Key Points
-
Despite the introduction 40 years ago of the inexpensive and effective four-drug (isoniazid, rifampicin, pyrazinamide and ethambutol) treatment regimen, tuberculosis (TB) continues to cause significant morbidity and mortality worldwide.
-
After five decades of near inactivity in TB drug development, the past 5 years has seen the development of a promising TB drug pipeline. For the first time since the 1960s, new and novel drugs and regimens for all forms of TB are emerging.
-
Several new TB drug candidates are in Phase II and Phase III clinical trials in addition to high activity in the hit-to-lead and lead optimization stages.
-
New TB drug development has led to the submission of two new TB drugs for regulatory approval: delamanid (also known as OPC67683) and bedaquiline (also known as TMC207 or R207910).
-
The US Food and Drug Administration recently approved bedaquiline as part of a combination therapy in the treatment of adults with multidrug-resistant TB.
-
New TB treatment regimens aimed at reducing the duration of chemotherapy or for use against drug-resistant TB using new chemical entities are now progressing through clinical trials.
-
Many of the candidates in clinical trials are drugs that were developed to treat other infectious diseases and have since been repurposed for TB (for example, fluoroquinolones, rifamycins, oxazolidinones and clofazimine).
-
Several newer approaches are currently being pursued with the aim of reducing the time required for evaluating new TB drugs through the various phases of clinical trials. These include the use of 14-day early bactericidal activity (EBA) studies to rapidly determine bactericidal activity, the use of innovative trial designs that include multi-arm, multi-stage determinations of efficacy of new drug combinations, and the exploration and qualification of new surrogate markers of treatment effect.
-
To facilitate this more rapid evaluation of new TB drugs, current clinical trials are initially testing new combinations of TB drugs in patients with drug-susceptible pulmonary TB.
-
This article covers current concepts and recent advances in TB drug discovery and development, including an update of ongoing TB treatment trials, newer clinical trial designs, TB biomarkers and adjunct host-directed therapies.
Abstract
Despite the introduction 40 years ago of the inexpensive and effective four-drug (isoniazid, rifampicin, pyrazinamide and ethambutol) treatment regimen, tuberculosis (TB) continues to cause considerable morbidity and mortality worldwide. For the first time since the 1960s, new and novel drugs and regimens for all forms of TB are emerging. Such regimens are likely to utilize both repurposed drugs and new chemical entities, and several of these regimens are now progressing through clinical trials. This article covers current concepts and recent advances in TB drug discovery and development, including an update of ongoing TB treatment trials, newer clinical trial designs, TB biomarkers and adjunct host-directed therapies.
Similar content being viewed by others
Main
Human tuberculosis (TB) is caused by infection with members of the Mycobacterium tuberculosis complex, which includes Mycobacterium tuberculosis itself, Mycobacterium africanum, Mycobacterium bovis, Mycobacterium caprae, Mycobacterium microti, Mycobacterium pinnipedii and Mycobacterium canettii1,2. Patients with active pulmonary TB are the main sources of infection and the majority of people infected with M. tuberculosis contain it as asymptomatic latent TB infection (LTBI). An estimated 2 billion people have LTBI and are at risk of re-activation of the disease1,3,4. TB continues to spread in every corner of the globe despite the introduction 40 years ago of the inexpensive and effective quadruple drug therapy regimen5 (Box 1).
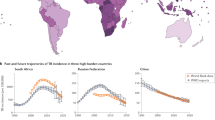
The seventeenth World Health Organization (WHO) report on the worldwide incidence of TB6 indicates that TB remains a global emergency. It estimates that in 2011 there were 8.7 million new cases and 1.4 million deaths from TB, including 350,000 deaths associated with co-infection with HIV. Sub-Saharan Africa has the highest rates per capita of TB, which is driven primarily by the HIV epidemic in that region. India, China, South Africa and the Russian Federation have almost 60% of the world's TB cases6. In the United States and Western Europe most cases of TB occur in residents from countries in which TB is highly endemic7,8. Multidrug-resistant TB (MDR-TB) is now widespread globally with an estimated half a million cases reported in 2011, and extensively drug-resistant TB (XDR-TB) has been reported in 84 countries. Owing to constraints in resources and inadequate laboratory infrastructure, only 19% (or 60,000 cases) of the total estimated numbers of MDR-TB cases worldwide were notified to the WHO in 2011 and less than 4% of MDR-TB cases are currently diagnosed worldwide.
TB treatment is challenging, requiring accurate and early diagnosis, drug-resistance screening and the administration of effective treatment regimens for at least 6 months through directly observed therapy (DOT) and follow-up support. There is an urgent need for the development and more efficient evaluation of new TB drugs and shorter treatment regimens. Over the past 10 years, significant investment by scientists, funding bodies and high-profile advocacy by the WHO's STOP TB department, and other organizations, has led to a renaissance of activity in the discovery and development of new TB drugs and TB treatment regimens. These efforts have culminated in historic advances in TB therapeutics, including the recent submissions to regulatory agencies for approval of two new drugs: delamanid (previously known as OPC67683) and bedaquiline (also known as TMC207 or R207910). The US Food and Drug administration (FDA) used its regulatory path for accelerated review of limited efficacy data on drugs to approve bedaquiline (Sirturo; Janssen Therapeutics)9 as part of combination therapy in the treatment of adults with MDR-TB when other alternatives are not available. This Review covers current concepts and recent advances in TB drug discovery, development and clinical trial evaluation, and provides an update of ongoing, planned and recently completed treatment trials.
Current tuberculosis treatment regimens
Drug-susceptible tuberculosis. Nearly 60 years following the identification of the first antibiotic active against M. tuberculosis (Box 1), the current recommended treatment of drug-susceptible TB is of at least 6 months duration and achieves cure rates of >95% when administered under DOT. Treatment requires a minimum of 6 months in two phases: 2 months of four drugs (isoniazid, rifampicin, pyrazinamide and ethambutol) in the intensive phase followed by 4 months of isoniazid plus rifampicin in the continuation stage (the so-called short-course chemotherapy). This regimen is currently implemented for pulmonary TB and most forms of extrapulmonary TB regardless of HIV status10,11.
However, several issues can complicate the treatment of TB in patients with HIV (Box 2). M. tuberculosis bacilli exist in a spectrum of replication states, from metabolically active and relatively rapid replicators (doubling time approximately 24 hours) to nearly dormant non-replicating persisters12. Isoniazid has particularly high early bactericidal activity (EBA), typically causing a 1–1.5 log10 decline in colony-forming units during the first 5 days of therapy. While active replicators are efficiently and quickly killed during the first days to few weeks of therapy, 6 months of treatment with currently available drugs is required to eradicate the non-replicating persisters of M. tuberculosis bacilli.
However, there are significant challenges associated with current therapy including the following: drug intolerance and toxicities, with the resultant need for treatment interruptions and changes to the regimen; pharmacokinetic drug–drug interactions, particularly with antiretroviral therapy (ART) drugs in patients co-infected with TB and HIV; and patient adherence given the lengthy treatment duration necessary to achieve non-relapsing cure. In HIV-infected individuals pharmacokinetic interactions with HIV drugs result in intolerance, loss of efficacy and toxicities.
No new TB drug classes have been developed or approved for drug-susceptible TB since the current 6-month four-drug combination was introduced in the 1970s. The absence for decades of concerted drug development and new combinations has paradoxically paved the way for the introduction of fixed-dose combinations of two (isoniazid and rifampicin), three (isoniazid, rifampicin and pyrazinamide) and four (isoniazid, rifampicin, pyrazinamide and ethambutol) drugs13. Given that most of the world's TB burden is caused by drug-susceptible strains of M. tuberculosis, the above two, three and four fixed-dose combinations13 have been introduced in an attempt to decrease the emergence of resistance and to improve ease of administration. However, challenges with the existing standard treatment regimen remain and continue to impede progress in global TB control. Significant effort is being invested in drug development for drug-susceptible TB, particularly for new regimens that are shorter in duration, better tolerated and with fewer drug–drug interactions14.
Multidrug-resistant-TB. The WHO estimates that only 10% of the annual 650,000 incident cases of MDR-TB worldwide receive high-quality, appropriate treatment and management. Ideally, treatment of MDR-TB requires 'individualized' regimens based on in vitro drug-susceptibility testing (DST) results for each patient's isolate15. In areas where facilities for M. tuberculosis culture are available, culture-based systems for first-line DST do not provide results for several weeks, and for second-line DST the results are frequently not available for several months. The choice of TB drugs is determined by the following factors: the pattern of drug resistance in the local geographical region; which drugs have been taken previously by the patient; whether the patient has underlying medical conditions; and the adverse effects associated with the drug. DST is not available for over 95% of patients with MDR-TB and the majority of cases are missed or treated empirically on suspicion of active TB. Patient groups for which empirical treatment for MDR-TB is considered, and offered, include those in whom TB treatment is failing (that is, who remain culture-positive after 4 months of treatment), any persons with recurrent TB, persons in contact with drug-resistant cases of TB, and persons who were born in countries, or reside in settings, where drug-resistant TB is highly prevalent.
The newly introduced Xpert MTB/RIF Assay is a diagnostic test that can be used with minimal technical expertise, enabling rapid diagnosis of TB and simultaneous assessment of rifampicin resistance within 2 hours16,17. The test is fully automated and utilizes molecular beacon technology to detect DNA sequences amplified in a hemi-nested real-time PCR assay. The Xpert MTB/RIF assay provides a high sensitivity initial screen for MDR-TB and the WHO recommends that patients with rifampicin-resistant TB should receive MDR-TB therapy pending additional DST. High sensitivity for rifampicin resistance is accompanied by some false-positive results, requiring confirmatory drug sensitivity testing. Widespread implementation is underway in Africa and Asia and this is likely to increase the dectection of MDR-TB cases and increase the proportion of cases starting MDR-TB treatment.
