Abstract
Leptin treatment reverses hyperglycemia in animal models of poorly controlled type 1 diabetes (T1D)1,2,3,4,5,6, spurring great interest in the possibility of treating patients with this hormone. The antidiabetic effect of leptin has been postulated to occur through suppression of glucagon production, suppression of glucagon responsiveness or both; however, there does not appear to be a direct effect of leptin on the pancreatic alpha cell7. Thus, the mechanisms responsible for the antidiabetic effect of leptin remain poorly understood. We quantified liver-specific rates of hepatic gluconeogenesis and substrate oxidation in conjunction with rates of whole-body acetate, glycerol and fatty acid turnover in three rat models of poorly controlled diabetes, including a model of diabetic ketoacidosis8. We show that the higher rates of hepatic gluconeogenesis in all these models could be attributed to hypoleptinemia-induced activity of the hypothalamic-pituitary-adrenal (HPA) axis, resulting in higher rates of adipocyte lipolysis, hepatic conversion of glycerol to glucose through a substrate push mechanism and conversion of pyruvate to glucose through greater hepatic acetyl-CoA allosteric activation of pyruvate carboxylase flux. Notably, these effects could be dissociated from changes in plasma insulin and glucagon concentrations and hepatic gluconeogenic protein expression. All the altered systemic and hepatic metabolic fluxes could be mimicked by infusing rats with Intralipid or corticosterone and were corrected by leptin replacement. These data demonstrate a critical role for lipolysis and substrate delivery to the liver, secondary to hypoleptinemia and HPA axis activity, in promoting higher hepatic gluconeogenesis and hyperglycemia in poorly controlled diabetes.
Similar content being viewed by others
Main
To understand the mechanisms driving hyperglycemia in T1D, we induced T1D in otherwise normal rats using streptozotocin. Rats with T1D had severe fasting hyperglycemia and ketoacidosis associated with approximately 90% lower plasma insulin and leptin concentrations and 90% higher plasma glucagon concentrations compared to control nondiabetic rats (Fig. 1a–d and Supplementary Table 1). These changes occurred without any differences in the relative contributions of hepatic gluconeogenesis (91 ± 4% compared to 91 ± 2% (mean ± s.e.m.) in control rats and those with T1D, respectively) and renal gluconeogenesis (9 ± 4% compared to 9 ± 2% in control rats and those with T1D, respectively) to rates of whole-body glucose production. Normalizing plasma leptin concentrations in the rats with T1D with a 6-h intra-arterial leptin infusion resulted in 240 mg dl−1 lower plasma glucose concentrations compared to rats infused with an equal volume of saline associated with reversal of ketoacidosis without any differences in plasma insulin, glucagon, adiponectin or fibroblast growth factor 21 (FGF-21) concentrations or in the phosphorylation of the glucagon target cyclic AMP response element-binding protein (CREB) (Fig. 1a–d and Supplementary Fig. 1a–c). Notably, normalization of plasma glucagon concentrations in these rats did not occur until 24 h after leptin treatment, which was 18 h after the normalization of plasma glucose. Leptin treatment in rats with T1D was associated with 60% lower hepatic gluconeogenesis rates through reductions in the conversion of both pyruvate and glycerol to glucose (Fig. 1e). In contrast, although total tricarboxylic acid (TCA) cycle flux (VTCA) did not change, fatty acid oxidation was greater in the livers of rats with T1D compared to control nondiabetic rats, and this perturbation was reversed with leptin treatment (Supplementary Fig. 1d). The lower contribution of glycerol to hepatic gluconeogenesis with leptin treatment was strongly associated with lower rates of whole-body lipolysis in treated compared to untreated rats with T1D, as reflected by 60% lower rates of whole-body glycerol and palmitic acid turnover and plasma glycerol and non-esterified fatty acid (NEFA) concentrations in the treated rats (Fig. 1f,g and Supplementary Fig. 1e,f). The higher rates of whole-body lipolysis in leptin-deficient rats with T1D were also associated with threefold higher acetate turnover, 250% higher plasma acetate concentrations and 80% higher liver acetyl-CoA concentrations, all of which were reversed with leptin treatment (Fig. 1h,i and Supplementary Fig. 1g).
(a) Fasting plasma glucose concentrations in control nondiabetic rats, rats with T1D and rats with T1D treated with leptin (T1D-leptin). n = 8 controls, n = 6 T1D, n = 8 T1D-leptin. (b) Fasting plasma insulin concentrations. n = 7 controls, n = 7 T1D, n = 6 T1D-leptin. (c) Fasting plasma glucagon concentrations. n = 7 controls, n = 6 T1D, n = 16 T1D treated with leptin for 6 h, n = 5 T1D treated with leptin for 24 h. (d) Fasting plasma leptin concentrations. n = 8 for all groups. (e) Hepatic gluconeogenesis from pyruvate (lower bars) and glycerol (upper bars). The P values over the bars are from comparisons of total gluconeogenic flux. In e–h, n = 6 for all groups. (f–h) Whole-body glycerol, fatty acid (palmitate) and acetate turnover. (i) Liver acetyl-CoA concentrations. n = 12 controls, n = 6 T1D, n = 6 T1D-leptin. (j) Plasma corticosterone concentrations measured at 12:00 p.m. n = 7 controls, n = 8 T1D, n = 6 T1D-leptin. Throughout the figure, the data are shown as the mean ± s.e.m. *P < 0.05, ***P < 0.001, ****P < 0.0001 compared to control; ##P < 0.01, ###P < 0.001, ####P < 0.0001 compared to T1D; §§§P < 0.001 compared to T1D-leptin 6 h. NS, not significant. Throughout the figure, all groups were compared using analysis of variance (ANOVA) with Bonferroni correction.
