Abstract
Outcomes of kidney transplantation, in terms of graft and patient survival, have improved over the past few decades, partly as a result of the introduction of new immunosuppressive drugs. Many immunosuppressive agents are associated with an increased risk of cardiovascular events and an increased risk of cancer, however, which can compromise patient survival. Cancer is more common among solid-organ transplant recipients than it is in the general population or in patients on dialysis. In fact, malignancy is the third most common cause of death in renal transplant recipients. Immunosuppressive treatments used in renal transplant recipients can cause malignancy by supporting oncogenesis caused by certain viruses or by impairing immune surveillance thereby enabling faster tumor growth. In this Review, we describe the epidemiological and clinical characteristics of common tumor types occurring after kidney transplantation, and the etiopathogenetic factors that lead to their appearance, with a particular focus on the relationship between immunosuppressive treatment and malignancy. Immunosuppressive drugs associated with an increased risk of malignancy after transplantation are also discussed, as are immunosuppressive drugs that seem to have antioncogenic properties.
Key Points
-
Malignancy is the third most common cause of death after renal transplantation
-
Common malignancies in renal transplant recipients include skin cancer, melanoma, Kaposi's sarcoma and post-transplantation lymphoproliferative disorders
-
Factors associated with the development of cancer in transplant recipients include carcinogenic factors, impaired immune surveillance owing to immunosuppression, a genetic predisposition to cancer and the presence of certain viral infections
-
Renal transplant recipients should be screened for cancer regularly after transplantation to enable early intervention when necessary
-
Immunosuppressive treatments in renal transplant recipients should be modulated to try and balance the risks of graft rejection and cancer development
-
Malignancies should be managed with specific therapies for the particular tumor type and with strategies such as immunosuppression reduction, immunosuppression withdrawal or conversion to alternative immunosuppressive regimens
Similar content being viewed by others
Introduction
Patients with end-stage renal disease who undergo renal transplantation have superior overall survival and a better quality of life than patients on long-term dialysis.1,2 Several studies have demonstrated that renal transplantation is associated with a lower risk of mortality than staying on the transplantation waiting list on dialysis.3,4,5 As this finding has been confirmed in different age groups,6 in patients with diabetes,6 in patients of different ethnicities,6 and in patients who have been on long-term dialysis,7 renal transplantation seems to be the treatment of choice for patients with end-stage renal disease.
Outcomes of renal transplantation have improved over the past few decades, partly as a result of the development of new immunosuppressive drugs. The introduction of drugs such as tacrolimus and mycophenolate mofetil has decreased the incidence of acute graft rejection in renal transplant recipients.8,9 Although the reduction in rates of acute graft rejection has resulted in improved survival rates,8,9 chronic graft rejection is still a very common complication. Solid-organ transplant recipients who receive chronic treatment with immunosuppressive agents to prevent allograft rejection, however, have a higher risk of developing a malignancy than do the general population.10 In fact, malignancy is the third most common cause of death (after cardiovascular events and infection) among renal transplant recipients at all time points after transplantation.11,12,13 In this Review, we discuss the topic of malignancy following renal transplantation, focusing on the influence of immunosuppressive agents on the development of tumors or the prevention of malignancies.
General epidemiology
The etiology of post-transplantation malignancy seems to be multifactorial and probably involves a combination of the following events: impaired immune activity against viruses, impaired immunosurveillance of neoplastic cells, DNA damage and disruption of DNA repair mechanisms, and the upregulation of cytokines that can promote tumor progression (for example, transforming growth factor β1, interleukin [IL]-10, and vascular endothelial growth factor).14 All of these events certainly occur during long-term immunosuppressive therapy after renal transplantation.14
Many studies have focused on the relative incidences of malignancies following solid-organ transplantation.14,15,16,17,18,19 Solid-organ transplantation has been associated with the following increases in cancer incidence: a 20-fold increase in the incidence of non-melanoma skin cancers, Kaposi's sarcoma, and non-Hodgkin lymphomas; a 15-fold increase in the incidence of renal cell cancer; a fivefold increase in the incidence of melanoma, leukemia, and hepatobiliary, cervical, and vulvovaginal cancers; a threefold increase in the incidence of testicular and bladder cancer; and a twofold increase in the incidence of common tumors such as colon, lung, prostate, stomach, esophagus, pancreas, ovary, and breast tumors.14
Immunosuppression during the premalignant phase, however, has been shown to reduce the incidence of breast cancer and prolong life in mice.20 In addition, one series found that the incidence of breast cancer was 25–30% lower in women who were receiving immunosuppressive therapy after kidney or heart transplantation than it was in the general population.21 This reduction in the incidence of breast cancer might be the result of immunosuppressive therapies directly inhibiting specific immune mechanisms that can promote the development of breast cancer tumors in some women.21
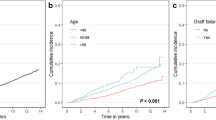
The risk of developing cancer is reported to be 2–4-fold higher among heart transplant recipients than among kidney transplant recipients.10,22,25 This finding is probably related to the fact that patients who have undergone heart transplantation require higher doses of immunosuppressive agents to prevent rejection. Renal transplant recipients aged <50 years have higher standardized cancer mortality ratios than the general population.26
Clinical characteristics
The clinical characteristics of malignancies after renal transplantation are of course related to the origin of the cancer. The time of presentation also depends on the nature of the malignancy, but one study found that the average time to cancer development was approximately 3 years after transplantation.27 For several common cancers, it seems that solid-organ transplant recipients experience worse outcomes than the general population.28 In addition, at the time of diagnosis, cancers seem to be more aggressive in solid-organ transplant recipients than in the general population.28
Skin cancer
Non-melanoma skin cancers are the most common cancer type following solid-organ transplantation.17,29 Basal cell carcinomas and squamous cell carcinomas account for >90% of all non-melanoma skin cancers occurring in solid-organ transplant recipients.17,29 Non-melanoma skin cancers have been reported to occur an average of 8 years after renal transplantation in recipients aged <40 years, and more quickly—after 3 years—in recipients aged >60 years; however, these data might only be a function of the follow-up period of the particular studies.30,31 In the general population, basal cell carcinoma is more common than squamous cell carcinoma.32