The 2011 WHO MDR-TB treatment guidelines recommend that the intensive phase of therapy is administered for at least 8 months for patients newly diagnosed with MDR-TB (that is, not previously treated for MDR-TB)15. Regimens should include at least four second-line drugs (Box 3) that will have nearly certain effectiveness and be given on a daily basis under DOT throughout the treatment duration. Total duration of therapy should be for at least 20 months when there is no history of previous MDR-TB treatment, and 28 months if there was previous MDR treatment. Pyrazinamide (Group 1; Box 3) and an injectable drug (Group 2; Box 3) are given only during the intensive phase. Durations for each phase should be modified according to the patient's response to therapy. Group 3 (Box 3) contains the fluoroquinolones (discussed in more detail below), of which moxifloxacin and levofloxacin are most active. The optimal dose for each is not clearly established, although moxifloxacin is widely dosed at 400 mg daily and levofloxacin at 750 mg daily. Studies are currently planned to further refine the optimal dose of levofloxacin in MDR-TB. Other approved second-line drugs for MDR-TB treatment included in Group 4 and Group 5 (Box 3) have either weak or unclear bacteriostatic activity, many of which also have very high rates of side effects and intolerance. As such, drugs in these groups are generally reserved for patients with MDR-TB for whom options available in forming an adequate treatment regimen are limited. Linezolid (an oxazolidinone) and clofazimine (a riminophenazine) are two drugs in Group 5 that are undergoing additional investigation to better define their safety, tolerability and efficacy as potential repurposed drugs for MDR-TB (Fig. 1).
Chemical structures of anti-infective agents that were initially developed for the treatment of other diseases that are now being evaluated for tuberculosis treatment. Note that sutezolid is also known as PNU-100480.
Extensively drug-resistant tuberculosis. XDR-TB takes substantially longer to treat than MDR-TB and requires the use of third-line anti-TB drugs, which are expensive and often have more side effects than first-line or second-line drugs. XDR-TB is associated with high mortality rates and in HIV-infected persons these may reach 100% if treatment commences too late18,19. In certain settings, aggressive and comprehensive management can achieve cure rates of up to 60% of patients infected with XDR-TB but not HIV20. Drug resistance beyond the definition of XDR-TB has been described and illustrates the urgent need for new drugs for drug-resistant TB21.
Totally drug-resistant tuberculosis. Some recent reports use the term totally drug-resistant TB (TDR-TB) to describe TB caused by M. tuberculosis strains that are resistant to all available first-line and second-line TB drugs22. In March 2012, the WHO convened an expert consultation that identified numerous concerns about this newly proposed categorization for highly drug-resistant TB, including poor reproducibility of DST results for second-line drugs across various microbiology laboratories, even those with significant expertise23. In addition, worldwide, few laboratories can accurately perform DST on all second-line and third-line drugs. Labelling patients as having TDR-TB is likely to generate additional and unnecessary stigma, and as such should be avoided, particularly given the serious concerns raised by the WHO. Moreover, since new drugs are being developed and evaluated to combat drug-resistant strains of M. tuberculosis, and many drugs are being repurposed, the categorization will soon become obsolete.
New anti-tuberculosis drug development
There are well-defined criteria for developing new TB drug candidates24,25,26. In addition to a fully validated safety profile, there are a number of other factors that a new TB drug should fulfil: be more potent than existing drugs in order to reduce the duration of therapy; should inhibit new targets so that MDR-TB and XDR-TB can be treated; be compatible with ART, as many patients are co-infected with HIV; and show no antagonism to other TB drugs or drug candidates so that a regimen comprising at least three active drugs can be constituted. There is also a growing awareness of the need for drugs that can kill M. tuberculosis in its different physiological states including LTBI27.
After five decades of near inactivity in TB drug development, the past 5 years has seen the emergence of a promising TB drug pipeline (Fig. 2). Combining these new drugs with existing TB drugs offers hope for regimens that are better tolerated, shorter in duration and with fewer drug–drug interactions when compared with existing regimens. A number of new therapeutic agents are concurrently under investigation and new treatment regimens are in clinical trials (Table 2).
Agents currently in discovery or development for the treatment of tuberculosis (TB) are shown. Ongoing projects without a lead compound series can be viewed at the Working Group on New TB Drugs — Discovery Portfolio website (see Further information). GLP, good laboratory practice; InhA, enoyl-CoA reductase; LeuRS, leucyl-tRNA synthetase.
There are several candidates in Phase II and Phase III clinical trials (Fig. 2) together with much activity in the hit-to-lead and lead optimization stages. There is, however, a worrying gap corresponding to late preclinical development and Phase I clinical trials that needs to be addressed in order to maintain a continuum of clinical activity and to compensate for possible attrition among the more advanced candidates. Drug candidates are typically first appraised for human efficacy in EBA studies, in which a reduction in the number of viable bacteria in sputum is measured during 0–2 days (classical EBA study, representing a measure of rapid killing of metabolically active bacilli) and 2–14 days (extended EBA study, hypothesized to potentially capture a drug's slower sterilizing activity) of treatment with the candidate drug before initiating appropriate combination therapy in newly diagnosed patients with smear-positive pulmonary TB28,29. Subsequently, through the conduct of Phase II trials, time to conversion of sputum cultures to negativity and the proportion of patients with culture-negative sputa after 2 months of treatment are often used as indicators of drug efficacy.
Many of the candidates currently in clinical trials are drugs that were developed to treat other infectious diseases (for example, fluoroquinolones, rifamycins, oxazolidinones and riminophenazines) and have since been repurposed (Fig. 1). As these repurposed compounds have generally been well-described elsewhere, they will only be discussed briefly here. Host-directed therapies, including drugs that are currently used for the treatment of rheumatological, parasitic and cardiovascular diseases, also have potential for adjunct TB treatment (Box 4).
Other drugs that were initially discovered as anti-mycobacterial agents and have subsequently been developed as potential TB drugs, including bedaquiline — recently approved by the FDA for use as part of combination therapy for adults with MDR pulmonary TB9 — the nitroimidazoles (PA-824 and OPC67683) and SQ109 are discussed below under new chemical entities. Several additional novel compounds are in preclinical development for TB (Fig. 2), including the nitroimodazole TBA-354, the fluoroquinolone DC-159a, the dipiperidine SQ609, the capuramycin SQ641, the benzothiazinone BTZ043 and the caprazene nucleoside CPZEN-45 (Fig. 2). Some of these novel compounds were back-ups from existing chemical families, but no details on their specific characteristics have been published.
Repurposed compounds
Fluoroquinolones. Fluoroquinolones target DNA gyrase and DNA topoisomerase in many bacteria and are frequently used for the treatment of MDR-TB as components of second-line regimens. Interest in their use as possible first-line drugs was renewed when it was shown that fluoroquinolones had the potential to reduce the duration of therapy in murine models of TB30.
Gatifloxacin and moxifloxacin (Fig. 2) are currently in Phase III clinical trials to establish whether drug-susceptible TB can be effectively treated in 4 months by substituting gatifloxacin for ethambutol, or moxifloxacin for ethambutol or isoniazid31. Since fluoroquinolones are broadly available, and used to treat many infectious diseases, concern has arisen regarding the development of drug resistance in patients with undiagnosed TB who are being treated with fluoroquinolones for other conditions. To counter this, efforts are underway to identify new inhibitors that are not based on the fluoroquinolone pharmacophore as DNA gyrase is a well-validated target.
Rifamycins. Rifampicin, which has been the backbone of TB chemotherapy for 40 years, targets the beta subunit of RNA polymerase, thereby preventing transcription. Rifapentine (Figs 1, 2), another rifamycin, acts in the same way but has a much longer half-life than rifampicin, so achieves better exposure and thus has the potential toshorten treatment duration32.
In a large, multicentre, non-inferiority clinical trial for LTBI conducted by the CDC TB Trials Consortium, a 3-month regimen containing rifapentine and isoniazid proved to be non-inferior at preventing progression to tuberculosis disease and was better tolerated than the current standard treatment of isoniazid for 9 months33. Several Phase II clinical trials are in progress, in which rifampicin is replaced by high-dose rifapentine, to assess its potential to shorten the treatment duration of drug-susceptible TB. Administering rifapentine daily, two or three times per week instead of once a week128, leads to higher rifapentine exposures and appears to be well tolerated. Based on the findings of a promising EBA study34, the possibility of shortening treatment duration through the use of higher rifampicin doses than the current 600 mg per day is also being investigated by several groups, including in a Phase II clinical trial (HIGHRIF, which is a series of studies; Table 2). A meta-analysis35 and a systematic review129 each revealed that the optimal dose for rifampicin had never been established and the HIGHRIF trial is thus testing higher doses of rifampicin. However, a major drawback of rifamycins is that they induce cytochromes P450 in the liver, which lead to drug–drug interactions with antiretroviral agents (particularly protease inhibitors) and other TB drug candidates such as bedaquiline36. There is therefore significant interest in developing rifamycin-free regimens.
Clofazimine. A meta-analysis of studies that used the leprosy drug clofazimine (Fig. 1) repurposed for TB treatment showed that it could have a major part to play in the treatment of MDR-TB37. An observational study evaluated the effectiveness of standardized regimens for patients with proven MDR-TB previously untreated with second-line drugs38. The most effective treatment regimen — achieving a relapse-free cure of 87.9% among 206 patients — required a minimum of 9 months of treatment with clofazimine, gatifloxacin, ethambutol and pyrazinamide throughout the treatment period supplemented by prothionamide, kanamycin and high-dose isoniazid during an intensive phase of a minimum of 4 months.
Clofazimine administration via the aerosol route using microparticles was effective in the treatment of a mouse model of TB39. This route of administration could potentially reduce the gastrointestinal and dermatological (skin discolouration) side effects of clofazimine. Clofazimine was also found to be active in a murine model of LTBI40, which suggests that it might have wider treatment applications. The optimal dose of clofazimine, duration and route of administration require further investigation.
