Abstract
Many peptides and transmitters found within the brain also have peripheral sites of action. We now demonstrate that the brain releases functionally active neurotransmitters/neuromodulators directly from the brain into the blood through a saturable P-glycoprotein (Pgp) transport system. Downregulating Pgp1 expression with antisense reduced the brain-to-blood transport of morphine, β-endorphin and other opioids. Lowering Pgp expression significantly enhanced systemic morphine analgesia and prevented tolerance, but diminished the analgesic activity of centrally administered morphine, implying that supraspinal analgesia resulted from a combination of central and peripheral mechanisms activated by morphine transported from the brain to the blood. Similarly, mice with a disruption of the Mdr1a gene were more sensitive to systemic morphine and less sensitive to morphine given centrally. This ability of the Pgp transport system to pump functionally active compounds from the brain to periphery defines a potentially important mechanism for the central nervous system to modulate peripheral systems.
Similar content being viewed by others
Main
The brain can influence the physiology of a wide range of bodily functions, in large part through the autonomic and peripheral nervous systems. Hormonal activity of the pituitary provides yet another mechanism through which the central nervous system can modulate the activity of peripheral organs. If released systemically, a wide variety of additional peptides and transmitters contained within the brain could have important peripheral activities. The blood–brain barrier effectively isolates the brain from many compounds and drugs in the blood, but it may be unidirectional. For example, intracerebroventricular administration of 125I-tumor necrosis factor-α (TNFα) leads to long-lasting blood levels higher than levels following intravenous administration after the initial distribution phase1. The secretion of other cytokines from the brain to the systemic circulation has also been explored2. Interleukin-1β given intracerebroventricularly stimulates the generation of interleukin-6 within the brain, and its subsequent release into the blood3. The ability of the brain to secrete active peptides into the circulation may be a general mechanism, providing direct neurochemical links to sites outside the nervous system.
Highly selective systems have been proposed that can transport peptides from the brain into circulation4,5,6, but it seems unlikely that all neuro-active peptides would have their own transporter. Implicated in the blood–brain barrier is Pgp, which was originally identified in studies exploring the resistance of tumors to chemotherapeutic drugs7,8,9,10,11,12,13. Pgp is highly localized in endothelial cells of the brain14, and is involved in limiting the access of substrate drugs to the CNS15. Mice lacking Pgp display increased central sensitivity to agents given systemically12,16, including opioids17. Here we describe the brain-to-blood transport of a range of opioids by Pgp, and the pharmacological significance of this system.
Results
[125I]TNFα is rapidly secreted into the blood following intracerebroventricular administration1. To determine whether similar effects could be observed with other compounds, we examined a series of opioids. Following intracerebroventricular administration, [125I]β-endorphin, [125I]morphine, [125I]DAMGO and [125I]DPDPE all were secreted into the blood (Fig. 1). The rates of appearance and the duration of their presence in the blood varied markedly among the agents. [125I]DPDPE appeared most rapidly, reaching a peak within 5 minutes, and then rapidly declining to almost baseline level within 15 minutes. [125I]Morphine and [125I]DAMGO also quickly appeared in blood, but maintained their blood levels for at least two hours. [125I] β-Endorphin approached a maximal level most slowly. Because the blood levels reflect both release of the compound into the blood from the brain and the compound's elimination, it is difficult to accurately compare the rates and extent of release among the agents. However, the data clearly demonstrated the transport of all four compounds from the brain into the blood.
Rats (n ≥ 3) were implanted with cannulae in the lateral ventricle and in the jugular vein. [125I]β-endorphin, [125I]morphine, [125I]DPDPE or [125I]DAMGO (5–10 × 106 c.p.m.) were administered intracerebroventricularly, and venous blood samples were taken at the indicated times. The samples were centrifuged and aliquots of plasma (100 μl) counted for radioactivity. Greater than 70% of radioactivity corresponded to intact radiolabel.
The transport of these agents was saturable. Efflux of [125I] β-endorphin, [125I]morphine or [125I]DPDPE was competed in a dose-dependent manner by the corresponding unlabeled compound (Fig. 2). The median inhibitory dose (ID50; 95% confidence limits) of β-endorphin against [125I]β-endorphin was 30 μg (21.9, 41.9), whereas the ID50 of morphine against [125I]morphine was 95.3 μg (90, 101). In addition to blocking its own transport with an ID50 of 22.2 μg (19.2, 25.6), DPDPE also significantly lowered the efflux of [125I]morphine and competed [125I]β-endorphin (ID50, 19 μg; 8.3, 30.2) as potently as itself, implying that they shared a saturable transport system.
