Abstract
Background
In 2010, sugar sweetened beverages (SSBs) were estimated to cause 12% of all diabetes, cardiovascular disease (CVD) and obesity-related cancer deaths in Mexico. Using new risk estimates for SSBs consumption, we aimed to update the fraction of Mexican mortality attributable to SSBs, and provide subnational estimates by region, age, and sex.
Methods
We used an established comparative risk assessment framework. All-cause mortality estimates were calculated from a recent pooled cohort analysis. Age- and sex-specific relative risks for SSBs-disease relationships were obtained from updated meta-analyses. Demographics and nationally representative estimates of SSBs intake were derived from the National Health and Nutrition Survey 2012; and mortality rates, from the National Institute of Statistics and Geography. Attributable mortality was calculated by estimating the population attributable fraction of each disease, with uncertainty in data inputs propagated through Monte Carlo probabilistic sensitivity analyses.
Results
In Mexican adults 20 years and older, 6.9% (95%UI: 5.4–8.5) of all cause-mortality was attributable to SSBs, representing 40,842 excess deaths/year (95%UI: 31,950–50,138). Furthermore, 19% of diabetes, CVD and obesity-related cancer mortality was attributable to SSBs (95%UI: 11.0–26.5), representing 37,000 excess deaths/year (95%UI 21,240–51,045). Of these, 35.6% were diabetes-related (95%UI 16.4–52.0). Proportional burden was highest in the South (22.8%), followed by the Center (18.0%) and North (17.4%). Men aged 45–64-years in the Center region had highest proportional mortality (37.2%), followed by 20–44-year-old men living in the South (35.7%) and both men and women aged 20–44 living in the Center (34.4%).
Conclusions
Utilizing current evidence linking SSBs to cardiometabolic disease and obesity-related cancers, earlier estimates of Mexican mortality attributable to SSBs could have been underestimated. Mexico urgently needs stronger policies to reduce SSBs consumption and reduce these burdens.
Similar content being viewed by others
Introduction
Sugar sweetened beverages (SSBs) represent a major source of rapidly digestable, high volume added sugars in many countries and globally [1, 2]. Long-term observational cohorts and randomized controlled trials, indicate that SSBs intake independently contributes to weight gain and obesity [1, 3]. In addition, experimental evidence and cohort studies suggest that SSBs intake could play an important role in type-2 diabetes and cardiovascular disease, not only through weight gain, but also through changes in insulin resistance and visceral fat [4,5,6]. Cardiometabolic diseases and obesity-related cancers are leading causes of death worldwide, having a higher contribution in middle- and high-income countries [7]. With increasing policy attention to address risks of SSBs [8], understanding the contributions of SSBs intake to national and subnational rates of obesity, diabetes, and CVD deaths, is crucial to inform and implement strategies to alleviate these burdens.
Mexico is a global leader in SSBs intake. In 2011, the Mexican population consumed an average of 163 l per capita, a higher consumption than the United States or other Latin-American countries [9, 10]. SSBs intake in Mexico contributes to 70% of the total added sugars in the diet [11], and represents 10% of all calories consumed [12]. Currently, 73% of the population is overweight or obese, and nearly 1 in 10 has diabetes [13]. In addition, data on SSBs purchases suggest strong regional disparities in SSBs intake and disease risk across the country [14]. However, to our knowledge, the regional burdens of disease due to SSBs intake in Mexico have not been established.
A previous study utilizing global modeling data, estimated that 12% of all adult deaths related to diabetes, cardiovascular disease, and obesity-related cancers in Mexico in 2010 were attributable to SSBs intake [2]. Since then, considerable new evidence has emerged to better document the links between SSBs intake and cardiometabolic diseases [4, 6]. In addition, prior estimates of disease burdens did not assess regional differences within Mexico, which are important for local policy planning and prevention efforts. Updated estimates of SSBs-associated disease burdens in Mexico, including data on regional differences, are crucial to enable policy makers to design targeted interventions aimed at specific high-risk groups.
To address these gaps and elucidate the impact of SSBs intake on disease risk in the overall Mexican population as well as in key subgroups, we aimed to quantify the proportion of diabetes, CVD, obesity-related cancer, and all-cause mortality attributable to SSBs intake overall and by age, sex, and region in Mexico.
