Abstract
Since the sixteenth century, competition between midwives and surgeons has created a culture of blame around the difficult delivery. In the late seventeenth century, 100 years before oxygen was discovered, researchers associated “apparent death of the newborn” with impaired respiratory function of the placenta. The diagnosis “birth asphyxia” replaced the term “apparent death of the newborn” during the mass phobia of being buried alive in the eighteenth century. This shifted the interpretation from unavoidable fate to a preventable condition. Although the semantic inaccuracy (“pulselessness”) was debated, “asphyxia” was not scientifically defined until 1992. From 1792 the diagnosis was based on a lack of oxygen. “Blue” and “white” asphyxia were perceived as different disorders in the eighteenth, and as different grades of the same disorder in the nineteenth century. In 1862, William Little linked birth asphyxia with cerebral palsy, and although never confirmed, his hypothesis was accepted by scientists and the public. Fetal well-being was assessed by auscultating heart beats since 1822, and continuous electronic fetal monitoring was introduced in the 1960s without scientific assessment. It neither diminished the incidence of birth asphyxia nor of cerebral palsy, but rather raised the rate of cesarean sections and litigation against obstetricians and midwives.
Similar content being viewed by others
Main
Birth asphyxia is neither the most dangerous nor most frequent life-threatening condition patients and doctors encounter, yet it is the most frequent cause of litigation (1, 2). Although not compatible with scientific evidence, birth asphyxia was and is frequently believed to be associated with cerebral palsy. It was hypothesized that lack of definition and interprofessional blaming contributed to the belief that birth asphyxia is preventable. By delineating the path from a non-entity to a condition suspected of resulting from malpractice, the present paper seeks to explain this phenomenon from a historical perspective. Its focus is the definition of birth asphyxia and the interprofessional controversy. It omits the history of neonatal resuscitation (3, 4, 5) and is short on historic aspects described before, such as obstetric forceps (6) and electronic fetal monitoring (7, 8). The use of the term “birth asphyxia” in the German literature was addressed by Stiller (9).
Obstetrics before the printing era
Hellas and Rome showed little sympathy for weaklings: malformed or premature infants were abandoned at the Taygettos canyon or the columna lactaria, respectively. The Greek goddesses Hera and Artemis and the Roman goddess Juno Lucina were believed to protect childbirth, and midwives enjoyed high esteem. A tombstone from Menidi, 4th century BCE, reads (10): “Phanostrate, a midwife and physician, lies here. She caused pain to none, and all lamented her death.”
Postnatal difficulties were believed to result from intrauterine conditions, and maintaining placental circulation was the main therapy. For poorly adapted neonates, the Corpus Hippocraticum (11) recommended in the 5th century BCE: “You should not remove their umbilical cord before they pass urine or sneeze or give voice, instead leaving it connected.... If the umbilical cord puffs up with air like a pouch, the child will move or sneeze and give voice; then you should remove the cord while the child is taking a breath. If, after a certain time, the umbilical cord does not puff up with air nor the child move, it will not survive. ” In the 4th century BCE, Aristotle (12) reported: “Often the baby seemed to be born dead when... the blood happens to run out into the umbilicus and the surrounding part; but certain midwives who have acquired this skill, squeezed the blood back inside, out of the umbilical [cord], and immediately the baby... has revived again.”
Roman midwives often began their career as slaves and were freed after a happy delivery. Soranus did not favor resuscitation in disturbed respiration in the 2nd century CE (13): “[the newborn is worth raising] who immediately cries with proper vigor; for one that lives for some length of time without crying, or cries but weakly, is suspected of behaving so on account of some unfavorable condition.” With the advent of Christianity, Greek and Roman ideas about human life changed. In 319 CE Roman Emperor Constantine decreed that the state provide maintenance and education for poor children and prevent the exposure, sale, and murder of infants (14). From Soranus (13) until Scipio Mercurio (15), the Middle Ages brought 1,400 years of stagnation in midwifery, the main reason being the “dead hand of Galen,” as Radcliffe characterized the medieval hostility towards research (16). Another reason was the century-long divorce of surgery from medicine that excluded barber-surgeons and midwives from academic training. Not until the printing press became available around 1,500 did obstetric knowledge dissipate and improve, despite the fact that most midwives and barber-surgeons were illiterate.
Interprofessional competition and blame
Interprofessional conflicts were common even before book printing weakened the privileges of learning. Rights and duties of midwives were regulated since the fourteenth century; a typical example is the Freiburg order of 1557 (17): “They shall not use any gruesome or clumsy instrument to break or extract the infant.” As late as 1786, Jean-François Icart listed four instruments that midwives were allowed to use and had been loaned by the diocese of Castres (18): (1) clyster-syringe for enemas; (2) catheter to empty the bladder; (3) small syringe for intrauterine baptism; (4) tube to ventilate the baby.
Barber-surgeons, all male, became active in obstetrics in the thirteenth century, their activities regulated by the guild. In London, the company of barber-surgeons was founded in 1540 (19), whereas midwives were legally regulated as late as 1902 (20). The surgeons’ arrival on the birth scene, however, heralded the death of mother or child, if not both: it was their privilege to use hooks (crochets), their duty to remove the dead fetus following prolonged or obstructed labor, oblique pelvis, or hydrocephalus, in an attempt to save the mother’s life (Figure 1). Not until the Chamberlen family’s secret—the obstetric forceps—leaked out around 1720, did that instrument become the key that opened the lying-in room for men (6). Benjamin Pugh, surgeon in Chelmsford, Essex, justified his treatise of midwifery “with regard to the operation” in 1754 (21): “as every young Surgeon now intends practicing Midwifery, and it is become almost as universal in this Kingdom, as ever it was in France. ” Male assistance first became fashionable in delivery rooms of the nobility: in 1670, Julien Clément delivered Madame Montespan, mistress of Louis XIV; in 1688, Hugh Chamberlen the wife of James II; in 1738, William Hunter attended the birth of George III, etc. Midwives and surgeons who published texts on obstetrics remained rare, as publishing was a strictly regulated privilege. Usually they were appointed to the royal courts, who gave them permission to publish without the need for consent by the medical faculties.