As acetyl-CoA is a potent allosteric activator of pyruvate carboxylase activity9,10,11,12 and an inhibitor of pyruvate dehydrogenase (PDH) activity13, the observed alterations in hepatic acetyl-CoA concentrations in the untreated and leptin-treated rats with T1D probably explain the observed differences in hepatic pyruvate carboxylase flux (VPC) and hepatic PDH flux (VPDH) between these groups of animals. To determine the reason for the improvement in ketoacidosis with leptin treatment, we measured hepatic malonyl-CoA concentrations and found that, consistent with the reversal of ketoacidosis in the rats with T1D rats (as reflected by the normalization of the anion gap and reductions in plasma β-hydroxybutyrate concentrations14), the lower malonyl-CoA concentrations in the rats with poorly controlled T1D were normalized after leptin treatment (Supplementary Fig. 1h).
It is possible that leptin may also have a direct effect on muscle glucose uptake, peripheral insulin sensitivity or both, as has been reported in some1,15,16 but not all2,17 studies. However, our data imply that the effect of leptin in reversing fasting hyperglycemia can be explained for the most part by leptin-mediated suppression of substrate delivery to the liver by reduction of whole-body rates of lipolysis, resulting in lower rates of hepatic gluconeogenesis. To examine the mechanism for the greater lipolysis and its reversal with leptin treatment, we measured plasma catecholamine, growth hormone and corticosterone concentrations. In contrast to the concentrations of plasma epinephrine and norepinephrine, which were not different between the groups, and growth hormone concentrations, which were lower in rats with T1D than in control rats, we found that plasma corticosterone and ACTH concentrations obtained at 12:00 p.m. were markedly greater in the rats with T1D than in control rats and that this effect was reversed with leptin treatment (Fig. 1j and Supplementary Fig. 1i–l). Taken together, these data suggest a critical role for the HPA axis in promoting the higher rates of lipolysis in the group with T1D.
To assess whether alterations in plasma insulin concentrations accounted for the hypoleptinemia, elevated gluconeogenesis or both in the streptozotocin-induced T1D model, we also measured hepatic fluxes in rats rendered both hyperglycemic and hyperinsulinemic by feeding a high-fat diet (HFD) for 3 days combined with low-dose streptozotocin and nicotinamide treatment (the hyperinsulinemic-diabetic rat model) and found that all alterations in hepatic anaplerotic and oxidative fluxes in the T1D rat model were replicated in the hyperinsulinemic-diabetic rats. Hyperinsulinemic-diabetic rats were equally as hyperglycemic as the T1D group despite having ∼40-fold higher plasma insulin concentrations (Supplementary Fig. 2a,b), but in contrast to the rats with T1D, the hyperinsulinemic-diabetic rats were not ketoacidotic (Supplementary Table 2). However, hyperinsulinemic-diabetic rats had similar leptin deficiency as rats with T1D (Supplementary Fig. 2d). Restoring plasma leptin concentrations with a 6-h intra-arterial leptin infusion normalized plasma glucose, corticosterone and ACTH concentrations and the rates of hepatic gluconeogenesis from pyruvate and glycerol without altering plasma insulin concentrations or VTCA flux (Supplementary Fig. 2a–h). Similar to the T1D group, whole-body glycerol, fatty acid and acetate turnover were reduced with leptin treatment, as were hepatic acetyl-CoA concentrations (Supplementary Fig. 2i–l). In contrast, mRNA and protein expression of key gluconeogenic enzymes were not different between the control, hyperinsulinemic-diabetic and T1D groups (Supplementary Fig. 3a–g). Taken together, these data imply that excess hepatic substrate flux, independent of insulin, is responsible for the uncontrolled gluconeogenesis of poorly controlled T1D and the improvement in glycemia associated with leptin treatment.