Methods
To estimate the fraction of adult mortality attributable to SSBs we linked three main sources of data: the consumption of SSBs in Mexico in 2012, the most updated relative risks from meta-analyses, and the number of deaths for SSBs-related diseases in the same year. Under the comparative risk assessment framework, we estimated the SSBs population attributable fractions (PAF) for diabetes, CVD, obesity-related cancers, and all-cause mortality stratified by population groups (age, sex, and region). Then, we multiplied the deaths due to diabetes, CVD, and obesity-related cancers by the corresponding PAF, which resulted in the SSBs absolute attributable mortality for each group. We obtained absolute attributable mortality by adding the number of deaths attributed to SSBs consumption for a given disease for all subgroups. Finally, to obtain proportional attributable mortality, the absolute attributable mortality was divided by the total number of deaths due to a given disease. An overview of the data sources that provide information on the Mexican population can be found in Table S1. Data sources for disease-specific relative risks are available in Table S2.
Population demographics
Data on population demographics for 2015 were derived from the National Population Council (CONAPO) estimates for 2010–2050 [15]. Given our focus on mortality, we only evaluated individuals aged 20+ years. Analyses were jointly stratified by age (20–44, 45–64, and 65+ years), sex, and region including Center (including Mexico City), North, and South (see S1 appendix for further details).
SSBs intake
Data on SSBs intake were obtained from the Mexican National Health and Nutrition Survey of 2012 (ENSANUT 2012). Briefly, ENSANUT 2012 uses a population-based, stratified, multistage, clustered design to obtain a representative sample of the Mexican population; further details are available [15]. Health and demographic data were obtained from a questionnaire provided to the entire adult sample, while dietary data were obtained in a randomly selected subsample using a Food Frequency Questionnaire (FFQ) in which subjects reported their food consumption over the previous week (n = 2642). We defined SSBs-servings (8 oz) according to the following categories: sugar-sweetened carbonated beverages; industrialized juices and “aguas frescas” with added sugar; prepared juices and “aguas frescas” with added sugars made at home or in a food establishment. To incorporate variation in SSBs intake by sex, age and region, SSBs intake in each stratum was aggregated at the individual level and then used as an input.
Cause-specific mortality
All-cause mortality data for adults 20 years and older were obtained for 2015 from the National Institute of Statistics and Geography (INEGI). INEGI statistics report underlying diseases as the cause of death; additional information regarding their methodology is available elsewhere [16]. For specific-cause mortality, we classified mortality according to the International Classification of Diseases, Tenth Revision (ICD-10), including deaths attributable to diabetes mellitus (E11), CVD [ischemic heart disease (I20–I25), ischemic stroke (I63, I65–I67, I69.3), and hypertensive heart disease (I11, I13)] and obesity-related cancers [postmenopausal breast cancer (C50), endometrial cancer (C54,C55), colon cancer (C18–C21), gall-bladder cancer (C23), esophageal adenocarcinoma (C15), pancreatic cancer (C25), and renal cancer (C64)]. All mortality data were stratified by age, sex, and region.