Instruments used by sixteenth and seventeenth century surgeons to dismember and extract dead fetuses. (a) Duck’s beak, depicted by Jacob Rueff, 1587 (92); (b–d) blunt and sharp hooks (crotchets) depicted by Jacques Dalechamps, 1573 (93) and Ambroise Paré, 1573 (26); (e) double hook with chains, depicted by Johannes Scultetus, 1666 (94); (f) infant head, with extractor (tire-tête) applied to the sagittal suture; (g) extractor (tire-tête), and (h) fontanel-lancet depicted by François Mauriceau, 1668 (36).
The respect for midwives waned immediately and bitter competition arose when men entered “real” obstetrics in which both mother and child were expected to survive. Named accoucheurs or man-midwife, they used their publications to blame the midwives for everything that could go wrong during a delivery. Eucharius Rösslin’s book first appeared in 1513, was frequently reprinted, and translated into English by Thomas Raynald in 1540 (22): The bellicose introductory poem stated:
“I mean the midwives each and all,
who know so little of their call,
that through neglect and oversight,
they destroy children far and wide."
In Paris, a statute of 1560 regulated supervision of the five matrones jurées (sworn matrons) by the Royal Barber Surgeon (23). In 1620, Royal accoucheur Charles Guillemeau in Paris criticized impatient midwives (24), “who with their fingernails break the membranes, have caused the death of many women and numberless infants” and in 1627 branded Royal midwife Louise Bourgeois as “presumptuous, ignorant, and brutal” (25). Ambroise Paré, surgeon at the Hôtel-Dieu—which served as school of midwifery—stated condescendingly in 1573 (26): “Midwives are to be admonished that as often as they perceiv the childe to be comming forth either with its bellie or his back forwards... that they should turn it, and draw it out by the feet; for the doing whereof, if they be not sufficient, let them crave the assistance and help of some expert Chirurgian.”
In 1672, Percival Willughby of Derby moaned (27): “midwives will follow their own wayes, and will have their own wills.” Constantly attacked by surgeons, the midwives retaliated, usually by claiming overuse of and complications using the forceps, and avarice of the accoucheur, who received higher wages than the midwife. In Prussia, the book of Royal Midwife Justine Siegmundin, first published in 1690, set the German standard for a century (28). She defined weakness as a form of suffocation, due to delayed onset of breathing. Andreas Petermann, professor of surgery at Leipzig University, attacked the book as “speculation-based, illogical, and dangerous for midwives and parturients” and tried to have the censor forbid it, without success. The 5-year controversy is reproduced in later editions of Siegemundin’s book. In England, Elizabeth Nihell attacked William Smellie in 1760 (29): “Pernicious quackery of those instruments [Smellie’s forceps, Figure 3b] has been artfully made the pretext of an innovation set on foot by Interest, adopted by Credulity, and fostered by Fashion.” The frontispiece of Samuel Fores’ book of 1793 (Figure 2) gives us an idea of the pamphlet wars between the two health professions (30). There are many other examples. The persistent controversy was described by Hagen in 1791 (31) and Donnison in 1977 (20). After two centuries of blaming, the stage was set for the courts. Midwives’ textbooks meticulously regulated every detail, as Hauck explained in 1815 (32): “to prove punishable offences.” A century later, Ahlfeld stated similar purposes in 1905 (33): “The official textbook of midwifery also serves as a guide for disciplinary avengement and desicions in foro (court trial)." The German textbook on forensic medicine resumed in 1872 (34): “Most frequently sued for alleged malpractice are obstetricians and midwives.” The surgeons had won a pyrrhic victory that maintained the hierarchy, but undermined the respect for both professions.
Example of a pamphlet deriding male obstetricians. Frontispiece of Samuel Fores: Man-midwifery dissected, 1793 (30): the instruments (lever, forceps, boring scissors, blunt hook) allude to the man-midwife’s cruelty, the aphrodisiacs on the shelf to his lechery (Wellcome Library L 0079917).
“Apparent death” classified by alleged causes
Apparent death [mors apparens] of the neonate was addressed in early printed books on obstetrics. In 1472, Padovan professor Paolo Bagellardo described birth asphyxia quite precisely (35): “[The midwife should examine] whether the infant is alive or not, or spotted, that is: whether black or white or of livid color, and whether it is breathing or not. If she finds it warm, not black, she should blow into its mouth, if it has no respiration, or into its anus.” Had he omitted the last words, we would praise Bagellardo as pioneer of neonatology. Whereas birth asphyxia was not differentiated from immaturity or weakness in the preterm infant, inability to breathe was regarded a treatable condition in the term infant. A century before the discovery of oxygen, several researchers were aware of normal and disturbed fetal gas exchange: Parisian accoucheur François Mauriceau described a prolapsed umbilical cord in 1668 (36): “Lacking placental respiration, the fetus now should inspire by the mouth, to refresh its heart... secluded in the womb, however, this path is not available, and the infant must soon die from suffocation, because both ways [placenta and lungs] are unavailable.” Mauriceau reported that more than half young infants died, and discerned several accidents leading to apparent death: (1) weakness in prematures; (2) violence due to difficult labour; (3) sudden suffocation.
Physiologist John Mayow of Oxford wrote in 1674 (37): “The foetus in the uterus, whose blood does not pass through the lungs but through special ducts, does not need to breathe at all.... With respect, then, to the use of respiration, it may be affirmed that an aerial something [sal-nitro] essential to life, whatever it may be, passes [from the placenta] into the mass of the blood.”