Squamous cell carcinoma is the most frequent non-melanoma skin cancer occurring after solid-organ transplantation, with the risk being 100 times greater in transplant recipients than in the general population; the incidence of basal cell carcinoma is 10-fold higher in transplant recipients than in the general population.29 Both tumor types are generally more aggressive in transplant recipients than in the general population, and the risk of recurrence after treatment is generally higher.29 Lesions also generally develop at a younger age in transplant recipients and are more likely to occur in multiple sites.29
The most important risk factor for the development of non-melanoma skin cancer in renal transplant recipients is prior exposure to ultraviolet radiation.33 In addition, the development of squamous cell carcinoma is usually associated with premalignant keratoses, Bowen's disease (squamous cell carcinoma in situ), and/or keratoacanthomas.27 A predictive index has been developed that could be used to enable targeted screening for non-melanoma skin cancer in renal transplant recipients.33 Predictive factors used in the index include age, outdoor ultraviolet radiation exposure, living in a hot climate, pretransplantation non-melanoma skin cancer, sunburn during childhood, and skin type.33
Melanoma
The risk of developing melanoma is 3.6 times greater in renal transplant recipients than in the general population.34 An analysis of the Australia and New Zealand Dialysis and Transplant Registry and the Australian National Cancer Statistics Clearing House showed that the risk of the development of melanoma in renal transplant recipients is positively associated with increasing age at transplantation and with the use of depleting anti-lymphocyte antibodies. By contrast, female sex, non-Caucasian race, and increasing time since transplantation were found to be inversely associated with risk of melanoma development.34 Although renal transplant recipients are at increased risk of melanoma, some studies have found that the outcomes of melanoma in transplant recipients are no different to those in the general population.35,36 Another study, however, reported that outcomes may be worse in transplant recipients than in the general population, as transplant recipients are more likely to have more advanced malignant melanoma at the time of diagnosis.28
Kaposi's sarcoma
The incidence of Kaposi's sarcoma is much higher in renal transplant recipients than in the general population.16 Kaposi's sarcoma is three times more common in male renal transplant recipients than in female renal transplant recipients.37 Kaposi's sarcoma is caused by human herpesvirus 8, as will be discussed. Most cases of post-transplantation Kaposi's sarcoma occur in individuals of Mediterranean, Jewish, Arabic, Caribbean, or African descent, a finding that probably corresponds with the geographic distribution of human herpesvirus 8.37 The choice of immunosuppressive therapy can also affect the risk of post-transplantation Kaposi's sarcoma: calcineurin inhibitors are associated with a higher risk of Kaposi's sarcoma development than are other immunosuppressive therapies.38
Classically, Kaposi's sarcoma presents as angiomatous lesions predominantly affecting the legs and causing lymphedema. Lesions can also occur on mucosal surfaces, lungs, gastrointestinal tract and lymphoid tissue.38 Kaposi's sarcoma is often limited to the skin in transplant recipients, but visceral involvement—which is associated with a worse prognosis—occurs in 10% of patients.38 The incidence of visceral involvement is lower in kidney transplant recipients than in heart or liver transplant recipients, probably because immunosuppression regimes involving calcineurin inhibitors are less intensive in renal transplantation.38 A 2009 multicenter French study in a large cohort of renal transplant recipients found that the presence of pre-existing or acquired human herpesvirus 8 infection had no effect on patient and graft survival, which suggests that patients who are seropositive for human herpesvirus 8 should not automatically be excluded from transplantation.39
Lymphoproliferative disorders
Post-transplantation lymphoproliferative disorder (PTLD) is a heterogeneous group of diseases characterized by abnormal lymphoid proliferation occurring after organ transplantation.40 Although PTLD usually presents as host-derived B-cell neoplasia, T-cell and donor-derived lymphomas have also been described.40 PTLD is more common among transplant recipients than B-cell and T-cell lymphoproliferative disorders are in the general population and in patients on the waiting list for transplantation.18 A study that analyzed United States Renal Data System data from 66,159 adult Medicare-covered kidney transplant recipients found that malignant lymphoid proliferations developed in 1,169 patients (1.8%) over an average follow-up duration of 10 years.41 Among these patients, 70% were diagnosed with non-Hodgkin lymphoma, 14% with multiple myeloma, 11% with lymphoid leukemia, and 5% with Hodgkin lymphoma.41 In pediatric renal transplant recipients, the reported incidence of PTLD approaches 5% at 10 years after transplantation.42
Although the average time to development of PTLD is 32 months after transplantation,41 the incidence of lymphoma development is highest during the first year after transplantation, when the risk of primary viral infection is highest and the level of immunosuppression is greatest.41 Notably, non-Hodgkin lymphoma has a more aggressive clinical course in renal transplant recipients than in the general population, with the involvement of extranodal areas and poorer outcome.41
Other cancers
Merkel's cell carcinoma
Merkel's cell carcinoma, an aggressive neuroendocrine skin cancer, has also been described in solid-organ transplant recipients.43,44 This cancer predominantly affects the head, neck and upper extremities, and has a more aggressive outcome in transplant recipients than in the general population. The mean time of occurrence of Merkel's cell carcinoma after transplantation has been reported to be approximately 7 years and mean survival after diagnosis is 18 months (range 0–135 months).43,44
Squamous cell carcinoma of the eye
The incidence of squamous cell carcinoma of the eye has also been described to be 20-fold higher in renal transplant recipients than in the general population.45 The incidence of squamous cell carcinoma of the eye is also increased in individuals with HIV infection, which suggests that this cancer type has an origin related to immune deficiency. This malignancy has also, however, been found to be associated with sun exposure.45
Cancers involving the anogenital region
The incidence of cancers involving the anogenital region have been reported to be 100-fold higher among renal transplant recipients than in the general population.17,46,47 The distribution of such cancer involves multiples sites, including the anus, perianal skin, and external genitalia of both sexes, and clinically this cancer manifests as maculopapular lesions.17,46,47
Lung cancer
The incidence of lung cancer is higher in heart or lung transplant recipients who smoke than in nonsmoking heart or lung transplant recipients; prophylactic globulins used for induction therapy have also been associated with lung cancer in solid-organ transplant recipients.48,49,50
Pathogenesis
Malignancies after solid-organ transplantation can develop directly, through the transmission of neoplastic cells from the donor to the recipient, or through de novo occurrence in the recipient.28 Retrospective studies of organ transplant recipients have reported that the risk of a donor organ with undetected cancer being transplanted into a recipient is about 1.3%, the risk of development of de novo neoplasia is 0.2%, and the risk of cancer developing in recipients who receive a kidney from donor with known or incidentally discovered cancer is 45%.51,52