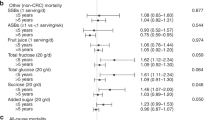
Effects of SSBs intake on cardiometabolic diseases, cancer and total mortality
The estimated effect of SSBs consumption on all-cause mortality (HR 1.06; 95%CI 1.05,1.07) was obtained from a pooled analysis of two United States cohorts. We selected the HR that did not adjust for BMI, to capture the total effect of SSBs intake on total mortality [17]. The etiologic effects of SSBs intake on diabetes, CVD, obesity-related cancers were estimated from published systematic reviews and meta-analyses (Table S2). The estimated effect of SSBs on diabetes (RR 1.39; 95%CI 1.18,1.64), was derived from a meta-analysis including 17 prospective cohorts that estimated the direct association between SSBs intake and type-2 diabetes; to capture the total effect of SSBs on diabetes we used the calibrated relative risk not adjusted for adiposity [4]. The estimated effect of SSBs consumption on CHD (RR 1.17; 95%CI 1.10,1.24) was derived from a meta-analysis of six prospective cohorts [6]. Due to the lack of availability of estimates of the total effect of SSBs on stroke and obesity-related cancers, we were forced to only consider the BMI-mediated effects of SSBs for these outcomes. Etiologic effects of SSBs on BMI were derived from pooled analyses of SSBs intake and long-term weight gain over 20 years, including 0.10 kg/m2 total BMI gain per daily SSBs serving for individuals with BMI <25 kg/m2 and 0.23 kg/m2 total BMI gain for individuals with BMI ≥25 kg/m2 [18]. Notably, these estimates are smaller than what would be expected considering the caloric content of SSBs, because they implicitly account for partial compensation, substitutes, and replacements with other beverages and foods. These estimates are also similar to demonstrated effects of changes in SSBs intake in randomized controlled trials of adolescents [19]. Effects of changes in BMI on stroke (RR 1.04; 95%CI[0.96,1.12] to 2.09; 95%CI[1.81,2.40]), hypertensive heart disease (RR 1.24; 95%CI[1.15,1.34] to 2.30; 95%CI[0.66,7.95]), and specific cancers (RR 1.07;95%CI [0.93,1.23] to 1.59; 95%CI[1.50,1.68]) were derived from pooled cohort analyses [20, 21]. All specific diseases and relative risks are shown in Table S2. For the purposes of this study the serving size used was 8 oz and all meta-analytic relative risks were adjusted accordingly.
Statistical analysis
The comparative risk assessment framework was used to estimate each stratum-specific and disease-specific PAF, which estimates the proportion of disease cases that would be averted if no SSBs were consumed, compared with the current distribution of SSBs intake. For each age, sex, and region stratum, we estimated the PAF of cause-specific deaths attributable to SSBs using an unbiased nonparametric estimate adapted from the maximum likelihood approach established by Taguri et al. [22]:
where, Xi denotes SSBs intake (servings per day) of the ith individual of the sample; with the sample weight wi; and θk which corresponds to the reported RR for one SSBs serving per day dependent on the kth disease, sex and age category to which the Xi individual belongs. The value obtained from evaluating RR(Xi; θk) is the specific relative risk for the ith individual considering consumption, sex, and age (Xi and θk). Corresponding functions to estimate stroke and obesity-related cancers are presented in the S2 Appendix.
The relative risks for diabetes and CHD that we used are not adjusted for BMI to capture the total effect of SSBs (that is BMI and non-BMI mediated), therefore we estimate them for each individual as follows:
Uncertainty intervals were obtained via bootstrap and 2642 simulations of the parameter θk. Replicate weights for bootstrap were obtained considering the complex design of the survey. The parameter θk was considered to be asymptotically normal with variance given by the squared standard error obtained from the reported 95% confidence intervals. The variables assumed to contribute to uncertainty were the relative risks and the prevalence of SSBs intake. All estimations were done in R software® with the pifpaf package [23].
For each age, sex, and region-specific stratum, the disease-specific PAFs and their uncertainty were multiplied by the total cases of death for that disease to estimate the absolute numbers and uncertainty of attributable deaths. Proportional mortality was calculated by summing the SSBs-attributable deaths across the outcomes of interest (diabetes mellitus, CVD, obesity-related cancer, and all-cause mortality), divided by the total number of deaths caused by these outcomes within the subgroup of interest [2].
Results
Population demographics are presented in Table 1. Mean SSBs intake among adults was 1.5 servings/day, with median of 0.87 servings/day and 16.9% of the population reporting zero SSBs intake (Table S3). SSBs intake varied substantially by sex, age, and region. Nationally, men had a higher consumption compared with women (1.7 servings/day vs. 1.3 servings/day, respectively). Adults 20–44 had highest consumption (1.9 servings/day), twice that of adults over 65. By region, the Center had the highest intake (1.6 servings/day), followed by the South (1.5 servings/day), and North (1.4 servings/day); with consistent age and sex patterns across regions.