Oxazolidinones. Oxazolidinones are a new class of drugs that inhibit protein synthesis by binding to the 23S rRNA in the 50S ribosomal subunit of bacteria. Linezolid, a first-generation oxazolidinone (Fig. 1), shows tuberculostatic activity in vitro and modest activity in murine models of TB41,42. Early off-label trials of linezolid in combination regimens suggested that the drug was effective against MDR-TB42 and definitive proof for this was recently obtained in a prospective, randomized clinical trial in patients with XDR-TB43. Linezolid was effective at achieving culture conversion but 82% of patients also had clinically significant adverse events, including neuropathy and myelosuppression that were thought to be linezolid-related. Patients who received 300 mg per day had fewer adverse events than those who received 600 mg per day throughout the study. The immediate addition of linezolid at a dose of 600 mg per day to background treatment regimens improved the time to sputum-culture conversion on solid medium, as compared with the delayed addition of linezolid; 34 out of the 39 patients (87%) had confirmed culture conversion within the 6 months of treatment. Notably, acquired linezolid resistance manifested in four patients in two forms: as mutations in either the 23S rRNA or the rplC genes43, which suggests that the drug interacts with both these ribosomal components. Apart from peripheral neuropathy and myelosuppression, several other serious side effects of linezolid occur, such as thrombocytopaenia and optic neuritis44.
Sutezolid (also known as PNU-100480; Fig. 1), a linezolid analogue that has stronger bactericidal activity in the murine model than linezolid, is currently in Phase II clinical trials45,46. Combination studies have been performed in whole-blood assays and these showed that sutezolid and TMC207 or SQ109 had additive effects, whereas those including PA-824 were less than additive or antagonistic47. These data are encouraging for the development of new combination therapies. AZD5847, a next-generation oxazolidinone, is bactericidal and acts like linezolid, as M.tuberculosis mutants that are resistant to AZD5847 harbour mutations in the genes encoding 23S rRNA and RplC. AZD5847 is not antagonistic with other TB drugs and has completed Phase I trials48.
Meropenem plus clavulanate combination. M. tuberculosis is naturally resistant to β-lactam antibiotics, such as meropenem, as it produces an efficient β-lactamase, BlaC, which hydrolyses them. Recently, it was elegantly demonstrated that inhibition of BlaC by clavulanate could lead to M. tuberculosis becoming susceptible to meropenem49. Meropenem acts by inhibiting dd-carboxypeptidase activity, thereby perturbing peptidoglycan biosynthesis50. Meropenem and clavulanate (Fig. 1) are both approved drugs and this combination has been used with some success, in conjunction with other drugs, to treat patients with MDR-TB and XDR-TB51,52. However, although the pharmacokinetic properties of meropenem (such as a short half-life) preclude its general use for TB treatment, this work49,50 has identified a vulnerable target that merits further exploration.
New chemical entities
Bedaquiline. The newly approved drug bedaquiline, a diarylquinoline (Fig. 3), inhibits the c subunit of ATP synthase, thereby decreasing intracellular ATP levels36. Bedaquiline was discovered using phenotypic screening and its target identified using whole-genome sequencing of M. tuberculosis mutants that spontaneously developed bedaquiline resistance36. These mutants harboured missense mutations in the atpE gene, which encodes the ATP synthase c subunit, and the substitutions D32V and A63P were associated with resistance. The c proteins oligomerize to form the c-ring, a component of the F0 subunit of ATP synthase, and bedaquiline is thought to act by interfering with the proton translocation step required for ATP production53. The human mitochondrial ATP synthase is 20,000-fold less sensitive to bedaquiline than its mycobacterial counterpart and this augurs well for tolerability54.
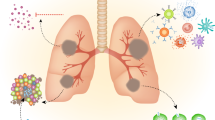
A simplified version of the cell envelope and the cytoplasmic membrane of Mycobacterium tuberculosis is shown together with schematized versions of the targets (where known) of chemical structures of drug candidates, lead compounds and hits discussed in the article. TMC207 (also known as bedaquiline) primarily targets the c-ring portion of the F0 subunit of ATP synthase. Nitroreduction of PA-824 and OPC67683 (also known as delamanid) by F420-deazaflavin-dependent nitroreductase (Ddn) releases nitric oxide, which is thought to inhibit cytochrome oxidase and other targets. There are two distinct cytochrome oxidases in M. tuberculosis119, the bioenergetically efficient aa3-type cytochrome c oxidase supercomplex (CtaCDE) and the cytochrome bd quinol oxidase (CydAB), which has a higher affinity for oxygen, but these are not distinguished in the figure. MmpL3 is involved in export of trehalose monomycolate, a mycolic acid component, and it has been shown that SQ109 and AU1235 inhibit trehalose monomycolate export76,78. BM212 and C215 are thought to work by inhibiting trehalose monomycolate export, but studies have yet to definitively demonstrate this. However, mutant M. tuberculosis strains resistant to BM212 and C215 harbour mutations in mmpL3. DPR epimerase comprises two subunits E1 and E2 that catalyse the conversion of decaprenyl-phosphoryl-d ribose (DPR) to decaprenyl-phosphoryl-d arabinose (DPA) the arabinan donor for arabinogalactan. DPA is thought to be exported by a flippase, shown as a barrel, but evidence for this is lacking. BTZ043, DNB1, VI-9376 and 377790 all form covalent bonds with a cysteine residue within the active site of DprE1, thus blocking the first step in the epimerization reaction84.
A more extensive molecular genetic study of 53 spontaneously acquired bedaquiline-resistant mutants of clinical isolates revealed that in 15 mutants, five different point mutations were present in the atpE gene (D28V, D28P, E61D, A63P and I66M)55. In the remaining 38 mutants, no atpE mutations were found and this suggests that either the drug has another target or that there is a second resistance mechanism, such as drug efflux or detoxification, but, as yet, no details of this are available55. More recent studies56 using NMR spectroscopy generated a low-resolution solution structure of the epsilon subunit of the F1F0 ATP synthase of M. tuberculosis, which, together with the gamma subunit, couples the F1F0 components. Using various biophysical and biochemical methods it was shown that bedaquiline also binds to the epsilon subunit. A model has been proposed whereby bedaquiline forms a wedge between the epsilon subunit and the c-ring56, and this model should facilitate the design of additional ATP synthase inhibitors.
An attractive feature of bedaquiline is its equipotent activity against both replicating and dormant M. tuberculosis bacilli57, and an explanation for this was provided by Rao et al.58, who showed that de novo ATP synthesis is essential for the viability of nonreplicating mycobacteria. This bacterial subpopulation is highly susceptible to bedaquiline in vitro, a finding that was subsequently confirmed by others using a novel murine model of LTBI55. Bedaquiline kills both drug-susceptible and drug-resistant M. tuberculosis strains, displaying minimal inhibitory concentrations equal to or lower than those of isoniazid and rifampicin. Unusually, after a classical EBA study involving patients with drug-susceptible pulmonary TB, bedaquiline was then tested in a Phase II trial on newly diagnosed MDR-TB cases59, thus establishing a new clinical paradigm that is attracting greater clinical interest. The addition of bedaquiline to standard therapy for MDR-TB reduced the time to culture conversion and greatly increased the proportion of patients whose sputum became culture-negative59. The clinical activity of bedaquiline validates ATP synthase as a highly vulnerable target of M. tuberculosis. Another remarkable feature of bedaquiline is its unusually long half-life, a desirable feature for inclusion of this drug in an intermittent regimen60. However, bedaquiline also accumulates in tissues, therefore care must be taken to avoid carry-over effects when measuring its activity61. Bedaquiline has a black-box warning due to its potential to induce arrhythmia9.
Nitroimidazoles. Nitroimidazole compounds, such as the classic metronidazole, were first investigated as TB drugs because of their known activity against anaerobic microorganisms, and anaerobiosis is thought to lead to LTBI21. Metronidazole kills M. tuberculosis in vitro under hypoxic but not aerobic conditions and displays widely contrasting effects in different animal models, ranging from good efficacy in the rabbit, with its caseous granulomas, to no efficacy in mice or guinea pigs. In a recent study involving cynomolgus macaques that present with active TB and LTBI, metronidazole treatment prevented reactivation of LTBI62. Furthermore, when used in conjunction with isoniazid and rifampicin, metronidazole helped shorten the length of treatment required to cure active TB in monkeys62.
Two newer nitroimidazoles, PA-824 (Ref. 63) and OPC67683 (now known as delamanid)64 (Fig. 3) are in clinical development, and, like metronidazole, both are prodrugs. PA-824 is activated intracellularly by an F420-deazaflavin-dependent nitroreductase (Ddn) present in M. tuberculosis65. The active form of PA-824 is the corresponding des-nitroimidazole, which, in turn, can generate reactive nitrogen species, including nitric oxide (NO), that are the major effectors of its anaerobic activity66. The activity of PA-824 is restricted to the M. tuberculosis complex; for example, M. leprae is not susceptible because the ddn gene has been deleted from its genome67. Many PA-824-resistant laboratory mutants of M. tuberculosis have lost the ability to produce the F420 cofactor and their Ddn nitroreductase is therefore inactive62. Such mutants display cross-resistance to OPC67683 and an unrelated class of compounds known as nitrofuranylamides68, which suggests that F420-deazaflavin-dependent nitroreduction may be a frequent activation mechanism for nitroaromatic drugs in M. tuberculosis.
Gene expression profiling analysis of the mode of action of PA-824 uncovered a mixed signature involving genes responsive to both cell wall inhibition and poisoning of the respiratory chain69. The aerobic killing mechanism of PA-824 has been suggested to stem from inhibition of mycolic acid biosynthesis, whereas the anaerobic killing mechanism is probably the result of NO poisoning of cytochrome c oxidase69. PA-824 has progressed to Phase II trials and is being assessed as a component of novel regimens (see below)70,71.