(a) Groups of rats (n ≥ 4) were given [125I]β-endorphin intracerebroventricularly following saline, or the indicated dose of β-endorphin (25–50 μg, i.c.v.) or DPDPE (15–50 μg, i.c.v.). Venous blood samples were taken at peak effect (60 min), and aliquots of plasma were counted. (b) Groups of rats (n ≥ 4) were given [125I]morphine intracerebroventricularly following saline, or the indicated dose of morphine (50–200 μg) or DPDPE (50 μg, i.c.v.). Venous blood samples were taken at 15 min and aliquots of plasma were counted. (c) Groups of rats (n ≥ 4) were given [125I]DPDPE intracerebroventricularly following either saline or DPDPE (12.5–50 μg, i.c.v.). Venous blood samples were taken at peak effect (1 min) and aliquots of plasma were counted.
Pgp is a transporter associated with the blood–brain barrier7,8,12,14,18,19,20,21,22,23. To explore whether Pgp is responsible for the transport of radiolabeled opioids, we targeted Pgp using antisense approaches effective against opioid receptors24,25,26,27,28 and Pgp29,30,31. Pgp is immunohistochemically demonstrated in the ventricular walls using both the C219 antibody (Fig. 3a and b) and the JSB1 antibody (data not shown). Of the three Pgp isoforms in the rat32,33, RT-PCR revealed only Pgp1 and Pgp3 in rat brain (Fig. 3e). An antisense probe directed against Pgp1, but not a corresponding mismatch probe, downregulated Pgp1 mRNA by greater than 50%, as determined with RT-PCR (Fig. 3f). All samples contained the predicted Pgp1 PCR fragment (350 bp), but the levels in the antisense-treated animals were reduced by 54%, as determined by counting the radioactivity in the bands. Immunohistochemically, the antisense treatment also markedly reduced the Pgp immunoreactivity around the edges of the lateral ventricles (Fig. 3c and d). Expression of Pgp in the rat choroid plexus could not be proven with certainty in these experiments, due to the possibility of contaminating tissue in the PCR studies, and the lack of absolute specificity of C219 antibody. However, the similar C219-antibody labeling of cells lining the ventricular wall that is readily seen in wild-type mice was absent in Mdr1a−/− mice (data not shown), further implying the specificity of labeling.
Sections of rat brain containing the choroid plexus were obtained and reacted with C219 antibody. Representative figures were obtained from control rats at low power (a) and high power (b) and from Pgp1 antisense-treated rats at low power (c) and high power (d). (e) RT-PCRs were done to determine the level of Pgp1, Pgp2 and Pgp3 mRNA expression in the rat frontal cortex (CTX), choroid plexus (CP), hippocampus (HIP), periaqueductal gray (PAG) and cerebellum (CRB). (f) Pgp1 mRNA expression was assessed using RT-PCR in control, Pgp1 antisense-treated and mismatch control rats. Loading was assessed by PCR of G3PDH, which gave the predicted 982 bp fragment in all lanes with equal intensity.
We then examined the ability of antisense probes against all three Pgp isoforms to influence the transport of [125I]β-endorphin (Fig. 4a). The Pgp1 antisense dramatically lowered the blood levels of [125I]β-endorphin by more than 75%, whereas its mismatch control and the antisense probes directed against Pgp2 and Pgp3 were ineffective. The curves were significantly different (F4,45 = 3.8; p < 0.0001). Post-hoc analysis (Dunnets) revealed that only the antisense targeting Pgp1 significantly decreased the secretion of [125I]β-endorphin (p < 0.001). The Pgp1 antisense also reduced the transport of [125I]DPDPE and [125I]morphine (Fig. 4b and c). The transport curves for [125I]morphine were significantly different (F20,99 = 3.84; p < 0.0001). Post-hoc analysis (Dunnets) revealed that only the antisense curve differed from the control (p < 0.05). Again, the mismatch control was inactive. Antisense significantly lowered the transport of [125I]DPDPE (F12,60 = 2.62, p < 0.007; post-hoc analysis, Dunnets), showing that only the antisense curve differed from the control (p < 0.01). [125I]DAMGO transport into the blood, as determined by the area under the time–action curve, was also significantly lowered by antisense treatment (p < 0.001; data not shown). Verapamil, a substrate for Pgp used as a Pgp inhibitor in many systems, given (2 μg, i.c.v.) before [125I]morphine-decreased efflux of the radiolabel by 78% (p < 0.001; Fig. 4d).
(a–c) Groups of rats (n ≥ 4) received saline or the indicated oligodeoxynucleotide (10 μg, i.c.v.) daily for five days. On day six, rats were injected with [125I]β-endorphin (i.c.v.; a), [125I]morphine (b) or [125I]DPDPE (c), and blood samples were taken at 1 min. (d) Groups of rats (n = 4) received saline (control) or verapamil (2 μg, i.c.v.) before [125I]morphine. Blood samples were taken at the indicated times.
