Abstract
Prostaglandins (PGs) are ubiquitous lipid mediators derived from cyclooxygenase metabolism of arachidonic acid that exert a broad range of physiologic activities, including modulation of inflammation, ovulation1,2 and arterial blood pressure3,4. PGE2, a chief cyclooxygenase product, modulates blood pressure and fertility, although the specific G protein–coupled receptors5,6 mediating these effects remain poorly defined. To evaluate the physiologic role of the PGE2 EP2 receptor subtype, we created mice with targeted disruption of this gene (EP2–/–). EP2–/– mice develop normally but produce small litters and have slightly elevated baseline systolic blood pressure. In EP2–/– mice, the characteristic hypotensive effect of intravenous PGE2 infusion was absent; PGE2 infusion instead produced hypertension. When fed a diet high in salt, the EP2–/– mice developed profound systolic hypertension, whereas wild–type mice showed no change in systolic blood pressure. Analysis of wild–type and EP2–/– mice on day 5 of pregnancy indicated that the reduced litter size of EP2–/– mice is due to a pre–implantation defect. This reduction of implanted embryos could be accounted for by impaired ovulation and dramatic reductions in fertilization observed on day 2 of pregnancy. These data demonstrate that the EP2 receptor mediates arterial dilatation, salt–sensitive hypertension, and also plays an essential part in female fertility.
Similar content being viewed by others
Main
The EP2 receptor gene (Ptgerep2) was disrupted by replacing part of the N–terminal coding sequence with a PGK–neo cassette. Homologously targeted embryonic stem clones were obtained after electroporation of 129/SvEvTac–derived TL1 cells with the targeting vector. Chimeric mice derived from a correctly targeted embryonic stem cell clone were crossed with C57BL/6 mice, and the resulting EP2+/– heterozygous F1 littermates were bred to produce homozygous null mice, as confirmed by Southern analysis (data not shown). Breeding of heterozygous mice produced homozygous EP2–/– mice in a Mendelian distribution that was gender–independent: EP2+/+:EP2+/–:EP2–/– = 68:142:73 for males (χ2 = 0.18; P = 0.91, not significant) and 80:138:73 for females (χ2 = 1.11; P = 0.57, not significant). The absence of EP2 mRNA in EP2–/– mice was confirmed by RT–PCR using lung RNA as a template (data not shown). EP2–/– mice develop normally, are healthy, give birth with infant mortality rates (15%) similar to that of their heterozygote F1 parents (13%) and have lifespans of more than 1 year. No gross abnormalities were found in mutant mice in their general behavior or overall appearance, by macroscopic examination of their internal organs or from differential white cell count of their peripheral blood.
The role of the EP2 receptor in modulating blood pressure was assessed in anesthetized wild–type and EP2–/– mice by direct blood pressure measurement through a carotid arterial catheter. Bolus administration of butaprost7 (10 μg/kg), a selective EP2 receptor agonist, elicited a significant fall in mean arterial pressure (MAP) from 114.2 ± 4.2 mm Hg to a nadir of 99.0 ± 2.6 mm Hg in EP2+/+ mice (P < 0.05), whereas butaprost infusion failed to elicit this hypotensive response in EP2–/– mice (Fig. 1a). In contrast, cicaprost, a prostacyclin receptor selective agonist, elicited similar hypotensive responses in both wild–type and EP2–/– mice, demonstrating an intact vasodilator mechanism in EP2–/– mice (Fig. 1c). Administration of the endogenous ligand PGE2 (100 μg/kg) produced a hypotensive effect in wild–type mice, with MAP falling from 115.8 ± 6.3 mm Hg to 86.6 ± 5.5 mm Hg within 20 seconds of drug infusion. Hypotension was transient, and MAP recovered to baseline levels within 170 seconds after PGE2 administration. In contrast, EP2–/– mice responded to PGE2 infusion with considerable hypertension (maximum MAP 152.8 ± 7.4 mm Hg at 50 seconds after PGE2 administration) before returning to baseline values (Fig. 1b). Thus, the absence of the EP2 receptor abolishes the ability of the mouse vasculature to vasodilate in response to PGE2. The observed hypertensive response in EP2–/– mice may be because of unopposed activation of vascular populations of constrictor EP1 or EP3 receptors5. To determine whether this hypertensive response to PGE2 in EP2–/– mice might be because of increased sensitivity of these mice to the pressor effects of PGE2, we infused mice with sulprostone, an EP1/3–selective agonist8. In contrast to the results with PGE2, infusion of 10 μg/kg sulprostone resulted in an increase in MAP in both wild–type and EP2–/– mice. Moreover, the hypertensive effects of sulprostone were of similar magnitude in both EP2–/– and wild–type mice, indicating that the PGE2–mediated hypertension is not because of enhanced sensitivity of the EP vasoconstrictor receptors (Fig. 1c). Apparently, disruption of the EP2 receptor unmasks vasoconstrictor EP receptor subtypes, which predominate over other vasodilatory EP receptors (for example, EP4). These results demonstrate that the EP2 receptor mediates PGE2–dependent arterial dilatation in the mouse.