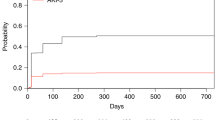
A number of factors seem to be associated with the development of de novo neoplasia in transplant recipients: impairment of immune surveillance through the use of immunosuppressive drugs after transplantation; carcinogenic factors such as sun exposure; and host factors such as a genetic predisposition to cancer, the presence of particular viral infections, and pretransplantation dialysis (Figure 1).28,53
Immunosuppressive therapy
The association of immunosuppressive therapy with an increased risk of cancer is well known; the incidence of cancer is higher in transplant recipients than in the general population or in patients in the waiting list.18
Intensity of immunosuppressive therapy
Some indirect evidence supports the idea that the intensity of immunosuppression after transplantation affects the risk of the development of a post-transplantation malignancy.53,54,55 Firstly, heart transplant recipients (who usually receive more intense immunosuppression than renal transplant recipients) have a higher risk of malignancy after transplantation than do renal transplant recipients.53 Secondly, the risk of PTLD is highest during the first year after transplantation, a time when the degree of immunosuppression is highest.10,56 Thirdly, a correlation has been found between increasing ciclosporin dose and the incidence of secondary cancers.57 Fourthly, a trial involving 231 patients randomized to receive ciclosporin doses adjusted to yield trough blood concentrations within the range 75–125 ng/ml (low-dose group) or trough blood concentrations within the range 150–225 ng/ml (normal-dose group) showed that low-dose ciclosporin was associated with a reduced incidence of cancer (19.8% versus 32.2%).57 The use of quadruple immunosuppressive therapy (ciclosporin A, azathioprine, prednisone and antilymphocyte globulin) has also been found to be associated with a higher incidence of non-Hodgkin lymphoma than the use of triple immunosuppressive therapy (ciclosporin A, azathioprine and prednisone).58 A correlation has also been found between CD4 lymphopenia and an increased incidence of skin cancer among kidney transplant recipients.59 Finally, the duration of immunosuppression has been shown to be associated with a gradual and cumulative increase in the risk of neoplasia in renal transplant recipients in the long term.33
Choice of drugs
The use of anti-T-cell therapy (muromonab-CD3 or antilymphocyte serum), but not anti-IL-2 receptor antibodies, has been shown predispose solid-organ transplant recipients to Epstein–Barr-virus-associated PTLD.56 Conflicting data surround the effect of other commonly used immunosuppressive drugs on the risk of PTLD.40 A paper published in 2007 reported that the use of thymoglobulin was associated with a significantly increased risk of PTLD (P = 0.0025), but that alemtuzumab, basiliximab or daclizumab were not associated with an increased risk of PTLD.60
Interestingly, the immunosuppressive effect may not be the only way in which immunosuppressant drugs confer an increased risk of malignancy. Both ciclosporin and tacrolimus have been shown to increase the levels of transforming growth factor β (TGF-β) in animal models, which might lead to the development of morphological changes in non-transformed cells and tumor growth in immunodeficient animal models.61,62 Azathioprine exposure has also been associated with an increased risk of skin cancer.63 Sirolimus, an inhibitor of the mammalian target of rapamycin (mTOR), is suggested to have anti-neoplastic effects. Laboratory and animal model experiments have shown that sirolimus is able to suppress tumor growth via the inhibition of p70 S6 kinase, IL-10, cyclins, and vascular endothelial growth factors A and C.64,65 Some clinical evidence also suggests that the incidence of post-transplantation malignancy is lower in patients receiving sirolimus than in patients receiving other immunosuppressive therapies.14,66,70 In addition, the use of sirolimus in place of ciclosporin has been associated with complete regression of Kaposi's sarcoma in renal transplant recipients.71,72 A large retrospective study that analyzed data from 33,249 deceased-donor primary solitary renal transplant recipients included in the Organ Procurement and Transplantation Network database found that the use of sirolimus or everolimus was associated with a reduction in the risk of post-transplantation malignancy development (relative risk 0.39, 95% CI 0.24–0.64; P = 0.0002).73
Exposure to carcinogenic factors
Exposure to carcinogenic factors is one of the most important factors in the development of neoplastic disease after solid-organ transplantation. The most-studied issue in transplant recipients is the relationship that shows that sun exposure, both before and after transplantation, is associated with an increased risk of skin cancer.33,74,75
Host factors
The genetic background of the host is clearly a very important factor in the development of post-transplantation malignancy, and although outside the scope of this Review it is of utmost importance in the clinical setting.16 Chronic pretransplantation dialysis treatment might also lead to an increased risk of cancer (particularly in the kidney, urinary tract and endocrine organs).76 Another important host factor that is more specifically related to the issue of transplantation is the co-existence of viral infections. Several viruses have been shown to be associated with the development of different neoplastic disorders after transplantation.
Epstein–Barr virus
Epstein–Barr virus is a gamma herpesvirus that is distributed worldwide. Antibodies against Epstein–Barr virus are found in around 90–95% of the world's population.77 After the primary infection, which is usually subclinical, the Epstein–Barr virus remains dormant in the patient for life, most of the time without any symptoms. Epstein–Barr virus has, however, been linked to Hodgkin and non-Hodgkin lymphomas and to nasopharyngeal carcinomas.78
Most cases of PTLD are associated with Epstein–Barr virus infection. Epstein–Barr virus infection can lead to cell transformation that, in the setting of chronic immunosuppression, allows tumor growth.78 Latent membrane protein-1 (LMP-1) of the Epstein–Barr virus has a central role in the pathogenesis of Epstein–Barr-virus-associated PTLD as it engages the signaling proteins from the tumor-necrosis-factor-receptor-associated factors (TRAFs) that lead to cell growth and transformation.79,80,81,82
As previously mentioned, some immunosuppressive regimens do seem to be associated with an increased risk of PTLD, although controversy still exists in this area. The use of muromonab-CD3 or antithymocyte globulin seems to be associated with an increased risk of PTLD mainly during the first year after transplantation, whereas the use of mycophenolate mofetil seems to be associated with a reduced incidence and later onset of PTLD.56,83,84 Considering calcineurin inhibitors, the use of ciclosporin (with or without azathioprine or steroids) is not associated with an increased risk of malignancy in transplant recipients compared with azathioprine or steroids alone, whereas tacrolimus is commonly associated with an increased risk of malignancy compared with ciclosporin.38,56,83,84,85,86 Finally, mTOR inhibitors might protect against the development of PTLD through the inhibition of proliferation signals: everolimus and sirolimus have shown a capacity to inhibit growth of PTLD cell lines in in vivo and in vitro models, respectively.73,74,75 Although some case reports suggest that conversion to mTOR-based immunosuppressive regimens might be useful in the treatment of PTLD,38,87,99 robust data are still lacking.