Delamanid is a nitro-dihydro-imidazooxazole that was first shown to be active against M. tuberculosis in vitro and then in mice64. Its mechanism of action is probably through inhibiting mycolic acid biosynthesis64 and it also kills intracellular tuberculosis bacilli. Like PA-824, delamanid requires nitroreduction by Ddn for activation; mutants lacking this enzyme are resistant to delamanid and unable to produce the des-nitro-imidazooxazole form64,65,66,67,68. It seems probable that delamanid, which is more potent than PA-824, also kills by producing NO or an as yet unidentified radical, and that this acts randomly within M. tuberculosis. PA-824 and delamanid, are currently in Phase II (PA-824) and Phase III (delamanid) clinical trials, respectively for the treatment of MDR-TB (Table 2).
The EBA of delamanid was established in a trial involving 48 patients with smear-positive TB who received 100 mg, 200 mg, 300 mg or 400 mg daily for 14 days72. The EBA of delamanid was found to be monophasic, with no significant difference between dosages although patients receiving 200 mg or 300 mg showed a stronger sputum decline. Subsequently, the efficacy of delamanid was assessed in a randomized, placebo-controlled, multi-centred clinical trial of patients with MDR-TB in which sputum culture conversion after 2 months was used as an end point. The two groups receiving delamanid at 100 mg or 200 mg twice a day showed a substantially increased rate of sputum-culture conversion compared to the control group who received placebo plus the background MDR-TB regimen73. However, QT prolongation was reported at a significantly higher frequency in patients receiving delamanid, thus suggesting that there is a risk of cardiotoxicity with delamanid. In a recent study, delamanid improved treatment outcome and reduced mortality among MDR-TB and XDR-TB patients when used with an optimized background regimen74.
SQ109 and other MmpL3 inhibitors. It is widely acknowledged that ethambutol is the weakest component of DOT and therefore ripe for replacement by a more potent drug. Attempts were made to synthesize more powerful diamine derivatives using combinatorial chemistry and these efforts resulted in the identification of SQ109 (Fig. 3), a novel 1,2-ethylenediamine-based analogue, from a library of over 60,000 compounds75. Insight into its mode of action recently became available and SQ109 was shown to target MmpL3, an essential membrane protein belonging to the resistance, nodulation and division (RND) family76. The role of MmpL3 is to transport trehalose monomycolate into the cell envelope and SQ109 inhibits mycolic acid biogenesis instead of arabinogalactan, the known mechanism of action of ethambutol. Combining SQ109 with bedaquiline is synergistic in vitro, thereby improving an already excellent minimal inhibitory concentration for M. tuberculosis H37Rv for bedaquiline by fourfold to eightfold, as well as the bactericidal rate over that of SQ109 and bedaquiline given alone77. The synergistic effects probably result from SQ109 weakening the cell wall thereby allowing bedaquiline to reach ATP synthase more efficiently. SQ109 is currently in Phase II clinical trials.
The development of SQ109 illustrates the capricious nature of TB drug targets and rational approaches to drug discovery. This is further underlined by the finding that several other lead compounds also inhibit MmpL3, thus preventing translocation of trehalose monomycolates. The best characterized of these compounds is the adamantyl urea derivative AU1235 (Fig. 3), a bactericidal compound whose activity is limited to mycobacteria78. There is structural resemblance between SQ109 and AU1235, which might explain their common activity, whereas two other compounds that seemingly inhibit MmpL3, the pyrrole derivative BM212 (Ref. 79) and C215 (N-(2,4-dichlorobenzyl)-1-propyl-1H-benzo[d]imidazol-5-amine)80 are completely unrelated to SQ109 (Fig. 3). It is intriguing that inhibitors of MmpL3 have such diverse chemical structures, and this raises the possibility that, in addition to exporting trehalose monomycolate, MmpL3 may also act as a drug efflux pump, as in each case resistant mutants raised against the compounds harboured missense mutations in the mmpL3 gene. More work, including cross-resistance studies, is required to unravel this issue.
Benzothiazinones. Benzothiazinones (Fig. 3) are the most potent inhibitors of M. tuberculosis yet described and display low nanomolar bactericidal activity against mycobacteria growing in vitro and in ex vivo models81. In murine models of acute or chronic TB, the preclinical candidate BTZ043 showed efficacy comparable with that observed with isoniazid and rifampicin. BTZ043 is active against drug-susceptible, MDR and XDR clinical isolates of M. tuberculosis82. Most importantly, when BTZ043 was used in combination with other TB drugs or drug candidates (rifampicin, isoniazid, ethambutol, bedaquiline, PA-824, moxifloxacin, meropenem (with or without clavulanate), and SQ-109) no antagonism was found. Almost all of the interactions elicited additive effects, but synergy was observed when BTZ043 was combined with bedaquiline83.
The mechanism of action of benzothiazinones is understood at the atomic level and its target, the essential enzyme decaprenylphosphoryl-beta-d-ribose 2′-epimerase (DprE1), has been extensively characterized81,84,130. The flavoenzyme DprE1 catalyses the conversion of decaprenyl-phosphoryl-d-ribose to decaprenyl-phosphoryl-d-arabinose, the sole arabinose precursor for the synthesis of the critical mycobacterial cell wall components arabinogalactan and lipoarabinomannan. BTZ043 undergoes nitroreduction by the reduced form of DprE1 to form a nitroso-species that covalently binds to a cysteine residue in the active site, thereby quantitatively and irreversibly inactivating DprE1 (Refs 85,86). Benzothiazinone derivatives are therefore suicide substrates and BTZ043 is now at the good laboratory practice toxicology stage of preclinical development.
Recently, three other series of nitroaromatic compounds were reported to be DprE1 inhibitors (Fig. 3) and these all target the same cysteine residue as BTZ043. These are the dinitrobenzamides (DNB1)87, benzoxyquinoxalines (VI-9376)88 and the novel nitro-substituted triazole 377790 (Ref. 77) (Fig. 3). DprE1 therefore appears to be a highly vulnerable target of M. tuberculosis with broad-spectrum nitroreductase activity; further nitroaromatic inhibitors may be found by whole-cell screening of chemical libraries.
Ongoing clinical trials for new regimens
A selection of ongoing, completed and planned clinical trials for both drug-susceptible and resistant TB are shown in Table 2. On the basis of preclinical data, new TB drug regimens, which include new drugs, need to have perceived benefits over existing regimens for them to enter clinical trial. These benefits include a shorter treatment duration (less than 6 months and less than 18–24 months for drug-susceptible and drug-resistant TB, respectively), greater efficacy in terms of cure rates and/or fewer side effects and drug–drug interactions.
When new regimens are found to be safe and tolerable in Phase II trials, lengthy Phase III trials are launched that advance the most promising regimen for confirmatory efficacy and tolerability assessments. These Phase III trials use classical, randomized trial designs that have two or three treatment groups with sample sizes ranging from 300 to 1,000 per group and long-term follow-up of 12–18 months after treatment has been completed89. Taking into account the numerous potential pitfalls in this approach — ranging from unsuspected toxicities when drugs are combined to the challenges of evaluating drugs whose principal contribution to a combination regimen is long-term sterilizing activity (rather than early rapid bactericidal activity), which cannot be reliably measured using EBA or Phase IIb trial designs — the probability of attrition is significant. Even when tolerability and efficacy are proven, classical Phase III studies, conducted in series with large sample sizes and long duration of follow-up, in combination can take as long as 15–20 years to complete before a new drug can reach the market. The development of the current 'short course' TB treatment regimen took decades of rigorous work and numerous clinical trials. The majority of ongoing Phase III trials (Table 2), such as ReMox, Oflotub and Rifaquin, are using a classical serial approach to regimen development.
Shortening duration of TB chemotherapy. Currently, three Phase III non-inferiority trials are evaluating fluoroquinolones to shorten therapy to 4 months. Oflotub (ClinicalTrials.gov identifier: NCT00216385)13,90 compares standard therapy with a regimen in which gatifloxacin is substituted for ethambutol, and gatifloxacin added to isoniazid and rifampicin during the 2-month maintenance phase. Follow-up has been completed and results are awaited. The ReMOX trial (ClinicalTrials.gov identifier: NCT00864383) is blinded and compares standard therapy with two regimens. In one regimen, moxifloxacin is substituted for ethambutol and moxifloxacin is included with isoniazid and rifampicin in the two-month maintenance phase. In the second regimen, moxifloxacin replaces isoniazid throughout the 4-month total treatment duration. Results of the ReMOX trial are expected in early 2014, 7 years after initiation of the trial. The Rifaquin trial (International Standard Randomised Controlled Trial Number: ISRCTN44153044) compares standard therapy with 2 months of moxifloxacin and rifapentine therapy in the maintenance phase. Several trials are now underway (Table 2) to determine the optimal dose of rifamycins to increase activity without a significant increase in toxicity. A recently completed Phase III randomized trial evaluating a shortened 4-month regimen using standard doses of rifampicin in patients with decreased risk for relapse (those with non-cavitary disease at baseline and in whom cultures converted by 8 weeks of therapy) was unable to show equivalence to the standard 6-month regimen, with significantly higher rates of relapse seen in those receiving the shortened regimen12. Going forward, Phase III trials will be needed to determine if high-dose rifamycins can indeed allow reduction of treatment to 4 months or shorter.