Mean arterial blood pressure was measured on anesthetized EP2+/+ (open squares and bars) and EP2–/– (filled squares and bars) mice by carotid artery catheterization. a, Mice received bolus administration of butaprost (10 μg/kg) through a catheter inserted into the jugular vein (n = 5). b, Mice received bolus administration of PGE2 (100 μg/kg) through a catheter inserted into the jugular vein (n = 5). c, Average change in mean arterial pressure in mice receiving bolus administration of either cicaprost (1 μg/kg) or sulprostone (10 μg/kg) through a catheter inserted into the jugular vein (n = 3). Baseline values were not affected in mice receiving vehicle alone (data not shown).
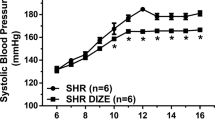
To determine whether the absence of the PGE2 vasodilator response was reflected in an altered baseline blood pressure in conscious mice, we measured tail–cuff blood pressure. There was a statistically significant increase in systolic blood pressure in female EP2–/– mice (8–16 weeks old) compared with that of F2 control mice (EP2+/+, 90 ± 2, n = 14; EP2–/–, 99 ± 3, n = 13; P < 0.02). Male mice had higher systolic blood pressures than did females, and although there was a slight increase in systolic blood pressure in EP2–/– mice compared with that of F2 wild–type control mice, this difference was not statistically significant (EP2+/+, 101 ± 3, n = 10; EP2–/–, 107 ± 2, n = 10; P = 0.09). Because the magnitude of hypertension may be influenced by dietary salt intake in some animal models and humans9, we assessed the effect of elevated salt intake on systolic blood pressure. Although there was no change in systolic blood pressure in wild–type F2 mice after they were switched to the high–salt diet (3.15% elemental Na+) from the control diet (0.25% elemental Na+), the EP2–/– mice experienced a rapid increase in blood pressure; it remained elevated while the mice were fed the high–salt diet (Fig. 2). This hypertension was quickly reversed by returning the mice to the control diet, and could be re–established by resumption of the high–salt diet. Urinary PGE2 production was increased in mice fed a high–salt diet, rising from 86 ± 24 ng/24 hours to 204 ± 26 ng/24 hours (P < 0.002) in EP2–/– mice, and from 93 ± 31 ng/24 hours to 202 ± 73 ng/24 hours (P < 0.08) in wild–type mice within 2 days of beginning the high–salt diet. These data indicate that absence of EP2 receptor activation by endogenous PGE2 contributes to salt–sensitive hypertension in EP2–/– mice. Unopposed EP1– and EP3–mediated vasoconstriction in the EP2–/– mice could contribute to the observed hypertension, particularly if PGE2 production were increased with a high–salt diet.
