Abstract
Portal hypertension is a severe, almost unavoidable complication of chronic liver diseases and is responsible for the main clinical consequences of cirrhosis. Measurement of the hepatic venous pressure gradient (HVPG) is currently the best available method to evaluate the presence and severity of portal hypertension. Clinically significant portal hypertension is defined as an increase in HVPG to ≥10 mmHg; above this threshold, the complications of portal hypertension might begin to appear. Measurement of HVPG is increasingly used in clinical hepatology, and numerous studies have demonstrated that the parameter is a robust surrogate marker for hard clinical end points. The main clinical applications for HVPG include diagnosis, risk stratification, identification of patients with hepatocellular carcinoma who are candidates for liver resection, monitoring of the efficacy of medical treatment, and assessment of progression of portal hypertension. Patients who experience a reduction in HVPG of ≥20% or to <12 mmHg in response to drug therapy are defined as 'responders'. Responders have a markedly decreased risk of bleeding (or rebleeding), ascites, and spontaneous bacterial peritonitis, which results in improved survival.
Key Points
-
Measurement of the hepatic venous pressure gradient (HVPG) is the gold standard technique for evaluation of portal hypertension in liver disease
-
In patients with cirrhosis, HVPG measurement provides independent prognostic information on survival and the risk of decompensation
-
The HVPG response to pharmacological therapy enables the identification of patients with portal hypertension who are most likely to benefit from treatment
-
Measurement of HVPG helps to assess the risk of liver failure and death after liver resection in patients with compensated chronic liver disease or hepatocarcinoma
-
No noninvasive alternatives to HVPG measurement are currently available
Similar content being viewed by others
Introduction
Portal hypertension, a frequently presenting clinical syndrome, is defined as a pathological increase in portal venous pressure. This increase in pressure causes the pressure gradient between the portal vein and the inferior vena cava (the so-called portal perfusion pressure of the liver or portal pressure gradient) to increase above the normal range (1–5 mmHg). When the portal pressure gradient increases to ≥10 mmHg, complications of portal hypertension can arise; these complications include formation of portosystemic collaterals and varices, upper gastrointestinal bleeding resulting from ruptured gastroesophageal varices and portal hypertensive gastropathy, ascites, renal dysfunction, hepatic encephalopathy, arterial hypoxemia, disorders in the metabolism of drugs or endogenous substances that are normally eliminated by the liver, bacteremia, and hypersplenism.1,2
The importance of portal hypertension is underscored by the relatively high incidence and severity of these complications. The main cause of this syndrome in Western countries is cirrhosis of the liver, a disease that affects mainly adults and represents the third to fifth leading cause of death in men over the age of 50 years in Europe and the US. The currently favored method for determining portal venous pressure involves catheterization of the hepatic vein and measurement of the hepatic venous pressure gradient (HVPG). This Review focuses on the measurement of HVPG and its clinical use in patients with chronic liver diseases.
Measurement of HVPG
Hepatic vein catheterization with measurement of HVPG is the current preferred technique for determining portal pressure; this method has almost totally replaced direct measurement of portal pressure by more invasive techniques, such as splenic pulp puncture and percutaneous transhepatic or transvenous catheterization of the portal vein. Direct techniques for determining the portal pressure gradient, such as the aforementioned ones (with the exception of the transjugular approach), require the simultaneous puncture of a hepatic vein and are currently used only in specific cases, mostly to assess presinusoidal portal hypertension or in cholestatic disorders.
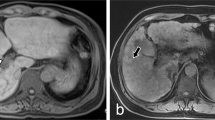
The portal pressure gradient (measured as HVPG) is the difference between the wedged hepatic venous pressure (WHVP) and the free hepatic venous pressure (FHVP). The WHVP is measured by occluding the hepatic vein; stopping the blood flow causes the static column of blood so formed to equalize in pressure with the preceding vascular territory—in this case, the hepatic sinusoids (Figure 1). Thus, WHVP is a measure of hepatic sinusoidal pressure, not of portal pressure. In the normal liver, WHVP is slightly lower (by ∼1 mmHg) than portal pressure, owing to pressure equilibration through the interconnected sinusoids.3 In liver cirrhosis, however, the static column of blood created by occluding the hepatic vein cannot be decompressed at the sinusoidal level because the connections between sinusoids are disrupted as a result of the presence of fibrous septa and nodule formation.4 In cirrhosis, therefore, WHVP gives an accurate estimate of portal pressure, as has been demonstrated both for alcoholic and viral cirrhosis.5 FHVP, as its name suggests, is a measure of the pressure of the unoccluded hepatic vein.
In the normal liver, after occlusion of blood flow in a hepatic vein with a balloon catheter, the pressure of the static column of blood (i.e. the wedged hepatic venous pressure [WHVP]) equilibrates through the interconnected sinusoids. WHVP, therefore, is a measurement of the hepatic sinusoidal pressure, which is slightly lower than the portal pressure (by ∼1 mmHg). In the cirrhotic liver, the pressure of the static column of blood created by balloon inflation cannot be decompressed at the sinusoidal level owing to sinusoidal narrowing and disruption of the normal intersinusoidal architecture by fibrosis and nodule formation. Consequently, WHVP equilibrates with and is equivalent to portal pressure in the cirrhotic liver.
