Abstract
Background/objectives:
Adult obesity has been shown to substantially heighten the risk of adverse health outcomes but its impact on life expectancy (LE) has not been quantified in Australia. Our aim is to estimate reductions in LE and years of life lost (YLL) associated with overweight and obesity, relative to those at a healthy weight for Australian adults aged 20–69 years.
Subjects/methods:
We used a microsimulation model of obesity progression in Australia that integrates annual change in BMI based on age and sex, with Australian life-table data and published relative risk of all-cause mortality for different BMI categories. Remaining LE and YLL compared to healthy weight were estimated using 10-year cohorts, by sex. A nationally representative sample of 12,091 adults aged 20–69 from the 2014/15 Australian National Health Survey were used to represent the input population of 14.9 million.
Results:
Estimated remaining years of LE for healthy weight men and women aged 20–29 years was approximately 57.0 (95% CI 56.7–57.4) and 59.7 (95% CI 59.4–60.0) years, respectively. YLL associated with being overweight at baseline was approximately 3.3 years. For those obese and severely obese the loss in LE was predicted to be 5.6–7.6 years and 8.1–10.3 years for men and women aged 20–29 years, respectively. Across men and women, excess BMI in the adult population is responsible for approximately 36.3 million YLLs. Men stand to lose 27.7% more life years compared to women.
Conclusions:
Overweight and obesity is associated with premature mortality at all ages, for both men and women. Adults aged 20–39 years with severe obesity will experience the largest YLL, relative to healthy weight. More needs to be done in Australia to establish a coherent, sustained, cost-effective strategy to prevent overweight and obesity, particularly for men in early adulthood.
Similar content being viewed by others
Introduction
Globally, obesity and severe obesity is a major public health problem due to its growing prevalence and association with a wide range of debilitating, chronic and life-threatening conditions. People who are obese have increased morbidity, mortality and reduced life expectancy (LE) when compared to those with healthy weight [1,2,3,4,5,6,7,8,9,10,11,12]. Accurate estimates of the impact of overweight, obesity and severe obesity on LE are important in measuring trends in mortality over time, identifying key gaps between sub-populations of interest and informing the design and targeting of interventions.
Previous studies have estimated the long-term impact of overweight, obesity and severe obesity on the years of life lost (YLL) relative to those with healthy weight [7,8,9,10,11,12]. Generally, when compared to healthy weight, more years of life are lost for higher BMI categories. For those with BMI values of 35 or greater, studies in over 20 countries have estimated the YLL to range from 2–14 years when compared to healthy weight [3, 5, 7, 8, 11]. In the literature, the impact of obesity on YLL and LE is mostly based on contemporaneous body mass index data and published life tables. However, while the literature has provided strong evidence for the association between weight status and LE, the YLL estimates across studies vary widely, may be potentially biased and subject to several limitations. Firstly, all but two of these studies relied on self-reported height and weight data to measure BMI. This could underestimate obesity prevalence and bias results, particularly if individuals with higher BMI underreport their weight [8, 10]. Secondly, the analyses in many of these studies assume that individuals remain in the same weight category over their life course [8], which may not be a realistic assumption. Given that there is a tendency for individuals to continue to gain weight into mid/late adulthood, restricting them to a base weight category may underestimate the impact of obesity on YLL.
In this study, we address these limitations by using a dynamic microsimulation model of obesity progression in Australian adults to project remaining LE and YLL by age, sex and baseline weight status groups. Importantly, our modelling methodology projects continuous age- and sex-specific changes in BMI and mortality and, therefore, allows individuals to move between weight categories over their future life course. Our study in the Australian context is of particular significance because the impact of increased weight on LE and YLL lost over the life course has not been explored for different aged adults. This is timely given that current obesity prevalence for Australian adults is estimated at 27.9% [13] and is expected to increase to 35% by 2025 [14].
Methods
Model description
We use a dynamic modelling approach that combines microsimulation and survey estimation techniques to model individual-level weight gain and weight-dependent mortality for the Australian adult population. The model uses annual discrete time steps, whereby each survey individual becomes one year older, may experience changes in BMI and/or die. Individual-level BMI changes are determined using annual weight gain equations based on age, sex and current position on the BMI spectrum [13]. We apply this model to investigate differences in mean LE and YLL lost (Independent samples t-test) by men and women of different ages in overweight, obese and severely obese groups compared to healthy weight.