Progress in newer treatment regimens for MDR-TB. Recent studies have brought additional treatment options for MDR-TB. An observational “Bangladesh” standardized regimen study38 with a duration of 9–12 months evaluated the efficacy of gatifloxacin, ethambutol, pyrazinamide and clofazimine given throughout the study, supplemented by kanamycin, prothionamide and isoniazid during an intensive phase of 4 months. The study concluded that outcomes were comparable with those observed with the usual 20-month course of MDR-TB treatment and that major adverse drug reactions were infrequent. This regimen achieved <1% failure and ∼90% relapse-free cure and is currently being tested within a clinical trial funded by the United States Agency for International Development that is being conducted by the International Union Against Tuberculosis and Lung Disease in partnership with the Medical Research Council, UK, named the STREAM trial (International Standard Randomised Controlled Trial Number: ISRCTN78372190). STREAM compares a regimen that includes moxifloxacin, ethambutol, pyrazinamide and clofazimine for 40 weeks, supplemented by kanamycin, high-dose isoniazid and prothionamide for the initial 16-week intensive phase against the WHO recommended standard regimen for MDR-TB. All drugs are given daily except for kanamycin, which is given three times a week after 12 weeks.
Improving efficiency of new drug evaluation
Several newer approaches for shortening the time for evaluating new TB drugs through the clinical trial phases of development are currently being pursued. These include the use of 14-day EBA studies to quickly determine bactericidal activity, the use of innovative trial designs that include multi-arm, multi-stage determinations of efficacy of new drug combinations, and the exploration and qualification of new surrogate markers of treatment effect that may improve upon the existing dichotomous microbiologic end points used in trials71,91. Together, these approaches hold promise for shortening the timeframe needed for evaluating regimens and for answering relevant questions about both efficacy and safety and tolerability, without loss in statistical validity or scientific integrity.
New regimens and 14-day EBA studies. With the aim of reducing the length and improving the efficiency of evaluation, as well as reducing costs, clinical trials have been set up that test new combinations in randomized 14-day EBA studies involving patients with drug-susceptible pulmonary TB71,91. These 14-day EBA studies are evaluating two-drug or three-drug combinations that contain pyrazinamide, PA-824 and/or bedaquiline, and/or moxifloxacin and comparing these combinations with the currently used standard four-drug therapy. As judged by two different microbiological end points, the combination of pyrazinamide, PA-824 and moxifloxacin was more effective than standard therapy in reducing the number of culturable M. tuberculosis bacilli in sputum in EBA71. This finding provides encouragement for further testing of new regimens for fully drug-susceptible and MDR-TB.
New designs for Phase II and III trials. Phase II studies that use multi-arm, multi-stage (MAMS) (Fig. 4) and seamless Phase II–III trials may improve efficiency by using treatment selection–adaptive trial design, in which multiple groups evaluating different treatment regimens are each simultaneously compared to a single control group91. MAMS uses planned repeated interim analyses that are pre-specified in the protocol, and poorly performing regimens are halted early and resources then switched to the evaluation of other potentially effective regimens. At each interim analysis, an independent data monitoring committee reviews the data and makes recommendations to the trial steering committee about which groups should continue or should stop. These interim analyses ensure that new patients recruited to the trial are no longer randomized to what is likely to prove to be an ineffective arm. The trial continues until there are sufficient data for the best regimen or regimens to be identified and taken forward to Phase III. A major advantage of this approach regarding regulatory authorities is that new regimens can be added with modifications to the protocol already submitted to the institutional review board approvals, rather than requiring the submission of a brand new protocol each time a modification is made.
This is an example of a five-arm Phase II clinical trial with a three-stage, multi-arm, multistage (MAMS) design91. At the first interim analysis, novel regimen 4 is considered to lack sufficient benefit compared with the control and is not taken forward to stage two. At the second interim analysis, recruitment to novel regimens 1 and 3 is stopped, and only the control regimen and novel regimen 2 continued until the end of the trial. All patients are followed up for time to culture conversion for the same duration (usually 8–10 weeks). This figure is reproduced, with permission, from Ref. 91 © (2012) Oxford University Press.
The AIDS Clinical Trial Group and the TB Trial Consortium, among other networks, are actively investigating the use of MAMS adaptive trial designs for more rapid and efficient testing of new regimens91. Challenges to overcome for MAMS study designs include the need for robust and real-time data monitoring and analysis systems, as well as having an adequate number of comparator arms.
Biomarkers for monitoring TB treatment response, cure and relapse. Whereas bactericidal activity, safety and tolerability of single agents can be assessed with relative simplicity, such determinations for regimens with combinations of drugs are difficult. Preclinical studies provide an indication of improved efficacy and suggest which combination of drugs to pursue further in clinical trials. Promising drug candidates are then tested one at a time in combination with existing standard regimens, resulting in numerous Phase II and Phase III clinical trials, each with large sample sizes and lengthy treatment and follow-up (up to 2.5 years)91.
The current gold-standard Phase II trial end point — sputum culture status at 2 months — is a key driver of the cost and complexity of TB trials today, particularly in evaluating new regimens for drug-susceptible TB. The sputum culture end point has notable drawbacks, which include the following: as a dichotomous signal, it gives limited information on the degree of response; it requires good-quality sputum, which is difficult to obtain at the outset and becomes more challenging later in a trial because cough resolves rapidly on treatment; as a culture-based biomarker it requires high quality, high biosafety level practices; and it has limited utility for monitoring treatment of paucibacillary disease, which is often found in children, extra-pulmonary TB, and in HIV-infected patients with active TB.
Consequently, new accurate and specific biomarkers are being developed to serially follow the progression or resolution of disease and to serve as surrogates of drug efficacy by measuring M. tuberculosis burden throughout treatment and follow-up92. Of these biomarkers being developed, automated liquid media systems that provide time to detection and time to culture conversion, in addition to serial sputum colony counts, are the most advanced in testing for qualification as potential surrogate markers for Phase IIb efficacy studies. The results of ongoing Phase III trials, which use both solid and liquid media, will provide the data needed to determine whether these approaches to interpreting microbiological data can be qualified as a surrogate marker.
In comparison to the progress made in developing new TB drugs over the past 5 years, TB biomarker discovery has been comparatively slow. Indeed, there is an urgent need for TB biomarkers for accurate diagnosis, for evaluating M. tuberculosis load in sputum93, for defining TB disease activity, and for predicting cure, relapse, or further progression92,94,95. Several M. tuberculosis and human biomarkers have been identified recently, and been proposed for use in monitoring treatment effect92,93,94,95,96. However, none of these biomarkers has been qualified or validated as surrogate markers94. The process of qualification and validation will be challenging and slow, partly because of the complex immunological and pathological interactions that occur during infection with M. tuberculosis and the spectrum of clinical manifestations of TB. To date, no biomarker has been identified that is easily detected or in the primary causal pathway to the clinically meaningful end point of interest: relapse after treatment completion94,95,96. New, non-culture based, real-time, quantitative, molecular and non-molecular biomarkers of treatment response are still in the early phases of development92.
Biobanks of biospecimens and comprehensive data obtained from patient cohorts who have had adequate follow-up for treatment failure and relapse will constitute a significant resource for the biomarker discovery field. In this regard, a biobank repository was set up through a partnership among the TB Alliance, the AIDS Clinical Trials Group and the TB Trials Consortium — named the Consortium for TB Biomarkers (CTB2) — and was launched in 2011 with funding from the FDA and the US National Institutes of Health96. This biobank repository will use samples taken from patients enrolled in clinical trials and the data recorded according to the standards set by the Clinical Data Interchange Standards Consortium (see Further information).
Growing networks for drug development and evaluation. A potential obstacle in the development of novel TB treatment regimens is bringing various pharmaceutical companies together so that the individual new TB drugs from each company can be tested in combination. Efforts by the Critical Path Institute (see Further information), an independent, non-profit organization, is creating collaborations among regulatory authorities (scientists from the FDA, the European Medicines Agency and the Japanese Pharmaceutical and Medical Devices Agency) and the pharmaceutical and diagnostics industry to improve testing methods and processes to evaluate the safety and effectiveness of new medical products.
The Critical Path to TB Drug Regimens initiative (see Further information) is a broad collaboration of multiple stakeholders including: pharmaceutical companies; academic institutions; government, regulatory and multilateral agencies; advocates; and non-government organizations. The objective of this large collaborative effort is to accelerate the development of new, safe and effective, shorter TB treatment regimens100.
Conclusions and perspectives
TB is now found in every corner of the globe and is threatening gains made in TB control in Europe97,98. This is despite the introduction of cheap and effective treatment with quadruple drug therapy 40 years ago. There is a great need for shorter, less toxic treatment regimens, new drugs and better and shorter ways of evaluating new TB drugs and drug regimens. The history and evolution of TB drug discovery, development and evaluation has been fascinating. Over the past 10 years a major investment by scientists, funders and the WHO has led to a renaissance of activity into new TB drug development and evaluation. There is an urgent need for increased coordination and enhanced collaboration among drug developers, funding agencies and clinical trial networks. Efforts by the Critical Path to TB Drug Regimens are underway to bring stakeholders together to develop shorter, more effective TB treatment regimens for the therapy of both drug-susceptible and drug-resistant TB, and can be progressed more quickly using newer clinical trial designs guided by more specific biomarkers.
References
Zumla, A., Raviglione, M., Hafner, R. & von Reyn, C. F. Tuberculosis. N. Engl. J. Med. 368, 745–755 (2013). An important update of current concepts on the clinical, epidemiological and management aspects of tuberculosis.
Grange, J. M. in Tuberculosis: A Comprehensive Clinical Reference (eds Schaaf, S. & Zumla, A. I.) 44–59 (Saunders, 2009).
Dye, C., Scheele, S., Dolin, P., Pathania, V. & Raviglione, M. C. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA 282, 677–686 (1999).
Diel, R. et al. Old ideas to innovate TB control: preventive treatment to achieve elimination. Eur. Respir. J. 8 Feb 2013 (10.1183/09031936.00205512).
Raviglione, M. et al. Scaling up interventions to achieve global tuberculosis control: progress and new developments. Lancet 379, 1902–1913 (2012).