HVPG reflects portal pressure, so the value changes when the factors that determine portal pressure (resistance and blood flow) are modified.6 Changes in hepatic resistance might be caused by mechanical (fibrosis, regenerative nodules, or thrombosis; Figure 1) or functional abnormalities (increased hepatic vascular tone), or by changes in the portal or collateral blood flow.
The procedure
Catheterization of the hepatic vein is carried out under sedation in conjunction with noninvasive vital sign monitoring (by electrocardiography, arterial blood pressure, and pulse oximetry). Under local anesthesia, the right jugular vein (or the femoral or antecubital vein) is catheterized, a venous introducer is placed, and a balloon-tipped catheter is advanced under fluoroscopic control into the inferior vena cava and a hepatic vein to measure WHVP, FHVP and pressure in the inferior vena cava, (Figure 2). This is a moderately invasive technique, but no more so than other routine procedures that are carried out in patients with chronic liver injury.
a | The antecubital vein, b | the jugular vein, or c | the femoral vein can be used for hepatic vein catheterization. As shown, the degree of invasiveness depends on the elected access site. Access via the antecubital vein is the least invasive approach and can be carried out on an outpatient basis. Access via the jugular or femoral veins is moderately invasive and requires admission for ∼1 day. The transjugular approach is the one most frequently used, as it enables a transvenous liver biopsy to be obtained as part of the procedure.
FHVP is measured by maintaining the tip of the catheter 'free' in the hepatic vein, at 2–4 cm from its opening into the inferior vena cava. The FHVP should be similar in value to the inferior vena cava pressure; a difference of >2 mmHg signifies that the catheter is probably inadequately placed or that a hepatic vein obstruction exists.
WHVP is measured by occluding the hepatic vein, either by 'wedging' the catheter into a small branch of a hepatic vein (Figure 3a) or by inflating a balloon at the tip of the catheter (Figure 3b). Adequate occlusion of the hepatic vein is confirmed by slowly injecting 5 ml of contrast dye into the vein (a procedure that should reveal a typical 'wedged' pattern) without observing reflux of the dye or its washout through communications with other hepatic veins. Occlusion of the hepatic vein by balloon inflation is the preferred technique, as the volume of liver circulation that is 'sensed' by this method is much larger than that attained by wedging the catheter (Figure 3a,b), which reduces measurement variability. Indeed, a high variability of HVPG values between different hepatic veins has been reported with end-hole, non-balloon catheters.7 WHVP should be measured until the value remains stable (usually >40 s). All measurements should be taken at least in duplicate, and permanent tracings should be obtained with a multichannel recorder and adequately calibrated transducers (Figure 3c, Box 1).
WHVP can be measured by a | a 'wedging' catheter or b | balloon occlusion. The balloon occlusion technique is preferred, as the volume of the liver circulation sensed by this technique is much larger than that assessed in the wedging catheter method, which increases the accuracy and stability of the results. c | A typical HVPG tracing. Please note the slow speed of the recorder (1 mm/s), the range of pressures, and that equilibration of WHVP requires over 25 s. HVPG is calculated as the difference between WHVP and FHVP. A valid measurement requires two consecutive determinations that differ by less than 1 mmHg, as illustrated. Abbreviations: HVPG, hepatic venous pressure gradient; FHVP, free hepatic venous pressure; WHVP, wedged hepatic venous pressure. Permission obtained from Georg Thieme Verlag © Bosch, J. et al. Measurement of portal pressure and its role in the management of chronic liver disease. Semin. Liver Dis. 26, 348–362 (2006).
The technique to obtain HVPG values is relatively straightforward; however, achieving accurate measurements requires specialist training, as the procedure differs from those used in heart catheterization laboratories, interventional radiology rooms, and intensive care units. A series of practical tips to ensure adequate measurements is outlined in Box 1.
Complications, contraindications, and tolerance
Measurement of HVPG is a safe procedure. No fatalities have occurred among over 12,000 studies performed in our laboratory. Major complications have been limited to local injury at the puncture site (femoral, jugular, or antecubital veins) and include leakage, hematoma and—rarely—arteriovenous fistulae or Horner syndrome (in the case of jugular puncture). Ultrasonographic guidance should always be used when available, as this tool considerably reduces the risk of procedural complications. Passage of the catheter through the right atrium might cause supraventricular arrhythmias (most commonly ectopic beats), but these are self-limited in over 90% of cases.
A history of allergic reaction to iodinated radiological contrast medium is not a contraindication to hepatic vein catheterization because CO2 can be used as a contrast agent. Although coagulation disorders are common in patients with cirrhosis, only cases of severe thrombocytopenia (platelet levels <20 × 109/l) or a low prothrombin ratio (below 30%) call for the replacement of platelets or transfusion of fresh frozen plasma.
The procedure entails very little discomfort. Carried out under moderate conscious sedation (0.2 mg/kg intravenous midazolam, which does not influence HVPG measurement),8 the procedure's acceptability is comparable to that of upper gastrointestinal tract endoscopy.
Associated procedures
In addition to pressure measurements, other procedures can be carried out during hepatic vein catheterization. Hepatic blood flow can be measured (by use of indicator dilution techniques), a transjugular liver biopsy can be obtained (which, in our laboratory, is carried out in ∼40% of cases), and retrograde CO2 portography can be performed. Furthermore, right heart catheterization with measurements of right atrial pressure can be carried out and pulmonary artery pressure, pulmonary wedged pressure and cardiac output can be measured. All these parameters can be very useful in the investigation of cardiopulmonary complications of cirrhosis.