Human herpesvirus 8
Human herpesvirus 8 is a gamma herpesvirus that has an important role in cellular proliferation and the development of malignancies. Kaposi's sarcoma is the most common neoplastic disorder associated with human herpesvirus 8, but other diseases, including primary effusion lymphoma and Castleman disease, have also been associated with human herpesvirus 8 infection.90,91
Human herpesvirus 8 can infect a number of different cells types including B cells, endothelial cells, macrophages, and epithelial cells.90 Similar to other herpesviruses, human herpesvirus 8 shows a latent and lytic phase, and the transition from the latent to the lytic phase can be triggered by some cytokines and growth factors.92 During the lytic phase, the virus produces structural and replicative gene products that lead to the production of virions.91,92,93,94 Human herpesvirus 8 can also modulate the host immune response through a number of mechanisms including directing inflammatory cell recruitment away from a T-helper-1-type towards a T-helper-2-type response (which enables evasion from the cytotoxic immune response) and through impairment of antigen presentation and impairment of T-cell activation.95,96,97,98,99,100 The virus can also lead to carcinogenesis by preventing apoptosis.101,102 The presence of several oncogenes in the human herpesvirus 8 genome explains the capacity of the virus to induce tumors: the oncogenes can interfere with cell-cycle regulation and the control of apoptosis.101,102,103,104,105
A study performed in Saudi Arabia found that the proportion of patients with antibodies against human herpesvirus 8 was higher among patients who developed Kaposi's sarcoma after renal transplantation than among those who did not.106 In addition, the incidence of Kaposi's sarcoma is higher among patients with evidence of human herpesvirus 8 infection at the time of transplantation than among patients without infection (15–28% versus <1%).107,108,109 Considering these findings, screening for human herpesvirus 8 during the pretransplantation work-up might be useful. As previously mentioned, however, seropositivity for human herpesvirus 8 is not always associated with an increased risk of developing Kaposi's sarcoma.39 As both human herpesvirus 8 and any tumor cells derived from the donor can be transmitted from the donor to the recipient,110,111 it may be useful to screen donors for human herpesvirus 8, at least in regions with a high prevalence of infection. The importance of the T-cell response is underscored in the setting of post-transplantation Kaposi's sarcoma: complete remission of disease can be achieved by tapering of immunosuppression or switching from calcineurin inhibitors to sirolimus, which can lead to restoration of specific human herpesvirus 8 T-cell responses.112
Prevention and treatment
Immunosuppressive treatment may enable faster growth of pre-existing tumors in kidney transplant recipients.26 The screening of patients on the waiting list for cancer might therefore be useful. As chronic dialysis treatment might also be associated with an increased risk of cancer (particularly in the kidney, urinary tract and endocrine organs),76 some authors advocate that patients on the waiting list who are on long-term dialysis should undergo pretransplantation ultrasound screening for renal cancer. This technique detected adenocarcinoma in 3.8% of 208 patients evaluated for renal transplantation, with a positive predictive value of 100%.113
Performing transplantation in patients who have active cancer should be avoided. Although the appropriate time to wait between the achievement of cancer remission and transplantation is not clear, waiting for 2–5 years to pass without recurrence seems appropriate in patients with a history of cancer.114,115,116,117 Such a waiting period is not required in patients with a history of basal cell carcinoma of the skin, in situ bladder cancer, or a noninvasive papillary tumor of the bladder. Clinicians determining the appropriate timepoint for performing transplantation after cancer remission must, however, consider a patient's risk and cancer type on a case-by-case basis.
The prevention and management of cancer in renal transplant recipients should focus on four key areas: the pretransplantation screening of recipients and donors for cancer; the post-transplantation screening of recipients for cancer; the administration of specific drug treatments for the particular type of neoplasia; and the modulation of immunosuppressive treatment to try and balance the risks of graft rejection and cancer development.
Post-transplantation screening
Systematic screening of transplant recipients for cancer after transplantation should be performed in all transplant units to enable early intervention where necessary.118 A set of recommendations regarding post-transplantation monitoring for cancer detection has recently been published by the Kidney Disease: Improving Global Outcomes (KDIGO) Group.119 For skin and lip cancer, recommendations include the following: patients should be educated about their increased risk of such cancers (especially if they have fair skin, have experienced high levels of sun exposure or have a prior history of skin cancer); patients should reduce their levels of sun exposure; patients should perform self-examinations and annual skin and lip examinations should be performed by qualified health professionals; and oral acitretin should be given to individuals with a prior history of skin cancer to prevent the development of new cancers.119 Recent studies recommend the introduction of patient education programs, particularly in countries with a high incidence of non-melanoma skin cancer owing to high rates of occupational sun exposure.120,121
For non-skin cancers, the recommendations of the KDIGO group are weaker and just reinforce the importance of cancer screening as per the recommendations in the general population (that is, cervical and breast cancer screening for women, prostate cancer screening for men and colon cancer screening for both men and women) and annual hepatic ultrasound and monitoring of α-fetoprotein levels in patients with compensated cirrhosis.119
Specific treatments
Although the discussion of specific treatments for the different neoplasms is outside the scope of this Review, we will briefly discuss the role of rituximab in the treatment of PTLD. Rituximab is a chimeric monoclonal antibody against the B-cell-specific CD20 antigen found in B-cell lymphomas including PTLD.122 Rituximab has been successfully used to treat PTLD following both solid-organ and hematopoietic-stem-cell transplantation.123,124,125,126 As the development of PTLD is closely associated with Epstein–Barr virus infection, monitoring for Epstein–Barr virus replication using real-time polymerase chain reaction in transplant recipients may facilitate the early detection of patients at high risk of PTLD and perhaps enable early intervention.127 Rituximab may also offer some protection against graft rejection when used as an immunosuppressive drug in the setting of solid-organ transplantation.128,129
Modulation of immunosuppression
As described, immunosuppressive drug therapy has been identified as a factor that is associated with the increased incidence of malignancies in renal transplant recipients.26 Moreover, epidemiological data suggest that both the intensity and the extent of exposure to immunosuppressive therapy affect the incidence of post-transplantation malignancies and patient outcome.26 In addition, a pivotal clinical trial showed that use of the new immunosuppressive drug belatacept in renal transplant recipients was associated with better renal function, similar patient and graft survival, and an improved cardiovascular risk profile over ciclosporin, but was associated with an increased incidence of PTLD.130
Some evidence suggests that mTOR inhibitors have some anti-tumor activity.73 These drugs might, therefore, be useful in the future in patients who develop cancer after transplantation.
Summary of recommendations
The approach to dealing with malignancies in the setting of solid-organ transplantation should start with preventive measures, such as the avoidance of excessive immunosuppression, the avoidance of repeated exposure to depleting anti-lymphocyte antibodies, the screening of donors and recipients for cancer, and the avoidance of carcinogenic factors such as high sun exposure.
Once detected, a malignancy should be managed with the specific therapies for the particular tumor type and with strategies such as immunosuppression reduction, immunosuppression withdrawal or conversion to alternative immunosuppressive regimens based on mTOR inhibition. In patients diagnosed with lymphoma, skin cancer or Kaposi's sarcoma, reducing the doses of calcineurin inhibitors is a good first approach to treatment.131
In renal transplant recipients with Kaposi's sarcoma, the substitution of calcineurin inhibitors for mTOR inhibitors (along with the reduction or discontinuation of the immunosuppressive regimen) can lead to complete regression of disease, particularly in patients with early, small, and low-grade lesions.71,132,133
Regression of PTLD has been described in renal transplant recipients who switched from calcineurin inhibitors to mTOR inhibitors, which suggests a potential role for this immunosuppressive drug in the management of PTLD.41 Some anecdotal reports have documented regression of other solid-organ post-transplantation malignancies (including colon, lung, breast, stomach, and larynx cancer) after conversion to mTOR inhibitors, but such reports lack follow-up data.134
If a transplant recipient receiving treatment with azathioprine develops recurrent skin cancer, the discontinuation of azathioprine and conversion to mTOR inhibitors should be considered.29 Two prospective trials in Europe and Australia are studying the potential benefits of conversion from calcineurin inhibitors to mTOR inhibitors on the recurrence of skin cancer in transplant recipients.
Although growing evidence seems to indicate that mTOR inhibitors have beneficial effects in terms of cancer regression and patient survival in the early stages of post-transplantation malignancies,135 long-term prospective clinical trials are needed.