Philipp Verheyen, anatomist in Louvain, was aware of the placenta’s respiratory function in 1693 (38): “In the fetus, whose lungs repose, this substance, which feeds the flame of life, is extracted by the placenta from the maternal blood, and admixed with the fetal blood (Figure 3).” Seven years after Lavoisier named oxygen, Swiss scientist Christoph Girtanner associated its deficiency with fetal asphyxia in 1792 (39): “The fetal lung is outside the body: It is the placenta.... The infant dies suddenly, when during birth the cord is compressed, and the circulation to and from the placenta is interrupted.” In 1819, Alexandre Lebreton published a book on neonatal diseases in which he classified apparent death according to six causes (40): (1) brain compression; (2) venous brain congestion; (3) spinal cord trauma; (4) anemia or emptiness of blood vessels; (5) weakness; (6) syncope, which meant overload with blood. From 1840 to 1874, several French obstetricians proposed returning to the term “apparent death” rather than the ill-defined terms syncope, apoplexy, weakness, suffocation, etc. (41).
Asphyxia was related to respiratory placental insufficiency at the end of the seventeenth century. (a) Chamberlen forceps type 2, around 1650 (6); (b) prolonged birth (longish head and vertex tumor) with William Smellie’s curved forceps, depicted in 1754 (95); (c) and (d) asphyctic infant at autopsy and fetal side of placenta, depicted by Philipp Verheyen, 1693 (38); (e) maternal side of the same placenta.
In Prussia, Christoph Hufeland used the term asphyxia in 1836 (42) for “a perfect image of death... cessation of circulation and respiration, and motion. It is often a continuance of the fetal state (hydatic life), a failure to commence atmospherical, independent existence....” He assumed three specific causes according to the infant’s appearance: (1) true weakness due to immaturity; (2) overload of blood in brain and heart due to prolonged labor or cord entanglement; (3) suffocation due to mucus obstruction.
Vitalism, burying alive, and the diagnosis “asphyxia”
During the eighteenth century, philosophical theories still exerted great influence in medicine. “Apparent death” was related to “viability” or “life force”—philosophical terms that originated with vitalism. To discern living and dead matter, Georg Ernst Stahl postulated an energia operandi (energy of action) in 1733. Albrecht von Haller defined life as the irritability of tissues, especially nerves and muscles in 1752. Johann Wolfgang Goethe, a vitalist himself, combined this concept by again blaming the midwife, when describing his own birth on 28 August 1749 (43): “The midwife was so unskilled that I was brought into the world as good as dead, and only with great difficulty could I be made to open my eyes and see the light... my grandfather, Johann Textor, who was chief magistrate, was moved by this to appoint an official birth-assistant and to reintroduce the instruction of midwives.”
The mass phobia of apparent death began with the books of Lancisi 1707 (44), Winslow, and Bruhier 1742 (45); These books went through many editions and translations, and accompanied the Europe-wide obsession of “being buried alive.” Humane Societies were founded to teach resuscitation (46) and pamphlets were distributed by Royal order to the public at governmental expense, as that of de Gardane 1774 in France (47) and 1781 in Prussia (48); and it was those very pamphlets that introduced incorrectly the term asphyxia [pulselessness] into medical texts as in John Aitken’s book on midwifery that appeared in 1784 in Edinburgh (49) and 1789 in Nürnberg (50). The term “asphyxia” was criticized from the beginning, but “apparent death” had fallen from grace and could no longer be used for a baby having difficulty breathing at birth. This change did not put forward a definition, but was understood as shift from unavoidable fate to preventable condition.
Asphyxia classified by alleged grades
The textbook on obstetrics by Heidelberg obstetrician Hermann Naegele exemplifies how the interpretation of birth asphyxia changed in the second half of the nineteenth century: In the fifth edition of 1863 (51), he proposed the traditional classification: (1) asphyxia livida suffocatoria due to compressed placenta or cord; (2) asphyxia livida apoplectica due to compressed brain; (3) asphyxia pallida due to exhausted nervous activity, blood loss, and placental insufficiency. In the eighth edition of 1872 (52), Naegele equated asphyxia and apparent death, defined as minimal signs of life with some vitality preserved, and specified three grades: (1) mild: skin blue, but some respiratory efforts; (2) medium: skin pale, gasping, poor reflex activity; (3) severe: slow heart action, no respiratory effort, no reflex activity. In 1931, New York anesthesiologist Paluel Flagg classified neonatal asphyxia in three grades according to reflex excitability (53): mild: depression; moderate: spasticity; severe: flaccidity.
Retrospective brain damage
In 1784, London surgeon and male midwife Micheal Underwood described palsy of the lower extremities: “it seems to arise from debility..., and usually attacks children one year old.... The first thing observed is debility of the lower extremities, which gradually become more infirm.” (54) In 1824, Pierre Flourens located the main respiratory regulator in the medulla oblongata and induced asphyxia in animals with lesions therein (55). In 1826, Johann Christian Jörg noted (56): “In too early and unripe born children a state of weakness may persist... in the muscles until puberty or even longer. It hinders the child in the use of its limbs and in holding head and trunk.”