a, Systolic blood pressure (bp) was measured on conscious F2 EP2+/+ (open squares) and EP2–/– (filled squares) mice by tail cuff (n = 5 for each group). Mice were sequentially fed either control diet (open bars) or high–salt diet (shaded bars) during the periods indicated. b, Blood pressure (bp) data were averaged for the periods indicated (horizontal axis). Open squares, EP2+/+; filled squares, EP2–/–. *, P < 0.0001
Involvement of prostaglandins in regulating reproduction has been suggested10,11,12. Here, all EP2–/– female mice became pregnant when mated with EP2–/– male mice, but consistently delivered fewer pups than did their wild–type control counterparts (Table). In contrast to the pups of cPLA2–deficient mice, which also deliver smaller litter sizes, EP2–/– pups did not experience increased neonatal mortality13,14. The defect in EP2–/– fertility could not be attributed to the male, as the litter size of EP2+/+ and EP2+/– female mice was not influenced by the genotype of the father. The involvement of PGs in fertility has been suggested by studies demonstrating that the non–steroidal anti–inflammatory drug indomethacin inhibits ovulation11 and implantation in mice, rabbits and rats15,16,17. To determine whether the smaller litter size was due to a pre–implantation defect, or could be accounted for by fetal loss later in pregnancy, mice were mated and the number of implanted embryos was assessed at day 5 of pregnancy. EP2–/– females yielded significantly fewer implantation sites when mated with either wild–type males (4.4 ± 1.4 sites) or EP2–/– males (4.4 ± 0.6 sites) than did the wild–type females (7.4 ± 0.4 sites, P < 0.05, and 9.3 ± 3.0 sites, P < 0.004, for matings with wild–type and EP2–/– males, respectively). These results demonstrate that the small litter size observed with EP2–/– females may be attributed to a pre–implantation defect. Mice lacking cyclooxygenase–2 also have pre–implantation deficiencies, including impaired ovulation, fertilization and implantation18. To determine precisely the nature of the observed fertility defect, we mated mice with wild–type males, and assessed the number of eggs ovulated and fertilized at day 2 of pregnancy. Wild–type females released, on average, 12.2 ± 0.8 eggs per ovulation, 10.9 ± 0.8 of which were fertilized. In contrast, EP2–/– mice yielded only 8.7 ± 0.7 eggs per ovulation, 4.0 ± 1.0 of which were fertilized. These data indicate that the absence of the EP2 receptor results in partially defective ovulation and fertilization processes, thereby limiting the number of embryos available for implantation, which leads to the observed reduction in litter sizes. Our finding here that EP2–/– mice show abnormalities at several essential points early in the reproductive cascade indicates that decreased EP2 receptor activation may contribute to the reduction in fertility observed in cyclooxygenase–2–/– and cPLA2–/– mice. Clinical use of non–steroidal anti–inflammatory drugs has been associated with some cases of human infertility characterized by dysfunctional ovulation1. Thus, failure of EP2 receptor activation may contribute to the reversible infertility associated with such non–steroidal anti–inflammatory drug use.
These results demonstrate the importance of the EP2 receptor in blood pressure control and fertility. Our findings indicate that the EP2 receptor mediates the vasodilator effects of PGE2 as well as certain effects of this arachidonic acid metabolite during reproduction. The EP2 receptor may thus prove to be a productive target for pharmacological intervention in the treatment of hypertension and infertility.
Methods
Cloning of the murine EP2–receptor gene and construction of the targeting vector.
A 15.6–kb genomic DNA clone encoding the mouse EP2 receptor was isolated from a murine 129/Sv genomic library using as a probe a human EP2 cDNA (ref. 19)(provided by D. Gil, Allergan, Irvine, California). The genomic DNA clone, which was mapped with several restriction endonucleases, contains the 5' upstream (putative promoter) region and sequence from the ATG start codon to sequence within the receptor encoding the sixth transmembrane segment. A gene targeting vector was constructed from the murine genomic clone (λ–EP2) and its subcloned fragments as follows: pPNT, a targeting vector that contains neo and TK genes under control of 5' and 3' PGK sequence20, was digested with XbaI, 'filled in', and a 3.0–kb KpnI–SacI fragment was 'filled in' and cloned in immediately downstream of the neo gene. For the 5' homology segment, an 8–kb BamHI restriction fragment was cloned into the unique NotI–XhoI site upstream of the neo gene. The construct contains 8 kb of 5' homology, a deletion of 2.2 kb including 420 nt of the coding region from the ATG start codon to codon 140, and 3.0 kb of 3' homology.
Transformation of embryonic stem cells and selection of targeted cell clones.
TL1 cells (3.5 × 107) were electroporated with 120 μg of pPNT–EP2 DNA linearized with NotI. Colonies were selected using both G418 (200 μg/ml) and gancyclovir (2 μM), transferred onto 96–well plates and screened by Southern blot analysis with a 3' external SacI–XbaI probe after XbaI digestion. Additional Southern blot analysis using the neo probe after XbaI digestion demonstrated a lack of extra insertional events in these clones (data not shown).
Development of EP2–deficient mice.