Study population
Life expectancy estimates were simulated for a baseline input population of adults from the 2014/15 Australian Bureau of Statistics National Health Survey (NHS) [14]. The survey was conducted in all states and territories and across urban, rural and remote areas of Australia. Approximately 19,000 people were sampled using a stratified multistage sampling design, which ensured representation of the Australian population. Data were available as confidential unit record files (CURFs) and include individual person survey weights, which permitted the use of survey estimation techniques to determine simulated outputs that are representative of the total Australian adult population. The input population consisted of 12,091 individuals aged between 20 and 69 years of age with measured height and weight, excluding those who were pregnant. This represents almost 15 million adults in 2014/15.
Measurement of BMI
Measurement of height and weight of survey participants was voluntary and carried out by trained interviewers. Height was measured using a stadiometer and recorded in centimetres correct to two decimal points. Weight was determined using digital platform scales and recorded in kilograms correct to one decimal point. Body mass index was calculated from weight in kg divided by height in metres squared, and weight status groups were defined as follows: healthy/underweight (BMI < 25), overweight (25 ≤ BMI < 30), obesity (30 ≤ BMI < 35) and severe obesity (BMI ≥ 35). In the 2014/15 NHS any missing data on BMI were imputed using a ‘hot decking’ imputation method [15], not used in previous national health surveys.
Calculation of mortality
Annual mortality is modelled separately as a function of age, sex and weight status. An increased risk of mortality for each 5-unit increase of BMI allowed the differentiation of mortality for individuals across the BMI distribution, including those severely obese (35 ≤ BMI < 40), extremely obese (40 ≤ BMI < 45) and morbidly obese (BMI ≥ 45) [2]. We used 2014/15 nationally representative BMI prevalence estimates by sex and 5-year age groups [14] and 2013–15 Australian life tables age- and sex-specific mortality rates [16] to partition mortality rates by weight status groups, sex and individual years of age. The formulae used to determine mortality rates have been described previously [13] and a figure presenting age-specific mortality rates, stratified by sex is included in the Supplementary Information (Fig. 1).
Validation
The model has been validated and shown to accurately predict weight gain and prevalence of healthy, overweight, obese and severely obese in Australian adult population until 2015 [13].
Model simulations
Life expectancy and years of life lost were estimated by age, stratified by sex and weight status (healthy, overweight, obese and severely obese) at baseline. To examine the effect of current weight status on remaining LE, simulations were run for Australian adults in five 10-year age cohorts 20–29, 30–39, 40–49 50–59 and 60–69 years starting with a baseline population from the 2014/15 NHS. This represents birth cohorts centred around 1950, 1960, 1970, 1980 and 1990. The model assumes that age-related annual weight gain, Australian age- and sex-specific mortality and risk of mortality associated with excess weight maintained beyond 2015.
Model simulations were run over a lifetime, or until all individuals died or reached 100 years of age. LE was determined from the area under the survivorship curves, with 95% confidence intervals reflecting individual-level heterogeneity. We summarised results by age cohort. For each age and sex cohort YLL was calculated as the difference in remaining LE between those in the healthy weight group and those in overweight, obese or severely obese baseline groups.
Code availability
All analyses and modelling were conducted using Stata version 14.2 (StataCorp, TX, USA). The model code is available upon request.
Risk chart
A risk chart for the Australian adult population aged 20–69 years was generated based on the results of the model simulations. The risk chart was stratified by 10-year age cohorts, sex and weight categories (overweight, obese and severely obese), showing the YLL relative to healthy weight.
Aggregate years of life lost
Lifetime YLL were estimated for the Australian adult population aged 20–69 years by multiplying 10-year age- and sex-specific estimates of average YLL for each weight category with the estimated prevalence of each overweight and obese group at baseline. These were calculated from 2014 until death or age 100 years, for each 10-year age and sex group.
