Key Points
-
The cancer-immunoediting hypothesis emphasizes that extrinsic immune pressure either can block tumour growth, development and survival or can facilitate tumour outgrowth (by sculpting tumour immunogenicity or by inhibiting host-protective antitumour immune responses). The acquired capacity of developing tumours to escape immune control is a seventh hallmark of cancer.
-
The interferons (IFNs) — both type I IFNs (IFNα and IFNβ) and type II IFN (IFNγ) — have long been recognized as pivotal antiviral and antimicrobial molecules. However, considerable evidence from physiologically relevant tumour models reveals that these molecules also have important roles in protecting the host against tumour development.
-
Endogenously produced IFNγ affects tumour cells directly during the antitumour immune response. IFNγ promotes tumour recognition by increasing the activity of the MHC class I pathway and by modulating the expression of ligands of NKG2D (natural-killer group 2, member D). IFNγ also affects the host immune system by polarization of T helper (TH) cells towards a TH1-cell phenotype, by induction of cytotoxic T lymphocytes and by inhibition of CD4+CD25+ regulatory T-cell development.
-
By contrast, endogenously produced type I IFNs do not act on tumour cells but, instead, on host haematopoietic cells, resulting in inhibition of tumour growth. Similar to tumours that are generated in mice that lack lymphocytes (recombination-activating gene 2 (RAG2)-deficient mice), tumours from mice that lack the IFNAR1 subunit of the type I IFN receptor are highly immunogenic and are therefore 'unedited'.
-
At present, type I IFNs are the only IFNs that are routinely used in a clinical setting for the treatment of cancer patients. Future work focused on controlling local delivery, identifying physiologically relevant IFN-producing cells and identifying IFN-dependent antitumour mechanisms will be vital to translate the well-established antitumour properties of the IFNs from animal modelsto the clinic.
Abstract
A clear picture of the dynamic relationship between the host immune system and cancer is emerging as the cells and molecules that participate in naturally occurring antitumour immune responses are being identified. The interferons (IFNs) — that is, the type I IFNs (IFNα and IFNβ) and type II IFN (IFNγ) — have emerged as central coordinators of tumour–immune-system interactions. Indeed, the decade-old finding that IFNγ has a pivotal role in promoting antitumour responses became the focus for a renewed interest in the largely abandoned concept of cancer immunosurveillance. More recently, type I IFNs have been found to have distinct functions in this process. In this Review, we discuss the roles of the IFNs, not only in cancer immunosurveillance but also in the broader process of cancer immunoediting.
Similar content being viewed by others
Main
As research into tumour immunology continues at an incredible pace, a considerable amount of work is aimed at exploring the mechanisms that underlie the immunological recognition and elimination of cancer and the downstream consequences of these processes. It is now clear that the capacity of the immune system for recognition is not limited solely to the classic models of self versus pathogen or self versus non-self but encompasses the more-subtle differences that exist between self and transformed self. This conclusion provided the argument for reconsidering the largely discarded hypothesis of cancer immunosurveillance. This hypothesis, proposed by Burnet and Thomas1,2 about five decades ago, holds that the immune system protects the host against the development of cancers of non-viral origin. Whereas studies that were carried out on partially immunodeficient mice in the 1970s provided arguments against this hypothesis, many contemporary studies of mice with molecularly defined inactivating defects in innate and/or adaptive immunity have shown that immunodeficient mice do indeed develop more spontaneous and carcinogen-induced tumours than their immunocompetent counterparts3,4,5,6,7 (Table 1). These data, therefore, now overwhelmingly support the existence of an effective cancer-immunosurveillance process in mice. Moreover, clinical data have led to a growing appreciation that cancer immunosurveillance also occurs in humans4,5.
Our understanding of natural immune responses to cancer has further improved following the realization that, as the immune system attempts to constrain tumour growth, tumour cells might escape or attenuate this immune pressure, similar to the way in which these cells evade classic mechanisms of tumour suppression8. This concept evolved from the observation that tumours from immunocompetent hosts and immunodeficient hosts have different immunogenic phenotypes6,9,10,11. Specifically, tumour cells that developed in the presence of an intact immune system — as usually occurs in humans — could form progressively growing tumours when transplanted into immunocompetent recipients, whereas tumour cells from immunodeficient mice were rejected when transplanted into wild-type hosts but not immunodeficient hosts. Therefore, the immunogenicity of a tumour reflects the immunological environment from which it was derived, indicating that the relationship between the immune system and cancer is more complex than was previously thought.
The dual opposing functions of immunity — host protection and tumour promotion — formed the conceptual basis for a process that we named cancer immunoediting3,4,5,6,9 (Fig. 1). The cancer-immunoediting hypothesis emphasizes that extrinsic immune pressure either can block tumour growth, development and survival or can facilitate tumour outgrowth by sculpting tumour immunogenicity or by inhibiting host-protective antitumour responses. In this manner, the acquired capacity of developing tumours to escape immune control is a seventh hallmark of cancer4,8. As depicted in Fig. 1, it is envisaged that the cancer-immunoediting process consists of three phases: elimination (also known as protection), equilibrium (persistence) and escape (progression). It is thought that many different immune cells might interact with tumour cells from the earliest stages of transformation to the terminal phase of widespread metastasis. These interactions are controlled by endogenously produced interferons (IFNs), and recent work indicates that type I IFNs (IFNα and IFNβ) and type II IFN (IFNγ) might have non-redundant functions in the cancer-immunoediting process by affecting distinct target-cell populations. This Review focuses on the recent data that link the IFNs to the immune-mediated elimination of cancer and sculpting of developing tumours (that is, cancer immunoediting).
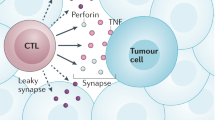
The process of cancer immunoediting is envisaged as three phases: elimination, equilibrium and escape. The first phase, the elimination phase (formerly known as cancer immunosurveillance), consists of the recognition of transformed cells by the innate and the adaptive immune system, leading to the killing of these cells. One recently identified mechanism by which the innate immune system discriminates between self cells and transformed self cells involves the interaction of the natural killer (NK)-cell activating receptor NKG2D (NK group 2, member D) with specific tumour-cell-expressed ligands, which are induced by genotoxic stress, viral infection or chemically mediated transformation89. In addition, CD4+ and CD8+ αβ T cells recognize tumour-specific or tumour-associated antigens in the context of MHC class II and class I molecules, respectively, and B cells produce antibodies that recognize antigens at tumour-cell surfaces (not shown). Recognition by innate and adaptive immune mechanisms leads to direct killing of tumour cells, as well as production of chemokines and other cytokines that facilitate killing of tumour cells. If some tumour cells are not killed in the elimination phase, then the process can progress to the second phase: the equilibrium phase, a subclinical phase in which the tumour persists but is prevented from expanding by immune pressure. The third phase, escape, begins when the balance between the immune response and the tumour tilts towards tumour growth as a result of immune exhaustion or inhibition or as a result of the emergence of tumour-cell variants (shown in purple) that enable the tumour to evade immune pressure. Non-immunogenic transformed cells directly enter the escape phase. This phase concludes with the appearance of clinically detectable, progressively growing tumours. BRCA, breast cancer, early onset; ECM, extracellular matrix; IDO, indoleamine 2,3-dioxygenase; IFN, interferon; MIC, MHC-class-I-polypeptide-related sequence; NK, natural killer; NKT, natural killer T; p53, tumour-suppressor protein p53; RAE1, retinoic acid early transcript 1; Rb, retinoblastoma protein; TRAIL, tumour-necrosis-factor-related apoptosis-inducing ligand; TReg, CD4+CD25+ regulatory T; ULBP, cytomegalovirus UL16-binding protein. This figure is modified, with permission, from Ref. 5 © (2004) Elsevier.
IFNs in cancer immunosurveillance
In the past, the term cancer immunosurveillance was used to describe the protective function of immunity in the control of tumour growth. However, it is now recognized that the scope of the tumour–immune-system interaction is much broader, thereby necessitating expansion of the concept of cancer immunosurveillance to become cancer immunoediting. The concept of cancer immunoediting incorporates the host-protective cancer-immunosurveillance functions of the immune system as the first phase in a multistage process, and these functions are now embodied in the term elimination (protection) (Fig. 1).
The IFN family was originally recognized for its capacity to protect naive cells against viral infection, but it is now known to have important roles in regulating and linking both the innate and the adaptive arms of immunity and has recently been shown to have obligate roles in the elimination phase of cancer immunoediting. Although type I IFNs were originally thought to be mainly antiviral agents, recent studies have shown their importance as immunomodulators12. By contrast, the immunomodulatory activity of IFNγ has long been appreciated, and its roles in the control of host immune responses are well established13. The key similarities and differences between type I IFNs and IFNγ that are important to our broader discussion of these cytokines in the context of cancer immunoediting are summarized in Table 2, and details of the IFN-mediated signalling pathways are presented in Table 2 and Fig. 2. Detailed reviews of IFN biology have been published elsewhere14,15,16.