On the basis of these data, we next examined whether the higher rates of whole-body lipolysis due to leptin deficiency might have a role in causing excess gluconeogenesis in the rats with T1D. We reasoned that increased glycerol turnover would drive hepatic gluconeogenesis through a substrate-dependent process3,18, whereas an increase in acetate and fatty acid turnover would increase gluconeogenesis through allosteric activation of pyruvate carboxylase by acetyl-CoA. To determine whether excess substrate availability alone could induce any of the changes to hepatic fluxes measured in rats with poorly controlled T1D, we performed a 24-h infusion of Intralipid along with heparin to activate lipoprotein lipase activity (Intralipid raises the levels of free fatty acids, and heparin activates lipoprotein lipase, which increases lipolysis, raising free fatty acid levels)19. Consistent with our hypothesis, this intervention resulted in higher plasma glucose concentrations and gluconeogenesis from both pyruvate and glycerol despite greater plasma insulin concentrations and no changes in plasma glucagon, FGF-21 or adiponectin concentrations (Fig. 2a,b and Supplementary Fig. 4a–d). As observed in the other diabetic rodent models, excess hepatic gluconeogenesis could be attributed to markedly higher rates of whole-body glycerol and fatty acid turnover compared to nondiabetic controls without any difference in total hepatic TCA cycle flux (Fig. 2c–e and Supplementary Fig. 4e,f). As predicted by the greater VPC and reduced VPDH flux, hepatic acetyl concentrations were ∼50% higher in the lipid-infused group compared to the saline-infused control group (Fig. 2f).
(a) Plasma glucose concentrations in high fat–fed nondiabetic untreated rats and rats fed a HFD and infused with heparin and Intralipid (HFD-lipid). (b) Hepatic gluconeogenesis from pyruvate (lower bars) and glycerol (upper bars). (c) TCA cycle flux from fatty acid oxidation (lower bars) and through PDH (upper bars). (d,e) Whole-body glycerol and fatty acid (palmitate) turnover. (f) Liver acetyl-CoA concentrations. Throughout the figure, the data are shown as the mean ± s.e.m. of n = 6 per group. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Statistical analyses were performed using two-tailed unpaired Student's t test. Asterisks under the lower bars represent comparisons of gluconeogenesis from pyruvate, asterisks over the upper bars represent comparisons of gluconeogenesis from glycerol and the uppermost asterisks represent comparisons with total gluconeogenesis.
To further investigate the putative role of substrate regulation as necessary for leptin's antidiabetic effects, we co-infused leptin-treated T1D rats with Intralipid and heparin and found that raising acetyl-CoA, glycerol and fatty acid concentrations by this intervention abrogated the effect of leptin to correct hyperglycemia and normalize the rates of hepatic gluconeogenesis from glycerol and pyruvate (Fig. 3a–f and Supplementary Fig. 5a–f).
(a) Fasting plasma glucose in rats with T1D treated with leptin or treated with leptin and infused with lipids (T1D-leptin-lipid). (b) Hepatic gluconeogenesis from pyruvate (lower bars) and glycerol (upper bars). (c) VTCA from fatty acid oxidation (lower bars) and through PDH (upper bars). (d,e) Whole-body glycerol and palmitic acid oxidation. (f) Liver acetyl-CoA concentrations. Throughout the figure, the data are shown as the mean ± s.e.m. of n = 6 per group. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Statistical analyses were performed using two-tailed unpaired Student's t test. Asterisks under the lower bars represent comparisons of gluconeogenesis from pyruvate, asterisks over the upper bars represent comparisons of gluconeogenesis from glycerol and the uppermost asterisks represent comparisons with total gluconeogenesis.
Taken together, these data demonstrate that excess substrate flux, derived from excess peripheral lipolysis, drives the higher rates of hepatic gluconeogenesis in poorly controlled diabetes through increasing both glycerol supply and hepatic acetyl-CoA concentrations, therefore allosterically activating pyruvate carboxylase. Thus, these studies demonstrate the critical roles of increased substrate delivery to the liver and allosteric regulation of pyruvate carboxylase activity as the key factors responsible for causing the higher rates of gluconeogenesis in poorly controlled T1D. Furthermore, by demonstrating marked elevations in the rates of hepatic gluconeogenesis independent of changes in hepatic gluconeogenic protein expression, these results also challenge the canonical role for alterations in hepatic gluconeogenic gene and protein expression as the major contributor to higher hepatic gluconeogenesis in poorly controlled diabetes.
Because hypercorticosteronemia has been observed in leptin-deficient and leptin-resistant rodent models20,21 and leptin has been identified as a suppressor of ACTH-dependent cortisol secretion in vitro22, we hypothesized that leptin deficiency may be responsible for higher HPA activity leading to higher rates of lipolysis and rates of gluconeogenesis in rats with T1D (Fig. 1e–j). To determine whether these elevations in plasma corticosterone concentrations would promote similar increases in rates of lipolysis as observed in rats with T1D, we injected HFD-fed rats with intra-arterial corticosterone for 24 h to achieve similar plasma levels of corticosterone as those in rats with T1D (163 ± 19 compared to 187 ± 30 ng ml−1 (mean ± s.e.m.), respectively, P = 0.6). This intervention resulted in approximately 100 mg dl−1 higher plasma glucose concentrations compared to control rats, as well as greater hepatic gluconeogenesis from both pyruvate and glycerol despite threefold higher plasma insulin concentrations (Fig. 4a–c). In contrast, these changes were not associated with any changes in the TCA cycle flux (Fig. 4d). The higher rates of hepatic gluconeogenesis in corticosterone-infused rats were driven by greater whole-body glycerol, fatty acid and acetate turnover compared to control rats associated with higher plasma glycerol, fatty acid and acetate concentrations, as well as hepatic acetyl-CoA concentrations similar to those in rats with T1D (Fig. 4e–h and Supplementary Fig. 6a–c). In contrast, there were no differences in plasma glucagon, FGF-21 or adiponectin concentrations between the rats treated with corticosterone and control rats (Supplementary Fig. 6d–f).