Conclusions
Malignancy is a common cause of death after renal transplantation. Clear associations have been found linking many of the immunosuppressive drugs in current use with cancer after transplantation. Research in this field is mainly focused on the development of strategies that aim to prevent or treat tumor development. In this regard, screening patients for cancer while they are on the transplantation waiting list and after they have undergone transplantation is very important. Minimizing doses of immunosuppressive drugs that are potential risk factors for cancer development is also an important prevention strategy in transplant recipients, and interest is growing in the potential antioncogenic properties and inherent immunosuppressive characteristics of mTOR inhibitors.
Review criteria
The PubMed database was searched using different combinations of the terms “kidney allograft”, “kidney transplantation”, “immunosuppression”, “malignancy”, “Epstein–Barr virus”, “post-transplant lymphoproliferative disorder”, “lymphoma”, “human herpesvirus 8”, “Kaposi's sarcoma”, “skin cancer”, “melanoma” and “rituximab”. The search was limited to papers published in the English language and focused particularly on papers published during the past 10 years.
References
Schnuelle, P., Lorenz, D., Trede, M. & Van Der Woude, F. J. Impact of renal cadaveric transplantation on survival in end-stage renal failure: evidence for reduced mortality risk compared with hemodialysis during long-term follow-up. J. Am. Soc. Nephrol. 9, 2135–2141 (1998).
Port, F. K., Wolfe, R. A., Mauger, E. A., Berling, D. P. & Jiang, K. Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. JAMA 270, 1339–1343 (1993).
Wolfe, R. A. et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N. Engl. J. Med. 341, 1725–1730 (1999).
Meier-Kriesche, H. U. et al. Survival improvement among patients with end-stage renal disease: trends over time for transplant recipients and wait-listed patients. J. Am. Soc. Nephrol. 12, 1293–1296 (2001).
Oniscu, G. C., Brown, H. & Forsythe, J. L. Impact of cadaveric renal transplantation on survival in patients listed for transplantation. J. Am. Soc. Nephrol. 16, 1859–1865 (2005).
Ojo, A. O. et al. Comparative mortality risks of chronic dialysis and cadaveric transplantation in black end-stage renal disease patients. Am. J. Kidney Dis. 24, 59–64 (1994).
Gill, J. S. et al. The impact of waiting time and comorbid conditions on the survival benefit of kidney transplantation. Kidney Int. 68, 2345–2351 (2005).
O'Grady, J. G., Burroughs, A., Hardy, P., Elbourne, D. & Truesdale, A. Tacrolimus versus microemulsified ciclosporin in liver transplantation: the TMC randomized controlled trial. Lancet 360, 1119–1125 (2002).
Knight, S. R. et al. Mycophenolate mofetil decreases acute rejection and may improve graft survival in renal transplant recipients when compared with azathioprine: a systematic review. Transplantation 87, 785–794 (2009).
Opelz, G. & Henderson, R. Incidence of non-Hodgkin lymphoma in kidney and heart transplant recipients. Lancet 342, 1514–1516 (1993).
Howard, R. J. et al. The changing causes of graft loss and death after kidney transplantation. Transplantation 73, 1923–1928 (2002).
Collins, A. J. et al. Excerpts from the United States Renal Data System 2003 Annual Data Report: atlas of end-stage renal disease in the United States. Am. J. Kidney Dis. 42 (Suppl. 5), S1–S230 (2003).
Briggs, J. D. Causes of death after renal transplantation. Nephrol. Dial. Transplant. 16, 1545–1549 (2001).
Wimmer, C. D. et al. The janus face of immunosuppression—de novo malignancy after renal transplantation: the experience of the Transplantation Center Munich. Kidney Int. 71, 1271–1278 (2007).
Penn, I. Malignant melanoma in organ allograft recipients. Transplantation 61, 274–278 (1996).
Birkeland, S. A., Lokkegaard, H. & Storm, H. H. Cancer risk in patients on dialysis and after renal transplantation. Lancet 355, 1886–1887 (2000).
Adami, J. et al. Cancer risk following organ transplantation: a nationwide cohort study in Sweden. Br. J. Cancer 89, 1221–1227 (2003).
Kasiske, B. L., Snyder, J. J., Gilbertson, D. T. & Wang, C. Cancer after kidney transplantation in the United States. Am. J. Transplant. 4, 905–913 (2004).
Grulich, A. E., van Leeuwen, M. T., Falster, M. O. & Vajdic, C. M. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 370, 59–67 (2007).
Visonneau, S., Cesano, A., Torosian, M. H., Miller, E. J. & Santoli, D. Growth characteristics and metastatic properties of human breast cancer xenografts in immunodeficient mice. Am. J. Pathol. 152, 1299–1311 (1998).
Stewart, T., Tsai, S. C., Grayson, H., Henderson, R. & Opelz, G. Incidence of de-novo breast cancer in women chronically immunosuppressed after organ transplantation. Lancet 346, 796–798 (1995).
Mihalov, M. L., Gattuso. P., Abraham, K., Holmes, E. W. & Reddy, V. Incidence of post-transplant malignancy among 674 solid-organ-transplant recipients at a single center. Clin. Transplant. 10, 248–255 (1996).
Jensen, P. et al. Skin cancer in kidney and heart transplant recipients and different long-term immunosuppressive therapy regimens. J. Am. Acad. Dermatol. 40, 177–186 (1999).
Fortina, A. B. et al. Skin cancer in heart transplant recipients: frequency and risk factor analysis. J. Heart Lung Transplant. 19, 249–255 (2000).
Penn, I. Incidence and treatment of neoplasia after transplantation. J. Heart Lung Transplant. 12, S328–S336 (1993).
Kiberd, B. A., Rose, C. & Gill, J. S. Cancer mortality in kidney transplant recipients. Am. J. Transplant. 9, 1868–1875 (2009).
Pedotti, P., Cardillo, M., Rossini, G. & Arcuri, V. Incidence of cancer after kidney transplant: results from the North Italy transplant program. Transplantation 76, 1448–1451 (2003).
Miao, Y. et al. De novo cancers arising in organ transplant recipients are associated with adverse outcomes compared with the general population. Transplantation 87, 1347–1359 (2009).
de Fijter, J. W. Use of proliferation signal inhibitors in non-melanoma skin cancer following renal transplantation. Nephrol. Dial. Transplant. 22 (Suppl. 1), i23–i26 (2007).
Webb, M. C., Compton, F., Andrews, P. A. & Koffman, C. G. Skin tumours posttransplantation: a retrospective analysis of 28 years' experience at a single centre. Transplant. Proc. 29, 828–830 (1997).
Euvrard, S. et al. Comparative epidemiologic study of premalignant and malignant epithelial cutaneous lesions developing after kidney and heart transplantation. J. Am. Acad. Dermatol. 33, 222–229 (1995).
Christenson, L. J. et al. Incidence of basal cell and squamous cell carcinomas in a population younger than 40 years. JAMA 294, 681–690 (2005).
Urwin, H. R. et al. Predicting risk of nonmelanoma skin cancer and premalignant skin lesions in renal transplant recipients. Transplantation 87, 1667–1671 (2009).