National SSBs-attributable mortality
National mortality rates and the estimated mortality attributable to SSBs intake are presented in Tables 2 and 3. Overall 40,842 deaths/year were attributable to SSBs (95%CI 31,950–50,138) corresponding to 6.9% of all-cause mortality in the country. For cardiometabolic diseases and cancers, 37,094 deaths/year were attributable to SSBs (95%UI 21,240–51,045; Table S4), corresponding to 491 annual deaths per million adults (95%UI 281–675), which represent 19.3% of all deaths due to the included specific causes (95%UI 11.0–26.5). This rate was higher for men, 589 per million adults per year (95%UI 363–778), compared with 400 per million adults per year for women (95%UI 206–580). As expected, adults over 65 years of age had the highest absolute number of SSBs-attributable cause-specific deaths (men: 10,428 deaths (95%IUI 6,323–14,323); women: 10,116 deaths (95%UI 5,185–14,794)); while younger adults (age 45–64 for men and 20–44 for women) had the highest proportions of SSBs-attributable cause-specific deaths (men: 33.2%, 95%UI 20.4–42.5; women:29.6, 95%UI 17.2–39.2) and total mortality (men 12.0%, 95%UI 10.2–13.7; women 10.2%, 95%UI 8.4–12.2).
National SSBs-attributable mortality, by disease
Diabetes had the highest SSBs-attributable absolute mortality (23,433 deaths/year (95%UI 10 795–34 206), 310 annual deaths per million (95%UI 143–452)), corresponding to 35.6% of all deaths due to diabetes in Mexico (95%UI 16.4–52.0). SSBs were estimated to result in 13,517 CVD deaths/year (95%UI 10,377–16,630), equivalent to 179 deaths per million/year (95%UI 137–220), or 12.7% of these deaths (95%UI 9.7–15.6); and 144 obesity-mediated cancer deaths/year (95%UI 68–209), equivalent to 2 per million/year (95%UI 1–3), or 0.7% of these deaths (95%UI 0.3–1.0); detailed information is provided in Tables 2 and 3, and in Table S4.
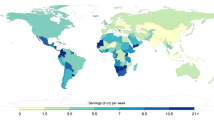
SSBs-attributable mortality by age, sex, and region
Mortality rates and the absolute mortality attributable to SSBs intake according to age, sex, and region are presented in Tables S4 and S5, while the proportion of SSBs-related mortality is presented in Table S6. In all regions, the proportion of SSBs-related cause-specific mortality exceeded 25% among both men and women aged 20–44. The region with the highest SSBs-attributable mortality rate was the South (593 annual deaths per million, 95%UI 309–842), followed by the Center (472, 95%UI 287–632) and North (410, 95%UI 239–568). These deaths correspond to a 22.8% (95%UI 11.9–32.4), 18% (95%UI 11.0–24.1), and 17.4% (95%UI 10.1–24.1) of all deaths due to these causes in these regions, respectively. Influenced by population size, the largest number of absolute SSBs-attributable deaths were found in the Center (16,254 deaths; 95%UI 9,881–21,737), followed by the South (12,684 deaths; 95%UI 6,606–18,013), and North (8,156 deaths; 95%UI 4,753–11,295). In all regions diabetes was the disease with the highest SSBs-attributable mortality exceeding 50% for both men and women aged 20–44, except for women in the South region (42%, 95%UI 21.0–58.9). There were no significant differences in all-cause mortality estimates across regions.
Discussion
In this study, we estimated the all-cause and cardiometabolic and obesity-related cancer deaths attributable to SSBs intake in Mexico in 2015, overall and stratified by age, sex, and region. We found that 6.9% of all-cause mortality among Mexican adults is attributable to SSBs consumption. In addition, when looking at cause-specific mortality, we found that 19.3% of cause-specific deaths were attributable to SSBs nationally, corresponding to more than 37,000 deaths annually, or more than 3000 deaths each month; the largest toll of death was linked to diabetes, since 35.6% of diabetes deaths were attributable to SSBs consumption. The proportion of SSBs-attributable cause-specific deaths was higher for men (22.0%) than women (16.5%), and for people living in the South (22.8%) than the Center (18.0%) or North (17.4%). Older men had the highest absolute rate of SSBs-related cause-specific mortality (2,818 annual deaths per million), while men 45–64 years and 20–44 years had highest proportional attributable mortality (33.2% and 32.7%, respectively). Overall, men age 45–64 years in the Center region were the most affected group (proportional attributable cause-specific mortality: 37.2%).