(a) Fasting plasma glucose in nondiabetic, saline-infused control rats and rats fed a HFD and infused with corticosterone (HFD-cort). (b) Hepatic gluconeogenesis from pyruvate (black or white bars) and glycerol (gray bars). (c) Fasting plasma insulin. (d) TCA cycle flux from fatty acid oxidation (lower bars) and through PDH (upper bars). (e–g) Whole-body glycerol, fatty acid (palmitate) and acetate turnover. (h) Liver acetyl-CoA concentrations. Throughout the figure, the data are shown as the mean ± s.e.m. of n = 6 per group. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Statistical analyses were performed using two-tailed unpaired Student's t test.
To test the mechanism of ACTH-driven increases in corticosterone in driving hyperglycemia in rats with T1D, we inhibited the activity of the glucocorticoid receptor–the receptor for corticosterone–by treating diabetic rats with mifepristone, a potent antagonist for this receptor23. Consistent with a major role for higher HPA activity in driving greater lipolysis and hepatic gluconeogenesis, treatment with mifepristone resulted in >200 mg dl−1 lower fasting plasma glucose concentrations compared to the control group with T1D despite identical fasting plasma insulin and glucagon concentrations (Supplementary Fig. 7a–c). Improvements in glycemia in the treated group could be attributed to less hepatic gluconeogenesis from both pyruvate and glycerol without any changes in total VTCA (Supplementary Fig. 7d,e). As compared to control rats with T1D, mifepristone-treated rats with T1D exhibited 75–85% lower whole-body glycerol, fatty acid and acetate turnover, as well as >40% lower plasma glycerol, fatty acid and acetate concentrations associated with 60% lower hepatic acetyl-CoA concentrations (Supplementary Fig. 7f–l). Thus, the lower fasting plasma glucose concentrations in hyperglycemic rats with T1D treated with mifepristone could be attributed to lower rates of whole-body lipolysis and less hepatic acetyl-CoA content.
To determine whether these findings were specific to the acute ketoacidotic state of rats with streptozotocin-induced T1D, we also examined BioBreeding (BB) rats, a genetic rat model of spontaneous T1D. Similar to the streptozotocin-induced T1D model, the BB rats exhibited severe hyperglycemia associated with hypoleptinemia, as well as hyperglucagonemia and insulinopenia (Supplementary Fig. 8a–d). Correcting hypoleptinemia normalized plasma glucose concentrations and hepatic gluconeogenesis within 6 h by correcting lipolysis and normalizing hepatic acetyl-CoA concentrations (Supplementary Fig. 8e–j). Consistent with our findings in other diabetic rat models, hyperglycemia was associated with higher plasma corticosterone and ACTH concentrations compared to control animals, which were corrected in the leptin-infused group (Supplementary Fig. 8k,l). Also similar to our observations in streptozotocin-treated rats with T1D, plasma glucagon concentrations normalized after 24 h of leptin treatment, which was more than 12 h after the reductions in plasma concentrations of ACTH, corticosterone and plasma glucose, thus temporally dissociating leptin-induced reductions in plasma glucagon concentrations from leptin-induced reductions in plasma ACTH, corticosterone and glucose concentrations (Supplementary Fig. 8c).
Taken together, these data identify a key role for hypoleptinemia-induced increases in HPA activity in contributing to the higher rates of hepatic gluconeogenesis, fasting hyperglycemia and ketoacidosis in rodent models of T1D through glucocorticoid-mediated increases in lipolysis (Supplementary Fig. 9a) and provide the mechanism for correction of hyperglycemia in these animals after administration of leptin (Supplementary Fig. 9b)2,24,25. Furthermore, these results have potential translational importance given that previous studies have documented increases in plasma cortisol concentrations in diabetic ketoacidosis in patients with T1D26,27,28. Whether this mechanism also contributes to the ability of leptin to reverse insulin resistance and hyperglycemia in patients with severe lipodystrophy, in addition to its ability to decrease hepatic steatosis and intramyocellular lipid content29, remains to be determined.
Methods
Animals.
Male Sprague-Dawley rats weighing 300–400 g were obtained from Charles River Laboratories (Wilmington, MA) and allowed to acclimate for 1 week before any studies were performed. Rats underwent surgery under general anesthesia with isoflurane to place catheters in the common carotid artery and internal jugular vein (PE50 and PE90 tubing, respectively, Instech Laboratories, Plymouth Meeting, PA). After at least 5 d of recovery, the animals underwent the studies described below. A timeline for each animal study is shown in the Supplementary Methods. All protocols were approved by the Yale University Animal Care and Use Committee.