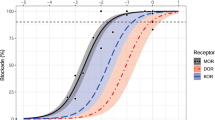
The Pgp transport system was pharmacologically relevant. Downregulation of Pgp1 enhanced the potency of systemic morphine, as indicated by the significant shift of the dose–response curve of the saline group (median effective dose, ED50, 4.6 mg/kg, s.c.; 1.7, 5.7) to the left following antisense (ED50, 0.99 mg/kg, s.c.; 0.5, 1.8), but not mismatch treatment (ED50, 4.6 mg/kg, s.c.; 4.3, 4.9; Fig. 5a). Lowering Pgp1 levels prolonged the duration of analgesia as determined by areas under the curve (p < 0.01) even when the morphine dose in the antisense-treated animals was lowered to achieve an equi-analgesic peak response to the saline and mismatch groups (Fig. 5b).
(a) Groups of rats (n ≥ 6) received either saline, Pgp1 antisense or mismatch. On day six, cumulative dose–response curves were determined. (b) Groups of rats (n ≥ 6) received either saline, Pgp1 antisense or mismatch. On day six, they received peak equi-analgesic doses of morphine (saline and mismatch, morphine, 6 mg/kg, s.c.; Pgp antisense, morphine, 2 mg/kg, s.c.), and analgesia was assessed at the indicated time. (c) Groups of rats (n ≥ 6) received either saline, Pgp1 antisense or mismatch. On day six, they started receiving peak equi-analgesic doses of morphine (saline and mismatch, morphine, 6 mg/kg, s.c.; Pgp1 antisense, morphine, 2 mg/kg, s.c.) daily along with either saline, antisense or mismatch (i.c.v.) and analgesia was assessed on the indicated days. (d) Groups of rats (n ≥ 6) received either saline, Pgp1 antisense or mismatch. On day six, they received the indicated morphine dose supraspinally.
Previous studies had implicated Pgp in morphine tolerance7. In our model, downregulating Pgp1 eliminated the tolerance seen in control and mismatch-treated animals following ten days of morphine treatment (Fig. 5c). The curves for the different groups over the ten days differed significantly (F10,54 = 16.14; p < 0.0001). Post-hoc analysis (Dunnets) revealed that the antisense group was significantly different (p < 0.05) from the other two.
A very different picture emerged when morphine was given intracerebroventricularly. Here, downregulating Pgp1 lowered morphine's analgesic effectiveness (Fig. 5d), significantly shifting the dose–response curve to the right, and suggesting that the transport of morphine from the brain into the blood was important in producing the analgesic response. The ED50 values were 2.4 μg, i.c.v. (1.5, 3.9) for saline, 28.2 μg, i.c.v. (16.7, 47.5) for the antisense group and 2.7 μg, i.c.v. (0.8, 9.2) for the mismatch group.
Potent, synergistic interactions exist between peripheral and central opioid mechanisms34,35. To examine whether peripheral opioid actions produced by the transport of the drug from the brain to the blood were involved, we examined whether topical naltrexone could reverse the analgesia produced by intracerebroventricular opioids. In this protocol, the tail was partially immersed in a naltrexone solution. Administered in this fashion, the actions of the drug are limited to only the region of the tail exposed to the solution34. The analgesic responses of morphine, β-endorphin and DPDPE given intracerebroventricularly were markedly diminished when tested on regions of the tail exposed to naltrexone, but not when tested on more proximal regions of the tail that were not exposed to naltrexone (Table 1). This difference confirmed that naltrexone was acting locally. Thus, the analgesia elicited by intracerebroventricular opioids was dependent upon both central and peripheral mechanisms. Downregulation of Pgp1 by antisense markedly reduced the analgesic potency of supraspinal morphine even more effectively than the topical application of naltrexone. The inability of naltrexone to antagonize the response further implied the absence of a peripheral mechanism in the antisense-treated animals. Thus, the supraspinal opioid analgesia depended upon the transport of the drug from the brain into the blood by Pgp1.
Similar results were seen in Mdr1a−/− mice. As in the rat antisense studies, systemic morphine was far more potent in the Mdr1a−/− animals (ED50, 2.1 mg/kg, s.c.) compared to wild-type mice (ED50 5.7 mg/kg, s.c.; p < 0.05; Fig. 6a), whereas morphine given centrally was significantly less active in the Mdr1a−/− mice (Fig. 6b). The response to supraspinal morphine in wild types was similar to the response in other control mice. The response in Mdr1a−/− mice was significantly lower than response in the wild-type mice (p < 0.001). As in rats, the decreased activity of central morphine in the Mdr1a−/− animals seemed to reflect the loss of a peripheral site of action. In wild-type mice, topical naltrexone reversed the analgesic activity of centrally administered morphine (0.7 μg, i.c.v.). In contrast, topical naltrexone was without effect against an equi-analgesic dose of centrally administered morphine in the Mdr1a−/− mice (2.1 μg, i.c.v.).
