Abstract
Breast cancer is a chief cause of cancer-related mortality that affects women worldwide. About 8% of cases are hereditary, and approximately half of these are associated with germline mutations of the breast tumor suppressor gene BRCA1 (refs. 1,2). We have previously reported a mouse model in which Brca1 exon 11 is eliminated in mammary epithelial cells through Cre-mediated excision3. This mutation is often accompanied by alterations in transformation-related protein 53 (Trp53, encoding p53), which substantially accelerates mammary tumor formation. Here, we sought to elucidate the underlying mechanism(s) using mice deficient in the Brca1 exon 11 isoform (Brca1Δ11/Δ11). Brca1Δ11/Δ11 embryos died late in gestation because of widespread apoptosis. Unexpectedly, elimination of one Trp53 allele completely rescues this embryonic lethality and restores normal mammary gland development. However, most female Brca1Δ11/Δ11 Trp53+/− mice develop mammary tumors with loss of the remaining Trp53 allele within 6–12 months. Lymphoma and ovarian tumors also occurr at lower frequencies. Heterozygous mutation of Trp53 decreases p53 and results in attenuated apoptosis and G1–S checkpoint control, allowing Brca1Δ11/Δ11 cells to proliferate. The p53 protein regulates Brca1 transcription both in vitro and in vivo, and Brca1 participates in p53 accumulation after γ-irradiation through regulation of its phosphorylation and Mdm2 expression. These findings provide a mechanism for BRCA1-associated breast carcinogenesis.
Similar content being viewed by others
Main
We generated mice heterozygous for the deletion of exon 11 (Brca1+/Δ11) by crossing mice with a 'floxed' Brca1 exon 11 (ref. 3) with mice transgenic for EIIa–Cre (adenovirus early transcription region IIa promoter-Cre.) (ref. 4), which express Cre in germ cells (Fig. 1). After intercrossing Brca1+/Δ11 mice, we found 3 of 215 newborns dead. All three were Brca1Δ11/Δ11, whereas all live mice were either wild type or Brca1+/Δ11 at a ratio of about 1 to 2. This indicates that deletion of Brca1 exon 11 results in recessive embryonic lethality, although a very small number survived. We dissected embryos obtained on different gestational days to determine the timing of this Brca1Δ11/Δ11 lethality. At embryonic days 9.5–11.5 (E9.5–11.5), we found 14 Brca1Δ11/Δ11 embryos among 71 dissected deciduas. Four were morphologically indistinguishable from their wildtype and heterozygous littermate controls, whereas the rest were smaller (Fig. 2a). From E12.5, all mutant embryos (n=33) were either smaller or abnormal, indicating that the loss of exon 11 began to severely affect embryonic development at this time. About 10% of mutant embryos showed exencephaly (Fig. 2b–d), and more than half showed a sac-like structure on their backs with empty spaces of varying sizes (Fig. 2e,f). Mutant wildtype skin was relatively normal, but the muscle tissue underneath the skin was mostly absent (Fig. 2f,h). In wild-type embryos, northern blot analysis demonstrated transcripts of approximately 7.2 kb (full-length) and 3.9 kb (lacking exon 11). In Brca1Δ11/Δ11 embryos, the full-length transcripts were absent (Fig. 1d). The intensity of the bands representing transcripts lacking exon 11 was increased, perhaps because all transcripts from exon 10 were directly spliced into exon 12. The presence of these transcripts may account for the extended survival of the Brca1Δ11/Δ11 embryos.
a, Brca1 structure: wildtype allele (upper) and a 'conditional' allele (lower). The Brca1 'conditional' allele contains two loxP sites, which were placed into intron 10 at an XbaI site (Xb) and intron 11 at an EcoRI site (Ec), respectively. Ev, EcoRV; Xh, XhoI. b, Deletion of exon 11 of Brca1 from mouse germ line by crossing with EIIa–Cre mice. c, Southern blot analysis, showing DNA from E14.5 Brca1Δ11/Δ11 (lanes 1 and 2), Brca1+/Δ11 (lane 3) and wildtype (lane 4) embryos. DNA digested with XbaI (Xb) was incubated with a 0.7-kb XhoI–EcoRI probe. The wildtype (9.5 kb) and deletion (3.5 kb) alleles are indicated. d, Northern blot analysis, showing RNA isolated from E14.5 wild-type and Brca1Δ11/Δ11 embryos. Poly-A RNA (5 μg) was hybridized with a 509-bp cDNA probe containing exons 10 and 12. Gapdh, hybridization to a glyceraldehyde phosphodehydrogenase probe (loading control).