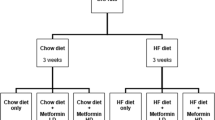
To induce T1D, normal chow-fed rats were injected with 75 mg kg−1 streptozotocin, and studies on those with tail vein blood glucose concentrations >300 mg dl−1 measured by the AlphaTrak2 glucometer were initiated 24 h later. BioBreeding (BB) rats were purchased from Biomedical Research Models, and studies were initiated when random tail vein blood glucose concentrations exceeded 400 mg dl−1. In the hyperinsulinemic-diabetic model, chow-fed rats were treated with 60 mg kg−1 nicotinamide and, 15 min later, 60 mg kg−1 streptozotocin. Studies on those with blood glucose >250 mg dl−1 began 36 h later. Rats with anion gap >15 mEq l−1 measured by COBAS as described below, indicating diabetic ketoacidosis, were excluded from the hyperinsulinemic-diabetic group. In the leptin infusion studies, T1D or hyperinsulinemic-diabetic rats were infused with leptin for 6 h (0.125 mg kg−1 total) or an equivalent volume of saline, and glucose and fatty acid metabolism were studied as described below. Separate groups of T1D and BB rats were infused with leptin for 24 h and euthanized after an overnight fast. Plasma samples were obtained for measurement of glucagon concentrations.
In the HFD-lipid model, rats previously fed a safflower oil–based high-fat diet (HFD) (Dyets, Inc.) for 3 d to increase lipid turnover were infused through the arterial catheter for 24 h with heparin (2 U ml−1) and Intralipid (43.2 ml kg−1 total) or an equivalent volume of saline (control). Glucose and fatty acid metabolism were studied as described below.
In the HFD-corticosterone infused model, rats previously fed safflower-oil HFD for 3 d to increase lipid turnover were infused intra-arterially with corticosterone for 24 h (50 mg kg−1 total) or an equivalent volume of saline (control). Glucose and fatty acid metabolism were studied as described below.
In the leptin and substrate infusion studies, T1D rats were co-infused with leptin and heparin (2 U ml−1)/Intralipid (10.8 ml kg−1 total) or saline for 6 h, as illustrated in the Supplementary Methods. Glucose and fatty acid metabolism were studied as described below for the last 2 h of the study.
To further study the effect of excess glucocorticoids in type 1 diabetes, T1D was induced as described above. T1D rats were given an intraperitoneal injection of mifepristone (40 mg kg−1) 1 h before initiating an isotope infusion to study glucose and fatty acid metabolism.
13C and 3H tracer infusions.
[3-13C] lactate and [3-3H] glucose were infused intra-arterially for 120 min in a primed-continuous infusion as described previously30. After 120 min, rats were euthanized by intravenous pentobarbital, and the liver was freeze clamped in situ in liquid nitrogen and stored at −80 °C for further analysis. To measure total glutamate, alanine, pyruvate, malate, succinate and aspartate enrichment from livers of rats infused with [3-13C] lactate, ∼100 mg of liver was homogenized in 400 μl 50% acetonitrile, vortexed briefly and centrifuged at 4,000 r.p.m. for 10 minutes. The clear liquid layer was purified by filtration with the Pall Nanosep (100K) device for liquid chromatography–tandem mass spectrometry (LC/MS/MS) analysis, which was performed on an AB Sciex QTRAP 6500 equipped with a Shimadzu ultra fast liquid chromatography system and electrospray ionization source with negative-ion detection. The total 13C enrichment was monitored by neutral loss of water. The 13C atom percentage excess was calculated directly from the multiple reaction monitoring (MRM) peak intensities. A hypercarb HPLC column was used to separate glutamate and glutamine with a mixture solvent of water and acetonitrile because of their partial MRM transition overlaps. The optimized parameters for the mass spectrometer were as follows: curtain gas, 30; collision gas medium, probe temperature, 600 °C; ion source Gas 1 and 2, 70; declustering potential, −50 V; entrance potential, −10 V; collision energy, −14.5 V; and collision cell exit potential, −13 V. Total hepatic citrate concentration was measured using this LC/MS method in samples spiked with an internal standard (d4 taurine), and glutamate and glutamine concentrations were measured biochemically using the YSI Analyzer. Acetyl-CoA was measured as described below.
To measure positional metabolite enrichment, the liver samples were extracted for nuclear magnetic resonance (NMR) spectroscopy. ∼3–4 g of ground liver was centrifuged in ∼30 ml 7% perchloric acid. The pH of the supernatant was adjusted to 6.5–7.5, and the extract was dehydrated by lyophilizing for 2–3 d. The extract was resuspended in 500 μl potassium phosphate buffer (2.4 mM NaCOOH, 30 mM K2HPO4, 10 mM KH2PO4 and 20 mM DMSO (internal standard) in 100% D2O). The samples were run on the AVANCE 500-MHz NMR spectrometer (Bruker Instruments). Spectra were acquired with relaxation time = 1 s, dummy scans = 32 and number of scans = 8,000 per block × three blocks. Correction factors for differences in T1 relaxation times were determined from fully relaxed spectra of standard glutamate solutions. The total glutamate enrichment measured by LC/MS/MS was divided algebraically between the five carbons of glutamate based on the relative areas of the 13C NMR peaks.