World Health Organization. Global Tuberculosis Report 2012 (WHO, 2012).
European Centre for Disease Prevention and Control/WHO Regional Office for Europe. Tuberculosis Surveillance and Monitoring in Europe (European Centre for Disease Prevention and Control, 2012).
Hill, A. N., Becerra, J. & Castro, K. G. Modelling tuberculosis trends in the USA. Epidemiol. Infect. 140, 1862–1872 (2012).
Cohen, J. Infectious disease. Approval of novel TB drug celebrated — with restraint. Science 339, 130 (2013).
World Health Organization. Treatment of Tuberculosis Guidelines 4th edn (WHO, 2010).
Tuberculosis Coalition for Technical Assistance. International Standards for Tuberculosis Care (ISTC) 2nd edn (Tuberculosis Coalition for Technical Assistance, 2009)
Johnson, J. L. et al. Shortening treatment in adults with noncavitary tuberculosis and 2-month culture conversion. Am. J. Respir. Crit. Care Med. 180, 558–563 (2009).
Lienhardt, C. et al. Efficacy and safety of a 4-drug fixed-dose combination regimen compared with separate drugs for treatment of pulmonary tuberculosis: the study C randomized controlled trial. JAMA 305, 1415–1423 (2011).
Dooley, K. E. et al. Old drugs, new purpose: retooling existing drugs for optimized treatment of resistant tuberculosis. Clin. Infect. Dis. 55, 572–581 (2012).
Falzon, D. et al. WHO guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. Eur. Respir. J. 38, 516–528 (2011).
Lawn, S. D. & Zumla, A. Advances in tuberculosis diagnostics: the Xpert MTB/RIF assay and future prospects for a point-of-care test. Lancet Infect. Dis. 13, 349–361 (2013). A critical review of the Xpert MTB/RIF assay and the advantages and limitations of its utility in clinical practice.
Weyer, K. et al. Rapid molecular TB diagnosis: evidence, policy-making and global implementation of Xpert®MTB/RIF. Eur. Respir. J. 22 Nov 2012 (10.1183/09031936.00157212).
Gandhi, N. R. et al. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet 368, 1575–1580 (2006).
Dheda, K. et al. Early treatment outcomes and HIV status of patients with extensively drug-resistant tuberculosis in South Africa: a retrospective cohort study. Lancet 375, 1798–1807 (2010).
Jacobson, K. R., Tierney, D. B., Jeon, C. Y., Mitnick, C. D. & Murray, M. B. Treatment outcomes among patients with extensively drug-resistant tuberculosis: systematic review and meta-analysis. Clin. Infect. Dis. 51, 6–14 (2010).
Migliori, G. B. et al. Drug resistance beyond XDR-TB: results from a large individual patient data meta-analysis. Eur. Respir. J. 11 Oct 2012 (10.1183/09031936.00136312).
Udwadia, Z. F., Amale, R. A., Ajbani, K. K. & Rodrigues, C. Totally drug-resistant tuberculosis in India. Clin. Infect. Dis. 54, 579–581 (2012).
World Health Organization. “Totally Drug-Resistant TB”: a WHO consultation on the diagnostic definition and treatment options. World Health Organization[online], (2012).
Cole, S. T. & Riccardi, G. New tuberculosis drugs on the horizon. Curr. Opin. Microbiol. 14, 570–576 (2011).
Koul, A., Arnoult, E., Lounis, N., Guillemont, J. & Andries, K. The challenge of new drug discovery for tuberculosis. Nature 469, 483–490 (2011).
Global-Alliance for TB Drug Development. Tuberculosis. Scientific blueprint for tuberculosis drug development. Tuberculosis (Edinb.) 81, (Suppl. 1), 1–52 (2001).
Barry, C. E. et al. The spectrum of latent tuberculosis: rethinking the biology and intervention strategies. Nature Rev. Microbiol. 7, 845–855 (2009).
Jindani, A., Doré, C. J. & Mitchison, D. A. Bactericidal and sterilizing activities of antituberculosis drugs during the first 14 days. Am. J. Respir. Crit. Care Med. 167, 1348–1354 (2003).
Donald, P. R. & Diacon, A. H. The early bactericidal activity of anti-tuberculosis drugs: a literature review. Tuberculosis (Edinb.) 88, (Suppl. 1), 75–83 (2008).
Nuermberger, E. L. et al. Moxifloxacin-containing regimen greatly reduces time to culture conversion in murine tuberculosis. Am. J. Respir. Crit. Care Med. 169, 421–426 (2004).
Ma, Z., Lienhardt, C., McIlleron, H., Nunn, A. J. & Wang, X. Global tuberculosis drug development pipeline: the need and the reality. Lancet 375, 2100–2109 (2010).
Rosenthal, I. M. et al. Daily dosing of rifapentine cures tuberculosis in three months or less in the murine model. PLoS Med. 4, e344 (2007).
Sterling, T. R. et al. Three months of rifapentine and isoniazid for latent tuberculosis infection. N. Engl. J. Med. 365, 2155–2166 (2011).
Diacon, A. H. et al. Early bactericidal activity of high-dose rifampin in patients with pulmonary tuberculosis evidenced by positive sputum smears. Antimicrob. Agents Chemother. 51, 2994–2996 (2007).
van Ingen, J. et al. Why do we use 600 mg of rifampicin in tuberculosis treatment? Clin. Infect. Dis. 52, e194–e199 (2011).
Andries, K. et al. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science 307, 223–227 (2005). A landmark paper describing the discovery and development of bedaquiline and the validation of a novel yet ubiquitous new drug target for TB.
Dey, T. et al. Outcomes of clofazimine for the treatment of drug-resistant tuberculosis: a systematic review and meta-analysis. J. Antimicrob. Chemother. 68, 284–293 (2013).
Van Deun, A. et al. Short, highly effective, and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am. J. Respir. Crit. Care Med. 182, 684–692 (2010). An observational “Bangladesh” standardized regimen study, with a duration of 9–12 months, that included gatifloxacin, ethambutol, pyrazinamide and clofazimine throughout, supplemented by kanamycin, prothionamide and isoniazid. During an intensive phase of 4 months this regimen achieved <1% failure and ∼90% relapse-free cure.
Verma, R. K. et al. Inhaled microparticles containing clofazimine are efficacious in treatment of experimental tuberculosis in mice. Antimicrob. Agents Chemother. 57, 1050–1052 (2013).
Zhang, M. et al. Streptomycin-starved Mycobacterium tuberculosis 18b, a drug discovery tool for latent tuberculosis. Antimicrob. Agents Chemother. 56, 5782–5789 (2012).
Ashtekar, D. R. et al. Oxazolidinone, a new class of synthetic antituberculosis agent: in vitro and in vivo activities of DuP-721 against Mycobacterium tuberculosis. Diagn. Microbiol. Infect. Dis. 14, 465–471 (1991).
Fortun, J. et al. Linezolid for the treatment of multidrug-resistant tuberculosis. J. Antimicrob. Chemother. 56, 180–185 (2005).
Lee, M. et al. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N. Engl. J. Med. 367, 1508–1518 (2012). A demonstration that linezolid, a drug with poor EBA, can improve the prognosis of patients with XDR-TB, thus providing hope that next-generation oxazolidinones may be even better.
Sotgiu, G. et al. Efficacy, safety and tolerability of linezolid containing regimens in treating MDR-TB and XDR-TB: systematic review and meta-analysis. Eur. Respir. J. 40, 1430–1442 (2012).
Wallis, R. S. et al. Biomarker-assisted dose selection for safety and efficacy in early development of PNU-100480 for tuberculosis. Antimicrob. Agents Chemother. 55, 567–574 (2010).
Wallis, R. S. et al. Pharmacokinetics and whole-blood bactericidal activity against Mycobacterium tuberculosis of single doses of PNU-100480 in healthy volunteers. J. Infect. Dis. 202, 745–751 (2010).
Wallis, R. S. et al. Rapid evaluation in whole blood culture of regimens for XDR-TB containing PNU-100480 (sutezolid), TMC207, PA-824, SQ109, and pyrazinamide. PLoS ONE 7, e30479 (2012).
Reele, S. et al. A 14-day multiple ascending dose study: AZD5847 is well tolerated at predicted exposure for treatment of tuberculosis (TB) (Abstract A1-1735). 51st Annual Interscience Conference on Antimicrobial Agents and Chemotherapy [online], (2011).
Hugonnet, J. E. et al. Meropenem-clavulanate is effective against extensively drug-resistant Mycobacterium tuberculosis. Science 323, 1215–1218 (2009).
Kumar, P. et al. Meropenem inhibits D,D-carboxypeptidase activity in Mycobacterium tuberculosis. Mol. Microbiol. 86, 367–381 (2012).
Dauby, N., Muylle, I., Mouchet, F., Sergysels, R. & Payen, M. C. Meropenem/clavulanate and linezolid treatment for extensively drug-resistant tuberculosis. Pediatr. Infect. Dis. J. 30, 812–813 (2011).
De Lorenzo, S. et al. Efficacy and safety of meropenem/clavunate added to linezolid containing regimens in the treatment of M/XDR-TB. Eur. Respir. J. 20 Sept 2012 (10.1183/09031936.00124312).
Koul, A. et al. Diarylquinolines target subunit c of mycobacterial ATP synthase. Nature Chem. Biol. 3, 323–324 (2007).
Haagsma, A. C. et al. Selectivity of TMC207 towards mycobacterial ATP synthase compared with that towards the eukaryotic homologue. Antimicrob. Agents Chemother. 53, 1290–1292 (2009).
Huitric, E. et al. Rates and mechanisms of resistance development in Mycobacterium tuberculosis to a novel diarylquinoline ATP synthase inhibitor. Antimicrob. Agents Chemother. 54, 1022–1028 (2009).