Targeted cell lines were injected into C57BL/6 host blastocysts and implanted in pseudopregnant female recipients to generate chimeric mice. Chimeric male mice were bred to C57BL/6 females. Heterozygous F1 progeny carrying the disrupted EP2 gene were intercrossed to obtain F2 mice.
Tail–cuff blood pressure measurements.
Mouse blood pressure was measured using an IITC Life Science Model 27 cuff pump with a Model 179 blood pressure analyzer. Pressure was measured at 30 °C and was initiated as cuffs were inflated to 200 mm Hg and deflated at a rate of 3 mm Hg/sec. Mice were trained (for example, sham blood pressure measurements were taken to acclimate the mice to the procedure) for seven to ten days before actual data collection experiments. Measurements were obtained using male or female EP2+/+ and EP2–/– mice, 8–16 weeks old, weighing 20–35 g. Sessions 25 minutes in length were done once each day between 15:00 and 18:00, over a period of several days. For salt–loading studies, mice maintained on a control diet containing 0.25% elemental Na+ (Teklad, Madison, Wisconsin) were fed a high–salt diet containing 3.15% elemental Na+ (Teklad, Madison, Wisconsin). Diet changes were made in the evening immediately after blood pressure measurements and about 24 h before the next scheduled blood pressure measurement. Urinary PGE2 levels were determined by EIA (Oxford Biomedical Research, Oxford, Michigan) after collection of 24–hour urine output from mice (n = 5 for EP2–/–; n = 5 for wild–type) housed individually in diuresis cages (Nalgene, Rochester, New York).
Direct blood pressure measurements.
Female F2 EP2+/+ and EP2–/– mice 12–16 weeks old and 20–25 g in body weight were anesthetized using ketamine (100 μg/g) + inactin (100 μg/g) administered intraperitoneally, and were placed on a temperature–controlled table. After tracheostomy, PE10 tubing was inserted into the right carotid artery, a jugular vein catheter was also placed for infusion. Blood pressure was measured with a Cobe CDX II transducer connected to a blood pressure analyzer (Micro–med, Louisville, Kentucky). Blood pressure and heart rate were continuously monitored for 30–60 min until stable values were obtained. After the equilibration period, the test agent (for example, 100 μg/kg PGE2 or 10 μg/kg butaprost; 25 μl, injected intravenously) was administered, and vital signs were recorded for an additional 20 min. Cicaprost (1 μg/kg) and sulprostone (10 μg/kg) were similarly assessed using male F3 EP2+/+ and EP2–/– mice, 8–12 weeks old.
Fertility analysis.
For implantation studies, wild–type and EP2–/– F2 female mice were mated with either wild–type or EP2–/– F2 male mice, and the number of implantation sites were evaluated on day 5 of pregnancy. Before mice were killed, they were injected with Chicago blue B dye solution in saline18. Implantation sites were demarcated as localized blue bands along the uterine horns. For determination of ovulation and fertilization, wild–type (n = 9) and EP2–/– (n = 9) F2 female mice were mated with wild–type F2 male mice, and their oviducts were flushed on day 2 of pregnancy. Ovulated eggs were counted and were assessed for fertilization status either by appearance of a multi–celled embryo or the presence of two polar bodies.
Statistical analysis.
Reproductive genetics were evaluated by χ2 testing. Litter size and tail–cuff blood pressures were evaluated by unpaired Student's t–test. Statistical significance was given to comparisons with P < 0.05. Data are expressed as mean ± s.e.m.
References
Smith, G., Roberts, R., Hall, C. & Nuki, G. Reversible ovulatory failure associated with the development of luteinized unruptured follicles in women with inflammatory arthritis taking non–steroidal anti–inflammatory drugs. Br. J. Rheumatol. 35, 458– 462 (1996).
Downs, S.M. & Longo, F.J. Effects of indomethacin on preovulatory follicles in immature, superovulated mice. Am. J. Anatomy 164, 265–274 (1982).
Gurwitz, J.G. et al. Initiation of antihypertensive treatment during nonsteroidal anti–inflammatory drug therapy. J. Am. Med. Assoc. 272, 781–786 (1994).
Johnson, A.G. NSAIDs and increased blood pressure. What is the clinical significance? Drug Saf. 17, 277–289 (1997).
Coleman, R.A., Kennedy, I., Humphrey, P.P.A., Bunce, K. & Lumley, P. in Comprehensive Medical Chemistry (ed. Emmer, J.C.) 643–714 (Pergammon, Oxford,1990).
