbored R140Q IDH2 mutation, and had PMF. Only one patient (A4; Table 1) with an IDH2 mutation (R140W) harbored the JAK2V617F mutation concurrently; interestingly, both mutations could be identified in both chronic- (that is, PMF) and blast-phase samples in this particular instance; furthermore the JAK2V617F allele burden was remarkably stable in the serial samples.
Consistent with previous studies, the observed IDH mutations were heterozygous in every instance in this study (Figures 1A and B). Finally, for future practical purposes, we explored the use of HRM curve analysis in detecting IDH1 mutations and all five IDH1 mutations detected by direct nucleotide sequencing were also picked up by HRM analysis (Figure 2).
The high-resolution DNA melting (HRM) curve analysis is a high-throughput analysis for mutations in exon 4 of IDH1 and IDH2; the top left panel shows a schematic of the plate format and well location of a sample harboring the IDH1R132C mutation; the top right panel shows the negative derivative of the melting curve allowing visualization of the sample harboring IDH1R132C; the bottom panel shows the sequence trace of the sample flagged by HRM analysis and confirmed to carry IDH1R132C by direct sequencing.
Discussion
IDH1 and IDH2 catalyze the oxidative decarboxylation of isocitrate to α-ketoglutarate thereby generating NADPH from NADP+ as part of the citric acid cycle in the cytosol/peroxisomes and mitochondria, respectively. To date, all cases of IDH mutations have been heterozygous, and involve evolutionarily conserved Arg residues that normally form hydrogen bonds with the isocitrate substrate;14 furthermore, there is no reported instance of concurrent IDH1and IDH2 mutations. Functional characterization suggests that IDH mutations lead to depletion of cellular α-ketoglutarate with downstream activation of the oncogenic HIF-1α pathway.15 Other studies have reported an R132 IDH1 and an R172 IDH2 mutation-associated gain of function in catalyzing NADPH-dependent reduction of α-ketoglutarate to the (R) enantiomer of 2-hydroxyglutarate (2-HG); excess accumulation of 2-HG has been shown in both glioma and AML and is thought to contribute to oncogenesis.7, 16, 17
In this study, IDH mutations were identified in 21% of patients with either post-PMF or post-PV AML and also not infrequently (prevalence ∼4%) in patients with chronic-phase PMF. Although we did not identify IDH mutations in the current cohort of AML patients without antecedent MPN or patients with chronic phase PV or ET, the number of patients studied was too small to allow any conclusion in this regard. However, it is reasonable to conclude, based on this and other similar studies, that IDH mutations are relatively frequent in post-MPN AML and that their incidence in the particular setting is probably higher than that of either chronic-phase MPN or primary AML.
We noted a slight preponderance of IDH1 relative to IDH2 mutations, a pattern also seen in a previous small study of blast-phase MPN patients.8 We failed to detect any mutation involving residue R172 of IDH2; this observation is consistent with some studies,5, 8 but not others,7 of AML patients; however, the small number of patients involving heterogeneous groups (i.e., de novo AML vs blast-phase MPN) in these studies makes it difficult to draw any definitive conclusions in this regard. All three IDH-mutated patients with chronic-phase MPN had PMF, and mutations were detected in both IDH1 (R132C; n=1) and IDH2 (one each with R140Q and R140W).
Within the blast-phase MPN and PMF subgroups wherein IDH mutations were identified, there were no particular disease characteristics that segregated with mutation-positive patients, as compared with the mutation-negative patients; specifically, there was no discernible link between presence of the mutation and either duration of disease, or a particular antecedent treatment or cytogenetic abnormality. In our cohort, a third of patients (n=3), all with blast-phase MPN, concurrently harbored an IDH mutation and JAK2V617F; two patients had antecedent PMF and one patient antecedent PV. Incidentally, in one patient with antecedent PMF (B20; Table 2), a very high JAK2V617 allele burden (96%), was noted; it can be safely predicted that R132S IDH1 and JAK2V617 coexisted in the same clone in this patient. In the other patient with antecedent PMF (A4; Table 1), both mutations (R140W IDH2 and JAK2V617F) were detected not only in the leukemic sample but also in the chronic-phase sample that was collected 9 months earlier (Figure 1b); the mutant allele burden for both mutations was relatively constant in the paired specimens (in the case of R140W IDH2, being inferred through peak size on the chromatogram traces), arguing that leukemic transformation occurred through acquisition of additional genetic events in the clone that harbored both mutations in chronic phase.
There are several inferences that can be drawn from the aforementioned observations. First, IDH mutations are relatively rare in chronic-phase MPN, and when seen, appear to be restricted to PMF patients. In contrast, a significant proportion (∼20%) of blast-phase MPN patients harbored IDH mutations; this mutation frequency is higher than previously reported for AML without antecedent MPN, although confirmation in a larger cohort of blast-phase MPN patients will be important. Second, a majority of IDH mutation-positive patients did not concurrently harbor JAK2V617F; thus, although both mutations can occur concurrently in a given patient, and even possibly in the same clone, it appears that, in general, IDH mutations emerge independently of JAK2V617F, although confirmation of this point will require study of larger numbers of MPN patients with IDH mutations.