a, E10.5 embryos. The mutant embryo (left) seems normal except that it is much smaller than the littermate control (right). b,c, Exencephaly in E14.5 (b) and E16.5 (c) mutant embryos. d, An E16.5 control embryo. e, E14.5 embryos. The arrow indicates a sac-like structure in the mutant embryo (left), which is not present in the control embryo (right). f, Saggital section through the sac-like structure of the mutant embryo shown in e. Body muscle is absent under the skin, which seems otherwise normal. g, Detail of section shown in f. h, A region comparable to that in g, in a wild-type embryo. Arrows in g and h indicate hair follicles. Scale bar (h) represents 1 mm for a, 1.86 mm for b and e, 5 mm for c and d, 570 μm for f and 120 μm for g and h.
We further analyzed mutant and control embryos for apoptotic and dead cells to help determine the causes of the embryonic lethality. Staining of embryos with Nile Blue sulfate, a dye that specifically stains dead cells, produced signals throughout the mutant embryos, with higher intensities in the head and neural tube (Fig. 3a,e). TdT-mediated dUTP nick end labeling (TUNEL) assay of histological sections showed massive apoptosis in the developing nervous system of all mutant embryos examined (n=12; Fig. 3c,g). We also found randomly distributed clusters of dead cells in many other areas (Fig. 3i,j). In contrast, control embryos (Fig. 3b,f) and sections (Fig. 3d,h) had very few apoptotic or dead cells. Thus, the high incidence of cell death correlates with the embryonic lethality of Brca1Δ11/Δ11 embryos.
E12.5 mutant (a,e) and control (b,f) embryos were stained with Nile Blue sulfate to view dead cells. There is substantial staining in the brain (a) and neural tube (e) of mutant but not control embryos. Lines indicate levels of cross-sections shown in c,d,g,h. Large numbers of apoptotic cells (arrows) are shown by TUNEL assay in mutant (c,g) but not control (d,h) embryos. Apoptosis is also present in other regions, such as the trunk (i) and tail (j) of mutant embryos. Scale bar (j) represents 1.5 mm for a,b,e,f and 150 μm for c,d,g–j.
To address the potential mechanisms of the increased apoptosis in Brca1Δ11/Δ11 embryos, we examined p53 protein levels; these were slightly increased in four of seven mutant embryos compared with levels in wildtype controls (Fig.4a; data not shown). Although activation of p53 is usually associated with increased levels of the protein, this is not always the case5. To determine the transcriptional regulation activity of p53, we studied expression of genes downstream of p53 in cell cycle checkpoint or apoptotic pathways. All seven mutant embryos showed increased expression of p21Cip1/Waf1 (encoded by cyclin-dependent kinase inhibitor 1A, or Cdkn1a), a potent Cdk inhibitor that mediates the p53-dependent G1–S cell cycle checkpoint6,7 (Fig. 4a). This indicates that p53 is activated in these embryos despite the fact that the protein levels are either slightly or not increased. Chromosome 'spreads' of E10.5 Brca1Δ11/Δ11 embryos (n=5) showed that all contained numerical and structural changes (data not shown). This genetic instability inherent in the mutant embryos is probably the 'trigger' for p53 activation. There was little or no difference in the levels of B-cell leukemia/lymphoma X (Bclx) or Bcl2-associated X protein (Bax); (Fig. 4a). However, there were significantly higher levels of Fas receptor and Fas antibody-induced apoptosis in Brca1Δ11/Δ11 cells (Fig. 4b,c). Although p53 contributes to Fas-mediated apoptosis8, a specific function for p53 in this pathway has not been established. Nonetheless, the significantly lower levels of apoptosis and complete rescue seen in Brca1Δ11/Δ11 embryos when one or both Trp53 alleles are deleted establish that this process is p53-dependent. The endogenous genetic instability arising from loss of the full-length Brca1 isoform probably leads to activation of p53 and some of its downstream pathways.