Coleman, R.A. et al. A novel inhibitory prostanoid receptor in piglet saphenous vein. Prostaglandins 47, 151– 168 (1994).
Gardiner, P.J. Characterization of prostanoid relaxant/inhibitory receptors (psi) using a highly selective agonist, TR4979. Br. J. Pharmacol. 87, 45–56 (1986).
Coleman, R.A., Kennedy, I. & Sheldrick, R.L.G. New Evidence with Selective Agonists and Antagonists for the Subclassification of PGE2 –sensitive (EP) Receptors. Adv. Prostaglandin Thromboxane Leukot. Res. 17, 467–470 (1987).
Simpson, F.O. in Hypertension: Pathophysiology, Diagnosis, and Management (eds. Laragh, J.H. & Brenner, B.M.) 273–280 (Raven, New York, 1995).
Challis, J.R.G. Prostaglandins and reproduction–what do knockouts really tell us? Nature Med. 3, 1326–1327 (1997).
Priddy, A.R. & Killick, S.R. Eicosanoids and ovulation. Prostaglandins Leukot. Essent. Fatty Acids 49, 827– 831 (1993).
Weitlauf, H.M. in The Physiology of Reproduction (eds. Knobil, E. & Neill, J.) pp 391–440 (Raven, New York, 1994).
Bonventre, J.V. et al. Reduced fertility and postischaemic brain injury in mice deficient in cytosolic phospholipase A2. Nature 390, 622–625 (1997).
Uozumi, N. et al. Role of cytosolic phospholipase A2 in allergic response and parturition. Nature 390, 618– 622 (1997).
Lau, I.F., Saksena, S.K. & Chang, M.C. Pregancy blockade by indomethacin, an inhibitor of prostaglandin synthesis: its reversal by prostaglandins and progesterone in mice. Prostaglandins 4, 795– 803 (1973).
Hoffman, L. Antifertility effect of indomethacin during early pregnancy in the rabbit. Biol. Reprod. 18, 148– 153 (1978).
Kennedy, T.G. Evidence for a role for prostaglandins in the initiation of blastocyst implantation in the rat. Biol. Reprod. 16, 286– 291 (1977).
Lim, H., Paria, B.C., Das, S.K., Dinchuk, J.E., Langenbach, R., Trzaskos, J.M., and Dey, S.K. Multiple female reproductive failures in cyclooxygenase 2–deficient mice. Cell 91, 197–208 (1997).
Regan, J.W. et al. Cloning of a novel human prostaglandin receptor with characteristics of the pharmacologically defined EP2 subtype. Mol. Pharmacol. 46, 213–220 (1994).
Tybulewicz, V. & Mulligan, R. Neonatal lethality and lymphopenia in mice with a homozygous disruption of the c–abl proto–oncogene. Cell 65, 1153–1163 (1991).
Acknowledgements
We thank A. George, T. Inagami and D. Threadgill for critical reading of the manuscript. Gene targeting and embryonic stem cell microinjection were done by the Vanderbilt Transgenic/ES Cell Shared Resource. Support for this project was provided in part by NIH grants GM–15431 (J.A.O. and R.M.B.), DK–46205 (R.M.B.) and DK–37097 (M.D.B.). C.R.J.K. is the recipient of an NKF fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kennedy, C., Zhang, Y., Brandon, S. et al. Salt–sensitive hypertension and reduced fertility in mice lacking the prostaglandin EP2 receptor. Nat Med 5, 217–220 (1999). https://doi.org/10.1038/5583
Issue Date:
DOI: https://doi.org/10.1038/5583
This article is cited by
-
Neuroinflammatory mediators in acquired epilepsy: an update
Inflammation Research (2023)
-
Metabolism pathways of arachidonic acids: mechanisms and potential therapeutic targets
Signal Transduction and Targeted Therapy (2021)
-
COX-2-derived PGE2 triggers hyperplastic renin expression and hyperreninemia in aldosterone synthase-deficient mice
Pflügers Archiv - European Journal of Physiology (2018)
-
Prostaglandins E2 signal mediated by receptor subtype EP2 promotes IgE production in vivo and contributes to asthma development
Scientific Reports (2016)
-
Prostaglandin E2 and programmed cell death 1 signaling coordinately impair CTL function and survival during chronic viral infection
Nature Medicine (2015)