Biukovic, G. et al. Variations of subunit ε of the Mycobacterium tuberculosis F1F0 ATP synthase and a novel model for mechanism of action of the TB drug TMC207. Antimicrob. Agents Chemother. 57, 168–176 (2013).
Koul, A. et al. Diarylquinolines are bactericidal for dormant mycobacteria as a result of disturbed ATP homeostasis. J. Biol. Chem. 283, 25273–25280 (2008).
Rao, S. P., Alonso, S., Rand, L., Dick, T. & Pethe, K. The protonmotive force is required for maintaining ATP homeostasis and viability of hypoxic, nonreplicating Mycobacterium tuberculosis. Proc. Natl Acad. Sci. USA 105, 11945–11950 (2008).
Diacon, A. H. et al. The diarylquinoline TMC207 for multidrug-resistant tuberculosis. N. Engl. J. Med. 360, 2397–2405 (2009). An important publication documenting the considerable impact of bedaquiline on the prognosis of patients with MDR-TB and the value of testing new drugs in MDR cohorts.
Veziris, N. et al. A once-weekly R207910-containing regimen exceeds activity of the standard daily regimen in murine tuberculosis. Am. J. Respir. Crit. Care Med. 179, 75–79 (2009).
Lounis, N. et al. Prevention of drug carryover effects in studies assessing antimycobacterial efficacy of TMC207. J. Clin. Microbiol. 46, 2212–2215 (2008).
Lin, P. L. et al. Metronidazole prevents reactivation of latent Mycobacterium tuberculosis infection in macaques. Proc. Natl Acad. Sci. USA 109, 14188–14193 (2012).
Stover, C. K. et al. A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis. Nature 405, 962–966 (2000).
Matsumoto, M. et al. OPC-67683, a nitro-dihydro-imidazooxazole derivative with promising action against tuberculosis in vitro and in mice. PLoS Med. 3, e466 (2006).
Manjunatha, U. H. et al. Identification of a nitroimidazo-oxazine-specific protein involved in PA-824 resistance in Mycobacterium tuberculosis. Proc. Natl Acad. Sci. USA 103, 431–436 (2006).
Singh, R. et al. PA-824 kills nonreplicating Mycobacterium tuberculosis by intracellular NO release. Science 322, 1392–1395 (2008). An important publication documenting a novel M. tuberculosis killing mechanism mediated by PA-824 (and later by delaminid) that provides proof of concept for developing novel NO donor drugs for treating TB.
Manjunatha, U. H. et al. Mycobacterium leprae is naturally resistant to PA-824. Antimicrob. Agents Chemother. 50, 3350–3354 (2006).
Hurdle, J. G. et al. A microbiological assessment of novel nitrofuranylamides as anti-tuberculosis agents. J. Antimicrob. Chemother. 62, 1037–1045 (2008).
Manjunatha, U., Boshoff, H. I. & Barry, C. E. The mechanism of action of PA-824: Novel insights from transcriptional profiling. Commun. Integr. Biol. 2, 215–218 (2009).
Diacon, A. et al. Phase II dose-ranging trial of the early bactericidal activity of PA-824; Antimicrob. Agents Chemother. 56, 3027–3031 (2012).
Diacon, A. H. et al. 14-day bactericidal activity of PA-824, bedaquiline, pyrazinamide, and moxifloxacin combinations: a randomised trial. Lancet 380, 986–993 (2012). A seminal study describing how the use of EBA with combination therapies has the potential to reduce the time needed for developing new multidrug regimens.
Diacon, A. H. et al. Early bactericidal activity of delamanid (OPC-67683) in smear-positive pulmonary tuberculosis patients. Int. J. Tuberc. Lung Dis. 15, 949–954 (2011).
Gler, M. T. et al. Delamanid for multidrug-resistant pulmonary tuberculosis. N. Engl. J. Med. 366, 2151–2160 (2012). An encouraging publication demonstrating that delamanid could enhance treatment options for patients with MDR-TB.
Skripconoka, V. et al. Delamanid improves outcomes and reduces mortality for multidrug-resistant tuberculosis. Eur. Respir. J. 27 Sept 2012 (10.1183/09031936.00125812).
Lee, R. E. et al. Combinatorial lead optimization of [1,2]-diamines based on ethambutol as potential antituberculosis preclinical candidates. J. Comb. Chem. 5, 172–187 (2003).
Tahlan, K. et al. SQ109 targets MmpL3, a membrane transporter of trehalose monomycolate involved in mycolic acid donation to the cell wall core of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 56, 1797–1809 (2012).
Reddy, V. M., Einck, L., Andries, K. & Nacy, C. A. In vitro interactions between new antitubercular drug candidates SQ109 and TMC207. Antimicrob. Agents Chemother. 54, 2840–2846 (2010).
Grzegorzewicz, A. E. et al. Inhibition of mycolic acid transport across the Mycobacterium tuberculosis plasma membrane. Nature Chem. Biol. 8, 334–341 (2012).
La Rosa, V. et al. MmpL3 is the cellular target of the antitubercular pyrrole derivative BM212. Antimicrob. Agents Chemother. 56, 324–331 (2012).
Stanley, S. A. et al. Identification of novel inhibitors of M. tuberculosis growth using whole cell based high-throughput screening. ACS Chem. Biol. 7, 1377–1384 (2012).
Makarov, V. et al. Benzothiazinones kill Mycobacterium tuberculosis by blocking arabinan synthesis. Science 324, 801–804 (2009). A landmark paper presenting both a new chemical entity and a novel drug target for TB therapy.
Pasca, M. R. et al. Clinical isolates of Mycobacterium tuberculosis in four European hospitals are uniformly susceptible to benzothiazinones. Antimicrob. Agents Chemother. 54, 1616–1618 (2010).
Lechartier, B., Hartkoorn, R. C. & Cole, S. T. In vitro combination studies of benzothiazinone lead compound BTZ043 against Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 56, 5790–5793 (2012).
Neres, J. et al. Structural basis for benzothiazinone-mediated killing of Mycobacterium tuberculosis. Sci. Transl. Med. 4, 150ra121 (2012).
Trefzer, C. et al. Benzothiazinones: prodrugs that covalently modify the decaprenylphosphoryl-β-d-ribose 2′-epimerase DprE1 of Mycobacterium tuberculosis. J. Am. Chem. Soc. 132, 13663–13665 (2010).
Trefzer, C. et al. Benzothiazinones are suicide inhibitors of mycobacterial decaprenylphosphoryl-β-d-ribofuranose 2′-oxidase DprE1. J. Am. Chem. Soc. 134, 912–915 (2012).
Christophe, T. et al. High content screening identifies decaprenyl-phosphoribose 2′ epimerase as a target for intracellular antimycobacterial inhibitors. PLoS Pathog. 5, e1000645 (2009).
Magnet, S. et al. Leads for antitubercular compounds from kinase inhibitor library screens. Tuberculosis (Edinb.) 90, 354–360 (2010).
Nunn, A. J., Phillips, P. P. & Mitchison, D. A. Timing of relapse in short-course chemotherapy trials for tuberculosis. Int. J. Tuberc. Lung Dis. 14, 241–242 (2010).
Merle, C. S. et al. A pivotal registration phase III, multicenter, randomized tuberculosis controlled trial: design issues and lessons learnt from the gatifloxacin for TB (OFLOTUB) project. Trials 13, 61 (2012).
Phillips, P. P. et al. Innovative trial designs are practical solutions for improving the treatment of tuberculosis. J. Infect. Dis. 205, (Suppl. 2), 250–257 (2012).
Wallis, R. et al. Tuberculosis biomarkers discovery: developments, needs and challenges. Lancet Infect. Dis. 13, 362–372 (2013). An important review of the latest information on progress on TB biomarkers development.
Horne, D. J. et al. Sputum monitoring during tuberculosis treatment for predicting outcome: systematic review and meta-analysis. Lancet Infect. Dis. 10, 387–394 (2010).
Walzl, G., Ronacher, K., Hanekom, W., Scriba, T. J. & Zumla, A. Immunological biomarkers of tuberculosis. Nature Rev. Immunol. 11, 343–354 (2011).
McNerney, R. et al. Tuberculosis diagnostics and biomarkers: needs, challenges, recent advances, and opportunities. J. Infect. Dis. 205 (Suppl. 2), 147–158 (2012).
Nahid, P. et al. CDC/NIH Workshop. Tuberculosis biomarker and surrogate endpoint research roadmap. Am. J. Respir. Crit. Care Med. 184, 972–979 (2011).
Skrahina, A. et al. Alarming levels of drug-resistant tuberculosis in Belarus: results of a survey in Minsk. Eur. Respir. J. 39, 1425–1431 (2012).
Abubakar, I. et al. Drug resistant tuberculosis: time for visionary political leadership. Lancet Infect. Dis. 24 Mar 2013 (10.1016/S1473-3099(13)70030-6).
Schatz, A., Bugie, E. & Waksman, S. A. Streptomycin, a substance exhibiting antibiotic activity against Gram-positive and Gram-negative bacteria. Proc. Soc. Exp. Biol. Med. 55, 66–69 (1944).
Wassersug, J. D. Pulmonary tuberculosis. N. Engl. J. Med. 235, 220–229 (1946).
Marshall, G. Streptomycin in the treatment of pulmonary tuberculosis. A Medical Research Council investigation. BMJ 1, 382–386 (1949).
American Thoracic Society. Treatment of tuberculosis. Am. J. Respir. Crit. Care Med. 167, 603–662 (2003).
Gengiah, T. N., Gray, A. L., Naidoo, K. & Karim, Q. A. Initiating antiretrovirals during tuberculosis treatment: a drug safety review. Expert Opin. Drug Saf. 10, 559–574 (2011).
Havlir, D. V. et al. Timing of antiretroviral therapy for HIV-1 infection and tuberculosis. N. Engl. J. Med. 365, 1482–1491 (2011).