Interferon-γ (IFNγ; type II IFN) induces reorganization of the IFNγ-receptor subunits, IFNGR1 and IFNGR2, activating the Janus kinases JAK1 and JAK2, which are constitutively associated with each subunit, respectively14,16. The JAKs phosphorylate a crucial tyrosine residue of IFNGR1, forming a STAT1 (signal transducer and activator of transcription 1)-binding site; they then tyrosine phosphorylate receptor-bound STAT1, which homodimerizes through SRC homology 2 (SH2)-domain–phosphotyrosine interactions and is fully activated by serine phosphorylation. STAT1 homodimers enter the nucleus and bind promoters at IFNγ-activated sites (GASs) and induce gene transcription in conjunction with co-activators, such as CBP (cyclic-AMP-responsive-element-binding protein (CREB)-binding protein), p300 and minichromosome maintenance deficient 5 (MCM5)90,91. Disruption of the gene that encodes IFNγ, IFNGR1, IFNGR2, JAK1, JAK2 or STAT1 has shown that each of these molecules is required for signalling through the IFNγ receptor92. Further studies have revealed that IFNγ-mediated signalling is controlled by several mechanisms: by dephosphorylation of IFNGR1, JAK1 and STAT1 (mediated by SH2-domain-containing protein tyrosine phosphatase 2, SHP2)92; by inhibition of the JAKs (mediated by suppressor of cytokine signalling 1, SOCS1)93,94; by proteasomal degradation of the JAKs92; and by inhibition of STAT1 (mediated by protein inhibitor of activated STAT 1, PIAS1)95. The type I IFNs (IFNα and IFNβ) bind a receptor that consists of the subunits IFNAR1 and IFNAR2, which are constitutively associated with tyrosine kinase 2 (TYK2) and JAK1, respectively96,97. Type-I-IFN-induced JAK–STAT signalling is propagated similarly to IFNγ-induced JAK–STAT signalling. Activated TYK2 and JAK1 phosphorylate STAT1 or STAT2. Type-I-IFN-induced signalling then induces homodimerization of STAT1 and heterodimerization of STAT1 and STAT2. STAT1 and STAT2 associate with the cytosolic transcription factor IFN-regulatory factor 9 (IRF9), forming a trimeric complex known as IFN-stimulated gene factor 3 (ISGF3). On entering the nucleus, ISGF3 binds IFN-stimulated response elements (ISREs). Studies of gene-targeted mice have shown that JAK1, STAT1, STAT2 and IRF9 are required for signalling through the type I IFN receptor97. TYK2 is required for optimal type-I-IFN-induced signalling98,99. CTL, cytotoxic T lymphocyte; DC, dendritic cell; NK, natural killer; TH1, T helper 1; TReg, CD4+CD25+ regulatory T. This figure is modified, with permission, from Nature Reviews Immunology Ref. 96 © (2005) Macmillan Publishers Ltd.
IFNγ in cancer immunosurveillance. Although the role of IFNγ in promoting host immune responses to microorganisms is well recognized, the finding that IFNγ also promotes host antitumour immunity reinvigorated interest in the cancer-immunosurveillance process. The original data that pointed to an important role for endogenously produced IFNγ in promoting tumour elimination came from experiments that sought to identify the cytokines required for the lipopolysaccharide (LPS)-dependent rejection of transplanted Meth A cells (which are 3-methylcholanthrene (MCA)-induced fibrosarcoma cells of BALB/c mice)17. Neutralization of IFNγ with a specific monoclonal antibody, but not neutralization of tumour-necrosis factor (TNF) with a specific monoclonal antibody, abrogated the LPS-dependent rejection of Meth A cells. In addition, other sarcomas induced by the carcinogen MCA grew more aggressively when transplanted into naive mice that had been treated with neutralizing IFNγ-specific monoclonal antibody.
The antitumour activity of IFNγ observed in these studies was subsequently confirmed in primary tumorigenesis models. The initial report showed that IFNγ-insensitive 129/Sv mice — lacking either the IFNGR1 subunit of the IFNγ receptor or the transcription factor STAT1 (signal transducer and activator of transcription 1) — developed MCA-induced sarcomas more rapidly and 3–5-fold more frequently than did their wild-type counterparts18. A similar observation was made using C57BL/6 mice that lack the gene that encodes IFNγ19. IFNγ-insensitive mice were also more susceptible to spontaneous tumour formation. Specifically, mice that lack both the tumour-suppressor protein p53 and sensitivity to IFNγ (as a result of deficiency in either IFNGR1 or STAT1) formed tumours significantly more rapidly than did IFNγ-sensitive p53-deficient mice, and these mice also developed a broader range of tumour types18. In another study, IFNγ-deficient C57BL/6 mice developed disseminated lymphomas more frequently than did wild-type mice. By contrast, a small proportion of IFNγ-deficient BALB/c mice developed lung adenocarcinomas but not disseminated lymphomas, whereas wild-type BALB/c mice remained tumour free20. Another study showed that IFNγ cooperates with other cytokines to prevent tumour formation. Mice deficient in both granulocyte/macrophage colony-stimulating factor (GM-CSF) and IFNγ, as well as mice deficient in these cytokines and interleukin-3 (IL-3), developed lymphoma and non-lymphoid solid cancers at a higher rate than did mice deficient in GM-CSF alone, both IL-3 and GM-CSF, or IFNγ alone21. Compared with the other experimental models that have been discussed here, interpretation of this study is complicated by the dependence of neoplasia on infection; therefore, more work is needed to understand the relationships between chronic infection, unopposed inflammation, cancer and immunosurveillance. Nevertheless, taken together, the findings show that IFNγ participates in a cancer elimination (immunosurveillance) process that protects mice against chemically induced, spontaneously arising and transplantable tumours.
Additional studies revealed that the antitumour activity of IFNγ overlaps with that of recombination-activating gene (RAG)-protein-expressing lymphocytes. Specifically, 129/Sv mice that lack IFNγ responsiveness (as a result of IFNGR1 or STAT1 deficiency), 129/Sv mice that lack lymphocytes (as a result of RAG2 deficiency) and 129/Sv mice that lack both (as a result of STAT1 and RAG2 deficiency) showed similar increases in the incidence of MCA-induced sarcomas compared with wild-type controls6. So these data show that the IFNγ-dependent, STAT1-dependent and lymphocyte-dependent pathways of tumour suppression overlap considerably. This conclusion is also supported by other studies of carcinogenesis in which mice that lack both perforin and IFNγ showed only a small increase in the incidence of tumours compared with mice that lack either factor19.
Work has begun to identify the sources of IFNγ during the cancer-elimination phase. A study by Gao et al.22 showed that γδ T cells are an important source of IFNγ during the development of protective antitumour immune responses. This study used two groups of bone-marrow-chimeric mice in which the only difference was the inability of γδ T cells in one group to produce IFNγ. When challenged with MCA, mice with IFNγ-deficient γδ T cells were significantly more susceptible to tumorigenesis than were control mice and showed a tumour incidence equivalent to that seen in IFNγ-deficient mice. Additional studies will be necessary to identify other physiologically relevant sources of IFNγ in the cancer-immunosurveillance process and to elucidate the pathways that lead to IFNγ production.
Studies of the contribution of IL-12 to antitumour immunity provide further insight into the physiologically relevant stimuli for IFNγ production during the cancer-elimination phase. IL-12 regulates the induction of IFNγ expression in both the innate and the adaptive immune compartments13,23,24. A role for the IL-12–IFNγ axis was first shown in tumour therapy models involving administration of exogenous IL-12 to tumour-bearing mice. In one study, IL-12-dependent rejection of MC-38 sarcoma cells was abrogated by injection of neutralizing IFNγ-specific monoclonal antibody25. This observation was extended to primary tumorigenesis models in which mice that were challenged with MCA and treated with exogenous IL-12 formed fewer sarcomas than did control mice26,27. Other experiments showed that mice that lack the p40 subunit of the IL-12 heterodimer developed 2–3-fold more MCA-induced sarcomas than did their wild-type counterparts27. These data show that endogenously produced IL-12 also promotes cancer elimination and mediates some of its antitumour effects through induction of IFNγ expression.