Vajdic, C. M. et al. Cutaneous melanoma is related to immune suppression in kidney transplant recipients. Cancer Epidemiol. Biomarkers Prev. 18, 2297–2303 (2009).
Dapprich, D. C. et al. Outcomes of melanoma in recipients of solid organ transplant. J. Am. Acad. Dermatol. 59, 405–417 (2008).
Matin, R. N. et al. Melanoma in organ transplant recipients: clinicopathological features and outcome in 100 cases. Am. J. Transplant. 8, 1891–1900 (2008).
Campistol, J. M. & Schena, F. P. Kaposi's sarcoma in renal transplant recipients—the impact of proliferation signal inhibitors. Nephrol. Dial. Transplant. 22 (Suppl. 1), i17–i22 (2007).
Moosa, M. R. Racial and ethnic variations in incidence and pattern of malignancies after kidney transplantation. Medicine 84, 12–22 (2005).
Francès, C. et al. The impact of preexisting or acquired Kaposi sarcoma herpesvirus infection in kidney transplant recipients on morbidity and survival. Am. J. Transplant. 9, 2580–2586 (2009).
Pascual, J. Post-transplant lymphoproliferative disorder—the potential of proliferation signal inhibitors. Nephrol. Dial. Transplant. 22 (Suppl. 1), i27–i35 (2007).
Caillard, S., Agodoa, L. Y., Bohen, E. M. & Abbott, K. C. Myeloma, Hodgkin disease, and lymphoid leukemia after renal transplantation: characteristics, risk factors and prognosis. Transplantation 81, 888–895 (2006).
Koukourgianni, F. et al. Malignancy incidence after renal transplantation in children: a 20-year single centre experience. Nephrol. Dial. Transplant. 25, 611–616 (2010).
Berg, D. & Otley, C. C. Skin cancer in organ transplant recipients: epidemiology, pathogenesis, and management. Am. Acad. Dermatol. 47, 1–17 (2002).
Penn, I. & First, M. R. Merkel's cell carcinoma in organ recipients: report of 41 cases. Transplantation 68, 1717–1721 (1999).
Vajdic, C. M. et al. Increased incidence of squamous cell carcinoma of eye after kidney transplantation. J. Natl Cancer Inst. 99, 1340–1342 (2007).
Penn, I. Cancers complicating organ transplantation. N. Engl. J. Med. 323, 1767–1769 (1990).
Penn, I. Cancers of the anogenital region in renal transplant recipients. Analysis of 65 cases. Cancer 58, 611–616 (1986).
Anyanwu, A. C. et al. Primary lung carcinoma after heart or lung transplantation: management and outcome. J. Thorac. Cardiovasc. Surg. 124, 1190–1197 (2002).
Rinaldi, M. et al. Neoplastic disease after heart transplantation: single center experience. Eur. J. Cardiothorac. Surg. 19, 696–701 (2001).
Goldstein, D. J. et al. Carcinoma of the lung after heart transplantation. Transplantation 62, 772–775 (1996).
Buell, J. F. et al. Donor transmitted malignancies. Ann. Transplant. 9, 53–56 (2004).
Kauffman, H. M., McBride, M. A. & Delmonico, F. L. First report of the United Network for Organ Sharing Transplant Tumor Registry: Donors with a history of cancer. Transplantation 70, 1747–1751 (2000).
Morath, C. et al. Malignancy in renal transplantation. J. Am. Soc. Nephrol. 15, 1582–1588 (2004).
Ramsay, H. M., Fryer, A. A., Reece, S., Smith, A. G. & Harden, P. N. Clinical risk factors associated with nonmelanoma skin cancer in renal transplant recipients. Am. J. Kidney Dis. 36, 167–176 (2000).
Fortina, A. B. et al. Immunosuppressive level and other risk factors for basal cell carcinoma and squamous cell carcinoma in heart transplant recipients. Arch. Dermatol. 140, 1079–1085 (2004).
Opelz, G. & Döhler, B. Lymphomas after solid organ transplantation: a collaborative transplant study report. Am. J. Transplant. 4, 222–230 (2004).
Dantal, J. et al. Effect of long-term immunosuppression in kidney-graft recipients on cancer incidence: randomized comparison of two cyclosporin regimens. Lancet 351, 623–628 (1998).
Melosky, B. et al. Lymphoproliferative disorders after renal transplantation in patients receiving triple or quadruple immunosuppression. J. Am. Soc. Nephrol. 212 (Suppl.), S290–S294 (1992).
Caforio, A. L. et al. Skin cancer in heart transplant recipients: risk factor analysis and relevance of immunosuppressive therapy. Circulation 102 (Suppl. 3), III222–III227 (2000).
Kirk, A. D. et al. Dissociation of depletional induction and posttransplant lymphoproliferative disease in kidney recipients treated with alemtuzumab. Am. J. Transplant. 7, 2619–2625 (2007).
Hojo, M. et al. Cyclosporine induces cancer progression by a cell-autonomous mechanism. Nature 397, 530–534 (1999).
Maluccio, M. et al. Tacrolimus enhances transforming growth factor-β1 expression and promotes tumor progression. Transplantation 76, 597–602 (2003).
Harwood, C. A. et al. PTCH mutations in basal cell carcinomas from azathioprine-treated organ transplant recipients. Br. J. Cancer 99, 1276–1284 (2008).
Guba, M. et al. Rapamycin inhibits primary and metastatic tumor growth by antiangiogenesis: involvement of vascular endothelial growth factor. Nat. Med. 8, 128–135 (2002).
Luan, F. L. et al. Rapamycin is an effective inhibitor of human renal cancer metastasis. Kidney Int. 63, 917–926 (2003).
Guba, M., Graeb, C., Jauch, K. W. & Geissler, E. K. Pro- and anti-cancer effects of immunosuppressive agents used in organ transplantation. Transplantation 77, 1777–1782 (2004).
Campistol, J. M. et al. Sirolimus therapy after early cyclosporine withdrawal reduces the risk for cancer in adult renal transplantation. J. Am. Soc. Nephrol. 1, 581–589 (2006).
Mathew, T., Kreis, H. & Friend, P. Two-year incidence of malignancy in sirolimus-treated renal transplant recipients: results from five multicenter studies. Clin. Transplant. 18, 446–449 (2004).
Euvrard, S., Ulrich, C. & Lefrancois, N. Immunosuppressants and skin cancer in transplant patients: focus on rapamycin. Dermatol. Surg. 30, 628–633 (2004).
Kahan, B. D. et al. Low incidence of malignancy among sirolimus/cyclosporine-treated renal transplant recipients. Transplantation 80, 749–758 (2005).
Campistol, J. M., Gutierrez-Dalmau, A. & Torregrosa, J. V. Conversion to sirolimus: a successful treatment for posttransplantation Kaposi's sarcoma. Transplantation 77, 760–762 (2004).
Stallone, G. et al. Sirolimus for Kaposi's sarcoma in renal-transplant recipients. N. Engl. J. Med. 352, 1317–1323 (2005).