(a) A cumulative dose–response curve was generated for both the wild-type (ED50, 5.7 mg/kg, s.c.; 4.5, 7.2) and the Mdr1a−/− animals (ED50, 2.1 mg/kg, s.c.; 1.5, 2.9). (b) Groups of wild-type and Mdr1a−/− mice received morphine supraspinally (0.7 μg, i.c.v.). Baseline values were approximately 2.6 s for all groups before drug administration. (c) Wild-type (0.7 μg, i.c.v.) and Mdr1a−/− mice (2.1 μg, i.c.v.) received equi-analgesic doses of morphine supraspinally. Fifteen minutes later, the distal portion of their tails were immersed in a naltrexone solution, and tail-flick latencies were determined on the region exposed to naltrexone and a more proximal control region that had not been exposed to naltrexone. Baseline values were approximately 2.6 s for all groups before drug administration.
Discussion
The brain has long been considered a privileged site because of the blood–brain barrier, which prevents the entry of many systemic agents into the brain. Pgp helps to maintain the blood–brain barrier, as evidenced by the increased entry of a variety of compounds in mice in which the Pgp gene has been disrupted12,22. Pgp has broad substrate specificity, actively transporting many natural products and drugs, including many important anti-neoplastic agents. Structurally, Pgp is localized on the luminal surface of endothelial cells, a site suitable for modulating the blood–brain barrier14,18,23,36. However, evidence suggests that the blood–brain barrier is unidirectional. For example, the protein [125I]TNF does not pass into the brain to an appreciable degree when given intravenously. Yet, it is rapidly excreted from the brain into the blood1. The current study reveals a saturable transport system involving Pgp1 that can secrete a wide range of structurally diverse and pharmacologically active compounds from the brain to the systemic circulation.
Unlike transport systems proposed earlier that are highly selective for specific compounds6, the Pgp system described here secretes a number of agents differing widely in their sizes and structures. The system is saturable, and the various compounds can compete with each other for secretion from the ventricular system into the blood. Antisense approaches established the importance of Pgp1 in this action. Antisense oligodeoxynucleotides effectively downregulated the levels of both Pgp 1 mRNA and protein, which, in turn, reduced the efflux of the compounds from the brain into the circulation. These findings were consistent with the ability of the Pgp inhibitor verapamil to block the efflux of [125I]morphine into the blood.
Similar results were found in studies in a mouse model in which the Mdr1a gene had been disrupted. Systemic morphine was more potent in Mdr1a−/− mice, but absence of Pgp1 left Mdr1a−/− mice less sensitive to centrally administered morphine. As in the rat model, this decreased activity in the Mdr1a−/− mice reflected the loss of a peripheral site of action following central drug, as shown by the inability of topical naltrexone to inhibit the analgesic response in the Mdr1a−/− mice as it did in the wild-type controls.
The Pgp1 transport system is functionally relevant. Earlier studies suggested that morphine transport into the brain was important in tolerance37, and Pgp was subsequently shown to be involved7. Our findings support these earlier observations. Downregulation of Pgp1 enhanced both the potency and duration of action of systemic morphine, and blocked the development of tolerance. However, the importance of Pgp transcends its involvement in maintaining the blood–brain barrier. Its active transport of compounds out of the brain into the circulation was crucial for the analgesic actions of a series of centrally administered opioids. The ability of topical naltrexone to block these actions established a peripheral effect, and the loss of naltrexone's actions in Mdr1a−/− mice or following antisense in the rat confirmed the role of Pgp1. The levels of opioid in the blood following central administration are likely to be quite low, but the presence of potent, synergistic interactions between peripheral and central opioid systems likely explains their pharmacological importance34.
In conclusion, our findings demonstrate that the brain has the ability to secrete a wide range of peptides and drugs into the circulation. Although the current studies focused upon opioids, this transport system will likely involve a far wider range of compounds. Thus, the Pgp transport system may provide a general mechanism for communication between the central nervous system and the periphery through the secretion of peripherally acting peptides and hormones, and may help explain the physiological interactions between the mind and body.
Methods
[d-Pen2, d-Pen5]enkephalin (DPDPE), β-endorphin, [d-Ala2, MePhe4,Gly(ol)5]enkephalin, morphine and naltrexone were gifts from the Research Technology Branch of the National Institute on Drug Abuse (Rockville, Maryland). Antisense oligodeoxynucleotides were designed from rat sequences, synthesized by Midland Certified Reagent (Midland, Texas), purified in our laboratory and administered in 0.9% saline. Ketamine was purchased from Fort Dodge Laboratories (Fort Dodge, Iowa) and Na[125I] from New England Nuclear (Boston, Massachusetts). All other compounds were purchased from the Sigma Chemical (St. Louis, Missouri). Peptides were iodinated at room temperature with a tenfold excess of peptide, and the reaction was terminated with sodium metabisulfite, as previously described38,39. [125I]β-endorphin and [125I]DPDPE were purified by HPLC over a C18 reverse-phase column, using an acetonitrile/0.1% trifluoroacetic acid gradient.