Type I IFNs in cancer immunosurveillance. In the late 1960s, it was shown that mice that were transplanted with syngeneic tumours had significantly increased survival times when treated with crude preparations of type I IFNs28,29. Subsequently, similar results were obtained when type I IFNs were administered to mice with Friend leukaemia cell (FLC) tumours or AGS melanomas (which lack STAT1), or when type I IFNs were ectopically overexpressed in several tumour types30. Although this work, using exogenously delivered type I IFNs, clearly showed the therapeutic antitumour potential of this cytokine family, studies of endogenously produced type I IFNs have only recently assessed its involvement in the cancer-elimination phase.
Gresser and colleagues31 were the first to address this question by showing that neutralizing polyclonal goat antisera specific for mouse type I IFNs increased the growth and metastasis in mice of several different tumour-cell xenografts (human HeLa cells and baby hamster kidney cells). Subsequent work showed that mice that were challenged with either allogeneic or syngeneic mouse tumours showed higher tumour growth rates and significantly decreased survival times when treated with serum that contained IFN-specific antibodies than when treated with control serum32. However, in this study, the FLC tumours that were reported to be syngeneic to the DBA/2 recipient mice actively shed the Friend leukaemia virus, introducing the potentially confounding variable of antiviral immunity to this study of antitumour immunity. Additional efforts have been made to extend these data using tumour-transplantation approaches in mice that lack the IFNAR1 subunit of the type I IFN receptor33. However, because none of these tumours was rejected by wild-type mice, it is difficult to draw firm conclusions about the specific roles of type I IFNs in the cancer-elimination phase on the basis of these models.
A more recent study directly showed the requirement for endogenously produced type I IFNs in protecting hosts against transplanted and primary syngeneic tumours9. Mice that had been treated with blocking monoclonal antibody specific for the type I IFN receptor34 failed to reject a panel of highly immunogenic, unedited, MCA-induced sarcomas that were rejected by wild-type mice that had been treated with a control monoclonal antibody. This result shows that type I IFNs have an obligate role in the elimination of immunogenic syngeneic tumours. This study also shows that type I IFNs participate in naturally occurring, protective immune responses to primary tumours. Specifically, IFNAR1-deficient 129/Sv mice that were challenged with MCA were significantly more susceptible to tumour formation and formed tumours with faster kinetics than their wild-type counterparts. These findings have been independently corroborated using IFNAR1-deficient C57BL/6 mice and IFNAR2-deficient C57BL/6 mice (M. J. Smyth, personal communication).
The findings that both type I IFNs and IFNγ have crucial roles in promoting host antitumour immunity clearly identify these cytokines as pivotal components in the cancer-elimination phase of the cancer-immunoediting process. Therefore, together with the establishment of roles for γδ T cells, αβ T cells, natural killer (NK) cells, natural killer T (NKT) cells, perforin and TNF-related apoptosis-inducing ligand (TRAIL) in protection of the host against tumour formation, the cancer-elimination phase is beginning to be elucidated at the molecular and cellular levels (Table 1). In defining the antitumour machinery of the host, further work is needed to understand how the crucial cells and molecules in different mouse tumour models work together to protect individuals against a broad range of cancers. Therefore, organism-wide immune elimination of cancer might be more relevant to some tissues than others, because it requires the integration of antitumour processes that are specific to the anatomical location, the original cell type and the transformation programme of a tumour.
Cancer immunoediting
Classically, tumour suppression has been considered to be a cell-intrinsic programme mediated by pathways that involve proteins such as p53 and Rb (retinoblastoma protein). These pathways coordinately defend cells from the oncogenic and/or genotoxic stimuli that can lead to malignant transformation35,36. However, the data that support the existence of a cancer-immunosurveillance process illustrate that suppression of tumour growth might also be mediated by extrinsic forces, including the immune system. Additional work has shown that tumour cells that are under the pressure of immunosurveillance behave in a way that is central to tumour biology: they escape the mechanisms that operate to suppress them. The realization that this occurs was the main motivation in changing our thinking about tumour–immune-system interactions and led to the development of the term cancer immunoediting to describe this process3,4,5.
The first phase of cancer immunoediting is elimination, which is the host-protective cancer-immunosurveillance process and represents one possible outcome of immunoediting. Because this mechanism inhibits tumour development and/or growth, it influences the number of tumours that arises. If incomplete, the cancer-immunoediting process can advance to the second phase — equilibrium — in which residual cancer cells that are highly mutable persist in the immunocompetent host. Therefore, equilibrium might be similar to the older concept of tumour dormancy37,38, and it represents either a second possible outcome of cancer immunoediting or a period of transition to the third phase of the cancer-immunoediting process — escape. Cancer cells that develop the capacity to circumvent immunological suppression of tumours, by averting immune responses and/or by directly attenuating the protective antitumour functions of immune effectors, grow progressively and therefore enter the escape phase, which is a third possible outcome of cancer immunoediting. In this manner, immunity influences the immunogenic quality of the tumours that grow.
Whereas the evidence for cancer immunosurveillance has come from studies of tumour incidence, the evidence for cancer immunoediting has come from studies of the immunogenicity of tumours that arise in immunocompetent versus immunodeficient hosts. The clearest demonstration of cancer immunoediting came from studies showing that sarcomas from mice deficient in RAG2 (which are therefore immunodeficient) were significantly more immunogenic (as a group) than tumours from wild-type mice (which arose in the presence of an intact immune system)6. In that study, all MCA-induced sarcomas, from either wild-type mice or RAG2-deficient mice, grew progressively when transplanted into immunodeficient (RAG2 deficient) hosts6. However, whereas all MCA-induced sarcomas from wild-type mice grew progressively when transplanted into wild-type (naive immunocompetent) mice, 40% of tumours from RAG2-deficient mice were rejected by wild-type hosts6. Independent studies have shown that lymphomas and sarcomas from mice deficient in perforin20,39, as well as sarcomas generated in mice deficient in the joining gene segment Jα281 of the T-cell receptor α-chain11,40 (which lack NKT cells), were also highly immunogenic and were rejected by wild-type mice. Studies are ongoing to determine whether the same immune components that constitute the host-protective cancer-immunosurveillance network also participate in the editing functions of immunity.
Recently, one group reported that tumours that develop in immunocompetent mice expressing a cryptic oncogene were immunogenic and were therefore unsculpted41. They used these results to argue against the idea that cancer immunoediting has physiological relevance. However, these oncogene-induced tumour cells caused potent immunosuppression in the tumour-bearing host. Because tumour-induced immunosuppression is an escape mechanism that is integral to cancer immunoediting, we think that the results support the validity of this process rather than refute it.
IFNs in cancer immunoediting
Both type I IFNs and IFNγ have been shown to be crucial components of the cancer-immunoediting process. This is because IFN-unresponsive hosts show an increased tumour incidence, and the tumours that arise in IFN-unresponsive environments are highly antigenic and are therefore qualitatively distinct from sarcomas from wild-type mice. One of the first studies to document the contributions of IFNs to cancer immunoediting centred on IFNγ18. Specifically, tumours that developed in IFNGR1-deficient mice were found to grow aggressively in immunocompetent recipients. However, when sensitivity to IFNγ was conferred on the tumour cells by introducing the receptor subunit IFNGR1, the tumour cells became highly immunogenic and were rejected in a CD4+ and CD8+ T-cell-dependent manner. Therefore, tumours from IFNGR1-deficient mice represent sarcomas that cannot display their inherently high antigenicity because of their inability to respond to IFNγ. These findings indicate that IFNγ has a key role in promoting tumour immunogenicity.
More recently, type I IFNs were also shown to participate in tumour-sculpting effects9. Ninety-five percent of sarcoma cell lines (35 of 36) from wild-type mice grew progressively when transplanted into naive syngeneic mice that were immunocompetent. By contrast, ∼45% of MCA-induced sarcoma cells from IFNAR1-deficient mice were highly immunogenic and were rejected when transplanted into wild-type mice. IFNAR1-deficient MCA-induced sarcomas therefore show an immunogenic phenotype similar to sarcomas from RAG2-deficient mice6.