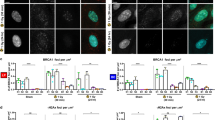
a, Western blot analysis of p53, p21Waf1/Cip1, Bax and Bclx expression in E14.5 Brca1Δ11/Δ11 and wildtype embryos. b, Fas expression, as detected by staining with fluorescein isothiocyanate-conjugated anti-Fas antibody. Mean, median and peak channel are presented in fluorescence units (fu). c, Susceptibility of MEFs to cell death induced by anti-Fas antibody, expressed as percent cell survival relative to untreated cells. d, Mammary tumor formation in Brca1Δ11/Δ11Trp53+/− female mice (n=22). In addition to developing mammary tumors, seven developed lymphomas and two developed ovarian tumors. e, Cell proliferation analysis of MEFs derived from E14.5 embryos. f, Quantitative analysis of the effects of γ-irradiation (10 Gy) on the progression of G0/G1-synchronized MEFs into S phase over 24 h (10,000 cells analyzed/genotype). Percentages in parentheses represent the ratios of BrdU+ cells in irradiated versus untreated samples. g–i, Haploid loss of Trp53 decreases Brca1 deficiency-associated apoptosis, as shown by TUNEL assays for apoptotic cells in E14.5 embryos. Genotypes are indicated.
Next, we tested whether p53 loss affected the survival of Brca1Δ11/Δ11 embryos by crossing Brca1+/Δ11 and Trp53+/− mice, as p53 deficiency partially rescues Brca1-null embryos9,10. This cross generated Brca1+/Δ11Trp53+/− mice, which were healthy and tumor-free during a study period of 1 year. Unexpectedly, when we interbred these mice, we found that Brca1Δ11/Δ11 mice were viable in either a Trp53+/− or a Trp53+/+ background. Of 278 mice genotyped, 27 were Brca1Δ11/Δ11Trp53+/−. In contrast, we recovered only two live Brca1Δ11/Δ11Trp53+/+ mice (Table 1). This indicates that haploid loss of p53 completely rescues the embryonic lethality caused by the Brca1Δ11/Δ11 mutation. Moreover, the number of Brca1Δ11/Δ11Trp53−/− mice was statistically lower than that expected by a mendelian ratio (Table 1). Because a subset of Trp53−/− embryos died during gestation (ref. 11; data not shown), the reduced number of Brca1Δ11/Δ11Trp53−/− mice is probably due to the p53 deficiency. Consistent with the lack of effect of Brca1 status on Bax levels (Fig. 4a), crossing Brca1Δ11/+ and Bax−/− mice12 did not rescue the embryonic lethality of Brca1Δ11/Δ11 embryos (data not shown). Despite increased p21Cip1/Waf1 levels in the Brca1Δ11/Δ11 embryos (Fig. 4a), crosses with Cdkn1a−/− mice7 also did not result in rescue after birth (Table 1). Thus, it is likely that the rescue of Brca1Δ11/Δ11 embryos by haploid or homozygous loss of p53 results from the compromise of a combination of p53 pathways13, as elimination of individual downstream pathways was insufficient.