Blanc, F. X. et al. Earlier versus later start of antiretroviral therapy in HIV-infected adults with tuberculosis. N. Engl. J. Med. 365, 1471–1481 (2011).
De Cock, K. M. & El-Sadr, W. M. When to start ART in Africa — an urgent research priority. N. Engl. J. Med. 368, 886–889 (2013).
Subbian, S. et al. Phosphodiesterase-4 inhibition alters gene expression and improves isoniazid-mediated clearance of Mycobacterium tuberculosis in rabbit lungs. PLoS Pathog. 7, e1002262 (2011).
Tobin, D. M. et al. Host genotype-specific therapies can optimize the inflammatory response to mycobacterial infections. Cell 148, 434–446 (2012).
Skerry, C., Harper, J., Klunk, M., Bishai, W. R. & Jain, S. K. Adjunctive TNF inhibition with standard treatment enhances bacterial clearance in a murine model of necrotic TB granulomas. PLoS ONE 7, e39680 (2012).
Napier, R. J. et al. Imatinib-sensitive tyrosine kinases regulate mycobacterial pathogenesis and represent therapeutic targets against tuberculosis. Cell Host Microbe 10, 475–485 (2012).
Ivanyi, I. & Zumla, A. Non-steroidal anti-inflammatory drugs for adjunctive tuberculosis treatment. J. Infect. Dis. 5 Apr 2013 (10.1093/infdis/jit153).
Amaral, L., Martins, M. & Viveiros, M. Enhanced killing of intracellular multidrug-resistant Mycobacterium tuberculosis by compounds that affect the activity of efflux pumps. J. Antimicrob. Chemother. 59, 1237–1246 (2007).
Adams, K. N. et al. Drug tolerance in replicating mycobacteria mediate macrophage-induced efflux mechanism. Cell 145, 39–53 (2011).
Lim, L. E. et al. Anthelmintic avermectins kill M. tuberculosis, including multidrug-resistant clinical strains. Antimicrob. Agents Chemother. 57, 1040–1046 (2013).
Maiga, M. et al. Successful shortening of tuberculosis treatment using adjuvant host-directed therapy with FDA-approved phosphodiesterase inhibitors in the mouse model. PLoS ONE 7, e30749 (2012).
Uhlin, M., Andersson, J., Zumla, A. & Maeurer, M. Adjunct immunotherapies for tuberculosis. J. Infect. Dis. 205 (Suppl. 2), 325–334 (2012).
Bruns, H. et al. Abelson tyrosine kinase controls phagosomal acidification required for killing of Mycobacterium tuberculosis in human macrophages. J. Immunol. 189, 4069–4078 (2012).
Kuijl, C. et al. Intracellular bacterial growth is controlled by a kinase network around PKB/AKT1. Nature. 450, 725–730 (2007).
Boshoff, H. I. & Barry, C. E. 3rd. Tuberculosis — metabolism and respiration in the absence of growth. Nature Rev. Microbiol. 3, 70–80 (2005).
Pym, A. S. & Cole, S. T. in Bacterial Resistance to Antimicrobials 2nd Edn (eds Wax, R. G., Lewis, K., Salyers, A. A. & Taber, H.) 313–342 (CRC, 2008).
Shi, W. et al. Pyrazinamide inhibits trans-translation in Mycobacterium tuberculosis. Science 333, 1630–1632 (2011).
Chakraborty, S., Gruber, T., Barry, C. E. 3rd, Boshoff, H. I. & Rhee, K. Y. Para-aminosalicylic acid acts as an alternative substrate of folate metabolism in Mycobacterium tuberculosis. Science 339, 88–91 (2013).
Sirgel, F. A. et al. gyrA mutations and phenotypic susceptibility levels to ofloxacin and moxifloxacin in clinical isolates of Mycobacterium tuberculosis. J. Antimicrob. Chemother. 67, 1088–1093 (2012).
Sirgel, F. A. et al. Mutations in the rrs A1401G gene and phenotypic resistance to amikacin and capreomycin in Mycobacterium tuberculosis. Microb. Drug Resist. 18, 193–197 (2012).
Salian, S. et al. Structure–activity relationships among the kanamycin aminoglycosides: role of ring I hydroxyl and amino groups. Antimicrob. Agents Chemother. 56, 6104–6108 (2012).
Global Alliance for TB Drug Development. Cycloserine. Tuberculosis (Edinb.) 88, 100–101 (2008).
Bruning, J. B., Murillo, A. C., Chacon, O., Barletta, R. G. & Sacchettini, J. C. Structure of the Mycobacterium tuberculosis d-alanine:d-alanine ligase, a target of the antituberculosis drug d-cycloserine. Antimicrob. Agents Chemother. 55, 291–301 (2010).
Benator, D. et al. Rifapentine and isoniazid once a week versus rifampicin and isoniazid twice a week for treatment of drug-susceptible pulmonary tuberculosis in HIV-negative patients: a randomised clinical trial. Lancet 360, 528–534 (2002).
Steingart, K. R., et al. Higher-dose rifampin for the treatment of pulmonary tuberculosis: a systematic review. Int. J. Tuber. Lung Dis. 15, 305–316 (2011).
Batt, S. M., et al. Structural basis of inhibition of Mycobacterium tuberculosis DprE1 by benzothiazinone inhibitors. Proc. Natl Acad. Sci. USA 109, 11354–11359 (2012).
Acknowledgements
The work of S.T.C. is supported by the European Community's Seventh Framework Programme (FP7/2007–2013) under the grant agreement number 260872. The work of A.Z. is supported by the Medical Research Council, UK, the European Union FP7, the European Developing Countries Clinical Trials Partnership, the National Institutes for Health Research (NIHR) University College London (UCL) Hospitals NHS Trust Biomedical Research Centre and the UBS Optimus Foundation, Switzerland. The work of P.N. is supported by the National Institutes of Health through National Institute of Allergy and Infectious Diseases funding (1R01AI104589), the Centers for Disease Control and Prevention TB Trials Consortium, and the Bill and Melinda Gates Foundation. Adam Zumla, UCL School of Pharmacy, UK, provided technical and administrative assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Stewart T. Cole is named as the inventor on patents or patent applications related to the work in this article.
Related links
DATABASES
FURTHER INFORMATION
Glossary
- Multidrug-resistant TB
-
(MDR-TB). Tuberculosis (TB) caused by Mycobacterium tuberculosis bacilli that are resistant to at least isoniazid and rifampicin.
- Extensively drug-resistant TB
-
(XDR-TB). Tuberculosis (TB) caused by Mycobacterium tuberculosis bacilli that are resistant to rifampicin, isoniazid, plus any fluoroquinolone and at least one of the three injectable second-line drugs: amikacin, kanamycin and capreomycin.
- Directly observed therapy
-
(DOT). An approach to patient management that involves carers directly observing patients taking their tuberculosis drugs.
- Drug-susceptible TB
-
Tuberculosis (TB) caused by Mycobacterium tuberculosis bacilli that is susceptible to first-line TB drugs.
- Early bactericidal activity
-
(EBA). A commonly used assay in which the Mycobacterium tuberculosis bacilli load in sputum from the lungs of infected patients is periodically monitored for loss of viability, or culture conversion, using microbiological techniques. The duration of the assay has been extended from 7 days to 14 days since its conception.
- Antiretroviral therapy
-
(ART). A combination of antiviral drugs used for treatment of diseases due to HIV.
- Randomized, controlled clinical trial
-
The random allocation of patients to therapeutic regimens after enrolment. Assurances on strict adherence to interventions and minimizing losses from the trial population throughout treatment and follow-up are also key elements of randomized clinical trials.
- Repurposed drugs
-
In this article, these are drugs that were developed to treat other diseases and have since been repurposed for treating tuberculosis.
- Immune reconstitution inflammatory syndrome
-
Describes a collection of inflammatory disorders that are associated with the paradoxical worsening of pre-existing infectious conditions following the initiation of antiretroviral therapy in HIV-infected individuals.
- Biomarker
-
A host or pathogen (for example, Mycobacterium tuberculosis) characteristic that is objectively measured and evaluated as an indicator of normal biological processes or pathogenic processes, or as an indicator of pharmacological responses to a therapeutic intervention.
- Paucibacillary disease
-
Pulmonary tuberculosis with low Mycobacterium tuberculosis load in sputum.
- Biobanks
-
Repositories that store biospecimens and data obtained from well-characterized patient cohorts who have had adequate follow-up for therapeutic failure and relapse. Biobanks will constitute a significant resource for the biomarker discovery field.
Rights and permissions
About this article
Cite this article
Zumla, A., Nahid, P. & Cole, S. Advances in the development of new tuberculosis drugs and treatment regimens. Nat Rev Drug Discov 12, 388–404 (2013). https://doi.org/10.1038/nrd4001
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrd4001
This article is cited by
-
Assessment of interleukin 6 (IL-6) as a marker of inflammation among adult patients with pulmonary tuberculosis in Zaria, Nigeria
The Egyptian Journal of Bronchology (2024)
-
Whole genome sequencing reveals candidate genes involving in PAS resistance in M. Tuberculosis isolated from patients in Thailand
World Journal of Microbiology and Biotechnology (2024)
-
Antitubercular drugs: possible role of natural products acting as antituberculosis medication in overcoming drug resistance and drug-induced hepatotoxicity
Naunyn-Schmiedeberg's Archives of Pharmacology (2024)
-
Structure-based drug design and characterization of novel pyrazine hydrazinylidene derivatives with a benzenesulfonate scaffold as noncovalent inhibitors of DprE1 tor tuberculosis treatment
Molecular Diversity (2024)
-
A first-in-class leucyl-tRNA synthetase inhibitor, ganfeborole, for rifampicin-susceptible tuberculosis: a phase 2a open-label, randomized trial
Nature Medicine (2024)