Supporting evidence for the physiological relevance of IFNs in the cancer-immunoediting process comes from the identification of a subset of naturally arising human tumours that have lost the capacity to signal through the IFN receptors and therefore cannot induce genes that are classically regulated by IFNs. So these tumour cell lines might represent edited tumours that were selected for in vivo outgrowth (escape) by an IFN-dependent cancer-immunoediting process. Specifically, 4 of 17 lung adenocarcinoma cell lines were unable to signal through the IFNγ receptor due to identifiable defects in the proximal IFNγ-receptor signalling cascade: one tumour lacked expression of IFNGR1; two tumours expressed abnormal forms of Janus kinase 2 (JAK2); and one tumour lacked expression of JAK1 (Ref. 18). Another study extended this observation to prostate cancers42. The well-studied cell line LNCaP, which is known to be insensitive to IFNγ43, was found to be unresponsive to type I IFNs as well, owing to repression of JAK1 expression by epigenetic mechanisms. Other studies have identified a set of melanomas that are unresponsive to IFNs as a result of negligible expression of STAT1 or overexpression of STAT5, as well as squamous-cell carcinomas that are resistant to IFNs as a result of reduced STAT1 expression (owing to methylation of the STAT1 promoter)44,45,46. In addition, many tumours that lack expression of immunologically relevant genes that are regulated by IFNs — such as MHC molecules, TAP1 (transporter associated with antigen processing 1) and LMP2 (low-molecular-mass protein 2) — have been identified47,48,49. Moreover, another study showed that overexpression of SOCS1 (suppressor of cytokine signalling 1), a negative regulator of IFN-mediated signalling, correlates with melanoma progression50. Taken together, these data show that, in addition to their involvement in cancer immunosurveillance (that is, in the elimination phase of cancer immunoediting), IFNs can provide the selective pressure that drives the cancer-immunoediting capacity of the immune system, leading to progression into the equilibrium and escape phases.
Cancer immunoediting and IFNγ
A role for IFNγ in increasing tumour immunogenicity. At present, more is known about the cellular targets of IFNγ during cancer immunoediting than the targets of type I IFNs. Studies of Meth A cells were the first to show that tumour cells are obligate targets of IFNγ17. Whereas treatment with LPS induced rejection of parent Meth A cells (which are IFNγ sensitive) growing in syngeneic BALB/c mice, it had no effect on IFNγ-unresponsive Meth A cells overexpressing a dominant-negative IFNGR1 mutant (denoted IFNGR1.ΔIC) that lacked all but three amino-acid residues of the intracellular domain17,51. Moreover, unlike parent Meth A cells, IFNγ-insensitive Meth A cells expressing IFNGR1.ΔIC failed to induce protection against the parent Meth A cell line when transplanted into wild-type mice and then surgically resected. Finally, overexpression of IFNGR1.ΔIC in the MCA-207 sarcoma cell line generated more-aggressive tumours than did the same tumour cell line transfected with empty vector. Subsequently, it was shown that several rejectable (highly immunogenic and poorly tumorigenic) sarcomas from RAG2-deficient mice6 were converted into progressively growing (poorly immunogenic and highly tumorigenic) tumours when rendered insensitive to IFNγ through overexpression of IFNGR1.ΔIC (C.M.K., G.P.D. and R.D.S., unpublished observations). Together, these results show that antigenic tumours become non-immunogenic in the absence of IFNγ sensitivity.
Using the converse approach, Kaplan et al.18 showed that RAD–gR.28 cells, which are MCA-induced sarcoma cells from an IFNGR1-deficient mouse (and therefore are IFNγ unresponsive), grew aggressively in syngeneic 129/Sv mice, even when injected at low cell numbers. By contrast, RAD–gR.28 cells that were engineered to be IFNγ responsive through enforced expression of IFNGR1 were rejected after transplantation into wild-type mice. Similarly, introduction of IFNGR1 into MCA-induced sarcoma cells from a mouse that lacked both IFNGR1 and IFNAR1 converted these cells into highly immunogenic tumour cells that were rejected by wild-type mice9. These results show that a tumour needs to be responsive to IFNγ to be immunogenic. This relationship between the IFNγ sensitivity of a tumour cell and its tumorigenicity has also been noted in models of immunotherapy and angiogenesis52,53.
Additional work from our laboratory has begun to shed light on the mechanisms by which tumour-cell responsiveness to IFNγ contributes to successful, naturally occurring antitumour immune responses. This work has shown that the ability of IFNγ to promote tumour rejection is mediated, at least in part, through its capacity to upregulate the MHC class I pathway of antigen processing and presentation in tumour cells. Specifically, enforced expression of the MHC class I pathway components TAP1 (Ref. 6) or H2-Db (A. T. Bruce and R.D.S., unpublished observations) to levels similar to those in IFNγ-sensitive tumour cells that have been treated with IFNγ was found to convert RAD–gR.28 cells (which are IFNγ insensitive) into cells that were rejected by wild-type mice in a CD8+ T-cell-dependent manner, despite their unresponsiveness to IFNγ. Subsequent work showed that selective overexpression of TAP1 or H2-Db increased the susceptibility of RAD–gR.28 cells to in vitro killing by RAD–gR.28-specific cytotoxic T lymphocytes (CTLs). These findings show that augmented expression of components of the MHC class I pathway is sufficient to induce the rejection of an otherwise IFNγ-insensitive tumour.
A recent finding by Bui et al.54 points to a distinct mechanism by which the effects of IFNγ on tumour-cell immunogenicity might coordinate the progression of the antitumour immune response. In this study, the molecule H60 was identified as the most prevalent ligand for the NK-cell receptor NKG2D (NK group 2, member D) on a range of MCA-induced sarcomas from 129/Sv mice. The in vitro or in vivo exposure of these sarcoma cells to IFNγ or IFNα transcriptionally downregulated H60 expression (resulting in less H60 at the cell surface) while concomitantly upregulating MHC class I expression. Furthermore, in vitro treatment of tumour targets with IFNγ decreased their killing by NK cells in a manner that was independent of IFNγ-induced increases in MHC class I expression. However, increased expression of these MHC molecules enhanced the sensitivity of a tumour to recognition and/or lysis by CTLs. These data indicate that the actions of IFNγ on tumour cells might coordinate the progression of the immune response to growing tumours so that the early recognition and/or elimination of cancer cells by the innate immune system transitions to immune attack by the adaptive immune system.
Because IFNγ regulates various biological programmes14,15 that, a priori, could participate in abrogating tumour growth, additional work is required to identify the full range of IFNγ-induced effects on a tumour that contribute to tumour rejection. Given the scope of this Review, it is not possible to discuss every antitumour mechanism that might be induced by IFNγ; however, some of the processes that might be important include the capacity of IFNγ to inhibit cellular proliferation55,56, to promote apoptosis through effects on the expression of caspases, CD95 (also known as FAS) and TRAIL10,57,58,59, and to inhibit angiogenesis60. Because it is probable that the IFNγ-induced processes that are responsible for eliminating cancer cells might differ by tumour type, it will be important to use in vivo models of primary tumorigenesis to establish the physiological relevance of these IFNγ-induced processes.
Host targets of IFNγ in antitumour immunity. Compared with the role of IFNγ in increasing tumour immunogenicity, less is known about how the effects of IFNγ on host cells might contribute to the antitumour immune response. One demonstration of how IFNγ regulates host antitumour function came from the observation that IFNγ was required for the eradication of IFNγ-insensitive 6132A-PRO tumour cells by lymph-node cells from mice that had been immunized with tumour-antigen-derived peptide61. In other studies, STAT1-deficient mice, which are insensitive to IFNs and have a deficiency in polarization of T helper (TH) cells towards TH1 cells, failed to eliminate IFN-responsive tumour cells that were rejected by wild-type mice62. Furthermore, STAT6-deficient mice, which default to TH1-cell immune responses as a result of a block in the differentiation of TH cells into TH2 cells, rejected tumour cells that grew progressively in wild-type mice63. These studies are consistent with an important role for IFNγ in inducing development of the TH1-cell lineage, rather than the TH2-cell lineage, in turn promoting cell-mediated antitumour immune responses by facilitating CTL maturation and macrophage activation13,23. However, because these studies used mice deficient in STAT1 (and therefore unresponsive to IFNs), additional experiments in mice that lack host-cell sensitivity to only IFNγ are necessary to define the host-cell targets of IFNγ in antitumour immunity.
Another mechanism by which the effects of IFNγ on host immune cells promote effective antitumour immune responses was elucidated by a more recent study showing that IFNγ inhibits the generation and/or activation of naturally occurring (CD4+CD25+) regulatory T (TReg) cells64. Previous work from the same research group showed that immunization of wild-type mice with plasmids encoding specific tumour-expressed self antigens (such as DnaJ-like 2) elicits a potent TReg-cell response65. In both tumour-transplantation studies and MCA-induced carcinogenesis studies, mice that received plasmids encoding tumour-expressed self antigen and IFNγ were found to develop fewer tumours, with slower kinetics, and to mount a less potent TReg-cell response than mice that received plasmids encoding only tumour-expressed self antigen64. These results indicate that early production of IFNγ blocks the development and/or immunosuppressive actions of TReg cells. CD8+ T cells were reported to be the probable source of the IFNγ that was suppressing the TReg cells.