Brca1Δ11/Δ11Trp53+/− mice showed normal mammary gland development and most of them developed mammary tumors within 6–10 months, nearly all of which had lost the remaining wildtype allele of Trp53 (Fig. 4d; data not shown). This is consistent with the finding that Cre–loxP-mediated deletion of Brca1 exon 11 in mammary epithelium results in tumor formation, which is considerably accelerated in the Trp53+/− background3. Although the molecular basis for such acceleration is not well understood, it may share similarities with the mechanism(s) by which the haploid loss of p53 rescues the Brca1Δ11/Δ11 embryos. To address this at a cellular level, we obtained mouse embryo fibroblasts (MEFs) from E14.5 embryos with the following genotypes: Brca1Δ11/Δ11Trp53+/+, Brca1Δ11/Δ11Trp53+/−, Brca1Δ11/Δ11Trp53−/−, Brca1+/+Trp53+/+, Brca1+/+Trp53+/− and Brca1+/+Trp53−/−. The Brca1Δ11/Δ11Trp53+/+ cells grew very poorly. However, with the removal of one Trp53 allele (Brca1+/+Trp53+/−), their growth improved. After removal of both p53 alleles (Brca1+/+Trp53−/−), they grew even better than wild-type cells (Fig. 4e). These results indicate that the poor growth of Brca1Δ11/Δ11 cells is due to the presence of wildtype Trp53.
One mechanism by which p53 halts cell proliferation is through its control of a DNA damage-induced G1–S cell cycle checkpoint13. This checkpoint was functional in Brca1Δ11/Δ11Trp53+/+ MEFs, as they underwent a reduction of cells that progressed into S phase similar to that of wildtype cells. However, in a Trp53+/− or Trp53−/− background, Brca1Δ11/Δ11 MEFs showed partial or complete loss of the G1–S checkpoint, respectively (Fig. 4f). Thus, a relaxed p53-mediated G1–S damage checkpoint correlates with the improved proliferation of mutant cells.
In addition to its role in checkpoint regulation, p53 can also reduce proliferation by triggering apoptosis. To assess the effect of p53 on spontaneous apoptosis, we carried out TUNEL assays of E14.5 Brca1Δ11/Δ11Trp53+/+, Brca1+/+Trp53+/− and Brca1+/+Trp53−/− embryos. Consistent with our earlier findings (Fig. 3), we found many TUNEL-positive cells in Brca1Δ11/Δ11Trp53+/+ embryos (Fig. 4g). In contrast, we found very few apoptotic cells in Brca1+/+Trp53+/− or Brca1+/+Trp53−/− embryos (Fig. 4h,i). This indicates that haploid loss of p53 is sufficient to overcome the apoptosis triggered by a deficiency of Brca1 exon 11. The substantially reduced apoptosis is probably an important factor that rescues the Brca1Δ11/Δ11 mutant embryos. We also found decreased apoptosis in thymocytes of adult mutant mice (data not shown).
To determine the molecular mechanism(s) underlying the phenotypic rescue of Brca1 exon 11 deficiency by Trp53 heterozygous mutation, we next studied Brca1 and Trp53 expression in thymocytes and MEFs. Northern blot analysis showed that the deletion of Brca1 exon 11 did not affect Trp53 expression in either γ-irradiated or untreated cells (Fig. 5a), indicating that Brca1 does not regulate Trp53 at the transcriptional level. However, Trp53 transcripts were reduced by about half in both MEFs (Fig. 5a) and thymocytes (Fig. 5b) after elimination of one copy of Trp53. Levels of p53 protein were also significantly decreased in these cells (Fig. 5c,e). These observations provide a molecular basis for the observed p53 haploinsufficiency.
RNA and protein obtained from MEFs or thymocytes isolated from mice at the indicated time points after irradiation (10 Gy) were analyzed by northern (about 20 μg total RNA) and western (about 30 μg total protein) blot analysis. For thymocytes, each lane represents a different mouse. a, Northern blot analysis of Trp53 expression in MEFs. b, Western blot analysis of p53 isolated from MEFs. c,d, Northern-blot analysis of Trp53 (b) or Brca1 (d) expression in thymocytes. e–g, Western blot analysis of p53 (e–g) and Mdm2 (e) or Ser18-phophorylated p53 (f,g) in thymocytes. Loading controls, 28S rRNA and β-actin.