Over the last decade, SSBs intake has been established as an independent risk factor for weight gain and cardiometabolic diseases [4, 6, 20]. In addition, growing evidence indicates that such effects extend beyond change in weight, as SSBs intake is also independently associated with increases in visceral adiposity, systemic inflammation, blood triglyceride levels, and the development of hypertension and hyperuricemia; all supporting the observed direct risks on diabetes and CHD independent of change in BMI alone [24]. Importantly, SSBs intake is only one of many risk factors for cardiometabolic diseases and cancers, and it is not the largest single contributor [25]. Yet, in countries such as Mexico where SSBs intake is very high, and in population subgroups such as young adults who would otherwise have very low risk of such diseases, SSBs can contribute importantly to disease risk.
Globally, SSBs are estimated to contribute to 1.2% of cardiometabolic and obesity-related cancer deaths [2]. The present findings demonstrate how significant Mexico is as an outlier, due to its global-leading rates of SSBs intake, obesity, and diabetes. In addition, compared with prior findings utilizing earlier estimated etiologic effects [2], we identified a higher proportion (19.3% vs 12.1% reported by Singh et al.) of SSBs-attributable deaths due to these causes, suggesting that the toll of SSBs in Mexico and globally could have been previously underestimated. This difference is primarily attributable to the use of updated risk estimates, but also to some differences in data sources and methods. For example, Singh, et al. used aggregated population averages of SSBs intake adjusted for international comparability, while we used individual-level data directly from national registries and ENSANUT 2012, allowing us to capture more variability and the right tail of heavy consumers in Mexico. In addition, we incorporated the direct estimated links between SSBs and diabetes and CHD [4, 6], which are higher than purely BMI-mediated effects included in some previous studies [2]. Importantly, neither our work nor any of the prior estimates included potential risks of SSBs intake in youth, which could lead to underestimation of true long-term health burdens.
Our new regional analyses suggest that highest burdens of SSBs intake are in the South region, despite this region having a modestly lower SSBs intake compared with the Center region. Mexico has important differences among regions including geographic, political, and socioeconomic components that might influence both SSBs intake and the burden of cardiometabolic diseases and obesity-related cancers [26]. For example, states in the South consistently exhibit poorer health, education, and economic outcomes; [14] and higher overall burdens of cardiometabolic diseases [27]. While SSBs intake is not the sole contributor to the pandemic of obesity and cardiometabolic diseases in Mexico, reducing SSBs presents a unique opportunity to improve health and reduce health disparities observed across Mexico. In addition, our finding supports the need to target all generations, including older adults who have the highest absolute risk and younger generations who have the highest proportional benefit to be gained.
Several interventions to reduce obesity and cardiometabolic diseases are being studied and implemented in Mexico, including food labeling, taxation, and reformulation [28]. In 2014, the Mexican government implemented a 1 peso per liter tax on all non-alcoholic beverages with added sugar; [29] recent purchase data showed a 7.6% reduction in SSBs purchase nationally attributable to the tax [30]. Yet, national data on SSBs prices demonstrate heterogeneity in price changes; in the South, for example, the price increases following the SSBs tax were smaller compared with other regions, suggesting active industry efforts to minimize the pass-through of the tax in poorer, rural areas [31]. Despite this, a recent study estimated that relative obesity prevalence might decrease by 2.5% in the Mexican population over the next 10 years due to the 10% tax [32]. Recently, a call was made to increase the SSBs tax to 20%, to further increase its health benefits [33]. Reevaluating SSBs-related mortality with long-term data on post-tax SSBs consumption will be important to assess the potential impact of this intervention in the Mexican population.