A role for IFNγ in controlling transformation. Ongoing work in several laboratories is only now beginning to address how immunological influences (including chronic inflammation) that occur throughout malignant transformation ultimately determine whether the pro-tumour or antitumour functions of the immune system dominate. Indeed, chronic inflammation has been associated with an increased risk of developing cancer, possibly in response to the chronic production of reactive oxygen and nitrogen species leading to DNA damage, tissue remodelling and, ultimately, transformation66,67. Recent studies have shown that certain pro-inflammatory cytokines (such as IL-23 and TNF) and pro-inflammatory cell types (such as IL-17-producing TH cells, TH17 cells) can promote tumour development and growth, because these tumour processes are decreased in the absence of such cytokines68,69. Furthermore, dysregulation of IFNγ production and IFNγ-mediated signalling has been shown to promote spontaneous carcinogenesis in the colon of mice that express SOCS1 only in T cells and B cells70. Further studies are needed to determine whether the main role of chronic inflammation in tumorigenesis is to increase transformation or to increase tumour growth in cells that have been transformed by other mechanisms, and to identify whether these processes are linked to chronic infection.
Cancer immunoediting and type I IFNs
Immune elimination of type-I-IFN-insensitive tumours. The accumulating data that support the involvement of endogenously produced type I IFNs in host antitumour immunity have fuelled efforts to elucidate the mechanisms that underlie their effects. Type I IFNs have been studied in many disease models and are reported to regulate a panoply of immunological and non-immunological processes71. However, as most of these studies monitored the physiological effects of exogenously delivered type I IFNs, rather than endogenously produced type I IFNs, it is unclear which of the many functions that have been ascribed to type I IFNs are relevant to naturally occurring antitumour immune responses.
A recent study from our laboratory assessed the physiologically relevant cellular targets of type I IFNs during the tumour-rejection process9. This study showed that type I IFNs do not act on tumour cells directly during the antitumour immune response, thereby delineating an important difference between type I IFNs and IFNγ. First, the study found that, despite insensitivity to type I IFNs, four IFNAR1-deficient MCA-induced sarcomas were rejected when transplanted into naive syngeneic wild-type recipients. Second, several other IFNAR1-deficient sarcomas that grew progressively in wild-type mice were not converted into regressor tumours when their sensitivity to type I IFNs was restored by enforced expression of IFNAR1. These findings are in contrast to our observation that progressively growing IFNGR1-deficient MCA-induced sarcomas are converted into highly immunogenic tumour cells that are rejectable when transduced with DNA encoding IFNGR1 (Ref. 18). Third, IFNAR1-deficient sarcoma cells, which are usually rejected by wild-type mice, formed progressively growing tumours when engineered to be insensitive to IFNγ through introduction of the dominant-negative receptor subunit IFNGR1.ΔIC. Last, sarcoma cells from mice deficient in both IFNAR1 and IFNGR1 (which lack sensitivity to both types of IFN) were rejected when sensitivity to IFNγ was restored but not when sensitivity to type I IFNs was restored. Together, these data show that tumour-cell responsiveness to IFNγ, but not type I IFNs, is required for the development of antitumour immune responses, thereby highlighting a clear difference in how these cytokines contribute to the elimination phase of cancer immunoediting.
Host targets of type I IFNs in antitumour immunity. Additional work from our laboratory showed that host cells (rather than tumour cells) are the crucial targets of the antitumour activity of type I IFNs9. Specifically, a panel of highly immunogenic sarcomas were rejected by wild-type mice but grew progressively when transplanted into IFNAR1-deficient mice. Bone-marrow-chimera approaches also showed that host haematopoietic cells need to be sensitive to type I IFNs for tumour rejection to occur. Highly immunogenic sarcoma cell lines were rejected by wild-type mice but formed progressively growing tumours in IFNAR1-deficient mice or RAG2-deficient mice. By contrast, these tumour cells were rejected by lethally irradiated IFNAR1-deficient mice or RAG2-deficient mice that had been reconstituted with wild-type bone marrow. These studies, which show the requirement for host-cell responsiveness to endogenously produced type I IFNs, are consistent with findings that were obtained using exogenously administered type I IFNs. Gresser's research group29,72 showed that treatment with type I IFNs increased the survival of DBA/2 mice that were challenged with either syngeneic IFN-sensitive or syngeneic IFN-insensitive tumour cells, indicating that host cells were the crucial targets of type I IFNs. More recently, the administration of exogenous IFNα was shown to increase the survival of wild-type C57BL/6 mice, but not of STAT1-deficient mice (which are unresponsive to IFNs), that were challenged with AGS tumour cells from a STAT1-deficient mouse73. Taken together, these data indicate that endogenously produced or therapeutically administered type I IFNs mediate their antitumour effects mainly through acting on the haematopoietic cells of the host.
Owing to the broad range of powerful immunoregulatory effects of type I IFNs, many cell types are probably physiologically relevant targets of their antitumour activity. For example, type I IFNs have been found to activate dendritic cells, to increase the cytolytic activity of macrophages and NK cells, to induce the production of IL-15, to prime T cells, to increase the survival of T cells and to increase the production of stromally derived angiostatic molecules74,75. Therefore, it is clear from many studies that type I IFNs can promote numerous immune functions, but further work using appropriate in vivo tumour models is required to reveal which of these immune functions are physiologically relevant for antitumour immunity.
A role for type I IFNs in controlling transformation. In addition to the functions of type I IFNs during the development of immune responses to established tumours, recent findings have raised the possibility that type I IFNs might also have a role at an even earlier stage, in the inhibition of the process by which normal cells are transformed into tumour cells. Specifically, type I IFNs were reported to upregulate expression of the tumour-suppressor protein p53, and IFNβ was found to inhibit the in vitro transformation of wild-type mouse embryonic fibroblasts. Therefore, type I IFNs provide cells with an increased potential to control the transformation process76. Another line of evidence that type I IFNs might have a role in blocking cellular transformation comes from the finding that the endoribonuclease RNaseL, which is regulated by type I IFNs, can function as a tumour suppressor in human cells77. Studies of microdissected prostate tumours from patients with germline mutations in RNASEL showed that there was a loss of heterozygosity at the RNASEL locus. In addition, germline mutations in RNASEL have been linked to the prostate-cancer-susceptibility locus HPC1 (hereditary prostate cancer 1)78 and to a significantly increased risk of developing the disease79. However, it remains unclear whether the tumour-suppressor functions of RNaseL depend on IFNs80. Additional studies are needed to determine whether type I IFNs contribute to the function of tumour-suppressor proteins in physiological models of transformation and whether the targets of the antitumour activity of type I IFNs change during the progression from cellular transformation to malignancy.
Conclusions
In the past 12 years, there has been a reversal in how the interaction of a developing tumour with the otherwise-unperturbed immune system is viewed. From both mouse models and human clinical trials, there is now overwhelming evidence in support of the conclusion that the immune system does indeed protect the host against tumour development, thereby carrying out a cancer immunosurveillance (tumour elimination) function. However, there is also a substantial amount of evidence showing that the immune system can promote tumour growth, either by sculpting tumour immunogenicity or by suppressing host-protective immune effector mechanisms. These diverse effects of immunity on developing tumours form the basis of the cancer-immunoediting hypothesis.
Although, in this Review, we have discussed the strong evidence that supports an obligatory role for IFNs in this process, we have only a 'low-resolution picture' of their functions at present. It is clear that endogenously produced type I IFNs and IFNγ do not function in a completely overlapping manner and that they exert their effects on different host-cell populations. It is also clear that IFNγ, but not IFNα and IFNβ, controls the immunogenicity of tumour cells, possibly as a result of the selective production of IFNγ in the tumour microenvironment. Future efforts need to define better the molecular pathways that are affected by the IFNs, to sharpen the acuity of our picture of the cancer-immunoediting process.
Nevertheless, one could predict that the lessons that have been learned about the roles of the IFNs in promoting natural immune responses to developing tumours should be useful in therapeutic settings. However, except for a few types of cancer (Box 1), this prediction has not yet been realized. The limited success of the therapeutic use of IFNs might reflect our inability to target the right IFNs to the right place at the right dose. This issue is particularly relevant to the IFNs, because nearly all cells constitutively express functional IFN receptors, so systemic administration of these cytokines might not necessarily augment immune effector functions at the tumour site. We speculate that this could lead to a state of immunological 'confusion', resulting in either a lack of appropriate cellular infiltration into the tumour or a state of host-cell or tumour-cell unresponsiveness. Ultimately, we hope that future studies of IFN-dependent cancer immunoediting will provide insights that lead to the development of more-effective IFN-based cancer immunotherapies.
Note added in proof
A recent study adds strong support for the existence of a cancer-immunoediting process in humans. Using a combination of histological and gene-expression analyses, Galon et al.113 showed that the presence, location and density of T cells and their products within colorectal tumours was a much better predictor of the survival of patients witu cancer than the commonly used tumour-staging criteria, which are based on the size and spread of a tumour. These data therefore not only show that naturally occurring immune responses to tumours take place in humans but also support the concept that the immune system can maintain a subclinical tumour in an equilibrium state.