Third, we have shown that IDH mutations are not only restricted to blast-phase MPN, but also detected at low frequency in chronic-phase disease (that is, PMF). This argues that IDH mutations can emerge relatively early in MPN development and is consistent with our inability to show the acquisition of IDH mutations during leukemic transformation of 11 patients in whom paired chronic-blast-phase MPN samples were available. Instead, the mutation was present in both chronic- and blast-phase diseases in the only IDH-mutated patient with paired samples. These observations suggest the possibility that IDH mutations in MPN represent early genetic events that might facilitate leukemic transformation. Such a scenario would be similar to that seen in gliomas where IDH1 mutations are found at high frequency in secondary glioblastomas (that is, those developing from lower-grade lesions), and in one study, IDH1 mutations were identified in both the low- and high-grade tumors in all glioma cases where paired specimens were available.2 Furthermore, IDH mutations co-segregated with TP53 mutations in anaplastic astrocytomas and glioblastomas, but not with other early genetic alterations such as PTEN mutations, EGFR amplifications, or deletions of CDKN2A or CDKN2B. Thus IDH mutations in MPN, as in gliomas, can represent early genetic events during disease development.
References
Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, Angenendt P et al. An integrated genomic analysis of human glioblastoma multiforme. Science 2008; 321: 1807–1812.
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med 2009; 360: 765–773.
Bleeker FE, Lamba S, Leenstra S, Troost D, Hulsebos T, Vandertop WP et al. IDH1 mutations at residue p.R132 (IDH1(R132)) occur frequently in high-grade gliomas but not in other solid tumors. Hum Mutat 2009; 30: 7–11.
Park SW, Chung NG, Han JY, Eom HS, Lee JY, Yoo NJ et al. Absence of IDH2 codon 172 mutation in common human cancers. Int J Cancer 2009; 125: 2485–2486.
Mardis ER, Ding L, Dooling DJ, Larson DE, McLellan MD, Chen K et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med 2009; 361: 1058–1066.
Chou WC, Hou HA, Chen CY, Tang JL, Yao M, Tsay W et al. Distinct clinical and biological characteristics in adult acute myeloid leukemia bearing isocitrate dehydrogenase 1 (IDH1) mutation. Blood 2010; 115: 2749–2754.
Ward PS, Patel J, Wise DR, Abdel-Wahab O, Bennett BD, Coller HA et al. The common feature of leukemia-associated IDH1 and IDH2 mutations is a neomorphic enzyme activity converting alpha-ketoglutarate to 2-hydroxyglutarate. Cancer Cell 2010; 17: 225–234.
Green A, Beer P . Somatic mutations of IDH1 and IDH2 in the leukemic transformation of myeloproliferative neoplasms. N Engl J Med 2010; 362: 369–370.
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 2009; 114: 937–951.
Watanabe T, Nobusawa S, Kleihues P, Ohgaki H . IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol 2009; 174: 1149–1153.
Nobusawa S, Watanabe T, Kleihues P, Ohgaki H . IDH1 mutations as molecular signature and predictive factor of secondary glioblastomas. Clin Cancer Res 2009; 15: 6002–6007.
Ruan GR, Jiang B, Li LD, Niu JH, Li JL, Xie M et al. MPL W515L/K mutations in 343 Chinese adults with JAK2V617F mutation-negative chronic myeloproliferative disorders detected by a newly developed RQ-PCR based on TaqMan MGB probes. Hematol Oncol 2009; 28: 33–39.
Tefferi A, Lasho TL, Huang J, Finke C, Mesa RA, Li CY et al. Low JAK2V617F allele burden in primary myelofibrosis, compared to either a higher allele burden or unmutated status, is associated with inferior overall and leukemia-free survival. Leukemia 2008; 22: 756–761.
Xu X, Zhao J, Xu Z, Peng B, Huang Q, Arnold E et al. Structures of human cytosolic NADP-dependent isocitrate dehydrogenase reveal a novel self-regulatory mechanism of activity. J Biol Chem 2004; 279: 33946–33957.
Zhao S, Lin Y, Xu W, Jiang W, Zha Z, Wang P et al. Glioma-derived mutations in IDH1 dominantly inhibit IDH1 catalytic activity and induce HIF-1alpha. Science 2009; 324: 261–265.
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature 2009; 462: 739–744.
Gross S, Cairns RA, Minden MD, Driggers EM, Bittinger MA, Jang HG et al. Cancer-associated metabolite 2-hydroxyglutarate accumulates in acute myelogenous leukemia with isocitrate dehydrogenase 1 and 2 mutations. J Exp Med 2010; 207: 339–344.
Acknowledgements
AP was partially supported by a research grant from the Henry J Predolin Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pardanani, A., Lasho, T., Finke, C. et al. IDH1 and IDH2 mutation analysis in chronic- and blast-phase myeloproliferative neoplasms. Leukemia 24, 1146–1151 (2010). https://doi.org/10.1038/leu.2010.77
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2010.77
Keywords
This article is cited by
-
Digital-droplet PCR assays for IDH, DNMT3A and driver mutations to monitor after allogeneic stem cell transplantation minimal residual disease of myelofibrosis
Bone Marrow Transplantation (2022)
-
Acute myeloid leukemia with isolated del(5q) is associated with IDH1/IDH2 mutations and better prognosis when compared to acute myeloid leukemia with complex karyotype including del(5q)
Modern Pathology (2020)
-
Philadelphia-Negative Myeloproliferative Neoplasms: Laboratory Workup in the Era of Next-Generation Sequencing
Current Hematologic Malignancy Reports (2019)
-
Blast phase myeloproliferative neoplasm: Mayo-AGIMM study of 410 patients from two separate cohorts
Leukemia (2018)
-
Impact of PCR-based molecular analysis in daily diagnosis for the patient with gliomas
Brain Tumor Pathology (2018)