To measure the total glucose enrichment, 30 μl of the extract for LC/MS/MS was extracted for glucose spectroscopy analysis as described previously31. 13C NMR spectra were obtained as described above, and for glutamate, the total glucose enrichment by gas chromatography–MS (GC/MS) was divided algebraically to measure the enrichment at each glucose carbon.
To measure positional alanine enrichment, liver samples were extracted for NMR as described above, and the enrichment at [3-13C] alanine was measured by proton-observed, carbon-edited NMR as reported previously32.
Measurement of hepatic flux ratios.
All flux ratios were measured from rats infused with [3-13C] lactate as described in the Supplementary Methods.
Measurement of absolute flux rates.
Whole-body glucose production was measured using steady-state (120 min) plasma samples infused with [3H] glucose. Plasma and tracer tritium activity were determined using a scintillation counter (PerkinElmer), and glucose production was calculated as reported previously33. To differentiate between hepatic and renal glucose production, we anesthetized a group of rats with isoflurane and infused [3H] glucose as described above to measure basal glucose production. We then ligated the kidneys by tying off the renal vascular supply with sutures and continued the [3H] glucose infusion. Renal glucose production was measured as the difference between basal glucose production and glucose production after ligating the renal vascular supply. Because our rats, which were fasted for 16 h before each study, were highly glycogen depleted, we expected minimal glycogen breakdown and minimal contribution of glycogen to glucose production; thus we assumed that all measured glucose production was the result of gluconeogenesis.
Absolute VPC was calculated by multiplying the percentage gluconeogenesis from pyruvate by the calculated hepatic glucose production based on the assumption that all glucose production from pyruvate was supplied by anaplerotic carbons through PC. Gluconeogenesis from glycerol was calculated as the difference between total gluconeogenesis and gluconeogenesis from pyruvate. Absolute VTCA was calculated by dividing the calculated VPC by the measured VPC/VTCA ratio. The absolute contribution of pyruvate to TCA cycle flux (VPDH) was calculated by multiplying the fraction of VPDH/VTCA by the calculated VTCA, and the fatty acid oxidation rate was calculated as the difference between VTCA and VPDH.
Whole-body acetate turnover was measured by assessing whole-body acetate turnover during a primed (0–5 min: 358 μmol/(kg-min), 5–10 min: 178 μmol/(kg-min))-continuous (10–120 min: 130 μmol/(kg-min)) infusion. Plasma acetate concentrations before acetate infusions and acetate enrichment at steady state were measured by GC/MS34. Acetate turnover was calculated using the measured plasma enrichment:

Whole-body glycerol and fatty acid turnover were measured by infusing rats with [1,1,2,3,3-d5] glycerol (1.5 μmol/(kg-min)) and [U-13C] palmitate (50 μg/(kg-min)) for 150 min. Steady-state glycerol enrichment and concentration as well as palmitate enrichment were measured by GC/MS, and whole-body palmitate and glycerol turnover were calculated using the equation shown above.
Biochemical analysis.
Plasma glucose concentrations were measured using the YSI Life Sciences 2700 Select Biochemistry Analyzer. Plasma insulin and glucagon concentrations were measured in samples spiked with aprotinin using radioimmunoassay by the Yale Diabetes Research Core. Plasma leptin, corticosterone, ACTH, epinephrine, norepinephrine, growth hormone, adiponectin and FGF-21 concentrations were measured by ELISA (Millipore, Abcam, MyBioSource, IBL International, IBL International, Life Technologies, Invitrogen and Millipore, respectively). Plasma electrolytes and carbon dioxide (as a surrogate for bicarbonate) were measured by COBAS, and anion gap was calculated as follows: anion gap = [Na+] + [K+] − ([CO2] + [Cl+]). Plasma β-hydroxybutyrate, alanine transaminase, aspartate transaminase and blood urea nitrogen concentrations were also measured by COBAS. NEFA concentrations were measured using a kit from Wako.
Measurement of liver CoA concentrations.
Hepatic acetyl-CoA and malonyl-CoA concentrations were measured by LC/MS/MS35,36.
mRNA and protein concentration measurements.
Liver concentrations of PC, G6Pase and cytosolic PEPCK mRNA were measured by real-time PCR9. Concentrations of pyruvate carboxylase, G6Pase and cytosolic PEPCK proteins in liver mitochondria were measured and normalized to glyceraldehyde 3-phosphate dehydrogenase (GAPDH) as reported previously37, with antibodies to each protein obtained from Santa Cruz (cat. nos. sc-46230, sc-33841, sc-377136 and sc-20357, respectively; dilutions 1:200, 1:200, 1:200 and 1:500, respectively). Antibodies to CREB and phosphorylated CREB were obtained from Cell Signaling (cat. nos. 9197 and 9198, respectively; dilutions 1:1,000 for both CREB and phosphorylated CREB), and western blots were performed as described above.