References
Burnet, F. M. Cancer: a biological approach. III. Viruses associated with neoplastic conditions. IV. Practical applications. Br. Med. J. 1, 841–847 (1957).
Thomas, L. in Cellular and Humoral Aspects of the Hypersensitive States (ed. Lawrence, H. S.) 529–532 (Hoeber–Harper, New York, 1959).
Dunn, G. P., Bruce, A. T., Ikeda, H., Old, L. J. & Schreiber, R. D. Cancer immunoediting: from immunosurveillance to tumor escape. Nature Immunol. 3, 991–998 (2002). The first review of the concept of cancer immunoediting, with a focus on the historical evolution of the concept.
Dunn, G. P., Old, L. J. & Schreiber, R. D. The three Es of cancer immunoediting. Annu. Rev. Immunol. 22, 329–360 (2004). A comprehensive review of the concept of cancer immunoediting, including extensive discussion of evidence that cancer immunoediting also occurs in humans.
Dunn, G. P., Old, L. J. & Schreiber, R. D. The immunobiology of cancer immunosurveillance and immunoediting. Immunity 21, 137–148 (2004).
Shankaran, V. et al. IFNγ and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature 410, 1107–1111 (2001). Reveals the dual function — both host protective and tumour sculpting — of cancer immunoediting.
Smyth, M. J., Dunn, G. P. & Schreiber, R. D. Cancer immunosurveillance and immunoediting: the roles of immunity in suppressing tumor development and shaping tumor immunogenicity. Adv. Immunol. 90, 1–50 (2006).
Hanahan, D. & Weinberg, R. A. The hallmarks of cancer. Cell 100, 57–70 (2000). A seminal review that discusses the essential hallmarks of cancer.
Dunn, G. P. et al. A critical function for type I interferons in cancer immunoediting. Nature Immunol. 6, 722–729 (2005). Describes the host-protective and tumour-sculpting activities of type I IFNs in cancer immunoediting.
Takeda, K. et al. Critical role for tumor necrosis factor-related apoptosis-inducing ligand in immune surveillance against tumor development. J. Exp. Med. 195, 161–169 (2002). Reveals an overlapping role for TRAIL and IFNγ in cancer immunoediting.
Crowe, N. Y., Smyth, M. J. & Godfrey, D. I. A critical role for natural killer T cells in immunosurveillance of methylcholanthrene-induced sarcomas. J. Exp. Med. 196, 119–127 (2002). Demonstrates the importance of NKT cells that express a semi-invariant T-cell receptor containing Jα281 and their IFNγ-producing capacity in cancer immunoediting.
Decker, T., Muller, M. & Stockinger, S. The Yin and Yang of type I interferon activity in bacterial infection. Nature Rev. Immunol. 5, 675–687 (2005).
Berenson, L. S., Ota, N. & Murphy, K. M. Issues in T-helper 1 development — resolved and unresolved. Immunol. Rev. 202, 157–174 (2004).
Bach, E. A., Aguet, M. & Schreiber, R. D. The IFNγ receptor: a paradigm for cytokine receptor signaling. Annu. Rev. Immunol. 15, 563–591 (1997).
Boehm, U., Klamp, T., Groot, M. & Howard, J. C. Cellular responses to interferon-γ. Annu. Rev. Immunol. 15, 749–795 (1997).
Stark, G. R., Kerr, I. M., Williams, B. R., Silverman, R. H. & Schreiber, R. D. How cells respond to interferons. Annu. Rev. Biochem. 67, 227–264 (1998).
Dighe, A. S., Richards, E., Old, L. J. & Schreiber, R. D. Enhanced in vivo growth and resistance to rejection of tumor cells expressing dominant negative IFNγ receptors. Immunity 1, 447–456 (1994).
Kaplan, D. H. et al. Demonstration of an interferon γ-dependent tumor surveillance system in immunocompetent mice. Proc. Natl Acad. Sci. USA 95, 7556–7561 (1998). Original description of the importance of IFNγ in cancer immunosurveillance.
Street, S. E., Cretney, E. & Smyth, M. J. Perforin and interferon-γ activities independently control tumor initiation, growth, and metastasis. Blood 97, 192–197 (2001).
Street, S. E., Trapani, J. A., MacGregor, D. & Smyth, M. J. Suppression of lymphoma and epithelial malignancies effected by interferon-γ. J. Exp. Med. 196, 129–134 (2002). Reveals that the functions of IFNγ and perforin in surveillance of spontaneous malignancies are not completely overlapping.
Enzler, T. et al. Deficiencies of GM-CSF and interferon-γ link inflammation and cancer. J. Exp. Med. 197, 1213–1219 (2003).
Gao, Y. et al. γδ T cells provide an early source of interferon-γ in tumor immunity. J. Exp. Med. 198, 433–442 (2003). Shows the importance of IFNγ production by γδ T cells in cancer immunosurveillance.
Tripp, C. S., Wolf, S. F. & Unanue, E. R. Interleukin 12 and tumor necrosis factor α are costimulators of interferon-γ production by natural killer cells in severe combined immunodeficiency mice with listeriosis, and interleukin 10 is a physiologic antagonist. Proc. Natl Acad. Sci. USA 90, 3725–3729 (1993).
Yang, J., Murphy, T. L., Ouyang, W. & Murphy, K. M. Induction of interferon-γ production in TH1 CD4+ T cells: evidence for two distinct pathways for promoter activation. Eur. J. Immunol. 29, 548–555 (1999).
Nastala, C. L. et al. Recombinant IL-12 administration induces tumor regression in association with IFN-γ production. J. Immunol. 153, 1697–1706 (1994).
Noguchi, Y., Jungbluth, A., Richards, E. & Old, L. J. Effect of interleukin 12 on tumor induction by 3-methylcholanthrene. Proc. Natl Acad. Sci. USA 93, 11798–11801 (1996).
Smyth, M. J., Crowe, N. Y. & Godfrey, D. I. NK cells and NKT cells collaborate in host protection from methylcholanthrene-induced fibrosarcoma. Int. Immunol. 13, 459–463 (2001).
Gresser, I., Bourali, C., Levy, J. P., Fontaine-Brouty-Boye, D. & Thomas, M. T. Increased survival in mice inoculated with tumor cells and treated with interferon preparations. Proc. Natl Acad. Sci. USA 63, 51–57 (1969).
Gresser, I., Maury, C. & Brouty-Boye, D. Mechanism of the antitumour effect of interferon in mice. Nature 239, 167–168 (1972).
Belardelli, F., Ferrantini, M., Proietti, E. & Kirkwood, J. M. Interferon-α in tumor immunity and immunotherapy. Cytokine Growth Factor Rev. 13, 119–134 (2002).
Reid, L. M. et al. Influence of anti-mouse interferon serum on the growth and metastasis of tumor cells persistently infected with virus and of human prostatic tumors in athymic nude mice. Proc. Natl Acad. Sci. USA 78, 1171–1175 (1981).
Gresser, I., Belardelli, F., Maury, C., Maunoury, M. T. & Tovey, M. G. Injection of mice with antibody to interferon enhances the growth of transplantable murine tumors. J. Exp. Med. 158, 2095–2107 (1983).
Picaud, S., Bardot, B., De Maeyer, E. & Seif, I. Enhanced tumor development in mice lacking a functional type I interferon receptor. J. Interferon Cytokine Res. 22, 457–462 (2002).
Sheehan, K. C. F. et al. Blocking monoclonal antibodies specific for mouse IFN-α/β receptor subunit 1 (IFNAR1) from mice immunized by in vivo hydrodynamic transfection. J. Interferon Cytokine Res. 26, 809–819 (2006).
Hahn, W. C. & Weinberg, R. A. Rules for making human tumor cells. N. Engl. J. Med. 347, 1593–1603 (2002).
Vogelstein, B. & Kinzler, K. W. Cancer genes and the pathways they control. Nature Med. 10, 789–799 (2004).
Wheelock, E. F., Weinhold, K. J. & Levich, J. The tumor dormant state. Adv. Cancer Res. 34, 107–140 (1981).
Uhr, J. W., Tucker, T., May, R. D., Siu, H. & Vitetta, E. S. Cancer dormancy: studies of the murine BCL1 lymphoma. Cancer Res. 51, 5045s–5053s (1991).
Smyth, M. J. et al. NKG2D function protects the host from tumor initiation. J. Exp. Med. 202, 583–588 (2005). Provides evidence that supports the idea of perforin-dependent cancer immunoediting of NKG2D ligands.
Smyth, M. J. et al. Differential tumor surveillance by natural killer (NK) and NKT cells. J. Exp. Med. 191, 661–668 (2000).