Wildtype TRP53 represses BRCA1 expression in cultured cells14,15; our data in cultured Trp53−/− MEFs confirmed this (data not shown). To determine whether this was also true in vivo, we irradiated wild-type and Trp53−/− animals and measured Brca1 expression in thymocytes. The basal level of Brca1 transcription was higher in Trp53−/− thymocytes than in wildtype cells (Fig. 5d). Brca1 levels were significantly induced after γ irradiation of p53−/−cells, reaching a peak at 4–6 hours and decreasing at 10 hours after treatment. In contrast, we found induction of Brca1 in Trp53+/+ cells only 2 hours after treatment, and the level was significantly decreased later (Fig. 5d). These results indicate that Trp53 status influences Brca1 transcript levels both in vitro and in vivo.
To further elucidate the mechanistic interactions between Trp53 and Brca1, we compared p53 protein levels in thymocytes from γ-irradiated mice. In wildtype mice, p53 accumulated to high levels within 2 hours, peaked by 4 hours and decreased substantially by 6 hours after treatment. In Trp53+/− mice, although we found similar accumulation of p53 at two hours after irradiation, it decreased substantially at four and six hours relative to its levels in wildtype cells (Fig. 5e). Thus, disruption of one copy of Trp53 significantly reduces the longevity of the p53 response, which may account for the decreases in apoptosis and G1–S checkpoint function in the Brca1Δ11/Δ11Trp53+/− embryos and cells. We next compared p53 levels in thymocytes of Brca1Δ11/Δ11Trp53+/− and Brca1Δ11/Δ11Trp53+/− mice. Consistent with the results obtained for the untreated whole embryos (Fig. 4a), p53 levels were similar or slightly increased in the untreated Brca1Δ11/Δ11 mice (0 h; Fig. 5e,f). Upregulation of p53 levels induced by γ-irradiation was reduced substantially in all of the Brca1Δ11/Δ11 mice examined (Fig. 5e–g). This indicates that p53 has decreased stability in the Brca1 exon 11 mutant background after treatment with exogenous DNA damaging agents.
We next investigated possible reasons for the reduced stability of p53 in Brca1 mutant cells. The stability of p53 is regulated mainly by transformed mouse 3T3 cell double minute 2 (Mdm2), an ubiquitin ligase that binds to the amino terminus of p53, targeting it for degradation16. Stabilization of p53 in response to γ-irradiation is caused by its dissociation from MDM2 due to phosphorylation of p53 at a number of serine residues in this region, including Ser15 in humans (Ser18 in the mouse)17, and perhaps due to phosphorylation of MDM2 itself18. Levels of Mdm2 in Brca1Δ11/Δ11Trp53+/− thymocytes were significantly increased after γ-irradiation compared with those of Brca1+/+Trp53+/− thymocytes (Fig. 5e). In addition, p53 phosphorylated at Ser18 increased rapidly in Brca1+/+Trp53+/− and Brca1+/+Trp53+/+ thymocytes after treatment, correlating with increased amounts of p53 (Fig. 5f,g). In contrast, accumulation of p53 phosphorylated at Ser18 was delayed and reduced in Brca1+/+Trp53+/− and Brca1Δ11/Δ11Trp53+/+ mutant thymocytes. Thus, both increased Mdm2 levels and decreased phosphorylation of p53 at Ser18 in γ–irradiated Brca1Δ11/Δ11 mutant cells are principal causes for the decreased stability of p53 in these cells.
The DNA damage-activated protein kinase ataxia telangiectasia mutated (ATM) can phosphorylate p53 Ser15/18, MDM2 and BRCA1 (refs. 18–20). Other kinases, including dsDNA-PK (ref. 21), checkpoint kinase 1 homolog (Chek1; ref. 22) and ataxia telangiectasia and rad3 related protein kinase (Atr; ref. 23) can also accomplish some of these phosphorylation events. This indicates at least transient physical interactions between these proteins. Full-length Brca1 may cooperate with such kinases in the phosphorylation of Mdm2 and/or p53. Thus, loss of exon 11 may inhibit p53 stabilization. Further studies are needed to determine which kinase(s) are involved.