Statistical analyses.
Statistical analyses were performed using GraphPad Prism 5.0d. Two-tailed unpaired Student's t test was used for comparisons of two groups, and one-way analysis of variance with Bonferroni's multiple comparison test was used for comparisons of three or four groups. Differences were considered significant at P < 0.05. All data are expressed as the mean ± s.e.m.
References
Fujikawa, T. et al. Leptin engages a hypothalamic neurocircuitry to permit survival in the absence of insulin. Cell Metab. 18, 431–444 (2013).
Meek, T.H. et al. Leptin action in the ventromedial hypothalamic nucleus is sufficient, but not necessary, to normalize diabetic hyperglycemia. Endocrinology 154, 3067–3076 (2013).
Fujikawa, T., Chuang, J.C., Sakata, I., Ramadori, G. & Coppari, R. Leptin therapy improves insulin-deficient type 1 diabetes by CNS-dependent mechanisms in mice. Proc. Natl. Acad. Sci. USA 107, 17391–17396 (2010).
Wang, M.Y. et al. Leptin therapy in insulin-deficient type I diabetes. Proc. Natl. Acad. Sci. USA 107, 4813–4819 (2010).
Chinookoswong, N., Wang, J.L. & Shi, Z.Q. Leptin restores euglycemia and normalizes glucose turnover in insulin-deficient diabetes in the rat. Diabetes 48, 1487–1492 (1999).
Lin, C.Y., Higginbotham, D.A., Judd, R.L. & White, B.D. Central leptin increases insulin sensitivity in streptozotocin-induced diabetic rats. Am. J. Physiol. Endocrinol. Metab. 282, E1084–E1091 (2002).
Chen, L., Philippe, J. & Unger, R.H. Glucagon responses of isolated alpha cells to glucose, insulin, somatostatin, and leptin. Endocr. Prac. 17, 819–825 (2011).
Craighead, J.E. Experimental models of juvenile onset (insulin-dependent) diabetes mellitus. Monogr. Pathol. 21, 166–176 (1980).
Utter, M.F. & Keech, D.B. Formation of oxaloacetate from pyruvate and carbon dioxide. J. Biol. Chem. 235, PC17–PC18 (1960).
Scrutton, M.C. & White, M.D. Pyruvate carboxylase from rat liver: catalytic properties in the absence, and at low concentrations, of acetyl-CoA. Biochem. Biophys. Res. Commun. 48, 85–93 (1972).
McClure, W.R., Lardy, H.A. & Kneifel, H.P. Rat liver pyruvate carboxylase. I. Preparation, properties, and cation specificity. J. Biol. Chem. 246, 3569–3578 (1971).
Warren, G.B. & Tipton, K.F. Pig liver pyruvate carboxylase. The reaction pathway for the carboxylation of pyruvate. Biochem. J. 139, 311–320 (1974).
Sugden, M.C. & Holness, M.J. Recent advances in mechanisms regulating glucose oxidation at the level of the pyruvate dehydrogenase complex by PDKs. Am. J. Physiol. Endocrinol. Metab. 284, E855–E862 (2003).
Kitabchi, A.E. & Wall, B.M. Diabetic ketoacidosis. Med. Clin. North Am. 79, 9–37 (1995).
Minokoshi, Y., Toda, C. & Okamoto, S. Regulatory role of leptin in glucose and lipid metabolism in skeletal muscle. Indian J. Endocrinol. Metab. 16, S562–S568 (2012).
Toda, C. et al. Extracellular signal-regulated kinase in the ventromedial hypothalamus mediates leptin-induced glucose uptake in red-type skeletal muscle. Diabetes 62, 2295–2307 (2013).
Laker, R.C. et al. Central infusion of leptin does not increase AMPK signaling in skeletal muscle of sheep. Am. J. Physiol. Regul. Integr. Comp. Physiol. 300, R511–R518 (2011).
Previs, S.F., Cline, G.W. & Shulman, G.I. A critical evaluation of mass isotopomer distribution analysis of gluconeogenesis in vivo. Am. J. Physiol. 277, E154–E160 (1999).
Boden, G., Chen, X., Rosner, J. & Barton, M. Effects of a 48-h fat infusion on insulin secretion and glucose utilization. Diabetes 44, 1239–1242 (1995).
Dubuc, P.U. Basal corticosterone levels of young og/ob mice. Horm. Metab. Res. 9, 95–97 (1977).
Coleman, D.L. & Burkart, D.L. Plasma corticosterone concentrations in diabetic (db) mice. Diabetologia 13, 25–26 (1977).
Szücs, N. et al. Leptin inhibits cortisol and corticosterone secretion in pathologic human adrenocortical cells. Pituitary 4, 71–77 (2001).