Male Sprague-Dawley rats (250–275 g; Charles River Laboratories, Wilmington, Massachusetts) and male Mdr1a−/− mice and wild-type controls (Taconic Farms) were maintained on a 12-h light/dark cycle with food and water available ad libitum. Wild-type (FVB/N) and Mdr1a−/− mice (FVB/Ntac-Pgy1tm1N7) were purchased from Taconic Farms. All studies were reviewed and approved by the Institutional Animal Care and Use Committee (IACUC) of Memorial Sloan-Kettering Cancer Center. Intracerebroventricular (i.c.v.) cannulae were implanted as previously described40,41 and the animals were allowed one week to recover from the surgery. Blood (200 μl) was sampled at the indicated times in tubes containing EDTA (70 μl, 0.2 mM) from indwelling jugular vein catheters placed under anesthesia 2 days before testing. Samples were centrifuged and aliquots (100 μl) of plasma were counted. In the competition studies, the unlabeled compounds were injected immediately before the radiolabel42,43.
Reverse transcriptase-polymerase chain reactions (RT-PCRs) were done to determine the level of Pgp1, Pgp2 and Pgp3 mRNA expression. Total cytoplasmic RNA from indicated regions plexus of treated rats was isolated and purified by the Ultraspec RNA isolation system (Biotecx Laboratories, Houston, Texas). Complementary DNA (cDNA) was generated from total RNA at 37EC for 1 h using 200 ng random hexamer oligonucleotide, 200 U of SuperScript II reverse transcriptase (GibcoBRL, Grand Island, New York), 10 mM dNTP and 0.1 M DTT in a reaction volume of 20 μl. Oligodeoxynucleotide primers were designed from the rat P-glycoprotein sequence (Pgp1, sense primer, 5′-CTGTCACAAAGGAAAGCATTTAGTCC-3′, nt 379–404; antisense primer, 5′-GACCCCTCCCCCATAGACTAAGTTTT-3′, nt 763–738, GenBank #X61103; Pgp2, sense primer, 5′ AGAGGGCCTTAACGGAAGAGCA-3′, nt 114–135; antisense primer, 5′-GCTCGGTCAGAATGCGGGTC-3′, nt 365–346, GenBank #M81855; Pgp3, sense primer 5′-CCTGGACGGCGACTTTGAACTA-3′, nt 70–92; antisense primer 5′-CATGGCGGTGCCCAGGAGC-3′, nt 212–194, GenBank #L15079). The cDNA was amplified in a Perkin-Elmer thermal cycler 480 for 35 cycles using T. aquaticus polymerase (Sigma) in the presence of α32P-dCTP (New England Nuclear). Each cycle consisted of a melting step (45 s at 94EC), an annealing step (45 s at 60EC) and an extension step (60 s at 72EC). Products were analyzed on a 2% agarose gel. We used rat glyceraldehyde 3-phosphate dehydrogenase (G3PDH) (sense primer, 5′-TGAAGGTCGGTGTCAACGGATTTGGC-3′, nt 35–60; antisense primer, 5′-CATGTAGGCCATGAGGTCCACCAC-3′, nt 1017–994; Clontech, Palo Alto, California) as an internal standard.
In the antisense studies, rats received five daily doses of oligodeoxynucleotide (10 μg in 2 μl, i.c.v.) or vehicle. The Pgp1 antisense (GenBank #X61103; GGACTAAATGCTTTCCTTTGTGACAG; nt 123–145), the Pgp 2 antisense (GenBank #M81855; AGCAGCGAGAGTTCCCAGAGCC; nt 249–270) and the PGP3 antisense (GenBank #L15079; CATGGCGGTGCCCAGGAGC; nt 193–211) were each unique to their respective isoforms. On the sixth day, animals received the [125I]peptides (5–10 × 106 c.p.m., i.c.v.) and 200 μl blood samples were taken from the jugular catheter at the indicated times in tubes containing EDTA (70 μl, 0.2 mM). Samples were centrifuged, and aliquots (100 μl) of plasma counted. In the competition studies, the unlabeled compounds were injected immediately before the radiolabel was injected. Changes in Pgp mRNA levels were examined using RT-PCR, as previously described44.