In 1862, London orthopedist William John Little published his influential paper relating deformities to “abnormal parturition, difficult labours, premature birth, and asphyxia neonatorum” (57): “a larger proportion of infants, either dead, stillborn, apoplectic, or asphyxiated at birth, have been rendered so by interruption of the proper placental relation of the fetus to the mother, and non-substitution of pulmonary respiration, than from direct mechanical injury to the brain and spinal cord.” A closer look into this paper reveals that half of Little’s 49 infants were preterm, and that only five had been both term and asphyctic; no postmorte findings were reported. From one case involving a traumatic breech delivery and a literature search on 34 cases with cerebral palsy, Sarah McNutt concluded in 1885 (58) that “meningeal hemorrhage at parturition [is] one of the commonest agencies in the production of spastic hemiplegia.” William Osler used the term cerebral palsy in 1889 for hemiplegia and diplegia in 140 children (59), ascribing its etiology to trauma and infection, but not to birth asphyxia. In 1897, Siegmund Freud contradicted Little (60): “Premature, precipitate and difficult birth and asphyxia neonatorum are not causal factors in the production of diplegia; they are only associated symptoms of deeper lying influences which have dominated the development of the foetus or the organism of the mother.” However, his criticism went unheeded: Little’s hypothesis fulfilled an obvious need for causality all too well. In 1927, Lotte Landé stressed the importance of malformations and cautioned against overestimating the role of birth trauma in causing cerebral palsy (61).
Eastman and DeLeon compared 96 children with cerebral palsy and a control group in 1955 (62): 41% of the CP patients had “poor” adaptation (controls: 2%); 34% were born preterm (controls: 9%); 50% had fever at birth (controls: 6%); and 15% had malformations (controls: 2%). The population-based prospective study from Australia (63) showed that <10% of cerebral palsies were associated with birth asphyxia. Considerable evidence has accumulated in recent decades that rather than birth asphyxia, prenatal events like growth retardation, infection, or genetic abnormalities are what causes cerebral palsy (64).
Measurements and definitions
The era of measurement dawned in the twentieth century, and blood gas analysis helped to better understand birth asphyxia: In 1928, Blair Bell and his associates in Liverpool reported a mean oxygen content of 9.02 vol% in blood of the umbilical vein and of 5.85 vol% in that of the umbilical artery at birth (65). In Baltimore in 1932, Nicholson Eastman published cord blood gas analyses of infants with and without asphyxia (66): “The primary blood chemical change in asphyxia neonatorum is a reduction in the oxygen content of the fetal blood to extremely low levels, the blood of the umbilical vein falling in fatal cases below one volume per cent.... The serum pH of asphyxiated infants is reduced to the lower limits compatible with life...”
The New York anesthesiologist Virginia Apgar, disturbed by the lack of specificity in resuscitation and by the poor quality of asphyxia studies, devised a clinical score in 1953 to quantify the degree of asphyxia and improve resuscitation efforts in the neonate (67). In a neurodevelopmental follow-up in 215 infants she found “no significant correlation between I.Q. and oxygen content or saturation at any time during the first three hours of life (68)” (Figure 4l). Apgar’s associate L Stanley James published blood gas measurements of umbilical venous and arterial blood in infants with and without asphyxia in 1958 (69): “Some degree of asphyxia, usually of brief duration, is a normal finding in all births... asphyxia produces a respiratory acidosis followed by a superimposed metabolic acidosis.” However, the Apgar score and base deficit correlated poorly (Figure 4r). In 1959, Dawes et al. (70) in Oxford found that severely hypoxic lamb fetuses survived up to 1 h by raising their blood pressure and heart rate. Apgar’s and James’ work paved the way towards a definition of asphyxia, but it remains difficult to understand how and why the Apgar score and cord blood gases were mistakenly employed for neurodevelopmental prognostication (71) and to justify bicarbonate buffering (72). Whereas the International Classification of Diseases continued to derive the birth asphyxia diagnosis from the Apgar score, the American Academy of Pediatrics stated in 1986 that the Apgar score alone suffices for neither diagnosis nor prognosis (71). The first clear definition of birth asphyxia was provided by the American College of Obstetrics and Gynecology in 1992 (73), demanding each of four criteria: pH<7.00; Apgar score <4 for more than 5 min; neonatal neurologic sequelae; multiorgan dysfunction. Endorsed by 16 scientific societies, this template was further specified in 1999 by MacLennan (74): “Essential criteria defining an acute intrapartum hypoxic event: pH <7.0, base excess >12 mmol/l, early symptoms of neonatal encephalopathy, later cerebral palsy. Additional nonspecific criteria that help to time the lesion are: a sentinel hypoxic event, sudden sustained decrease of fetal heart rate, Apgar 0–6 for longer than 5 min, early multiorgan failure, early cerebral imaging with evidence of brain damage.” In 2005 the ACOG decreed (75): “The term birth asphyxia is nonspecific and should not be used.”
Assessment of birth asphyxia by Virginia Apgar 1955 and L Stanley James 1958. (Left, ref. (68)) Correlation between heel blood O2 content at 10–14.9 min and Stanford–Binet Intelligence Quotient (I.Q.) at 28 months to 5 years in 215 infants. (Right, ref. (69)) Correlation between Apgar score at 1 min and buffer base in umbilical artery blood in 43 infants with a low oxygen saturation and high CO2 tension, signaling “some degree of asphyxia”. Open/closed circles, regional/inhalation anaesthesia at vaginal delivery; open/closed squares, regional/inhalation anesthesia at cesarean section.