Results
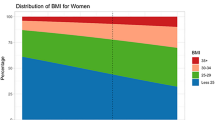
Table 1 presents the nationally representative input population in 10-year age cohorts, by sex and weight categories as estimated by the 2014/15 NHS. The cohorts represent 14.9 million Australian adults aged between 20 and 69 years. In 2014/15, the estimated prevalence of healthy weight decreased with increasing cohort age, while the prevalence of obesity and severe obesity increased with each 10-year age cohort.
Model predictions for remaining LE and YLL by sex and weight status in 10-year age cohorts are presented in Figs. 1 and 2. In general, the results show that higher BMI corresponds to lower remaining LE at any starting age. For example, a 25-year-old healthy male could expect to live a further 57.0 (95% CI 56.7–57.4) years, whereas those in overweight, obese and severely obese groups will, on average, live for a further 52.8 (95% CI 52.5–53.2), 48.7 (95% CI 48.2–49.3) and 46.6 (95% CI 44.6–47.5) years, respectively. Remaining LE predicted for women was greater than that for men at each age cohort, with a 25-year-old female expected to live another 59.7 (95% CI 59.4–60.0), 56.1 (95% 55.7–56.5), 53.6 (95% CI 53.0–51.2) and 51.9 (95% CI 51.1–52.8) years in the healthy, overweight, obese and severely groups, respectively. For each age and sex group, those with severe obesity had lowest LE, when compared to those at healthy weight.
The predicted YLL relative to their healthy weight counterparts was greater for those starting in a higher BMI category at all ages. For example, an overweight 25-year-old male and female experience approximately 4.2 (95% CI 3.7–4.7) and 3.6 (95% CI 3.1–4.1) YLL, respectively. For those obese and severely obese at baseline, males and females lose 8.3 (95% CI 7.7–8.9) and 6.1 (95% CI 5.4–6.8) years and 10.5 (95% CI 9.5–11.5) and 7.7 (95% CI 6.9–8.7) years relative to their healthy male and female counterparts, respectively. For a 65-year-old, the absolute differences in YLL are smaller but the gap when compared to those at healthy weight remains. The YLL for overweight, obese and severely obese 65-year-old males and females are approximately: 1.1 (95% CI 0.6–1.7) and 1.3 (95% CI 0.9–1.8) years; 2.7 (95% CI 2.2–3.3) and 2.3 (95% CI 1.9–2.8) years; and 4.6 (95% CI 3.9–5.3) and 4.5 (95% CI 4.0–5.1) years, respectively.
To provide information on the aggregate YLLs associated with excess weight at a population level, Table 2 presents estimates of the lifetime YLLs due to overweight and obesity for the 2014 Australian adult population aged 20–69 years of age. Overweight and obesity is responsible for approximately 36.3 million YLL over the life course. When stratified by sex, 27.7% more life years will be lost to men than women. In all, 20–29-year-old males and 30–39-year-old females stood to lose the most, with 5.6 million and 4.2 million YLL, respectively. The proportion of YLL for overweight, obese and severely obese was 36.0, 34.4 and 29.6%. While those severely obese contributed almost one-third of the life years lost, they comprised only 11% of the population.
Discussion
Using a validated simulation model [13], our study investigated the impact of weight status in 2014/15 on remaining LE and YLL for Australian adults aged 20–69 years. The model enabled dynamic movements of BMI gain/loss over the remaining life course determined by one’s current BMI levels, age and sex. This is the first study of its kind in the Australian context. Our results predicted that remaining LE will fall as BMI increases, irrespective of age and sex. What is striking is the magnitude of effect of increased BMI in adulthood on premature mortality when compared to a person with healthy weight over the life course. For a 25-year-old, we predicted a 4.2 and 3.6 year decrease in remaining LE for overweight men and women, an 8.3 and 6.1 year decrease in obese men and women; and a 10.5 and 7.7 year decrease in severely obese men and women, respectively.
The impact on YLL was greatest for severely obese individuals in the youngest (20–29 years and 30–39 years) age cohorts, with approximately 8–10 YLL for both men and women. The recent threefold increase in prevalence of severe obesity in young adults since 1995 [17] and predictions of increasing severe obesity among Australian adults [13] suggests that YLL due to severe obesity will increase in the future.