Immunohistochemistry was done as previously described45. In brief, rats were perfused transcardially with 0.1 M phosphate-buffered saline and fixed with 4% formaldehyde in phosphate buffer. The brain was removed and placed in 4% formaldehyde solution for 2 h at room temperature, transferred to 30% sucrose, and stored at 4EC overnight. Sections (40 μm) were preincubated at room temperature for 30 min in 3% NGST (normal goat serum triton) and then incubated at room temperature overnight with antibody C219 (1:5000; Centocor, Malvern, Pennsylvania) or JSB-1 (Synbio, Uden, The Netherlands). The sections were washed with 1% NGST, incubated with the secondary anti-mouse IgG antibody (Vector Laboratories, Burlingame, California) at room temperature for 1 h, washed with phosphate buffer/saline, incubated with Elite ABC (Vector Laboratories) at room temperature for 1 h and washed with PB45. These sections were reacted at room temperature with nickel-DAB until the background increases and washed with PB.
Analgesia was assessed in the radiant heat tail-flick assay, as previously described46,47,48. Baseline latencies typically ranged from 2–3 s, and a cutoff of 10 s was used to minimize tissue damage in analgesic animals. To assess the involvement of peripheral mechanisms, the distal portion of the tail was immersed in a DMSO solution containing naltrexone (3 mM) to see if this reversed the analgesic response. This topical approach provides a pharmacological effect localized only to the region of the tail exposed to the solution34,39. We then did the tail-flick test over the region exposed to the naltrexone. As a control, we then tested a more proximal region of the tail that was not exposed. Analyses of variances (ANOVA) were done to determine overall significance. Bonferroni post-hoc comparisons were then made (p > 0.05) to examine individual differences in the groups. ED50 values were determined by a computer program based upon the Litchfield–Wilcoxin approach50.
References
Bodnar, R. J. et al. Mediation of anorexia by human, recombinant Tumor Necrosis Factor thorugh a peipheral action in the rat. Cancer Res. 49, 6280–6284 (1989).
Goodman, J. C., Robertson, C. S., Grossman, R. G. & Narayan, R. K. Elevation of tumor necrosis factor in head injury. J. Neuroimmunol. 30, 213–217 (1990).
Romero, L. I., Kakucska, I., Lechan, R. M. & Reichlin, S. Interleukin-6 (IL-6) is secreted from the brain after intracerebroventricular injection of IL-1β in rats. Am. J. Physiol. 270, R518–R524 (1996).
Banks, W. A. & Kastin, A. J. Saturable transport of peptides across the blood–brain barrier. Life Sci. 41, 1319–1338 (1987).
Banks, W. A., Kastin, A. J. & Ehrensing, C. A. Endogenous peptide Tyr-Pro-Trp-Gly-NH2 (Tyr-W-MIF-1) is transported from the brain to the blood by peptide transport system-1. J. Neurosci. Res. 35, 690–695 (1993).
Banks, W. A. & Kastin, A. J. Passage of peptides across the blood–brain barrier: pathophysiological perspectives. Life Sci. 59, 1923–1943 (1996).
Aquilante, C. L., Letrent, S. P., Pollack, G. M. & Brouwer, K. L. R. Increased brain P-glycoprotein in morphine tolerant rats. Life Sci. 66, L47–L51 (1999).
Chen, C. P. & Pollack, G. M. Enhanced antinociception of the model opioid peptide [d-Penicillamine2,5] enkephalin by P-glycoprotein modulation. Pharm. Res. 16, 296–301 (1999).
Egleton, R. D. & Davis, T. P. Transport of the δ-opioid receptor agonist [d-penicillamine2,5] enkephalin across the blood–brain barrier involves transcytosis. J. Pharm. Sci. 88, 392–397 (1999).
Jonker, J. W. et al. Role of blood–brain barrier P-glycoprotein in limiting brain accumulation and sedative side-effects of asimadoline, a peripherally acting analgaesic drug. Br. J. Pharmacol. 127, 43–50 (1999).
Letrent, S. P., Pollack, G. M., Brouwer, K. R. & Brouwer, K. L. R. Effects of a potent and specific P-glycoprotein inhibitor on the blood–brain barrier distribution and antinociceptive effect of morphine in the rat. Drug Metab. Dispos. 27, 827–834 (1999).
Schinkel, A. H.et al. Disruption of the mouse mdrla P-glycoprotein gene leads to a deficiency in the blood–brain barrier and to increased sensitivity to drugs. Cell 77, 491–502 (1994).
Xie, R. J., Hammarlund-Udenaes, M., De Boer, A. G. & De Lange, E. C. M. The role of P-glycoprotein in blood–brain barrier transport of morphine: transcortical microdialysis studies in mdr1a (−/−) and mdr1a (+/+)mice. Br. J. Pharmacol. 128, 563–568 (1999).
Cordon-Cardo, C. et al. Multidrug-resistance gene (P-glycoprotein) is expressed by endothelial cells at blood-barrier sites. Proc. Natl. Acad. Sci. USA 86, 695–698 (1989).