Alternative procedures
Although the HVPG measurement procedure is very well tolerated, the fact that it is invasive and not available at every hospital has prompted attempts to look for noninvasive alternatives, such as physical examination, laboratory tests, imaging techniques, and transient elastography (which measures liver stiffness).9,10 Transient elastography values correlate closely with HVPG values, but only up to 10 mmHg. Moreover, the patient's sex, hepatic inflammation, cholestasis, hepatocellular carcinoma (HCC), liver congestion, and the etiology of their liver disease all influence transient elastography values; this parameter cannot, therefore, substitute for HVPG measurements. Whether transient elastography can be used to identify patients with compensated cirrhosis who are at risk of developing clinically significant portal hypertension requires studies larger than those currently available, as well as trials that specifically focus on this subpopulation of patients.
Imaging techniques are very useful for identifying some of the causes of portal hypertension, such as portal vein or hepatic vein thrombosis. However, no imaging technique has proved sufficiently accurate to replace HVPG measurement, which remains the gold standard for identifying and grading sinusoidal portal hypertension.4
Applications of HVPG measurement
Diagnosis of portal hypertension
Portal hypertension is usually determined by means of the HVPG, the value of which closely correlates with that of the portacaval pressure gradient.5 In healthy adults, HVPG values are normally within the range 1–5 mmHg. An HVPG value of 6–9 mmHg corresponds to preclinical sinusoidal portal hypertension,2,11,12 whereas clinically significant portal hypertension is diagnosed when HVPG is ≥10 mmHg, at which point clinical manifestations of portal hypertensive syndrome, such as varices, bleeding, gastropathy, and ascites, might appear.1,11,13
Classification of portal hypertension
Any condition that interferes with blood flow within the portal system can cause portal hypertension, so this condition is classified according to the site of obstruction as prehepatic (involving the splenic, mesenteric, or portal veins), intrahepatic (parenchymal liver diseases) and posthepatic (diseases involving the hepatic venous outflow; Box 2).
Prehepatic hypertension
Prehepatic portal hypertension is most frequently caused by portal vein thrombosis. In children, such thromboses are often the result of omphalitis. In adults, however, thrombophilic syndromes, either congenital (such as a protein C or S deficiency) or acquired (such as latent myeloproliferative disease), both of which frequently occur in addition to local factors (such as sepsis, abdominal trauma, or surgery), can explain about 70% of cases.14 The remaining 30% of cases of adult portal vein thrombosis are idiopathic.14
Intrahepatic hypertension
The most common causes of portal hypertension are intrahepatic in nature. In Western countries, liver cirrhosis is responsible for about 90% of cases of portal hypertension, whereas schistosomiasis is the leading cause in certain other areas of the world. Intrahepatic portal hypertension can be further subclassified according to the results of hepatic vein catheterization.
Presinusoidal portal hypertension shows normal WHVP and FHVP values, as is the case for noncirrhotic portal hypertension and hepatic granulomatosis (which occurs during schistosomiasis, sarcoidosis, tuberculosis, and early stages of primary biliary cirrhosis). Sinusoidal portal hypertension gives rise to increased WHVP and normal FHVP and is found in most chronic liver diseases, except for primary biliary cirrhosis. In postsinusoidal portal hypertension, both WHVP and FHVP are increased, as is found in Budd–Chiari syndrome (hepatic vein thrombosis).
Subclassification according to hepatic vein catheterization, however, is not always straightforward. For example, in schistosomiasis, parasite eggs are initially deposited in portal venules, where they induce the formation of granulomas and fibrosis that obliterate the portal venules (presinusoidal portal hypertension). Fibrosis subsequently extends to the sinusoids (sinusoidal portal hypertension), with a hemodynamic and clinical pattern that resembles liver cirrhosis.
Posthepatic hypertension
Posthepatic portal hypertension occurs mainly as a result of Budd–Chiari syndrome. Obstruction, which can be observed in the hepatic veins or in the inferior vena cava, is usually caused by one or several underlying prothrombotic disorders (mainly myeloproliferative disorders), similar to the situation for portal vein thrombosis.
Assessment of disease severity and prognosis
Portal pressure as measured by HVPG is close to being a validated surrogate outcome measure in hepatology.15 HVPG can be applied to multiple clinical settings, which are summarized in Box 3.
Chronic viral hepatitis leading to cirrhosis
The development of portal hypertension owing to progression to cirrhosis is the main cause of death in patients with chronic viral hepatitis. However, the usual evaluation parameters for chronic hepatitis (for example, transaminase levels, viral kinetics, and liver biopsy) do not evaluate portal hypertension. Changes in HVPG might be better than standard evaluation parameters for staging chronic hepatitis and for evaluating the response of the disease to antiviral treatment; HVPG offers a much better reflection of liver parenchymal function than does liver biopsy, for example.16 Consistent with this view, HVPG correlates with the degree of histological liver fibrosis in patients with HBV-related17 and HCV-related chronic hepatitis;5 HVPG is over 5 mmHg in the majority of patients with significant fibrosis (stage ≥F2; according to the Metavir scoring system).17 Several studies have compared HVPG measurements taken before and after treatment in patients with chronic hepatitis C. Rincon et al.18 reported a significant reduction in HVPG following antiviral therapy in patients with advanced (Metavir stage F3 or F4) chronic hepatitis C. Combination treatment with pegylated interferon and ribavirin produced clinically significant reductions in HVPG in patients with HCV-related cirrhosis who achieved a sustained viral response to treatment.19 Thus, serial HVPG measurements might be the best way to evaluate the progression or regression of cirrhosis in patients with advanced chronic hepatitis C.