The YLL estimated for severely obese females in the 30–39 years age group was slightly greater than those estimated for the 20–29 years age group (7.7 vs. 9.5). This was explored in a sensitivity analysis (see Supplementary Tables 1 and 2), which found larger differences in the mean BMI between severe and healthy groups among those aged 30–39 years compared to the 20–29 year- and 40–49 year age groups. This could potentially be due to heterogeneity in real-life population data, sampling or measurement error and highlights how small changes in BMI can impact population-level YLL estimates in a simulation model.
Without effective action to address current trends, our analyses estimate that today’s adult population in Australia will collectively lose approximately 36.3 million years of life over a lifetime. Men will bear more of this burden, with 27.7% more life years lost compared to women. Collectively, young men and women stand to lose more years of life to overweight and obesity than do older men and women due in large part to greater potential years of life remaining. Interestingly, however, among men under 40 years and women under 30 years, the highest burden of disease in terms of YLL was not for those currently in obese or severely obese categories, but for those overweight. This suggests overweight, as well as obesity, should be targeted in treatment and prevention programs for young adults. Among older men the largest burden of YLL was for those currently obese and for older women was for those with severe obesity.
Our results corroborate with those that have modelled YLL for obese individuals over the life course using a life-table approach. One study estimated 6.2–10 YLL for severely obese adults in Canada [12], while other studies estimated between 6–13.7 YLL for severely and morbidly obese, respectively [3, 7]. However, all these studies used self-reported height and weight, which may have biased results due to misclassification across BMI categories [18]. Another study in the US that used a life-table approach with measured height and weight data estimated 6–7 YLL for 40-year old individuals with obesity when compared to healthy weight individuals [9], which are comparable to our estimates. Our study had larger YLL estimates in overweight cohorts compared to other studies [6, 8, 10], although the dynamic nature of the model updated change in BMI and mortality annually over the life course, whereas other studies were based on baseline weight status.
Risk charts are a good visualisation tool and have been widely used in general practice when assessing risk of cardiovascular disease in the general population [19, 20]. Our risk chart provides useful summary information on premature mortality for practitioners based on routinely collected data (age, sex, height and weight) in primary care. This risk chart could help improve risk communication between practitioners and patients by highlighting the potential years of life that could be gained by returning to a healthy weight. It can also be valuable for extrapolation of long-term health outcomes when assessing the impact of a short-term weight loss intervention.
The strengths of this study are the use of a validated model [13] that dynamically simulates age- and sex-specific weight gain using nationally representative survey data to accurately predict both obesity and severe obesity at a population level in Australia. By using continuous BMI rather than discrete BMI classes in the model, it enables us to quantify the increased impact of mortality at the upper end of the BMI distribution. This is important because an increasing proportion of the population are experiencing more severe levels of obesity at a population level, a relatively new phenomenon in Australia [21]. The relative risks associated with the estimated impact of weight gain on mortality are based on a large meta-analysis of over 900,000 individuals that adjusted for study differences, age at risk and baseline smoking status that limited reverse causality on the effects of pre-existing disease on BMI and mortality by excluding all person-years and deaths in the first 5 years of follow-up [2]. In the future, the model can be updated to incorporate Australian specific or updated mortality estimates when they become available.
Our results are subject to several limitations. The age-related annual weight gain equations in the model were based on the period 1995 to 2012 and we have assumed that these equations hold for this analysis, which predicts from 2014 into the future. Recent studies have indicated that the rate of weight gain has been slowing down [22, 23], suggesting that this assumption is reasonable. In the future, the flexible nature of this model enables the integration of re-estimated weight gain equations when new data become available, most notably the 2017/18 NHS. The age-specific mortality rates for each weight class were based on 2013/15 Australian Life Tables, throughout the simulation. This could potentially over-estimate the mortality rate and ultimately LE of healthy weight people, given life expectancies in Australia have been increasing over time. The model assumes that increase in weight and subsequently weight status has an instantaneous impact on mortality, yet we do not take into account whether increased weight status has a lagged effect on mortality. Further research in this area using longitudinal studies would help inform the model. The model does not adjust for smoking and hence is likely to underestimate mortality in smokers [3, 22]. However, the prevalence of Australian adults who currently smoke is low at 14.5%, having nearly halved in the past two decades and is expected to continue its downward trajectory [14]. Finally, we did not take into account the impact that increased BMI has on quality-of-life, where evidence has shown that there are significant impairments to health-related quality-of-life for individuals at more severe levels of obesity as a result of higher rates of co-morbidity and disability [24,25,26,27].