Beaulieu, E., Demeule, M., Ghitescu, L. & Beliveau, R. P-glycoprotein is strongly expressed in the luminal membranes of the endothelium of blood vessels in the brain. Biochemistry 326, 539–544 (1997).
Schinkel, A. H., Wagenarr, E., Van, D. L., Mol, C. A. & Borst, P. Absence of the mdrla P-Glycoprotein in mice affects tissue distribution and pharmacokinetics of dexamethasone, diagoxin and cyclosporin A. J. Clin. Invest. 96, 1698–1705 (1995).
Thompson, S. J., Koszdin, K. & Bernards, C. M. Opiate-induced analgesia is increased and prolonged in mice lacking P-glycoprotein. Anesthesiology 92, 1392–1399 (2000).
Hegmann, E. J., Bauer, H. C. & Kerbel, R. S. Expression and functional activity of P-glycoprotein in cultured cerebral capillary endothelial cells. Cancer Res. 52, 6969–6975 (1992).
Chen, C. P. & Pollack, G. M. Altered disposition and antinociception of [d-Penicillamine2,5] enkephalin in mdr1a-gene-deficient mice. J. Pharmacol. Exp. Ther. 287, 545–552 (1998).
Tatsuta, T., Naito, M., Oh-hara, T., Sugawara, I. & Tsuruo, T. Functional involvement of P-glycoprotein in blood–brain barrier. J. Biol. Chem. 267, 20383–20391 (1992).
Schinkel, A. H. et al. Multidrug resistance and the role of P-glycoprotein knockout mice. Eur. J. Cancer 31A, 1295–1298 (1995).
Schinkel, A. H., Wagenaar, E., Mol, C. A. & Van Deemter, L. P-glycoprotein in the blood–brain barrier of mice influences the brain penetration and pharmacological activity of many drugs. J. Clin. Invest. 97, 25617–22524 (1996).
Regina, A. et al. Mrp1 multidrug resistance-associated protein and P-glycoprotein expression in rat brain microvessel endothelial cells. J. Neurochem. 71, 705–715 (1998).
Standifer, K. M., Chien, C.-C., Wahlestedt, C., Brown, G. P. & Pasternak, G. W. Selective loss of δ opioid analgesia and binding by antisense oligodeoxynucleotides to a δ opioid receptor. Neuron 12, 805–810 (1994).
Pan, Y.-X. et al. Cloning and functional characterization through antisense mapping of a kappa 3-related opioid receptor. Mol. Pharmacol. 47, 1180–1188 (1995).
Standifer, K. M. et al. Antisense oligodeoxynucleotides to the cloned δ receptor, DOR-1: uptake, stability and regulation of gene expression. J. Neurochem. 65, 1981–1987 (1995).
Standifer, K. M., Rossi, G. C. & Pasternak, G. W. Differential blockade of opioid analgesia by antisense oligodeoxynucleotides directed against various G-protein α subunits. Mol. Pharmacol. 50, 293–298 (1996).
Kolesnikov, Y. A. et al. Functionally differentiating two neuronal nitric oxide synthase isoforms through antisense mapping: Evidence for opposing NO actions on morphine analgesia and tolerance. Proc. Natl. Acad. Sci. USA 94, 8220–8225 (1997).
Gao, Z. Q., Gao, Z. P., Fields, J. Z. & Boman, B. M. Co-transfection of MDR1 and MRP antisense RNAs abolishes the drug resistance in multidrug-resistant human lung cancer cells. Anticancer Res. 18, 3073–3076 (1998).
Motomura S. et al. Inhibition of P-glycoprotein and recovery of drug sensitivity of human acute leukemic blast cells by multidrug resistance gene (mdr1) antisense oligonucleotides. Blood 91, 3163–3171 (1998).
Wang, L. W., Chen, L. X., Walker, V. & Jacob, T. J. C. Antisense to MDR1 mRNA reduces P-glycoprotein expression, swelling-activated Cl− current and volume regulation in bovine ciliary epithelial cells. J. Physiol. (Lond.) 511, 33–44 (1998).
Gottesman, M. M., Hrcyna, C. A., Schoenlein, P. V., Germann, U. A. & Pastan, I. Genetic analysis of the multidrug transporter. Annu. Rev. Genet. 29, 607–649 (1995).
Roninson, I. B. in Molecular and Cellular Biology of Multidrug Resistance in Tumor Cells Ch. p (ed. Roninson, I. B.) 189–211 Plenum, New York, 1991).
Kolesnikov, Y. & Pasternak, G. W. Topical opioids in mice: analgesia and reversal of tolerance by a topical N-methyl-d-aspartate antagonist. J. Pharmacol. Exp. Ther. 290, 247–252 (1999).