Acute alcoholic hepatitis
Acute alcoholic hepatitis (AAH) is a severe condition with high mortality. In patients with alcoholic cirrhosis, the presence of AAH is associated with elevated HVPG values, which suggests that the inflammatory state of this condition contributes to increased portal pressure.20,21 In patients with severe AAH, HVPG (when measured early during hospitalization) provides prognostic information on short-term outcomes; values >22 mmHg were independently associated with a higher risk of death than were values below this threshold.22
Liver transplantation
In a retrospective study that included patients with cirrhosis who were awaiting liver transplantation, Ripoll and colleagues23 found that HVPG provides prognostic information on survival independent of the Model for End-Stage Liver Disease (MELD) score. Each 1 mmHg increase in HVPG predicted a 3% increase in risk of death. However, the discriminative ability of MELD improved only slightly with the inclusion of HVPG and age variables.
In patients who underwent liver transplantation for HCV-related cirrhosis, HVPG values were more accurate than liver biopsy at identifying the patients who were at highest risk of undergoing decompensation from recurrence of severe hepatitis C. In this setting, fibrosis often develops with a perisinusoidal pattern, which leads to inaccurate staging when scoring systems like the Metavir one are used; for example, patients classified as Metavir stage F2 had HVPG measurements >10–12 mmHg. For this reason, HVPG should be the standard measure to assess chronic viral hepatitis recurrence after orthotopic liver transplantation. The presence of portal hypertension at 12 months after orthotopic liver transplantation, as indicated by a HVPG value ≥6 mmHg, enabled the identification of patients with rapid deterioration of liver function and recurrence of cirrhosis.24,25,26,27 Serial HVPG measurements showed a similar improvement in condition to that seen by liver histology in liver-transplant recipients who responded to antiviral therapy.28
Hepatocellular carcinoma
In a secondary analysis of a randomized, controlled trial in patients with compensated cirrhosis, Ripoll and colleagues29 reported that HVPG, in addition to albumin levels and viral etiology, is an independent predictor of the risk of developing HCC. This risk is substantially higher in patients with clinically significant portal hypertension (HVPG ≥10 mmHg) than in patients with cirrhosis who have HVPG values <10 mmHg.
Similarly, in patients with well-compensated cirrhosis and resectable HCC, the presence of clinically significant portal hypertension markedly increases the risk of unresolved hepatic decompensation occurring within 3 months of hepatic resection.30,31 Surgical resection for HCC should, therefore, be restricted to patients without clinically significant portal hypertension.32
Cirrhosis
HVPG is a strong and independent predictor of several outcomes in patients with cirrhosis. Cross-sectional studies that addressed correlations between clinical and hemodynamic parameters have shown that clinically significant portal hypertension is necessary for gastroesophageal varices to form and bleed.1,33 This link has been confirmed in a prospective, randomized trial carried out in patients with compensated cirrhosis who had no esophageal varices at inclusion. The results showed that the presence of clinically significant portal hypertension is a major determinant of such patients' prognosis, and indicates an increased risk of developing varices,11 first decompensation,13 and HCC on follow-up.29 The importance of HVPG as a prognostic indicator in compensated cirrhosis has been further confirmed in a recent meta-analysis.34
In patients who had already developed decompensation, HVPG provided information about the risk of death during follow-up;23,35,36,37 16 mmHg was the optimum cut-off value for this correlation. On the basis of this evidence, current guidelines recommend the measurement of HVPG as soon as cirrhosis is diagnosed to help stratify patients' risk.38,39
Assessment of new therapeutic agents
The first step in the assessment of a potential new agent for treating portal hypertension should involve testing its capacity to modify this parameter (evaluated as HVPG). Portal hypertension in patients with cirrhosis results from increased resistance to portal blood flow through the liver and increased blood flow in the portal and collateral circulation. Portal hypertension should, therefore, be attenuated by drugs that decrease intrahepatic resistance, porto–collateral blood flow, or both.40
Any single agent, however, is unlikely to decrease the portal pressure sufficiently to completely protect against the risk of variceal bleeding or rebleeding in most patients. Prevention is probably more easily achieved by combinations of drugs that act through different mechanisms. The first drug combination used in patients with portal hypertension was vasopressin and nitroglycerin to treat acute variceal bleeding. The same concept (combining a vasoconstrictor and a nitrate-based vasodilator) was thereafter applied by administering propranolol (which acts as a vasoconstrictor in the splanchnic circulation) and isosorbide-5-mononitrate,41 a combination proven to cause a greater reduction in portal pressure than either drug alone. Another drug that enhances the portal pressure-reducing effect of propranolol is prazosin. The effect of this combination is significantly greater than that of propranolol plus isosorbide-5-mononitrate.42 This effect is mimicked by carvedilol alone, a nonselective β-blocker with intrinsic α1-adrenergic antagonist vasodilatory activity.43 Simvastatin also reduces HVPG, an effect related to the drug's capacity to increase the bioavailability of nitric oxide in the cirrhotic liver and to reduce hepatic vascular resistance.44 This effect was observed whether or not patients were receiving β-blockers, which suggests that the reduction in HVPG observed with simvastatin could potentially be additive to that achieved with β-blockers.44