In the future, the model can estimate the impact of successful weight loss interventions on different age groups to understand which groups stand to achieve the largest health gains. Further work is required to incorporate sub-models to estimate healthcare costs over time to enable modelling cost-effectiveness and long-term cost and health outcomes of different obesity prevention and management strategies.
We conclude that overweight and obesity is associated with a decrease in LE for all adults aged 20–69 years for both men and women in Australia. We predict that severely obese individuals in the 20–39 year age groups experience the greatest decrease, of approximately 8–10 years when compared to those in the healthy weight category. With an increase in the prevalence of severe obesity, the potential impact in the future could be much greater. More needs to be done in Australia to establish a coherent, sustained, cost-effective obesity prevention strategy [28], particularly in encouraging young adults (particularly men) to lose weight and in preventing them becoming obese, which in turn may involve programs targeting children and adolescents.
References
Chang S-H, Pollack LM, Colditz GA. Life years lost associated with obesity-related diseases for US non-smoking adults. PLoS ONE. 2013;8:e66550.
Collaboration PS. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Finkelstein EA, Brown DS, Wrage LA, Allaire BT, Hoerger TJ. Individual and aggregate years‐of‐life‐lost associated with overweight and obesity. Obesity. 2010;18:333–9.
Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–7.
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187–93.
Jia H, Zack MM, Thompson WW. Population-based estimates of decreases in quality-adjusted life expectancy associated with unhealthy body mass index. Public Health Rep. 2016;131:177–84.
Kitahara CM, Flint AJ, de Gonzalez AB, Bernstein L, Brotzman M, MacInnis RJ, et al. Association between class III obesity (BMI of 40–59 kg/m2) and mortality: a pooled analysis of 20 prospective studies. PLoS Med. 2014;11:e1001673.
Nagai M, Kuriyama S, Kakizaki M, Ohmori-Matsuda K, Sone T, Hozawa A, et al. Impact of obesity, overweight and underweight on life expectancy and lifetime medical expenditures: the Ohsaki Cohort Study. BMJ Open. 2012;2:e000940.
Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32.
Preston SH, Stokes A. Contribution of obesity to international differences in life expectancy. Am J Public Health. 2011;101:2137–43.
Reuser M, Bonneux L, Willekens F. The burden of mortality of obesity at middle and old age is small. A life table analysis of the US Health and Retirement Survey. Eur J Epidemiol. 2008;23:601.
Steensma C, Loukine L, Orpana H, Lo E, Choi B, Waters C, et al. Comparing life expectancy and health-adjusted life expectancy by body mass index category in adult Canadians: a descriptive study. Popul Health Metr. 2013;11:21.
Hayes A, Lung T, Bauman A, Howard K. Modelling obesity trends in Australia: unravelling the past and predicting the future. Int J Obes. 2016;41:178–85.
Australian Bureau of Statistics. National Health Survey: first results 2014-15 [Internet]. Canberra: ABS; 2015 [cited 9th August 2017]. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.001.
Australian Bureau of Statistics. 4363.0 - National Health Survey: Users' Guide, 2014-15: Imputation [Internet]. Canberra: ABS; 2017 [cited 9th August 2017]. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4363.0~2014-15~Main%20Features~Imputation~18.
Australian Bureau of Statistics. 3302.0.55.001 - Life Tables, States, Territories and Australia, 2013-2015: Data Cubes [Internet]. Canberra: ABS; 2016 [cited 9th August 2017]. Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3302.0.55.0012013-2015?OpenDocument#Data.