In summary, our analysis of mice deficient in Brca1 exon 11 isoform shows a complex pattern of genetic interactions between the tumor suppressors Brca1 and p53 in apoptosis, cell cycle control, genomic stability and tumorigenesis. As the main feature of Brca1 exon 11 deficiency is genetic instability, this instability may serve as an endogenous, indirect signal to activate p53-dependent cell cycle checkpoints and apoptosis, which is almost always lethal in a Trp53+/+ background. A unique feature of Brca1Δ11/Δ11 embryos, in contrast to other reported Brca1 mutant animals9,10,24,25,26, is that they still express the short isoform of Brca1 and show substantially delayed onset of embryonic lethality that can be completely rescued by p53 haploinsufficiency. The decreased Trp53 expression in Brca1Δ11/Δ11Trp53+/− mice results in a reduction of apoptosis and attenuated G1–S checkpoint control, which allows mutant cells to partially overcome their growth defects. The Brca1 full-length isoform is essential in DNA damage repair, G2–M cell cycle checkpoint and centrosome duplication27. Thus, the extended survival of Brca1Δ11/Δ11Trp53+/− mice and decreased p53 stability after DNA-damage stress will unavoidably allow the accumulation of further mutations, including the remaining wildtype allele of Trp53 and alterations of other unidentified genes. This may not cause tumor formation at early developmental stages due to the random nature of mutations. However, tumorigenesis may start any time after essential events occur, which completely overcome the proliferation deficiency caused by the Brca1 mutation. BRCA1 familial breast cancers have significantly higher frequencies of TRP53 mutations and chromosome damage than sporadic cancers28. Our finding that p53 loss rescues the proliferation deficiency of Brca1 mutant cells at the expense of genetic instability offers a plausible explanation for this phenomenon. The Brca1Δ11/Δ11Trp53+/− mice may be useful for further mechanistic and therapeutic studies of BRCA1-associated carcinogenesis.
Methods
Mating and genotyping of mice.
We genotyped Trp53−/− (ref. 29), Bax−/− (ref. 12), Cdkn1a−/− (ref. 7), EIIa–Cre transgenic4 and Brca1 'conditional' mutant3 mice as described. To delete exon 11 of Brca1 from the germ line, we crossed Brca1 'conditional' mice with EIIa–Cre transgenic mice. We genotyped the offspring using primer 1 (5′–CTGGGTAGTTTGTAAGCATCC–3′) and primer 2 (5′–CTGCGAGCAGTCTTCAGAAAG–3′). Primer 1 is located in intron 10 and primer 2 is located in exon 12. The distance between these primers in unrecombined cells is about 5.5 kb, and it is 621 bp in 'exon 11-deleted' cells.
Detection of apoptotic cells.
For whole-mount apoptosis staining, we 'dissected out' embryos at E12.5, placed them into Nile Blue A sulfate salt solution (Sigma), stained them at 37 °C for 30 min and then destained them in PBS until the background was clear. We viewed stained embryos using a dissection microscope and photographed them immediately. For TUNEL assays of apoptotic cells on tissue sections, we used the manufacturer's recommendations (Oncor). For flow cytometric detection of apoptosis, we isolated thymocytes from animals, fixed them in 70% ethanol, stained them with propidium iodide and analyzed them for sub-G0/G1 events on a Becton-Dickinson FACSCalibur.
Cell cultures and treatments.
We obtained primary mouse embryonic fibroblasts from E14.5 embryos using a standard procedure. For G1–S checkpoint analysis, we synchronized cells in G0/G1 by maintaining them for four days in medium containing 0.5% FBS. We then treated cells and plated them in complete medium containing 65 μM 5-bromodeoxyuridine (BrdU). Then, 24 h later, we collected cells, stained them for DNA content with propidium iodide and for replicative DNA synthesis with a fluorescein isothiocyanate-conjugated anti-BrdU antibody, and analyzed them by flow cytometry as described before7,30. To assay cell death induced by anti-Fas antibody (purchased from PharMingen), we plated 5×104 MEFs at passage 1 in each well of a 12-well plate 1 d before treatment. After treating cells with 1 μg/ml antibody for 36 h, we trypsinized cells and determined viability by trypan blue staining. For Fas expression analysis, we stained 1×106 MEFs at passage 1 with a fluorescein isothiocyanate-conjugated anti-Fas monoclonal antibody (PharMingen) for 1 h before flow cytometric analysis.