Response to therapy for portal hypertension
Esophageal varices do not develop unless the HVPG increases to ≥10 mmHg. Variceal bleeding and ascites occur when the value reaches ≥12 mmHg.1,12 Longitudinal studies have demonstrated that if the HVPG falls to ≤12 mmHg, either with drug therapy2,45 or spontaneously (owing to an improvement in liver disease),36 variceal bleeding is totally prevented and varices decrease in size. However, even if this target is not achieved, a decrease in HVPG of ≥20%45 from baseline levels offers almost total protection from variceal bleeding. Lack of achievement of these targets (reduction to ≤12 mmHg or of ≥20% from baseline) constitutes the strongest independent predictor of first variceal bleeding. In patients treated with β-adrenergic blockers with or without nitrates, the incidence of first variceal bleeding at 3 years was <10% in patients in whom HVPG decreased by ≥20% (HVPG 'responders') compared with a 20–40% incidence in 'nonresponders'. In addition, a decrease in HVPG of >15% was associated with a decreased risk of developing spontaneous bacterial peritonitis.46 Occasionally, fundal gastric varices might bleed at HVPG values <12 mmHg.4
Similarly, in patients without varices, or with varices that have never bled, a baseline HVPG of ≥16 mmHg has been consistently associated with an increased risk of death.35,37,47,48,49 Multivariable analysis showed that the value of HVPG was independent of and more accurate than the baseline degree of liver failure as a predictor of survival; thus, HVPG correctly classified patients at increased risk within each Child–Turcotte–Pugh class. In most studies, HVPG was analyzed as a continuous variable, but 16 mmHg seems to be a good cut-off value with which to predict survival.48 Baseline HVPG values do not predict survival in patients with alcoholic cirrhosis.36,50 However, in a study of alcoholic patients who became abstinent, HVPG was significantly reduced and could predict survival when measured after 1 year of abstinence.36
In patients with cirrhosis, early measurement of HVPG during acute variceal bleeding provides useful prognostic information in terms of how the bleeding episode might evolve and the patient's long-term survival. Patients hospitalized because of variceal hemorrhage who had an HVPG ≥20 mmHg were five times more likely to experience failure to control acute variceal bleeding or early rebleeding than those with an HVPG <20 mmHg.51 Patients with elevated HVPG values also required significantly more blood transfusions and days in the intensive care unit, and had a higher overall mortality on follow-up compared with patients with lower HVPG values. The prognostic value of this 20 mmHg threshold has been confirmed in a large series of patients.52,53
A meta-analysis of studies that evaluated the relationship between changes in HVPG and clinical outcome has shown that a good hemodynamic response (a decrease in HVPG of ≥20% from baseline or to ≤12 mmHg) markedly decreases the risk of subsequent rebleeding episodes.54 In addition, a good hemodynamic response was independently associated with a decreased risk of ascites and spontaneous bacterial peritonitis on follow-up and was an independent predictor of survival.55,56 Furthermore, a favorable hemodynamic response predicted survival after adjusting for liver function;55,56 this survival benefit could not be attributed to an improvement in liver function.56 These studies are of enormous conceptual importance, as they indicate that the overall prognosis in patients with cirrhosis who survive a variceal bleeding episode can be improved by decreasing portal pressure.
However, the clinical application of the prognostic value of changes in HVPG is hampered by the need for repeated measurements of HVPG, which is demanding and costly, and by the fact that many patients might bleed before a second HVPG measurement is taken.57 This situation might be improved, at least in part, by performing the second hemodynamic measurement as soon as the maximum tolerated dose of the drugs is reached. In addition, until now, no effective means of predicting the chronic HVPG response in the individual patient existed.
Two studies have shown that evaluation of the acute HVPG response to intravenous propranolol therapy is useful for predicting the efficacy of nonselective β-blockers at preventing first bleeding or rebleeding.58,59 Furthermore, the acute HVPG response to propranolol is independently associated with survival in patients with cirrhosis and portal hypertension.58 Of note, the threshold decrease in HVPG that defines a good response (associated with decreased bleeding and mortality) in these studies was a fall of 10–12% from baseline (rather than the 20% decrease that defines a good chronic response). If adequately validated, evaluation of the acute HVPG response to propranolol might be a more cost-effective strategy than evaluation of the chronic HVPG response, and the former might be useful to guide therapeutic decisions in patients with cirrhosis and portal hypertension.
Changes in HVPG and guidance of therapy
All the aforementioned studies provide a rationale for the use of the hemodynamic response as a marker for the treatment of portal hypertension. These studies demonstrate the potential of using these hemodynamic criteria to tailor the treatment of portal hypertension by measuring the patient's portal pressure response to pharmacological therapy.
Bleeding risk in chronic HVPG responders is extremely low, even lower than that achieved with surgical shunts or transjugular intrahepatic portosystemic shunts.60 Additional treatment (that is, endoscopic band ligation) is, therefore, unlikely to increase treatment efficacy further and might actually increase the risk of adverse events, as has been observed.57 Lifelong therapy with nonselective β-blockers is probably the 'ideal' treatment for HVPG responders. HVPG does not need to be further measured unless a clinical deterioration occurs, which might indicate loss of the HVPG response.