Willimsky, G. & Blankenstein, T. Sporadic immunogenic tumours avoid destruction by inducing T-cell tolerance. Nature 437, 141–146 (2005).
Dunn, G. P., Sheehan, K. C., Old, L. J. & Schreiber, R. D. IFN unresponsiveness in LNCaP cells due to the lack of JAK1 gene expression. Cancer Res. 65, 3447–3453 (2005).
Sanda, M. G. et al. Molecular characterization of defective antigen processing in human prostate cancer. J. Natl Cancer Inst. 87, 280–285 (1995).
Wong, L. H. et al. Interferon-resistant human melanoma cells are deficient in ISGF3 components, STAT1, STAT2, and p48-ISGF3γ. J. Biol. Chem. 272, 28779–28785 (1997).
Xi, S. et al. Decreased STAT1 expression by promoter methylation in squamous cell carcinogenesis. J. Natl Cancer Inst. 98, 181–189 (2006).
Wellbrock, C. et al. STAT5 contributes to interferon resistance of melanoma cells. Curr. Biol. 15, 1629–1639 (2005).
Seliger, B., Maeurer, M. J. & Ferrone, S. Antigen-processing machinery breakdown and tumor growth. Immunol. Today 21, 455–464 (2000).
Algarra, I., Cabrera, T. & Garrido, F. The HLA crossroad in tumor immunology. Hum. Immunol. 61, 65–73 (2000).
Marincola, F. M., Jaffee, E. M., Hicklin, D. J. & Ferrone, S. Escape of human solid tumors from T-cell recognition: molecular mechanisms and functional significance. Adv. Immunol. 74, 181–273 (2000).
Li, Z. et al. Expression of SOCS-1, suppressor of cytokine signalling-1, in human melanoma. J. Invest. Dermatol. 123, 737–745 (2004).
Dighe, A. S., Farrar, M. A. & Schreiber, R. D. Inhibition of cellular responsiveness to interferon-γ (IFNγ) induced by overexpression of inactive forms of the IFNγ receptor. J. Biol. Chem. 268, 10645–10653 (1993).
Coughlin, C. M. et al. Tumor cell responses to IFNγ affect tumorigenicity and response to IL-12 therapy and antiangiogenesis. Immunity 9, 25–34 (1998).
Beatty, G. & Paterson, Y. IFN-γ-dependent inhibition of tumor angiogenesis by tumor-infiltrating CD4+ T cells requires tumor responsiveness to IFN-γ. J. Immunol. 166, 2276–2282 (2001).
Bui, J. D., Carayannopoulos, L. N., Lanier, L. L., Yokoyama, W. M. & Schreiber, R. D. IFN-dependent down-regulation of the NKG2D ligand H60 on tumors. J. Immunol. 176, 905–913 (2006).
Chin, Y. E. et al. Cell growth arrest and induction of cyclin-dependent kinase inhibitor p21WAF1/CIP1 mediated by STAT1. Science 272, 719–722 (1996).
Bromberg, J. F., Horvath, C. M., Wen, Z., Schreiber, R. D. & Darnell, J. E. Jr. Transcriptionally active Stat1 is required for the antiproliferative effects of both interferon α and interferon γ. Proc. Natl Acad. Sci. USA 93, 7673–7678 (1996).
Chin, Y. E., Kitagawa, M., Kuida, K., Flavell, R. A. & Fu, X. Y. Activation of the STAT signaling pathway can cause expression of caspase 1 and apoptosis. Mol. Cell. Biol. 17, 5328–5337 (1997).
Xu, X., Fu, X. Y., Plate, J. & Chong, A. S. IFN-γ induces cell growth inhibition by Fas-mediated apoptosis: requirement of STAT1 protein for up-regulation of Fas and FasL expression. Cancer Res. 58, 2832–2837 (1998).
Meng, R. D. & El-Deiry, W. S. p53-independent upregulation of KILLER/DR5 TRAIL receptor expression by glucocorticoids and interferon-γ. Exp. Cell Res. 262, 154–169 (2001).
Luster, A. D. & Leder, P. IP-10, a C-X-C-chemokine, elicits a potent thymus-dependent antitumor response in vivo. J. Exp. Med. 178, 1057–1065 (1993).
Mumberg, D. et al. CD4+ T cells eliminate MHC class II-negative cancer cells in vivo by indirect effects of IFN-γ. Proc. Natl Acad. Sci. USA 96, 8633–8638 (1999).
Fallarino, F. & Gajewski, T. F. Differentiation of antitumor CTL in vivo requires host expression of Stat1. J. Immunol. 163, 4109–4113 (1999).
Kacha, A. K., Fallarino, F., Markiewicz, M. A. & Gajewski, T. F. Spontaneous rejection of poorly immunogenic P1.HTR tumors by Stat6-deficient mice. J. Immunol. 165, 6024–6028 (2000).
Nishikawa, H. et al. IFN-γ controls the generation/activation of CD4+CD25+ regulatory T cells in antitumor immune response. J. Immunol. 175, 4433–4440 (2005). Illustrates the important influence of IFNγ on T Reg -cell-dependent suppression of cancer immunosurveillance.
Nishikawa, H. et al. CD4+ CD25+ T cells responding to serologically defined autoantigens suppress antitumor immune responses. Proc. Natl Acad. Sci. USA 100, 10902–10906 (2003).
de Visser, K. E., Eichten, A. & Coussens, L. M. Paradoxical roles of the immune system during cancer development. Nature Rev. Cancer 6, 24–37 (2006).
Kawanishi, S., Hiraku, Y., Pinlaor, S. & Ma, N. Oxidative and nitrative DNA damage in animals and patients with inflammatory diseases in relation to inflammation-related carcinogenesis. Biol. Chem. 387, 365–372 (2006).
Langowski, J. L. et al. IL-23 promotes tumour incidence and growth. Nature 442, 461–465 (2006). Details the importance of the IL-12 and IL-23 cytokine milieu in determining the balance between the tumour-promoting and tumour-suppressive actions of the antitumour immune response. And begins to synthesize, into one process, the seemingly contradictory processes of tumour-promoting inflammatory reactions and host-protective immune responses.
Moore, R. J. et al. Mice deficient in tumor necrosis factor-α are resistant to skin carcinogenesis. Nature Med. 5, 828–831 (1999).
Hanada, T. et al. IFNγ-dependent, spontaneous development of colorectal carcinomas in SOCS1-deficient mice. J. Exp. Med. 203, 1391–1397 (2006).
Brassard, D. L., Grace, M. J. & Bordens, R. W. Interferon-α as an immunotherapeutic protein. J. Leukoc. Biol. 71, 565–581 (2002).
Belardelli, F., Gresser, I., Maury, C. & Maunoury, M. T. Antitumor effects of interferon in mice injected with interferon-sensitive and interferon-resistant Friend leukemia cells. I. Int. J. Cancer 30, 813–820 (1982).
Lesinski, G. B. et al. The antitumor effects of IFN-α are abrogated in a STAT1-deficient mouse. J. Clin. Invest. 112, 170–180 (2003).
Bogdan, C., Mattner, J. & Schleicher, U. The role of type I interferons in non-viral infections. Immunol. Rev. 202, 33–48 (2004).
Kerbel, R. & Folkman, J. Clinical translation of angiogenesis inhibitors. Nature Rev. Cancer 2, 727–739 (2002).
Takaoka, A. et al. Integration of interferon-α/β signalling to p53 responses in tumour suppression and antiviral defence. Nature 424, 516–523 (2003).
Silverman, R. H. Implications for RNase L in prostate cancer biology. Biochemistry 42, 1805–1812 (2003).
Carpten, J. et al. Germline mutations in the ribonuclease L gene in families showing linkage with HPC1. Nature Genet. 30, 181–184 (2002).
Casey, G. et al. RNASEL Arg462Gln variant is implicated in up to 13% of prostate cancer cases. Nature Genet. 32, 581–583 (2002).
Urisman, A. et al. Identification of a novel γ retrovirus in prostate tumors of patients homozygous for R462Q RNASEL variant. PLoS Pathog. 2, e25 (2006).
Kirkwood, J. M. et al. Interferon α-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. J. Clin. Oncol. 14, 7–17 (1996).
Gogas, H. et al. Prognostic significance of autoimmunity during treatment of melanoma with interferon. N. Engl. J. Med. 354, 709–718 (2006).
Gleave, M. E. et al. Interferon γ-1b compared with placebo in metastatic renal-cell carcinoma. Canadian Urologic Oncology Group. N. Engl. J. Med. 338, 1265–1271 (1998).
Wiesenfeld, M. et al. Controlled clinical trial of interferon-γ as postoperative surgical adjuvant therapy for colon cancer. J. Clin. Oncol. 13, 2324–2329 (1995).