Kauffman, H. M., Cherikh, W. S., Cheng, Y., Hanto, D. W. & Kahan, B. D. Maintenance immunosuppression with target-of-rapamycin inhibitors is associated with a reduced incidence of de novo malignancies. Transplantation 80, 883–889 (2005).
Ramsay, H. M. et al. Factors associated with nonmelanoma skin cancer following renal transplantation in Queensland, Australia. J. Am. Acad. Dermatol. 49, 397–406 (2003).
Dreno, B. Skin cancers after transplantation. Nephrol. Dial. Transplant. 8, 1052–1058 (2003).
Chu, P. G. et al. Epstein–Barr virus (EBV) nuclear antigen (EBNA)-4 mutation in EBV-associated malignancies in three different populations. Am. J. Pathol. 155, 941–947 (1999).
van Leeuwen, M. T. et al. Immunosuppression and other risk factors for early and late non-Hodgkin lymphoma after kidney transplantation. Blood 114, 630–637 (2009).
Liebowitz, D. Epstein–Barr virus and a cellular signaling pathway in lymphomas from immunosuppressed patients. N. Engl. J. Med. 338, 1413–1421 (1998).
Izumi, K. M., Kaye, K. M. & Kieff, E. D. The Epstein–Barr virus LMP1 amino acid sequence that engages tumor necrosis factor receptor associated factors is critical for primary B lymphocyte growth transformation. Proc. Natl Acad. Sci. USA 94, 1447–1452 (1997).
Song, Y. J., Izumi, K. M., Shinners, N. P., Gewurz, B. E. & Kieff, E. IRF7 activation by Epstein–Barr virus latent membrane protein 1 requires localization at activation sites and TRAF6, but not TRAF2 or TRAF3. Proc. Natl Acad. Sci. USA 105, 18448–18453 (2008).
Mosialos, G. Cytokine signaling and Epstein–Barr virus-mediated cell transformation. Cytokine Growth Factor Rev. 12, 259–270 (2001).
Caillard, S., Dharnidharka, V., Agodoa, L., Bohen, E. & Abbott, K. Posttransplant lymphoproliferative disorders after renal transplantation in the United States in era of modern immunosuppression. Transplantation 80, 1233–1243 (2005).
Robson, R., Cecka, J. M., Opelz, G., Budde, M. & Sacks, S. Prospective registry-based observational cohort study of the long-term risk of malignancies in renal transplant patients treated with mycophenolate mofetil. Am. J. Transplant. 5, 2954–2960 (2005).
Pirsch, J. D. Cytomegalovirus infection and posttransplant lymphoproliferative disease in renal transplant recipients: results of the U. S. multicenter FK506 Kidney Transplant Study Group. Transplantation 68, 1203–1205 (1999).
Birkeland, S. A. & Hamilton-Dutoit, S. Is posttransplant lymphoproliferative disorder (PTLD) caused by any specific immunosuppressive drug or by the transplantation per se? Transplantation 76, 984–988 (2003).
Majewski, M. et al. The immunosuppressive macrolide RAD inhibits growth of human Epstein–Barr virus-transformed B lymphocytes in vitro and in vivo: a potential approach to prevention and treatment of posttransplant lymphoproliferative disorders. Proc. Natl Acad. Sci. USA 97, 4285–4290 (2000).
Majewski, M. et al. Immunosuppressive TOR kinase inhibitor everolimus (RAD) suppresses growth of cells derived from posttransplant lymphoproliferative disorder at allograft-protecting doses. Transplantation 75, 1710–1717 (2003).
Nepomuceno, R. R. et al. Rapamycin inhibits the interleukin 10 signal transduction pathway and the growth of Epstein–Barr virus B-cell lymphomas. Cancer Res. 63, 4472–4480 (2003).
Akula, S. M., Pramod, N. P., Wang, F. Z. & Chandran, B. Integrin α3β1 (CD 49c/29) is a cellular receptor for Kaposi's sarcoma-associated herpesvirus (KSHV/HHV-8) entry into the target cells. Cell 108, 407–419 (2002).
Paulose-Murphy, M. et al. Transcription program of human herpesvirus 8 (Kaposi's sarcoma-associated herpesvirus). J. Virol. 75, 4843–4853 (2001).
Mercader, M. et al. Induction of HHV-8 lytic cycle replication by inflammatory cytokines produced by HIV-1-infected T cells. Am. J. Pathol. 156, 1961–1971 (2000).
Chang, J., Renne, R., Dittmer, D. & Ganem, D. Inflammatory cytokines and the reactivation of Kaposi's sarcoma-associated herpesvirus lytic replication. Virology 266, 17–25 (2000).
Davis, D. A. et al. Hypoxia induces lytic replication of Kaposi sarcoma-associated herpesvirus. Blood 97, 3244–3250 (2001).
Weber, K. S. et al. Selective recruitment of Th2-type cells and evasion from a cytotoxic immune response mediated by viral macrophage inhibitory protein-II. Eur. J. Immunol. 31, 2458–2466 (2001).
Lubyova, B. & Pitha, P. M. Characterization of a novel human herpesvirus 8-encoded protein, vIRF-3, that shows homology to viral and cellular interferon regulatory factors. J. Virol. 74, 8194–8201 (2000).
Brander, C. et al. Impaired CTL recognition of cells latently infected with Kaposi's sarcoma-associated herpes virus. J. Immunol. 165, 2077–2083 (2000).
Ishido, S., Wang, C., Lee, B. S., Cohen, G. B. & Jung, J. U. Downregulation of major histocompatibility complex class I molecules by Kaposi's sarcoma-associated herpesvirus K3 and K5 proteins. J. Virol. 74, 5300–5309 (2000).
Coscoy, L. & Ganem, D. A viral protein that selectively downregulates ICAM-1 and B7-2 and modulates T cell costimulation. J. Clin. Invest. 107, 1599–1606 (2001).
Bertin, J. et al. Death effector domain-containing herpesvirus and poxvirus proteins inhibit both Fas- and TNFR1-induced apoptosis. Proc. Natl Acad. Sci. USA 94, 1172–1176 (1997).
Lundquist, A. et al. Kaposi sarcoma-associated viral cyclin K overrides cell growth inhibition mediated by oncostatin M through STAT3 inhibition. Blood 101, 4070–4077 (2003).
Flore, O. et al. Transformation of primary human endothelial cells by Kaposi's sarcoma-associated herpesvirus. Nature 394, 588–592 (1998).
Pati, S. et al. Activation of NF-κB by the human herpesvirus 8 chemokine receptor ORF74: evidence for a paracrine model of Kaposi's sarcoma pathogenesis. J. Virol. 75, 8660–8673 (2001).
Bais, C. et al. G-protein coupled receptor of Kaposi's sarcoma-associated herpesvirus is a viral oncogene and angiogenesis activator. Nature 391, 86–89 (1998).
Wang, H. W. et al. Kaposi sarcoma herpesvirus-induced cellular reprogramming contributes to the lymphatic endothelial gene expression in Kaposi sarcoma. Nat. Genet. 36, 687–693 (2004).