While taxation has proved to be successful, other strategies to reduce SSB consumption have been implemented or are being considered under the National Strategy to Control and Prevent Overweight, Obesity and Diabetes [28]. Recent evidence suggests that SSBs reformulation could potentially be beneficial to the Mexican population, reducing obesity by 3.9% over 10 years if sugar content were to be decreased by 50% [34]. Other strategies that are being discussed is the implementation of a new food front of package labeling [35]. Nutritional guidelines in schools were implemented in Mexico in 2011 to limit the availability of sugary drinks and unhealthy foods while increasing the availability of water, fruits, and vegetables. Recent evidence suggests that children in schools complying with the guidelines tend to have healthier snacking; [36] yet, guidelines need to be updated and their implementation process has to be revised.
Our study has several strengths that must be mentioned. First, previous analyses used average consumption data and mortality to produce estimates and compare them globally; in our analysis, we used individual-level nationally-representative data on SSBs consumption and mortality, which allowed us to capture small nuances in the distribution of SSBs consumption and to calculate deaths attributable to SSBs consumption for key subgroups in the Mexican population. We coupled this rich individual-level data with a nonparametric method to estimate the population impact fraction using individual-level data, which reduced the likelihood of estimation problems due to the assumption of an underlying distribution [22]. Finally, the relative risks used for these analyses come from the most updated meta-analytic evidence, allowing us to update the association between SSBs and all the diseases considered; [4, 6, 17] also, due to their availability we were able to estimate the total effect of SSBs on CHD and diabetes, while previous studies only considered the BMI mediated pathway [2].
There are some limitations that must be addressed. First, our results might be underestimated given the underreporting of diabetes as the primary cause of death, found to be up to 35% in other countries [37]. However, people with diabetes often die of CVD causes which was included in our analyses, mitigating the possible underestimation of diabetes SSBs-related mortality. By using all-cause mortality estimates that are not subject to misclassification of specific causes, we captured 4,000 more deaths per year compared with cause-specific mortality; this difference could reflect the misclassification of specific causes into other categories, such as renal disease due to diabetes. Also, while the relative risks used for this study represent the best available information, they were mainly US-based estimates [4, 6, 17]. Evidence suggests that, Mexican-Americans have a higher risk of developing diabetes compared with other ethnic groups [38], which might indicate that the effect of SSBs on diabetes mortality could be higher. We used the relative risk of disease incidence as a proxy for the relative risk for mortality; this assumes that SSBs consumption does not affect survival, something that to our knowledge is not yet clear. If SSBs affect survival, it will likely do so by decreasing it, in which case our estimates will be conservative, since the RR for mortality would be higher than the RR for incidence. Lastly, SSBs intake data was obtained through the FFQ questionnaire in ENSANUT 2012; evidence comparing FFQ against other self-reporting dietary intake instruments and biologic markers consistently shows that FFQ underreports energy consumption, especially in obese adults [39]. Considering this evidence, by underestimating SSB intake, it is likely that we are underestimating the effect of SSB on mortality due to diabetes, CVD, and obesity related cancers.
Our findings provide updated evidence on the potential burden of disease due to SSBs consumption in Mexico. Mexico has declared an epidemiologic emergency on diabetes and obesity. Our results suggest that SSBs consumption could be largely driving this emergency. An integral strategy to reduce obesity and diabetes in Mexico is needed, in which the reduction of SSBs consumption has to be a fundamental piece.
Change history
15 March 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41366-024-01498-3
References
Malik VS, Popkin BM, Bray GA, Despres JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–64.
Singh GM, Micha R, Khatibzadeh S, Lim S, Ezzati M, Mozaffarian D, et al. Estimated global, regional, and national disease burdens related to sugar-sweetened beverage consumption in 2010. Circulation. 2015;132:639–66.
Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav. 2010;100:47–54.
Imamura F, O'Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. Brit Med J. 2015;351:h3576.
Micha R, Shulkin ML, Penalvo JL, Khatibzadeh S, Singh GM, Rao M, et al. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS ONE 2017;12:e0175149.
Xi B, Huang Y, Reilly KH, Li S, Zheng R, Barrio-Lopez MT, et al. Sugar-sweetened beverages and risk of hypertension and CVD: a dose-response meta-analysis. Br J Nutr. 2015;113:709–17.
Institute for Health Metrics and Evaluation. Global burden of diseases, risk factors, and injuries 2010 study. USA: University of Washington; 2010.
WHO. Guideline: sugars intake for adults and children. Geneva: WHO; 2015.