Efforts to improve therapy should focus on HVPG nonresponders. However, data on how to improve the outcome of this high-risk population are scarce and limited to shifting therapy to endoscopic band ligation or adding endoscopic band ligation to treatment with β-blockers. In the study by Bureau et al.,61 patients who did not respond to β-blockers (with or without isosorbide-5-mononitrate) were shifted to undergo endoscopic band ligation, with no benefit. Similarly, a multicenter, randomized controlled trial that compared drug therapy (nadolol with or without isosorbide-5-mononitrate) to the combination of drug therapy and endoscopic band ligation57 found no significant differences in rebleeding rates in HVPG nonresponders treated with drugs alone or with drugs plus endoscopic band ligation. These data suggest that adding endoscopic band ligation might not be the best option for the reduction of rebleeding in HVPG nonresponders; this population probably requires highly effective and aggressive therapy to reduce their high rebleeding risk (46–65% according to a 2003 survey).60 Indeed, Gonzalez et al.62 showed that a low rebleeding rate (19%) was evident in HVPG nonresponders treated with transjugular intrahepatic portosystemic shunt placement. Unfortunately, the study did not include a control group and, until more data become available, HVPG-guided therapy should be used only in the setting of clinical research. In our opinion, unless a very high risk group can be selected, alternative therapy should be based on new drugs or drug combinations rather than on transjugular intrahepatic portasystemic shunt placement.
HVPG-guided therapy has also been evaluated in acute variceal bleeding. As previously mentioned, an HVPG value of ≥20 mmHg independently predicts a poor outcome for this condition. A randomized controlled trial demonstrated that patients from this high-risk population who underwent early transjugular intrahepatic portosystemic shunt placement (within the first 24–48 h of admission) experienced significantly fewer failures to control bleeding and lower overall mortality than patients who received endoscopic therapy.52 These results have been confirmed in a larger, cooperative study of patients with advanced cirrhosis and acute variceal bleeding, in whom early use of transjugular intrahepatic portosystemic shunting with polytetrafluoroethylene-covered stents resulted in a dramatic improvement in terms of bleeding control, rebleeding and survival, compared with the current accepted standard therapy (drug therapy plus endoscopic band ligation).63
Conclusions
Measurement of HVPG remains one of the most useful techniques in the field of hepatology. HVPG is one of the best surrogate markers in chronic liver diseases; this parameter reflects disease severity and has strong prognostic value with regard to survival and decompensation in patients with compensated cirrhosis, during acute bleeding and before liver resection surgery. Furthermore, repeat measurements of HVPG provide unique information on the response to medical treatment of portal hypertension and represent an invaluable tool for developing new drugs for this syndrome. Moreover, changes in HVPG also correlate with the extent of structural changes in the liver, so this measurement is increasingly used to assess the effects of antiviral therapy in hepatitis B-related and hepatitis C-related cirrhosis and to assess the effects of antifibrotic agents. Hepatologists should be familiar with the procedure for measuring HVPG and with interpretation of the results because of the wide range of applications of this measurement.
Review criteria
PubMed was searched in April 2009 for full-text publications in English that contained the terms “HVPG”, “portal hypertension”, “treatment of portal hypertension”, “cirrhosis prognosis”, “beta-blockers” and “cirrhosis”. Additional papers were identified by cross-checking the reference lists of previously identified papers and by referring to the abstract book from conferences of the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. No date limitations were applied.
References
Garcia-Tsao, G. et al. Portal pressure, presence of gastroesophageal varices and variceal bleeding. Hepatology 5, 419–424 (1985).
Groszmann, R. J. et al. Hemodynamic events in a prospective randomized trial of propranolol versus placebo in the prevention of a first variceal hemorrhage. Gastroenterology 99, 1401–1407 (1990).
Groszmann, R. J. & Wongcharatrawee, S. The hepatic venous pressure gradient: anything worth doing should be done right. Hepatology 39, 280–282 (2004).
Bosch, J., Garcia-Pagan, J. C., Berzigotti, A. & Abraldes, J. G. Measurement of portal pressure and its role in the management of chronic liver disease. Semin. Liver Dis. 26, 348–362 (2006).
Perello, A. et al. Wedged hepatic venous pressure adequately reflects portal pressure in hepatitis C virus-related cirrhosis. Hepatology 30, 1393–1397 (1999).
Bosch, J., Abraldes, J. G., Berzigotti, A. & Garcia-Pagan, J. C. Portal hypertension and gastrointestinal bleeding. Semin. Liver Dis. 28, 3–25 (2008).
Keiding, S. & Vilstrup, H. Intrahepatic heterogeneity of hepatic venous pressure gradient in human cirrhosis. Scand. J. Gastroenterol. 37, 960–964 (2002).
Steinlauf, A. F. et al. Low-dose midazolam sedation: an option for patients undergoing serial hepatic venous pressure measurements. Hepatology 29, 1070–1073 (1999).
de Franchis, R., Dell'Era, A. & Primignani, M. Diagnosis and monitoring of portal hypertension. Dig. Liver Dis. 40, 312–317 (2008).
Vizzutti, F., Arena, U., Rega, L. & Pinzani, M. Non-invasive diagnosis of portal hypertension in cirrhotic patients. Gastroenterol. Clin. Biol. 32, 80–87 (2008).
Groszmann, R. J. et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N. Engl. J. Med. 353, 2254–2261 (2005).
Casado, M. et al. Clinical events after transjugular intrahepatic portosystemic shunt: correlation with hemodynamic findings. Gastroenterology 114, 1296–1303 (1998).
Ripoll, C. et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology 133, 481–488 (2007).