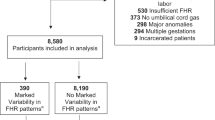
Electronic fetal monitoring and litigation
Information on the fetal state was scarce up to the nineteenth century. In 1766 Wrisberg (76) and in 1818 Mayor (77) used direct auscultation, but fetal heart rate monitoring became generally accepted with Lejumeau de Kergaradec’s use of the stethoscope in 1822 (78). Electric augmentation and graphic registration were used by Sampson et al. in 1926 (79). Continuous electronic fetal heart rate monitoring was developed in the late 1950s by Hon and Hess (New Haven) (80), Roberto Caldeyro-Barcia (Montevideo) (81) (4th Intern. Conf.), and Konrad Hammacher (Düsseldorf) (82). Its history has been detailed by Goodlin (7) and Banta and Thacker (8). Electronic monitoring during birth was generally introduced in the 1970s without scientific validation, but with strong support by the monitoring industry. In 1985, Devoe et al. (83) collected 21 different analysis criteria used in 45 studies, many without calculating sensitivity, specificity, and predictive values. Controlled studies shed doubts on this technique, as was reported by Banta and Thacker in 1978 (84): “No decrease in perinatal deaths, no fewer admissions to NICU, no less cerebral palsy.... We found no benefit but substantial risk due to increased incidence of Caesarean delivery.” A fierce controversy began (8): “Obstetricians were outraged at the conclusions of this report...” an editorial stated: “the findings were sweeping, poorly thought out, and extremely negative.” This did not change the facts, and 40 years later the 2017 Cochrane review, which included 13 randomized trials involving over 37,000 women gave no better news (85): “Compared with intermittent auscultation, continuous cardiotocography reduced the neonatal seizure rate, but showed no improvement in perinatal deaths and cerebral palsy rates.... There was an increase in Caesarean sections [by 63%] and instrumental vaginal deliveries.” Meanwhile from 5% in 1970, the rate of cesarean deliveries skyrocketed to 20% in Asia, 26% in Europe, 33% in North America, and 42% in Latin America (86). Also the number of malpractice tort trials rose. However, electronic fetal monitoring persisted, as did cerebral palsy, which remained constant at 2 per 1,000 (87). Rapidly, they both made their way into litigation. Obstetricians became the most frequently sued physicians in the United States of America (2). In 2006, their insurance premiums had risen up to US$ 299,420 per year (1), and 60% of the malpractice insurance premiums covered lawsuits for allegedly birth-related cerebral palsy (88). In Australia, obstetricians (2% of the physician group) account for 18% of all payments (89), while they are becoming an endangered species in the United States of America (90). In Germany, midwives could no longer afford the insurance premiums (91) and have disappeared from some regions.
Conclusions
Birth and birth asphyxia have been accompanied by 500 years of bitter competition between midwives and surgeons. The diagnosis “asphyxia” originated around 1774, not on scientific grounds but linked to the obsession of being buried alive, to avoid the emotionally charged “apparent death.” It is epistemiologically interesting that the term “asphyxia” was criticized from the very beginning because of its semantical incorrectness (pulselessness), but never for the more important lack of a definition. William Little’s unproven hypothesis of 1862 fulfilled perfectly the need for causality in families burdened with a child suffering from cerebral palsy. This tragic disease, sometimes accompanied by mental impairment, became less tolerated when infant deaths waned. As decried by Virginia Apgar, the poor definition of birth asphyxia precluded scientific studies for a long time. The unjustified linking of asphyxia to cerebral palsy, ascribing unproven diagnostic power to electronic monitoring, and the belief in prevention via cesarean section transformed common delivery techniques into malpractice. This may have been promoted by age-old competition between midwives and surgeons, which created a culture of blame and undermined the respect for both professions.
References
Hankins GD, MacLennan AH, Speer ME, Strunk A, Nelson K . Obstetric litigation is asphyxiating our maternity services. Obstet Gynecol 2006;107:1382–5.
Studdert DM, Mello MM, Gawande AA et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med 2006;354:2024–33.
Obladen M . History of neonatal resuscitation. Part 1: Artificial ventilation. Neonatology 2008;94:144–149.
Obladen M . History of neonatal resuscitation. Part 2: Oxygen and other drugs. Neonatology 2009;95:91–96.
Obladen M . History of neonatal resuscitation. Part 3: Endotracheal intubation. Neonatology 2009;95:198–202.
Aveling JH . The Chamberlens and the Midwifery Forceps. Churchill: London, UK, 1882: 222–223.
Goodlin RC . History of fetal monitoring. Am J Obstet Gynecol 1979;133:323–352.
Banta HD, Thacker SB . Historical controversy in health technology assessment: the case of electronic fetal monitoring. Obstet Gynecol Surv 2001;56:707–719.
Stiller S . Entstehung und Wandel der Diagnose “Geburtsasphyxie” [Origin and Change of the Diagnosis “Birth Asphyxia”]. Med. Inaug.-Diss: Freiburg, Germany, 2015.
Kaibel G . Epigrammata Graeca: ex lapidibus conjecta [Greek stone inscriptions]. Reimer: Berlin, Germany, 1878: 17.
Hippocrates. Superfetation. Edited and translated by Paul Potter: Hippocrates Works, vol. 9; Loeb Classical Library 509. Harvard University Press: Cambridge MA and London, UK, 2010: 329.
Aristotle. Historia animalium [History of Animals], Book VII–X Engl. translation by DM Balme: Loeb Classical Library 439 vol. 9. Harvard University Press: London, UL and Cambridge, MA, 1991: 587a20–24.
Temkin O . Soranus’ Gynecology. John Hopkins Press: Baltimore, MD, 1956: 80.
Theodosiani. Libri XVI cum constitutionibus Sirmondianis Th. Mommsen, vol. XI, Title 27 Weidmann: Dublin, Ireland, UK and Zürich, Germany, 1971: 616.
Mercurio S . Kinder-Mutter oder Hebammen-Buch [The Midwives' Book] (1st Italian ed. 1595). Translated by Gottfried Welsch. Tobias Mevii Erben und Elerd Schumacher: Wittenberg, Germany, 1671.
Radcliffe W . Milestones in Midwifery. John Wright & Sons: Bristol, UK, 1967: 11.
Burckhard G . Studien zur Geschichte des Hebammenwesens [Studies on the history of midwifery]. Band I, Heft 1: Die deutschen Hebammenordnungen von den ersten Anfängen bis auf die Neuzeit. Verlag von Wilhelm Engelmann: Leipzig, Germany, 1912: 162.
Icart J-F . Mémoire sur le besoin indispensable de quelques instruments simples et faciles a employer, dont les Sages-Femmes de la Campagne devraient être pourvues [Report on the need for some instruments with which the country midwives should be equipped]. Imprimerie de Robert: Castres, France, 1786.