Loose, D.S., Stover, E.P. & Feldman, D. Ketoconazole binds to glucocorticoid receptors and exhibits glucocorticoid antagonist activity in cultured cells. J. Clin. Invest. 72, 404–408 (1983).
da Silva, A.A., Tallam, L.S., Liu, J. & Hall, J.E. Chronic antidiabetic and cardiovascular actions of leptin: role of CNS and increased adrenergic activity. Am. J. Physiol. Regul. Integr. Comp. Physiol. 291, R1275–R1282 (2006).
Wang, J., Wernette, C.M., Judd, R.L., Huggins, K.W. & White, B.D. Guanethidine treatment does not block the ability of central leptin administration to decrease blood glucose concentrations in streptozotocin-induced diabetic rats. J. Endocrinol. 198, 541–548 (2008).
Hathout, E.H. et al. Changes in plasma leptin during the treatment of diabetic ketoacidosis. J. Clin. Endocrinol. Metab. 84, 4545–4548 (1999).
Kratzsch, J. et al. Metabolic decompensation in children with type 1 diabetes mellitus associated with increased serum levels of the soluble leptin receptor. Eur. J. Endocrinol. 155, 609–614 (2006).
Kitabchi, A.E. & Umpierrez, G.E. Changes in serum leptin in lean and obese subjects with acute hyperglycemic crises. J. Clin. Endocrinol. Metab. 88, 2593–2596 (2003).
Petersen, K.F. et al. Leptin reverses insulin resistance and hepatic steatosis in patients with severe lipodystrophy. J. Clin. Invest. 109, 1345–1350 (2002).
Perry, R.J. et al. Reversal of hypertriglyceridemia, fatty liver disease, and insulin resistance by a liver-targeted mitochondrial uncoupler. Cell Metab. 18, 740–748 (2013).
Erion, D.M. et al. The role of the carbohydrate response element-binding protein in male fructose-fed rats. Endocrinology 154, 36–44 (2013).
Alves, T.C. et al. Regulation of hepatic fat and glucose oxidation in rats with lipid-induced hepatic insulin resistance. Hepatology 53, 1175–1181 (2011).
Jurczak, M.J. et al. Dissociation of inositol-requiring enzyme (IRE1α)-mediated c-Jun N-terminal kinase activation from hepatic insulin resistance in conditional X-box-binding protein-1 (XBP1) knock-out mice. J. Biol. Chem. 287, 2558–2567 (2012).
Jucker, B.M., Rennings, A.J., Cline, G.W., Petersen, K.F. & Shulman, G.I. In vivo NMR investigation of intramuscular glucose metabolism in conscious rats. Am. J. Physiol. 273, E139–E148 (1997).
Hosokawa, Y., Shimomura, Y., Harris, R.A. & Ozawa, T. Determination of short-chain acyl-coenzyme A esters by high-performance liquid chromatography. Anal. Biochem. 153, 45–49 (1986).
Roughan, G. A semi-preparative enzymic synthesis of malonyl-CoA from [14C]acetate and 14CO2: labelling in the 1, 2 or 3 position. Biochem. J. 300, 355–358 (1994).
Kumashiro, N. et al. Role of patatin-like phospholipase domain-containing 3 on lipid-induced hepatic steatosis and insulin resistance in rats. Hepatology 57, 1763–1772 (2013).
Acknowledgements
We thank V. Samuel, D. Befroy and K. Petersen for helpful discussions and J. Dong, Y. Kosover, M. Kahn, B. Perler, J. Stack and M. Batsu for expert technical support. This study was funded by grants from the US National Institutes of Health (R01 DK-40936, R24 DK-085638, U24 DK-059635 and P30 DK-45735), an American Diabetes Association–Merck Clinical/Translational Science Postdoctoral Fellowship Award from the American Diabetes Association and the Novo Nordisk Foundation for Basic Metabolic Research.
Author information
Authors and Affiliations
Contributions
R.J.P. and G.I.S. designed the experimental protocols. R.J.P., X.-M.Z., D.Z., N.K., J.-P.G.C. and G.W.C. performed the studies. All authors contributed to the analysis of data. R.J.P. and G.I.S. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–9 and Supplementary Tables 1–2 (PDF 678 kb)
Supplementary Methods
Supplementary Methods (PDF 685 kb)
Rights and permissions
About this article
Cite this article
Perry, R., Zhang, XM., Zhang, D. et al. Leptin reverses diabetes by suppression of the hypothalamic-pituitary-adrenal axis. Nat Med 20, 759–763 (2014). https://doi.org/10.1038/nm.3579
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3579
This article is cited by
-
Arcuate AgRP, but not POMC neurons, modulate paraventricular CRF synthesis and release in response to fasting
Cell & Bioscience (2022)
-
Codon-optimized FAM132b gene therapy prevents dietary obesity by blockading adrenergic response and insulin action
International Journal of Obesity (2022)
-
Hepatic non-parenchymal S100A9-TLR4-mTORC1 axis normalizes diabetic ketogenesis
Nature Communications (2022)
-
Metformin effectively restores the HPA axis function in diet-induced obese rats
International Journal of Obesity (2021)
-
A neural basis for brain leptin action on reducing type 1 diabetic hyperglycemia
Nature Communications (2021)