Cell proliferation analysis.
We plated MEFs derived from E14.5 embryos at a density of 2×105 cells/well in six-well plates. Every three days, we trypsinized cells, counted them and plated them again at the same density. We used at least two embryos representing each genotype and obtained similar results.
Northern and western blots.
We isolated RNA from mouse thymus using RNA Tet-60 based on the protocol recommended by the manufacturer (Tel-Test B). We prepared PolyA+ RNA using a kit purchased from Pharmacia. We used a standard procedure for western blot analyses. We purchased antibodies against total p53 and Ser15-phosphorylated p53 from Transductional Signaling Cell, and antibodies against Bclx and Bax and against p21 from PharMingen and Calbiochem, respectively. The antibody against mouse Mdm2 was a gift from G. Lozano.
References
Hill, A.D., Doyle, J.M., McDermott, E.W. & O' Higgins, N.J. Hereditary breast cancer. Br. J. Surg. 84, 1334–1339 (1997).
Casey, G. The BRCA1 and BRCA2 breast cancer genes. Curr. Opin. Oncol. 9, 88–93 (1997).
Xu, X. et al. Conditional mutation of Brca1 in mammary epithelial cells results in blunted ductal morphogenesis and tumour formation. Nature Genet. 22, 37–43 (1999).
Lakso, M. et al. Efficient in vivo manipulation of mouse genomic sequences at the zygote stage. Proc. Natl. Acad. Sci. USA 93, 5860–5865 (1996).
Vaziri, H. et al. ATM-dependent telomere loss in aging human diploid fibroblasts and DNA damage lead to the post-translational activation of p53 protein involving poly(ADP-ribose) polymerase. Embo. J. 16, 6018–6033. (1997).
Brugarolas, J. et al. Radiation-induced cell cycle arrest compromised by p21 deficiency. Nature 377, 552–557 (1995).
Deng, C., Zhang, P., Harper, J.W., Elledge, S.J. & Leder, P. Mice lacking p21CIP1/WAF1 undergo normal development, but are defective in G1 checkpoint control. Cell 82, 675–684 (1995).
Bennett, M. et al. Cell surface trafficking of Fas: a rapid mechanism of p53-mediated apoptosis. Science 282, 290–293. (1998).
Hakem, R., de la Pompa, J.L., Elia, A., Potter, J. & Mak, T.W. Partial rescue of Brca1 (5–6) early embryonic lethality by p53 or p21 null mutation. Nature Genet. 16, 298–302 (1997).
Shen, S.X. et al. A targeted disruption of the murine Brca1 gene causes γ-radiation hypersensitivity and genetic instability. Oncogene 17, 3115–3124 (1998).
Sah, V.P. et al. A subset of p53-deficient embryos exhibit exencephaly. Nature Genet. 10, 175–180 (1995).
Knudson, C.M., Tung, K.S., Tourtellotte, W.G., Brown, G.A. & Korsmeyer, S.J. Bax-deficient mice with lymphoid hyperplasia and male germ cell death. Science 270, 96–99 (1995).
May, P. & May, E. Twenty years of p53 research: structural and functional aspects of the p53 protein. Oncogene 18, 7621–7636 (1999).
Andres, J.L. et al. Regulation of BRCA1 and BRCA2 expression in human breast cancer cells by DNA-damaging agents. Oncogene 16, 2229–2241 (1998).
MacLachlan, T.K., Dash, B., Dicker, D.T. & El-Deiry, W. Repression of BRCA1 through a feedback loop involving p53. J. Biol. Chem. 275, 31869–31875 (2000).
Haupt, Y., Maya, R., Kazaz, A. & Oren, M. Mdm2 promotes the rapid degradation of p53. Nature 387, 296–299 (1997).