Australian Institute of Health and Welfare. Overweight and obesity in Australia: a birth cohort analysis. Canberra: AIHW; 2017. 46p. Cat. no: 215.
Shields M, Gorber SC, Tremblay MS. Effects of measurement on obesity and morbidity. Health Rep. 2008;19:77.
National Vascular Disease Prevention Alliance. Absolutecardiovascular disease management. Quick reference guide for health professionals [Internet]. NVPA; 2012 [cited 9th August 2017]. Available from: http://cvdcheck.org.au/pdf/Absolute_CVD_Risk-Quick_Reference_Guide.pdf.
Sharpe N, Coppell K, Bennett W. New Zealand Cardiovascular Guidelines Handbook: a summary resource for primary care practitioners. Wellington: New Zealand: Guidelines Group; 2009.
Keating C, Backholer K, Gearon E, Stevenson C, Swinburn B, Moodie M, et al. Prevalence of class-I, class-II and class-III obesity in Australian adults between 1995 and 2011–12. Obes Res Clin Pract. 2015;9:553–62.
Peeters A, Magliano DJ, Backholer K, Zimmet P, Shaw JE. Changes in the rates of weight and waist circumference gain in Australian adults over time: a longitudinal cohort study. BMJ Open. 2014;4:e003667.
Hayes A, Gearon E, Backholer K, Bauman A, Peeters A. Age-specific changes in BMI and BMI distribution among Australian adults using cross-sectional surveys from 1980 to 2008. Int J Obes. 2015;39:1209–16.
Jia H, Lubetkin EI. The impact of obesity on health-related quality-of-life in the general adult US population. J Public Health (Bangk). 2005;27:156–64.
Sach T, Barton G, Doherty M, Muir K, Jenkinson C, Avery A. The relationship between body mass index and health-related quality of life: comparing the EQ-5D, EuroQol VAS and SF-6D. Int J Obes. 2007;31:189–96.
Sendi P, Brunotte R, Potoczna N, Branson R, Horber FF. Health-related quality of life in patients with class II and class III obesity. Obes Surg. 2005;15:1070–6.
Walter S, Kunst A, Mackenbach J, Hofman A, Tiemeier H. Mortality and disability: the effect of overweight and obesity. Int J Obes. 2009;33:1410–8.
Obesity Policy Coalition and The Global Obesity Centre. Tipping the Scales: Australian Obesity Prevention Consensus [Internet]. OPC; 2017 [cited 11th December 2017]. Available from: http://www.opc.org.au/downloads/tipping-the-scales/tipping-the-scales.pdf.
Acknowledgements
We thank the Australian Bureau of Statistics for access to confidential unit record files pertaining to Australian Health Survey data. Dr. Lung is supported by a National Health and Medical Research Council Early Career Fellowship and the National Heart Foundation Postdoctoral Fellowship (NHMRC APP1141392). SJ is supported by an NHMRC Principal Research Fellowship (NHMRC APP1119443). Ms Killedar is supported by the Kassulke scholarship for PhD research. Dr. Tan receives funding support from the National Health and Medical Research Council Centre of Research Excellence in Early Prevention of Obesity in Childhood.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Lung, T., Jan, S., Tan, E.J. et al. Impact of overweight, obesity and severe obesity on life expectancy of Australian adults. Int J Obes 43, 782–789 (2019). https://doi.org/10.1038/s41366-018-0210-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0210-2
This article is cited by
-
Obesity at age 20 and weight gain during adulthood increase risk of total and premature all-cause mortality: findings from women attending breast screening in Manchester
BMC Women's Health (2023)
-
Overweight or obesity increases the risk of cardiovascular disease among older Australian adults, even in the absence of cardiometabolic risk factors: a Bayesian survival analysis from the Hunter Community Study
International Journal of Obesity (2023)
-
Effect of excise tax on sugar-sweetened beverages in Catalonia, Spain, three and a half years after its introduction
International Journal of Behavioral Nutrition and Physical Activity (2022)
-
The nursing care of people with class III obesity in an acute care setting: a scoping review
BMC Nursing (2022)
-
Characterization of the prevalence of excess weight in Brazil
BMC Public Health (2022)