Jett, J. R. et al. Phase III trial of recombinant interferon γ in complete responders with small-cell lung cancer. J. Clin. Oncol. 12, 2321–2326 (1994).
Windbichler, G. H. et al. Interferon-γ in the first-line therapy of ovarian cancer: a randomized phase III trial. Br. J. Cancer 82, 1138–1144 (2000).
Giannopoulos, A. et al. The immunomodulating effect of interferon-γ intravesical instillations in preventing bladder cancer recurrence. Clin. Cancer Res. 9, 5550–5558 (2003).
Lienard, D., Eggermont, A. M., Kroon, B. B., Schraffordt Koops, H. & Lejeune, F. J. Isolated limb perfusion in primary and recurrent melanoma: indications and results. Semin. Surg. Oncol. 14, 202–209 (1998).
Gasser, S. & Raulet, D. H. The DNA damage response arouses the immune system. Cancer Res. 66, 3959–3962 (2006).
Zhang, J. J. et al. Two contact regions between Stat1 and CBP/p300 in interferon γ signaling. Proc. Natl Acad. Sci. USA 93, 15092–15096 (1996).
DaFonseca, C. J., Shu, F. & Zhang, J. J. Identification of two residues in MCM5 critical for the assembly of MCM complexes and Stat1-mediated transcription activation in response to IFN-γ. Proc. Natl Acad. Sci. USA 98, 3034–3039 (2001).
Schreiber, G. H. & Schreiber, R. D. in The Cytokine Handbook 4th edn (eds Thomson, A. & Lotze, M.) 567–601 (Academic, London, 2003).
Alexander, W. S. et al. SOCS1 is a critical inhibitor of interferon γ signaling and prevents the potentially fatal neonatal actions of this cytokine. Cell 98, 597–608 (1999).
Marine, J. C. et al. SOCS1 deficiency causes a lymphocyte-dependent perinatal lethality. Cell 98, 609–616 (1999).
Liu, B. et al. PIAS1 selectively inhibits interferon-inducible genes and is important in innate immunity. Nature Immunol. 5, 891–898 (2004).
Platanias, L. C. Mechanisms of type-I- and type-II-interferon-mediated signalling. Nature Rev. Immunol. 5, 375–386 (2005).
Pestka, S., Krause, C. D. & Walter, M. R. Interferons, interferon-like cytokines, and their receptors. Immunol. Rev. 202, 8–32 (2004).
Karaghiosoff, M. et al. Partial impairment of cytokine responses in Tyk2-deficient mice. Immunity 13, 549–560 (2000).
Shimoda, K. et al. Tyk2 plays a restricted role in IFNα signaling, although it is required for IL-12-mediated T cell function. Immunity 13, 561–571 (2000).
Girardi, M. et al. Regulation of cutaneous malignancy by γδ T cells. Science 294, 605–609 (2001).
Girardi, M. et al. The distinct contributions of murine T cell receptor (TCR)γδ+ and TCRαβ+ T cells to different stages of chemically induced skin cancer. J. Exp. Med. 198, 747–755 (2003).
Smyth, M. J. et al. Perforin-mediated cytotoxicity is critical for surveillance of spontaneous lymphoma. J. Exp. Med. 192, 755–760 (2000).
Hayashi, T. & Faustman, D. L. Development of spontaneous uterine tumors in low molecular mass polypeptide-2 knockout mice. Cancer Res. 62, 24–27 (2002).
Nishikawa, H. et al. Accelerated chemically induced tumor development mediated by CD4+CD25+ regulatory T cells in wild-type hosts. Proc. Natl Acad. Sci. USA 102, 9253–9257 (2005).
Mitra-Kaushik, S., Harding, J., Hess, J., Schreiber, R. & Ratner, L. Enhanced tumorigenesis in HTLV-1 tax-transgenic mice deficient in interferon-γ. Blood 104, 3305–3311 (2004).
Street, S. E. et al. Innate immune surveillance of spontaneous B cell lymphomas by natural killer cells and γδ T cells. J. Exp. Med. 199, 879–884 (2004).
van den Broek, M. F. et al. Decreased tumor surveillance in perforin-deficient mice. J. Exp. Med. 184, 1781–1790 (1996).
Cretney, E. et al. Increased susceptibility to tumor initiation and metastasis in TNF-related apoptosis-inducing ligand-deficient mice. J. Immunol. 168, 1356–1361 (2002).
Zerafa, N. et al. TRAIL deficiency accelerates hematological malignancies. J. Immunol. 175, 5586–5590 (2005).
Hayakawa, Y., Rovero, S., Forni, G. & Smyth, M. J. α-Galactosylceramide (KRN7000) suppression of chemical- and oncogene-dependent carcinogenesis. Proc. Natl Acad. Sci. USA 100, 9464–9469 (2003).
Barchet, W., Blasius, A., Cella, M. & Colonna, M. Plasmacytoid dendritic cells: in search of their niche in immune responses. Immunol. Res. 32, 75–84 (2005).
Ikeda, H., Old, L. J. & Schreiber, R. D. The roles of IFNγ in protection against tumor development and cancer immunoediting. Cytokine Growth Factor Rev. 13, 95–109 (2002).
Galon, J. et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313, 1960–1964 (2006).
Acknowledgements
The authors are grateful to the following individuals: L. J. Old and M. J. Smyth for past and continuing collaborations and for critical comment during the preparation of this Review; G. P. Linette for helpful comment on the clinical use of IFNs in cancer immunotherapy; and all past and present members of the Schreiber laboratory for their essential contributions to the development of the cancer-immunoediting hypothesis. This work was supported by grants from the National Cancer Institute (United States), the Ludwig Institute for Cancer Research (United States) and the Cancer Research Institute (United States).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Related links
FURTHER INFORMATION
Glossary
- Transformation
-
The process of conversion of a normal cell into a cancer cell.
- Cancer immunosurveillance
-
Immunological protection of the host against the development of cancer, resulting from immune effector functions stimulated by immune recognition of either stress ligands or antigens expressed on transformed cells.
- Hallmarks of cancer
-
A specific set of features that must be acquired by a malignant cell. These features are self-sufficiency in growth signals, insensitivity to growth-inhibitory signals, evasion of apoptotic cell death, limitless replicative potential, sustained angiogenesis, tissue invasion and evasion of the antitumour immune response.
- Primary tumorigenesis
-
Transformation and tumour formation that occurs entirely in the original host, in contrast to tumour formation in a host owing to transplantation of cells that were transformed in another host or in vitro.
- γδ T cell
-
T cells express either a T-cell receptor (TCR) composed of an α-subunit and a β-subunit (αβ-TCR) or a TCR composed of a γ-subunit and a δ-subunit (γδ-TCR). T cells that express αβ-TCRs mainly recognize antigenic peptides bound to conventional MHC class I or class II molecules. T cells that express γδ-TCRs are less abundant, and the ligands for these receptors are less well characterized.
- Natural killer T cell
-
(NKT cell). A T cell that expresses both natural killer (NK)-cell receptors and an αβ T-cell receptor. NKT cells are characterized by cytolytic activity and by rapid production of cytokines (including interferon-γ and interleukin-4), and they might regulate the function of other T cells.
- Epigenetic
-
Any heritable influence on the function of a chromosome or gene that is not caused by a change in DNA sequence.
- Regressor tumour
-
A cell line derived from a primary tumour that is rejected when transplanted into naive syngeneic hosts that are immunocompetent but grows progressively in syngeneic hosts that are immunocompromised.
- Angiostatic molecule
-
A molecule that blocks or opposes the growth of blood vessels and the formation of new blood vessels.
Rights and permissions
About this article
Cite this article
Dunn, G., Koebel, C. & Schreiber, R. Interferons, immunity and cancer immunoediting. Nat Rev Immunol 6, 836–848 (2006). https://doi.org/10.1038/nri1961
Issue Date:
DOI: https://doi.org/10.1038/nri1961
This article is cited by
-
Immunotherapy for Brain Tumors: Where We Have Been, and Where Do We Go From Here?
Current Treatment Options in Oncology (2024)
-
BRAF D594A mutation defines a unique biological and immuno-modulatory subgroup associated with functional CD8+ T cell infiltration in colorectal cancer
Journal of Translational Medicine (2023)
-
The crucial regulatory role of type I interferon in inflammatory diseases
Cell & Bioscience (2023)
-
The diagnostic/prognostic roles and biological function of the IFIT family members in acute myeloid leukemia
BMC Medical Genomics (2023)
-
Novel role of immune-related non-coding RNAs as potential biomarkers regulating tumour immunoresponse via MICA/NKG2D pathway
Biomarker Research (2023)