Euromonitor International. Euromonitor international’s passport global market. UK: Euromonitor International; 2012.
Singh GM, Micha R, Khatibzadeh S, Shi P, Lim S, Andrews KG, et al. Global, regional, and national consumption of sugar-sweetened beverages, fruit juices, and milk: a systematic assessment of beverage intake in 187 countries. PLoS ONE 2015;10:e0124845.
Sanchez-Pimienta TG, Batis C, Lutter CK, Rivera JA. Sugar-sweetened beverages are the main sources of added sugar intake in the mexican population. J Nutr. 2016;146:1888S–96S.
Aburto TC, Pedraza LS, Sanchez-Pimienta TG, Batis C, Rivera JA. Discretionary foods have a high contribution and fruit, vegetables, and legumes have a low contribution to the total energy intake of the Mexican population. J Nutr. 2016;146:1881S–7S.
Rojas-Martinez R, Basto-Abreu A, Aguilar-Salinas CA, Zarate-Rojas E, Villalpando S, Barrientos-Gutierrez T. Prevalence of previously diagnosed diabetes mellitus in Mexico. Salud Publica Mex. 2018;60:224–32.
Secretaria de Salud. Dirección General de Evaluación del Demespeño Informe sobre la Salud de los Mexicanos. Mexico: Secretaria de Salud; 2015.
Romero-Martinez M, Shamah-Levi T, Franco-Nuñez A, Villalpando-Hernandez S, Cuevas-Nasu L, Gutierrez JP, et al. National Health and Nutrition Survey 2012 design and coverage. Salud Pública Mex. 2013;55:s332–s40.
Geografía INdEy. Estadística de defunciones generales. Síntesis metodológica. 2014.
Malik VS, Li Y, Pan A, De Koning L, Schernhammer E, Willett WC, et al. Long-term consumption of sugar-sweetened and artificially sweetened beverages and risk of mortality in US adults. Circulation. 2019;139:2113–25.
Khatibzadeh S, Micha R, Afshin A, Rao M, Yakoob MY, Dariush M. Abstract: Major dietary risk factors for chronic diseases: a systematic review of the current evidence for causal effects and effect sizes. Circulation. 2012;125(Suppl10):AP060.
Luger M, Lafontan M, Bes-Rastrollo M, Winzer E, Yumuk V, Farpour-Lambert N. Sugar-sweetened beverages and weight gain in children and adults: a systematic review from 2013 to 2015 and a comparison with previous studies. Obesity Facts. 2017;10:674–93.
Singh GM, Danaei G, Farzadfar F, Stevens GA, Woodward M, Wormser D, et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS ONE 2013;8:e65174.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–78.
Taguri M, Matsuyama Y, Ohashi Y, Harada A, Ueshima H. Doubly robust estimation of the generalized impact fraction. Biostatistics. 2012;13:455–67.
Zepeda-Tello R, Camacho-Garcia-Formenti D. Pifpaf: potential impact fraction and population attributable fraction for cross-sectional data. CRAN R Package Documentation. 2017. https://rdrr.io/cran/pifpaf/.
Simin Liu JoAnnE, Manson JulieE, Buring MeirJ, Stampfer WalterC, Willett, Ridker PM. Relation between a diet with a high glycemic load and plasma concentrations of high-sensitivity C-reactive protein in middle-aged women. Am J Clin Nutr. 2002;75:492–8.
Collaboration TGBoMRFfCD. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2:634–47.
López-Olmedo N, Popkin BM, Taillie LS. The socioeconomic disparities in intakes and purchases of less-healthy foods and beverages have changed over time in urban Mexico. J Nutr. 2018;148:109–16.
Gómez-Dantés H, Fullman N, Lamadrid-Figueroa H, Cahuana-Hurtado L, Darney B, Avila-Burgos L, et al. Dissonant health transition in the states of Mexico, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2016;388:2386–402.
Salud Sd. Estrategia Nacional para la Prevención y el Control del Sobrepeso, la Obesidad y la Diabetes. Mexico City: Salud Sd; 2013.
Cámara de Diputados del Honorable Congreso de la Union. Ley del impuesto especial sobre producción y servicios. Mexico: Diario Oficial de la Federación; 2016.