Robinson JO . The barber-surgeons of London. Arch Surg 1984;119:1171–1175.
Donnison J . Midwives and Medical Men. A History of Inter-Professional Rivalries and Women's Rights. Schocken Books: New York, 1977.
Pugh B . A Treatise of Midwifery, Chiefly With Regard to the Operation. Buckland: London, UK, 1754: III.
Rösslin E . Der Swangern Frauwen und hebammen Rosegarten [Pregnant womens' rose garden]. (Engl. transl. Thomas Reynald 1540). Facsimile Antiqua Verlag Wutöschingen 1993: Straßburg, France: Martin Flach, 1513: A IVv, 94.
Petrelli RL . The regulation of French midwifery during the Ancien Régime. J Hist Med Allied Sci 1971;26:276–292.
Guillemeau J . De la grossesse et accouchement des femmes. Du gouvernement d'icelles; Ensemble de la nourriture des Enfans [Of Pregnancy and Childbirth, Treatment of Women, and Infant Nutrition]. Abraham Pacard: Paris, 1620: 174.
Perkins W . Midwives versus doctors: the case of Louise Bourgeois. The Seventeenth Century 1988;3:135–157.
Paré A . The generation of man (1st ed. Paris 1573). In: Thomas Johnson: The workes of that famous chirurgion Ambrose Parey, vol. 67. Richard Cotes and Willi Du-gard: London, UK, 1649: 603, 614, 647.
Willughby P . Observations on midwifery [1672]. Edited from the original manuscript by: Henry Blenkinsop. SR Publishers: Wakefield, Yorkshire, UK, 1972: 126.
Siegemundin J . Königl.-Preußische und Chur-Brandenburgische Hof-Wehe-Mutter, das ist: Ein höchst nöthiger Unterricht von schweren und unrecht-stehenden Geburthen [The Royal Prussian and Electoral Brandenburg Court Midwife] (1st ed. 1690). Christian Friedrich Voß: Berlin, Germany, 1752: 246.
Nihell E . A treatise on the art of midwifery. Setting Forth Various Abuses Therein, Especially as to the Practice with Instruments. Morley: London, UK, 1760: 245.
Fores SW . Man-Midwifery Dissected; or, the Obstetric Family-Instructor. For the Use of Married Couples, and Single Adults of Both Sexes. In Four Letters. Pseudonym: John Blunt. London, UK: Fores, 1793.
Hagen JP . Versuch eines allgemeinen Hebammen-Catechismus, oder: Anweisung für Hebammen, Unterricht für Schwangere, Gebährende und Wöchnerinnen; imgleichen Anleitung zur Einsicht, Beurtheilung und Heilung der Krankheiten und Zufälle neugebohrener Kinder und Säuglinge [An Attempt to Compile a General Midwives' Catechism], 4th edn. Friedrich Maurer: Berlin, Germany, 1791: XII–XVIII.
Hauck GP . Lehrbuch der Geburtshülfe zum Unterricht für die Hebammen in den Königlich Preussischen Landen [Textbook of Obstetrics for the Instruction of Midwives in Prussia]. Berlin, Germany: Enslin, 1815.
Ahlfeld F . Buchanzeige: Hebammen-Lehrbuch, herausgegeben im Auftrage des Königl. Preussischen Ministers der geistlichen, Unterrichts- und Medizinalangelegenheiten [Book review: The Royal Prussian Midwives' Textbook]. Monatsschr Geburtshülfe Gynäkol 1905;21:123–131.
Buchner E . Lehrbuch der gerichtlichen Medizin für Ärzte und Juristen [Textbook of forensic medicine for physicians and jurists], Nach dem Tode des Verfassers herausgegeben von: Karl von Hecker: 2nd edn Finsterlin: München, 1872: 449.
Bagellardo P . Opusculum recens natum de morbis puerorum, cum appendicibus magistri Petri Toleti [Little Book on the Diseases of Children, with Annotations by Peter Toletus] (1st ed. 1472),, France: [Jean Barbou] for German Rose, 1538: 4, 31, 43.
Mauriceau F . Traité des maladies des femmes grosses, et de celles qui sont accouchées; enseignant la bonne & véritable méthode pour bien aider les Femmes en leurs Accouchemens naturels, & les moyens de remedier a tous ceux qui sont contre nature, & aux indispositions des enfans nouveau-nés [The diseases of women with child, and in child-bed... and on newborn infants' disorders] (1st edn 1668), 7th edn, vol. 1, Compagnie des Libraires: Paris, France, 1740 329, 367, 481.
Mayow J . On the respiration of the foetus in the uterus (1st Latin ed. 1674). Alembic Club (ed). In:. Medico-Physical Works. Being a translation of Tractatus quinque medico-physici. Alembic Club: Edinburgh and London, UK, 1907: 203–204.
Verheyen P . Corporis humani anatomia [Anatomy of the Human Body]. Apud Aegidium Denique: Lovanii, Belgium, 1693: 116 Tabula 11.
Girtanner C . Anfangsgründe der antiphlogistischen Chemie [Basics of Antiphlogistic Chemistry]. Johann Friedrich Unger: Berlin, Germany, 1792: 248–253.
Lebreton A . Untersuchungen über die Ursachen und die Behandlung mehrerer Krankheiten der Neugeborenen [Investigation of Causes and Treatment of Several Disorders of Neonates]. (1st French ed. 1819). Translated by Gottlob Wendt. Leipzig, Germany: Industrie-Comptoir, 1820: 1.
Martel J . De la mort apparente chez le nouveau-né [On Apparent Death of the Newborn]. Baillière: Paris, France, 1874.
Hufeland CW . Enchiridion medicum or the practice of medicine (1st German ed. Berlin 1836). William Radde, 1855: 261 537.