Qunibi, W. et al. Serologic association of human herpesvirus eight with posttransplant Kaposi's sarcoma in Saudi Arabia. Transplantation 65, 583–585 (1998).
Frances, C. et al. Outcome of kidney transplant recipients with previous human herpesvirus-8 infection. Transplantation 69, 1776–1779 (2000).
Diociaiuti, A. et al. HHV8 in renal transplant recipients. Transpl. Int. 13 (Suppl. 1), S410–S412 (2000).
Cattani, P. et al. Kaposi's sarcoma associated with previous human herpesvirus 8 infection in kidney transplant recipients. J. Clin. Microbiol. 39, 506–508 (2001).
Regamey, N. et al. Transmission of human herpesvirus 8 infection from renal-transplant donors to recipients. N. Engl. J. Med. 339, 1358–1363 (1998).
Barozzi, P. et al. Post-transplant Kaposi sarcoma originates from the seeding of donor-derived progenitors. Nat. Med. 9, 554–561 (2003).
Barozzi, P. et al. Changes in the immune responses against human herpesvirus-8 in the disease course of posttransplant Kaposi sarcoma. Transplantation 86, 738–744 (2008).
Maisonneuve, P. et al. Cancer in patients on dialysis for end-stage renal disease: an international collaborative study. Lancet 354, 93–99 (1999).
Gulanikar, A. C., Daily, P. P., Kilambi, N. K., Hamrick-Turner, J. E. & Butkus, D. E. Prospective pretransplant ultrasound screening in 206 patients for acquired renal cysts and renal cell carcinoma. Transplantation 66, 1669–1672 (1998).
Kasiske, B. L. et al. The evaluation of renal transplant candidates: clinical practice guidelines. Am. J. Transplant. 1 (Suppl. 2), 3–95 (2001).
Kasiske, B. L. et al. The evaluation of renal transplant candidates: clinical practice guidelines. J. Am. Soc. Nephrol. 6, 1–34 (1995).
Knoll, G. et al. Canadian Society of Transplantation consensus guidelines on eligibility for kidney transplantation. CMAJ 173, S1–S25 (2005).
Penn, I. The effect of immunosuppression on pre-existing cancers. Transplantation 55, 742–747 (1993).
Ajithkumar, T. V., Parkinson, C. A., Butler, A. & Hatcher, H. M. Management of solid tumours in organ-transplant recipients. Lancet Oncol. 8, 921–932 (2007).
Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group. KDIGO clinical practice guideline for the care of kidney transplant recipients. Am. J. Transplant. (Suppl. 3), S1–S155 (2009).
Fuente, M. J. et al. A prospective study of the incidence of skin cancer and its risk factors in a Spanish Mediterranean population of kidney transplant recipients. Br. J. Dermatol. 149, 1221–1226 (2003).
Webster, A. C., Wong, G., Craig, J. C. & Chapman, J. R. Managing cancer risk and decision making after kidney transplantation. Am. J. Transplant. 8, 2185–2191 (2008).
Scott, S. D. Rituximab: a new therapeutic monoclonal antibody for non-Hodgkin's lymphoma. Cancer Pract. 6, 195–197 (2001).
Verschuuren, E. A. et al. Treatment of posttransplant lymphoproliferative disease with rituximab: the remission, the relapse, and the complication. Transplantation 73, 100–104 (2002).
Blaes, A. H., Peterson, B. A., Bartlett, N., Dunn, D. L. & Morrison, V. A. Rituximab therapy is effective for posttransplant lymphoproliferative disorders after solid organ transplantation. Cancer 104, 1661–1667 (2005).
Choquet, S. et al. Efficacy and safety of rituximab in B-cell post-transplantation lymphoproliferative disorders: results of a prospective multicenter phase 2 study. Blood 107, 3053–3057 (2006).
EBPG Expert Group on Renal Transplantation. European best practice guidelines for renal transplantation. Section IV: Long-term management of the transplant recipient. IV.6.1. Cancer risk after renal transplantation. Post-transplant lymphoproliferative disease (PTLD): prevention and treatment. Nephrol. Dial. Transplant. 17 (Suppl. 4), 31–33 (2002).
Sato, T. et al. Monitoring of Epstein–Barr virus load and antibody in pediatric renal transplant patients. Pediatr. Int. 50, 454–458 (2008).
Vo, A. A. et al. Use of intravenous immune globulin and rituximab for desensitization of highly HLA-sensitized patients awaiting kidney transplantation. Transplantation 89, 1095–1102 (2010).
van den Hoogen, M. W. & Hilbrands, L. B. More on B-cell-depleting induction therapy and acute cellular rejection. N. Engl. J. Med. 361, 1215 (2009).
Durrbach, A. et al. A phase III study of belatacept versus cyclosporine in kidney transplants from extended criteria donors (BENEFIT-EXT study). Am. J. Transplant. 10, 547–557 (2010).
Duman, S. et al. Successful treatment of post-transplant Kaposi's sarcoma by reduction of immunosuppression. Nephrol. Dial. Transplant. 17, 892–896 (2002).
Campistol, J. M. Minimizing the risk of posttransplant malignancy. Transplantation 87 (Suppl.), S19–S22 (2009).
Mohsin, N. et al. Complete regression of visceral Kaposi's sarcoma after conversion to sirolimus. Exp. Clin. Transplant. 3, 366–369 (2005).
Monaco, A. P. The role of mTOR inhibitors in the management of posttransplant malignancy. Transplantation 87, 157–163 (2009).
Gomez-Camarero, J. et al. Use of everolimus as a rescue immunosuppressive therapy in liver transplant patients with neoplasms. Transplantation 84, 786–791 (2007).
Acknowledgements
Laurie Barclay, freelance writer and reviewer, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the MedscapeCME-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Contributions
I. Rama and J. M. Grinyó both contributed to researching data for article, discussing the content, writing the article, and reviewing and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Rama, I., Grinyó, J. Malignancy after renal transplantation: the role of immunosuppression. Nat Rev Nephrol 6, 511–519 (2010). https://doi.org/10.1038/nrneph.2010.102
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2010.102
This article is cited by
-
Ipsilateral synchronous papillary renal neoplasm with reverse polarity and urothelial carcinoma in a renal transplant recipient: a rare case report with molecular analysis and literature review
Diagnostic Pathology (2023)
-
IL-37 overexpression promotes endometrial regenerative cell-mediated inhibition of cardiac allograft rejection
Stem Cell Research & Therapy (2022)
-
Laryngeal Dysplasia: To Biopsy or Not?
Indian Journal of Otolaryngology and Head & Neck Surgery (2022)
-
The effect of subsequent immunosuppressant use in organ-transplanted patients on prostate cancer incidence: a retrospective analysis using the Korean National Health Insurance Database
BMC Urology (2021)
-
Long-term Survival After Nephron-Sparing Surgery for Kidney Allograft Tumors: Case Reports from a Single Transplant Center
SN Comprehensive Clinical Medicine (2021)