Valla, D. C. & Condat, B. Portal vein thrombosis in adults: pathophysiology, pathogenesis and management. J. Hepatol. 32, 865–871 (2000).
Gluud, C., Brok, J., Gong, Y. & Koretz, R. L. Hepatology may have problems with putative surrogate outcome measures. J. Hepatol. 46, 734–742 (2007).
Burroughs, A. K. et al. Assessment of therapeutic benefit of antiviral therapy in chronic hepatitis C: is hepatic venous pressure gradient a better end point? Gut 50, 425–427 (2002).
Kumar, M. et al. Hepatic venous pressure gradient as a predictor of fibrosis in chronic liver disease because of hepatitis B virus. Liver Int. 28, 690–698 (2008).
Rincon, D. et al. Antiviral therapy decreases hepatic venous pressure gradient in patients with chronic hepatitis C and advanced fibrosis. Am. J. Gastroenterol. 101, 2269–2274 (2006).
Roberts, S. et al. Effect of sustained viral response on hepatic venous pressure gradient in hepatitis C-related cirrhosis. Clin. Gastroenterol. Hepatol. 5, 932–937 (2007).
Poynard, T., Degott, C., Munoz, C. & Lebrec, D. Relationship between degree of portal hypertension and liver histologic lesions in patients with alcoholic cirrhosis. Effect of acute alcoholic hepatitis on portal hypertension. Dig. Dis. Sci. 32, 337–343 (1987).
Sen, S. et al. Albumin dialysis reduces portal pressure acutely in patients with severe alcoholic hepatitis. J. Hepatol. 43, 142–148 (2005).
Rincon, D. et al. Prognostic value of hepatic venous pressure gradient for in-hospital mortality of patients with severe acute alcoholic hepatitis. Aliment. Pharmacol. Ther. 25, 841–848 (2007).
Ripoll, C. et al. Influence of hepatic venous pressure gradient on the prediction of survival of patients with cirrhosis in the MELD era. Hepatology 42, 793–801 (2005).
Blasco, A. et al. Hepatic venous pressure gradient identifies patients at risk of severe hepatitis C recurrence after liver transplantation. Hepatology 43, 492–499 (2006).
Carrion, J. A. et al. Transient elastography for diagnosis of advanced fibrosis and portal hypertension in patients with hepatitis C recurrence after liver transplantation. Liver Transpl. 12, 1791–1798 (2006).
Samonakis, D. N. et al. Hepatic venous pressure gradient to assess fibrosis and its progression after liver transplantation for HCV cirrhosis. Liver Transpl. 13, 1305–1311 (2007).
Kalambokis, G. et al. Clinical outcome of HCV-related graft cirrhosis and prognostic value of hepatic venous pressure gradient. Transpl. Int. 22, 172–181 (2009).
Carrion, J. A. et al. Efficacy of antiviral therapy on hepatitis c recurrence after liver transplantation: a randomized controlled study. Gastroenterology 132, 1746–1756 (2007).
Ripoll, C. et al. Hepatic venous pressure gradient predicts development of hepatocellular carcinoma independently of severity of cirrhosis. J. Hepatol. 50, 923–928 (2009).
Bruix, J. et al. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 111, 1018–1022 (1996).
Llovet, J. M., Fuster, J. & Bruix, J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 30, 1434–1440 (1999).
Forner, A. & Bruix, J. East meets the West-—portal pressure predicts outcome of surgical resection for hepatocellular carcinoma. Nat. Clin. Pract. Gastroenterol. Hepatol. 6, 14–15 (2009).
Lebrec, D., De Fleury, P., Rueff, B., Nahum, H. & Benhamou, J. P. Portal hypertension, size of esophageal varices, and risk of gastrointestinal bleeding in alcoholic cirrhosis. Gastroenterology 79, 1139–1144 (1980).
D'Amico, G., Garcia-Tsao, G. & Pagliaro, L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J. Hepatol. 44, 217–231 (2006).
Merkel, C. et al. Prognostic usefulness of hepatic vein catheterization in patients with cirrhosis and esophageal varices. Gastroenterology 102, 973–979 (1992).
Vorobioff, J. et al. Prognostic value of hepatic venous pressure gradient measurements in alcoholic cirrhosis: a 10-year prospective study. Gastroenterology 111, 701–709 (1996).
Gluud, C., Henriksen, J. H. & Nielsen, G. Prognostic indicators in alcoholic cirrhotic men. Hepatology 8, 222–227 (1988).
de Franchis, R. Evolving consensus in portal hypertension: report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J. Hepatol. 43, 167–176 (2005).
Garcia-Tsao, G., Bosch, J. & Groszmann, R. J. Portal hypertension and variceal bleeding-—unresolved issues: summary of an American Association for the Study of Liver Diseases and European Association for the Study of the Liver single-topic conference. Hepatology 47, 1764–1772 (2008).
Bosch, J., Abraldes, J. G. & Groszmann, R. J. Current management of portal hypertension. J. Hepatol. 38, S54–S68 (2003).
Garcia-Pagan, J. C. et al. Enhancement of portal pressure reduction by the association of isosorbide-5-mononitrate to propranolol administration in patients with cirrhosis. Hepatology 11, 230–238 (1990).
Albillos, A. et al. Propranolol plus prazosin compared with propranolol plus isosorbide-5-mononitrate in the treatment of portal hypertension. Gastroenterology 115, 116–123 (1998).