Goethe JW . From My Life. Poetry and Truth (1st German ed. Stuttgart 1811). Translated and edited by Robert R Heitner and Thomas P Saine. Suhrkamp: New York, 1987: 21.
Lancisi GM . Abhandlung von plötzlichen und seltsamen Todesfällen und ihren Ursachen [Treatise on Sudden and Unexplained Cases of Death]. (Lat. ed. Rome 1707). Weygand: Leipzig, Germany, 1785.
Winslow J . Dissertation sur l'incertitude des signes de la mort, et l'abus des enterrements. Dissertation on the Uncertainty of the Signs of Death. Translated by Jean-Jacques Bruhier. : Morel, Prault, Simon: Paris, France, 1742.
Ackerknecht EH . Death in the history of medicine. Bull Hist Med 1968;42:19–23.
De Garda[n]ne JJ . Catechisme sur les morts apparentes dites asphyxiés [Catechism of Apparent Death Called Asphyxia] (1st ed. 1781). Imprimé et publié par ordre du gouvernement. Dijon, France: Defay, 1783.
Garda[n]ne JJ . Katechismus der anscheinenden Todesfälle oder sogenannten Pulslosigkeit [Catechism of Apparent Death Called Asphyxia]. Friedrich Maurer: Berlin, Germany, 1787.
Aitken J . Principles of Midwifery, or Puerperal Medicine (1st ed. Edinburgh 1784). Edinburgh Lying-in Hospital: Edinburgh, UK, 1785.
Aitken J . Grundsätze der Entbindungskunst [Principles of Obstetrics]. Translated by: Carl Heinrich Spohr: Nürnberg, Germany: Raspische Buchhandlung, 1789.
Naegele HF . Lehrbuch der Geburtshülfe [Textbook of Obstetrics], 5th edn. Victor von Zabern: Mainz, Germany, 1863: 784–787.
Naegele HF . Lehrbuch der Geburtshülfe [Textbook of Obstetrics], 8th edn. Victor von Zabern: Mainz, Germany, 1872: 811–821.
Flagg PJ . The treatment of postnatal asphyxia. Am J Obstet Gynecol 1931;21:537–541.
Underwood M . A Treatise on the Disorders of Childhood, and Management of Infants from the Birth; Adapted to Domestic Use (1st edn London 1784), 2nd edn, vol. 1. London, UK: Matthews, 1801: 13, 91.
Flourens P . Recherches expérimentales sur les propriétés et les fonctions du système nerveux dans les animaux vertébrés [Experimental Research on Properties and Functions of the Nervous System]. Paris, France: Crevot, 1824.
Jörg JCG . Handbuch zum Erkennen und Heilen der Kinderkrankheiten. nebst der Physiologie, Psychologie und diätetischen Behandlung des Kindes [Handbook for the Diagnosis and Treatment of the Diseases of Children], vol. 1. Leipzig, Germany: Carl Cnobloch 1826: 369.
Little WJ . On the influence of abnormal parturition, difficult labours, premature birth and asphyxia neonatorum on the mental and physical condition of the child, especially in relation to deformities. Trans Obstet Soc Lond 1861–1862;3:293–344.
McNutt SJ . Double infantile spastic hemiplegia, with the report of a case. Am J Med Sci 1885;89:58–79.
Osler W . The cerebral palsies of children. A clinical study from the Infirmary for Nervous Diseases, Philadelphia. Lewis: London, UK, 1889: 91, 96.
Freud S . Die infantile Cerebrallähmung [The Infantile Cerebral Palsy]. In: Nothnagel H (ed). Specielle Pathologie und Therapie, vol 9. Wien, Germany, Alfred Hölder, 1897: 11.
Landé L . Zur Kritik der ätiologischen Überschätzung des Geburtstraumas [A Critique of Etiologic Overestimation of the Birth Trauma]. Zeitschr Kinderheilk 1927;44:435–445.
Eastman NJ, DeLeon M . The etiology of cerebral palsy. Am J Obstet Gynecol 1955;69:950–961.
McIntyre S, Blair E, Badawi N, Keogh J, Nelson KB . Antecedents of cerebral palsy and perinatal death in term and late preterm singletons. Obstet Gynecol 2013;122:869–876.
Nelson KB, Blair E . Prenatal factors in singletons with cerebral palsy born at or near term. N Engl J Med 2015;373:946–953.
Blair Bell W, Cunningham L, Jowett M, Millet H, Brooks J . The metabolism and acidity of the foetal tissues and fluids. BMJ 1928;1:126–131.
Eastman NJ . Foetal blood studies III. The chemical nature of asphyxia neonatorum and its bearing on certain practical problems. Bull J Hopkins Hosp 1932;50:39–50.
Apgar V . A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg 1953;32:260–267.
Apgar V, Girdany BR, McIntosh R, Taylor HC Jr . Neonatal anoxia. I. A study of the relation of oxygenation at birth to intellectual development. Pediatrics 1955;15:653–662.
James LS, Weisbrot IM, Prince CE, Holaday DA, Apgar V . The acid–base status of human infants in relation to birth asphyxia and the onset of respiration. J Pediatr 1958;52:379–394.
Dawes GS, Mott JC, Shelley HJ . The importance of cardiac glycogen for the maintenance of life in foetal lambs and new-born animals during anoxia. J Physiol 1959;146:516–538.
American Academy of Pediatrics Committee on Fetus and Newborn. Use and abuse of the Apgar score. Pediatrics 1986;78:1148–9.
Usher R . Reduction of mortality from respiratory distress syndrome of prematurity with early administration of intravenous glucose and sodium bicarbonate. Pediatrics 1963;32:966–975.
American College of Obstetrics and Gynecology. Fetal and neonatal neurologic injury. Technical Bulletin Number 163, January 1992. Int J Gynecol Obstet 1993;41:97–101.