Wang, Y. & Eckhart, W. Phosphorylation sites in the amino-terminal region of mouse p53. Proc. Natl. Acad. Sci. USA 89, 4231–4235 (1992).
Khosravi, R. et al. Rapid ATM-dependent phosphorylation of MDM2 precedes p53 accumulation in response to DNA damage. Proc. Natl. Acad. Sci. USA 96, 14973–14977. (1999).
Nakagawa, K., Taya, Y., Tamai, K. & Yamaizumi, M. Requirement of ATM in phosphorylation of the human p53 protein at serine 15 following DNA double-strand breaks. Mol. Cell Biol. 19, 2828–2834 (1999).
Cortez, D., Wang, Y., Qin, J. & Elledge, S.J. Requirement of ATM-dependent phosphorylation of brca1 in the DNA damage response to double-strand breaks. Science 286, 1162–1166 (1999).
Shieh, S.Y., Ikeda, M., Taya, Y. & Prives, C. DNA damage-induced phosphorylation of p53 alleviates inhibition by MDM2. Cell 91, 325–334 (1997).
Shieh, S.Y., Ahn, J., Tamai, K., Taya, Y. & Prives, C. The human homologs of checkpoint kinases Chk1 and Cds1 (Chk2) phosphorylate p53 at multiple DNA damage-inducible sites. Genes Dev. 14, 289–300 (2000).
Tibbetts, R.S. et al. A role for ATR in the DNA damage-induced phosphorylation of p53. Genes Dev. 13, 152–157 (1999).
Hakem, R. et al. The tumor suppressor gene Brca1 is required for embryonic cellular proliferation in the mouse. Cell 85, 1009–1023 (1996).
Liu, C.Y., Flesken-Nikitin, A., Li, S., Zeng, Y. & Lee, W.H. Inactivation of the mouse Brca1 gene leads to failure in the morphogenesis of the egg cylinder in early postimplantation development. Genes Dev. 10, 1835–1843 (1996).
Cressman, V.L. et al. Growth retardation, DNA repair defects, and lack of spermatogenesis in BRCA1-deficient mice. Mol. Cell Biol. 19, 7061–7075 (1999).
Deng, C.X. & Brodie, S. Roles of BRCA1 and its interacting proteins. BioEssays 22, 728–737 (2000).
Schuyer, M. & Berns, E.M. Is TP53 dysfunction required for BRCA1-associated carcinogenesis? Mol. Cell Endocrinol. 155, 143–152 (1999).
Donehower, L.A. et al. Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature 356, 215–221 (1992).
Linke, S.P., Clarkin, K.C. & Wahl, G.M. p53 mediates permanent arrest over multiple cell cycles in response to gamma-irradiation. Cancer Res. 57, 1171–1179 (1997).
Acknowledgements
We thank S.J. Korsmeyer for Bax−/− mice, L. Donehower for Trp53−/− mice, H. Westphal for EIIa-Cre transgenic mice and G. Lozano for antibody against Mdm2. We thank C. Li and B. Jeffries for technical assistance, and members of the Deng laboratory for discussions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xu, X., Qiao, W., Linke, S. et al. Genetic interactions between tumor suppressors Brca1 and p53 in apoptosis, cell cycle and tumorigenesis. Nat Genet 28, 266–271 (2001). https://doi.org/10.1038/90108
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/90108
This article is cited by
-
A transcriptomic model for homologous recombination deficiency in prostate cancer
Prostate Cancer and Prostatic Diseases (2022)
-
S100A9-CXCL12 activation in BRCA1-mutant breast cancer promotes an immunosuppressive microenvironment associated with resistance to immunotherapy
Nature Communications (2022)
-
Heterozygotic Brca1 mutation initiates mouse genome instability at embryonic stage
Oncogenesis (2022)
-
Consistency of variant interpretations among bioinformaticians and clinical geneticists in hereditary cancer panels
European Journal of Human Genetics (2022)
-
Porcine model elucidates function of p53 isoform in carcinogenesis and reveals novel circTP53 RNA
Oncogene (2021)