Kolesnikov, Y. A., Jain, S., Wilson, R. & Pasternak, G. W. Peripheral morphine analgesia: synergy with central sites and a target of morphine tolerance. J. Pharmacol. Exp. Ther. 279, 502–506 (1996).
Pardridge, W. M., Golden, P. L., Kang, Y. S. & Bickel, U. Brain microvascular and astrocyte localization of P-glycoprotein. J. Neurochem. 68, 1278–1285 (1997).
Roerig, S. C., O'Brien, S. M., Fujimoto, J. A. & Wilcox, G. L. Tolerance to morphine analgesia: decreased multiplicative interaction between spinal and supraspinal sites. Brain Res. 308, 360–363 (1984).
Mathis, J. P. et al. Biochemical evidence for orphanin FQ/nociceptin receptor heterogeneity in mouse brain. Biochem. Biophys. Res. Commun. 230, 462–465 (1997).
Pan, Y.-X. et al. Dissociation of affinity and efficacy in KOR-3 chimeras. FEBS Lett. 395, 207–210 (1996).
Rossi, G. C., Pasternak, G. W. & Bodnar, R. J. μ and δ opioid synergy between the periaqueductal gray and the rostro–ventral medulla. Brain Res. 665, 85–93 (1994).
Rossi, G. C., Pasternak, G. W. & Bodnar, R. J. Synergistic brainstem interactions for morphine analgesia. Brain Res. 624, 171–180 (1993).
Ling, G. S. F., Spiegel, K., Lockhart, S. H. & Pasternak, G. W. Separation of opioid analgesia from respiratory depression: evidence for different receptor mechanisms. J. Pharmacol. Exp. Ther. 232, 149–155 (1985).
Ling, G. S. F., Spiegel, K., Nishimura, S. & Pasternak, G. W. Dissociation of morphine's analgesic and respiratory depressant actions. Eur. J. Pharmacol. 86, 487–488 (1983).
Pan, Y.-X., Cheng, J., Xu, J. & Pasternak, G. W. Cloning, expression and classification of a kappa3-related opioid receptor using antisense oligodeoxynucleotides. Regul. Pept. 54, 217–218 (1994).
Rohde, D. S., McKay, W. R., Chang, D. S., Abbadie, C. & Basbaum, A. I. The contribution of supraspinal, peripheral and intrinsic spinal circuits to the pattern and magnitude of Fos-like immunoreactivity in the lumbar spinal cord of the rat withdrawing from morphine. Neuroscience 80, 599–612 (1997).
Rossi, G., Leventhal, L., Bolan, E. A. & Pasternak, G. W. Pharmacological characterization of orphanin FQ/nociceptin and its fragments. J. Pharmacol. Exp. Ther. 282, 858–865 (1997).
Rossi, G. C., Brown, G. P., Leventhal, L., Yang, K. & Pasternak, G. W. Novel receptor mechanisms for heroin and morphine-6β-glucuronide analgesia. Neurosci. Lett. 216, 1–4 (1996).
King, M. A., Rossi, G. C., Chang, A. H., Williams, L. & Pasternak, G. W. Spinal analgesic activity of orphanin FQ/nociceptin and its fragments. Neurosci. Lett. 223, 113–116 (1997).
Kolesnikov, Y. A. & Pasternak, G. W. Peripheral blockade of topical morphine tolerance by ketamine. Eur. J. Pharmacol. 374, R1–R2 (1999).
Tallarida, R. J. & Murray, R. B. Manual of Pharmacological Calculations with Computer Programs (Springer, New York, 1987).
Acknowledgements
This work was supported, in part, by research grants (DA02615 and DA07242) and a Senior Scientist Award (DA00220) to G. W. P. and a training grant (T32DA07274) to M. K. and W. S. from the National Institute on Drug Abuse, and a core grant from the National Cancer Institute (CA08748) to M.S.K.C.C.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
King, M., Su, W., Chang, A. et al. Transport of opioids from the brain to the periphery by P-glycoprotein: peripheral actions of central drugs. Nat Neurosci 4, 268–274 (2001). https://doi.org/10.1038/85115
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/85115
This article is cited by
-
Essential role of P-glycoprotein in the mechanism of action of oliceridine
Neuropsychopharmacology (2023)
-
Synthesis of the Mechanisms of Opioid Tolerance: Do We Still Say NO?
Cellular and Molecular Neurobiology (2021)
-
Candidate gene analyses for acute pain and morphine analgesia after pediatric day surgery: African American versus European Caucasian ancestry and dose prediction limits
The Pharmacogenomics Journal (2019)
-
An observational study examining the effects of a surgically induced inflammatory response on the distribution of morphine and its metabolites into cerebrospinal fluid
Canadian Journal of Anesthesia/Journal canadien d'anesthésie (2017)