MacLennan A . International Cerebral Palsy Task Force: a template for defining a causal relationship between acute intrapartum events and cerebral palsy: international consensus statement. BMJ 1999;319:1054–1059.
American College of Obstetrics and Gynecology. Committee Opinion Nr. 326: inappropriate use of the terms fetal distress and birth asphyxia. Obstet Gynecol 2005;106:1469–70.
Roederer JG . Elementa artis obstetriciae in usum auditorium [Elements of Obstetrics, to Accompany Lectures] (1st ed. Goettingiae 1753). edited by: Heinrich August Wrisberg: 2nd edn Abraham Vandenhoeck: Goettingiae, 1766 69, note 63.
Laennec RTH . Traité de l'auscultation médiate et des maladies des poumons et du coeur [Treatise of Indirect Auscultation and on the Diseases of Lung and Heart] (1st ed. Paris 1819), 4th edn., vol. 3 Chaudé: Paris, 1837: 520–521.
Lejumeau de Kergaradec J-A . Mémoire sur l'auscultation appliquée a l'étude de la grossesse, ou Recherches sur deux nouveaux signes propres à faire reconnaître plusieurs circonstances de l'état de géstation [Report on Auscultation in Pregnancy], Lu à l'Académie Royale de médecine dans sa séance générale du 26 décembre 1821 Méquignon-Marvis: Paris, France, 1822.
Sampson JJ, McCalla RL, Kerr WJ . Phonocardiography of the human fetus. Am Heart J 1926;1:717–734.
Hon E, Hess OW . Instrumentation of fetal electrocardiography. Science 1957;125:553–554.
Caldeyro-Barcia R . Estudio de la anoxia fetal intrauterina mediante el ECG fetal y el registro de la frecuencia cardiaca fetal [Study of fetal anoxia by ECG and continuous registration of fetal heart rate]. In: Tecer Congreso Latinoamericano de Obstetricia y Ginecologia. Ed. Escuela de Medicina de la Ciudad Universitaria, Mexico D.F., 1958, Vol 2, pp. 383–390.
Hammacher K . Neue Methode zur selektiven Registrierung der fetalen Herzschlagfrequenz [New method to selectively record fetal heart rate]. Geburtsh Frauenheilk 1962;22:1524–1543.
Devoe LD, Castillo RA, Sherline DM . The nonstress test as a diagnostic test: a critical reappraisal. Am J Obstet Gynecol 1985;152:1047–1053.
Banta HD, Thacker SB . Costs and Benefits of Electronic Fetal Monitoring. National Center for Health Services Research: Hyattsville, MD, 1978.
Alfirevic Z, Devane D, Gyte GML, Cuthbert A . Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Sys Rev 2017: CD006066.
Betran AP, Ye J, Moller A-B, Zhang J, Gülmezoglu AM, Torloni MR . The increasing trend in Caesarean section rates: Global, regional and national estimates: 1990–2014. PLoS ONE 2016;11:1–12.
Emond A, Golding J, Peckham C . Cerebral palsy in two national cohort studies. Arch Dis Child 1989;64:848–852.
Freeman JM, Freeman AD . Risk management foundation: no-fault neurological compensation: perhaps its time has come, again. Harvard Med Inst Forum 2003: 5–6.
Johnson SL, Blair E, Stanley FJ . Obstetric malpractice litigation and cerebral palsy in term infants. J Forensic Leg Med 2011;18:97–100.
Sartwelle TP, Johnston JC . Cerebral palsy litigation: change course or abandon ship. J Child Neurol 2015;30:824–841.
Peters M, Dintsios CM . Marktversagen im Haftungsbereich: Die aktuelle Haftpflichtversicherungssituation der Hebammen in Deutschland [Market failure in liability: the state of insurance of German midwives]. Gesundh Ökon Qual Manag 2015;20:157–162.
Rueff J . De conceptu, et generatione hominis : de matrice et eius partibus, nec non de conditione infantis in utero. [On Human Conception and Pregnancy]: Sigmund Feyerabend. Frankfurt, 1587:25.
Dalechamps J . Chirurgie Française [French surgery]. (1st ed. 1573). Olivier de Varennes: Paris, France, 1610: 323–336.
Scultetus J . Wund-Artzneyisches Zeug-Hauß. In zween Theil abgetheilt [The surgeon's store-house: in two parts]. Faksimile Druck hrsg. von Fa. L. Merckle, Blaubeuren, in Verbindung mit dem Stadtarchiv Ulm. Kommissionsverlag W. Kohlhammer, Stuttgart 1974. Johann Gerlins Seel. Wittib: Frankfurt, Germany, 1666: 42.
Smellie W . A Set of Anatomical Tables, with Explanations, and an Abridgement, of the Practice of Midwifery, with a View to Illustrate a Treatise on that Subject, and Collection of Cases. Freeman: London, UK, 1754 Table 21.
Acknowledgements
I thank Sieghard Irrgang, Kassel, for help with translations from Latin; Susanne Stiller, Karlsruhe, for sharing her literature collection and for critically reviewing the manuscript; Crestina Forcina, Wellcome Library, London, for Figure 2; and Carole Cürten, University of Freiburg, for editing the English.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Obladen, M. From “apparent death” to “birth asphyxia”: a history of blame. Pediatr Res 83, 403–411 (2018). https://doi.org/10.1038/pr.2017.238
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.238
This article is cited by
-
Additive interaction between birth asphyxia and febrile seizures on autism spectrum disorder: a population-based study
Molecular Autism (2024)
-
Meningitis, urinary tract, and bloodstream infections in very low birth weight infants enrolled in a heart rate characteristics monitoring trial
Pediatric Research (2020)
-
Insights in Pediatric Research
Pediatric Research (2019)
-
Mythen in der Neonatologie
Monatsschrift Kinderheilkunde (2018)