Colchero MA, Rivera-Dommarco J, Popkin BM, Ng SW. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Affairs.2017;36:564–71.
Colchero MA, Zavala JA, Batis C, Shamah-Levy T, Rivera-Dommarco JA. Changes in prices of taxed sugar-sweetened beverages and nonessential energy dense food in rural and semi-rural areas in Mexico. Salud Publica Mex. 2017;59:137–46.
Barrientos-Gutierrez T, Zepeda-Tello R, Rodrigues ER, Colchero MA, Rojas-Martinez R, Lazcano-Ponce E, et al. Expected population weight and diabetes impact of the 1-peso-per-litre tax to sugar sweetened beverages in Mexico. PLoS ONE 2017;12:e0176336.
Barrientos-Gutiérrez T, Colchero MA, Sánchez-Romero LM, Batis C, Rivera-Dommarco J. Posicionamiento sobre los impuestos a alimentos no básicos densamente energéticos y bebidas azucaradas. Salud Pública de México; 2018. vol. 60, p. 586.
Basto-Abreu A, Braverman-Bronstein A, Camacho-Garcia-Formenti D, Zepeda-Tello R, Popkin BM, Rivera-Dommarco J, et al. Expected changes in obesity after reformulation to reduce added sugars in beverages: a modeling study. PLoS Med. 2018;15:e1002664.
Kaufer-Horwitz M, Tolentino-Mayo L, Jáuregui A, Sánchez-Bazán K, Bourges H, Martínez S, et al. Sistema de etiquetado frontal de alimentos y bebidas para México: una estrategia para la toma de decisiones saludables. Salud Pública de México. 2018;60:479.
Pérez-Ferrer C, Barrientos-Gutierrez T, Rivera-Dommarco JA, Prado-Galbarro FJ, Jiménez-Aguilar A, Morales-Ruán C. et al. Compliance with nutrition standards in Mexican schools and their effectiveness: a repeated cross-sectional study. BMC Public Health. 2018;18:1411.
Murray CJL, Dias RH, Kulkarni SC, Lozano R, Stevens GA, Ezzati M. Improving the comparability of diabetes mortality statistics in the United States and Mexico. Diabetes Care. 2008;31:451–8.
Hu H, Huff CD, Yamamura Y, Wu X, Strom SS. The relationship between native american ancestry, body mass index and diabetes risk among Mexican-Americans. PLoS ONE 2015;10:e0141260.
Yikyung Park KWD, Kipnis V, Thompson FE, Potischman N, Schoeller DA, Baer DJ, et al. Comparison of self-reported dietary intakes from the automated self-administered 24-h recall, 4-d food records, and food-frequency questionnaires against recovery biomarkers. Am J Clin Nutr. 2018;107:80–93.
Acknowledgements
This paper was funded by the Bloomberg Philanthropies and supported by a grant from the Bill & Melinda Gates Foundation (PI Mozaffarian), and from the National Heart, Lung, and Blood Institute (grant number R00HL124321). Tonatiuh Barrientos was supported by the Lown Scholars program from Harvard University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Braverman-Bronstein, A., Camacho-García-Formentí, D., Zepeda-Tello, R. et al. Mortality attributable to sugar sweetened beverages consumption in Mexico: an update. Int J Obes 44, 1341–1349 (2020). https://doi.org/10.1038/s41366-019-0506-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0506-x
This article is cited by
-
Modelling the impact of sodium intake on cardiovascular disease mortality in Mexico
BMC Public Health (2023)
-
How Could Taxes on Sugary Drinks and Foods Help Reduce the Burden Of Type 2 Diabetes?
Current Diabetes Reports (2023)
-
Soft drink and non-caloric soft drink intake and their association with blood pressure: the Health Workers Cohort Study
Nutrition Journal (2022)
-
The role of sugar-sweetened beverages in the global epidemics of obesity and chronic diseases
Nature Reviews Endocrinology (2022)
-
Associations of psychosocial factors, knowledge, attitudes and practices with hospitalizations in internal medicine divisions in different population groups in Israel
International Journal for Equity in Health (2021)