Banares, R. et al. Randomized comparison of long-term carvedilol and propranolol administration in the treatment of portal hypertension in cirrhosis. Hepatology 36, 1367–1373 (2002).
Abraldes, J. G. et al. Simvastatin lowers portal pressure in patients with cirrhosis and portal hypertension: a randomized controlled trial. Gastroenterology 136, 1651–1658 (2009).
Feu, F. et al. Relation between portal pressure response to pharmacotherapy and risk of recurrent variceal haemorrhage in patients with cirrhosis. Lancet 346, 1056–1059 (1995).
Turnes, J. et al. Pharmacological reduction of portal pressure and long-term risk of first variceal bleeding in patients with cirrhosis. Am. J. Gastroenterol. 101, 506–512 (2006).
Tage-Jensen, U. et al. Plasma catecholamine level and portal venous pressure as guides to prognosis in patients with cirrhosis. J. Hepatol. 6, 350–358 (1988).
Merkel, C. et al. The hemodynamic response to medical treatment of portal hypertension as a predictor of clinical effectiveness in the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology 32, 930–934 (2000).
Stanley, A. J., Robinson, I., Forrest, E. H., Jones, A. L. & Hayes, P. C. Haemodynamic parameters predicting variceal haemorrhage and survival in alcoholic cirrhosis. QJM 91, 19–25 (1998).
Urbain, D. et al. Prognostic significance of hepatic venous pressure gradient in medically treated alcoholic cirrhosis: comparison to aminopyrine breath test. Am. J. Gastroenterol. 88, 856–859 (1993).
Moitinho, E. et al. Prognostic value of early measurements of portal pressure in acute variceal bleeding. Gastroenterology 117, 626–631 (1999).
Monescillo, A. et al. Influence of portal hypertension and its early decompression by TIPS placement on the outcome of variceal bleeding. Hepatology 40, 793–801 (2004).
Abraldes, J. G. et al. Hepatic venous pressure gradient and prognosis in patients with acute variceal bleeding treated with pharmacologic and endoscopic therapy. J. Hepatol. 48, 229–236 (2008).
D'Amico, G., Garcia-Pagan, J. C., Luca, A. & Bosch, J. Hepatic vein pressure gradient reduction and prevention of variceal bleeding in cirrhosis: a systematic review. Gastroenterology 131, 1611–1624 (2006).
Abraldes, J. G. et al. Hemodynamic response to pharmacological treatment of portal hypertension and long-term prognosis of cirrhosis. Hepatology 37, 902–908 (2003).
Villanueva, C. et al. Maintenance of hemodynamic response to treatment for portal hypertension and influence on complications of cirrhosis. J. Hepatol. 40, 757–765 (2004).
Garcia-Pagan, J. C. et al. Nadolol plus isosorbide mononitrate alone or associated with band ligation in the prevention of recurrent bleeding: a multicentre randomized controlled trial. Gut 58, 1144–1150 (2009).
LaMura, V. et al. Prognostic value of acute hemodynamic response to i.v. propranolol in patients with cirrhosis and portal hypertension. J. Hepatol. 51, 279–287 (2009).
Villanueva, C. et al. Acute hemodynamic response to β-blockers and prediction of long-term outcome in primary prophylaxis of variceal bleeding. Gastroenterology 137, 119–128 (2009).
Bosch, J. & Garcia-Pagan, J. Prevention of variceal rebleeding. Lancet 361, 952–954 (2003).
Bureau, C. et al. “A la carte” treatment of portal hypertension: adapting medical therapy to hemodynamic response for the prevention of bleeding. Hepatology 36, 1361–1366 (2002).
Gonzalez, A. et al. Hemodynamic response-guided therapy for prevention of variceal rebleeding: an uncontrolled pilot study. Hepatology 44, 806–812 (2006).
Garcia-Pagan, J. C. et al. An early decision for PTFE-TIPS improves survival in high risk cirhotic patients admitted with an acute variceal bleeding: a multicentric RCT [abstract 992]. J. Hepatol. 48, S371 (2008).
Acknowledgements
This work is supported in part by grants from Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación (FIS 06/0623, FIS 08/0193 and SAF 07/61298). CIBERehd is funded by Instituto de Salud Carlos III.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Bosch, J., Abraldes, J., Berzigotti, A. et al. The clinical use of HVPG measurements in chronic liver disease. Nat Rev Gastroenterol Hepatol 6, 573–582 (2009). https://doi.org/10.1038/nrgastro.2009.149
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2009.149
This article is cited by
-
Tissue inhibitor of matrix metalloprotinase-1 and collagen type IV in HCV-associated cirrhosis and grading of esophageal varices
Egyptian Liver Journal (2024)
-
Predictors and Outcomes of Post-transjugular Intrahepatic Portosystemic Shunt Liver Failure in Patients with Cirrhosis
Digestive Diseases and Sciences (2024)
-
Portal hypertension in patients with hepatocellular carcinoma and immunotherapy: prognostic relevance of CT-morphologic estimates
Cancer Imaging (2023)
-
Performance of spleen stiffness measurement by 2D-shear wave elastography in evaluating the presence of high-risk varices: comparative analysis of idiopathic portal hypertension versus hepatitis B virus
BMC Medical Imaging (2023)
-
Innovative angiography: a new approach to discover more hepatic vein collaterals in patients with cirrhotic portal hypertension
BMC Gastroenterology (2023)