Abstract
Background
Prenatal exposure to fine particulate matter (PM2.5) assessed through its mass concentration has been associated with foetal growth restriction in studies based on outdoor levels. Oxidative potential of PM2.5 (OP) is an emerging metric a priori relevant to mechanisms of action of PM on health, with very limited evidence to indicate its role on birth outcomes.
Objectives
We investigated the association of OP with birth outcomes and compared it with that of PM2.5 mass concentration.
Methods
405 pregnant women from SEPAGES cohort (Grenoble area) carried PM2.5 personal dosimeters for one or two one-week periods. OP was measured using dithiothreitol (DTT) and ascorbic acid (AA) assays from the collected filters. Associations of each exposure metric with offspring weight, height, and head circumference at birth were estimated adjusting for potential confounders.
Results
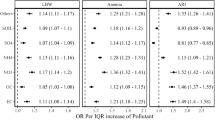
The correlation between PM2.5 mass concentration and \(OP_v^{DTT}\) was 0.7. An interquartile range increase in .. was associated with reduced weight (adjusted change, −64 g, −166 to −11, p = 0.02) and height (−4 mm, −6 to −1, p = 0.01) at birth. PM2.5 mass concentration showed similar associations with weight (−53 g, −99 to −8, p = 0.02) and height (−2 mm, −5 to 0, p = 0.05). In birth height models mutually adjusted for the two exposure metrics, the association with \(OP_v^{DTT}\) was less attenuated than that with mass concentration, while for weight both effect sizes attenuated similarly. There was no clear evidence of associations with head circumference for any metric, nor for \(OP_v^{AA}\) with any growth parameter.
Impact
PM2.5 pregnancy exposure assessed from personal dosimeters was associated with altered foetal growth. Personal OP exposure was associated with foetal growth restrictions, specifically decreased weight and height at birth, possibly to a larger extent than PM2.5 mass concentration alone. These results support OP assessed from DTT as being a health-relevant metric. Larger scale cohort studies are recommended to support our findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The readers may contact the corresponding authors for data requests. General information on the SEPAGES cohort is made publicly available at https://cohorte-sepages.fr/en.
References
Yang Y, Ruan Z, Wang X, Yang Y, Mason TG, Lin H, et al. Short-term and long-term exposures to fine particulate matter constituents and health: a systematic review and meta-analysis. Environ Pollut. 2019;247:874–82.
Sun X, Luo X, Zhao C, Zhang B, Tao J, Yang Z, et al. The associations between birth weight and exposure to fine particulate matter (PM2.5) and its chemical constituents during pregnancy: a meta-analysis. Environ Pollut. 2016;211:38–47.
Pedersen M, Gehring U, Beelen R, Wang M, Giorgis-Allemand L, Andersen A-MN, et al. Elemental constituents of particulate matter and newborn’s size in eight European cohorts. Environ Health Perspect. 2016;124:141–50.
Saffari A, Daher N, Shafer MM, Schauer JJ, Sioutas C. Global perspective on the oxidative potential of airborne particulate matter: a synthesis of research findings. Environ Sci Technol. 2014;48:7576–83.
Bates JT, Fang T, Verma V, Zeng L, Weber RJ, Tolbert PE, et al. Review of acellular assays of ambient particulate matter oxidative potential: methods and relationships with composition, sources, and health effects. Environ Sci Technol. 2019;53:4003–19.
Shi T, Knaapen AM, Begerow J, Birmili W, Borm PJA, Schins RPF. Temporal variation of hydroxyl radical generation and 8-hydroxy-2’-deoxyguanosine formation by coarse and fine particulate matter. Occup Environ Med. 2003;60:315–21.
Nel A. ATMOSPHERE: enhanced: air pollution-related illness: effects of particles. Science. 2005;308:804–6.
Kelly FJ, Mudway IS. Protein oxidation at the air-lung interface. Amino Acids. 2003;25:375–96.
Mudway IS, Stenfors N, Duggan ST, Roxborough H, Zielinski H, Marklund SL, et al. An in vitro and in vivo investigation of the effects of diesel exhaust on human airway lining fluid antioxidants. Arch Biochem Biophys. 2004;423:200–12.
Landreman AP, Shafer MM, Hemming JC, Hannigan MP, Schauer JJ. A Macrophage-Based Method for the Assessment of the Reactive Oxygen Species (ROS) Activity of Atmospheric Particulate Matter (PM) and Application to Routine (Daily-24 h) Aerosol Monitoring Studies. Aerosol Sci Technol. 2008;42:946–57.
Liu L, Urch B, Szyszkowicz M, Evans G, Speck M, Van Huang A, et al. Metals and oxidative potential in urban particulate matter influence systemic inflammatory and neural biomarkers: A controlled exposure study. Environ Int. 2018;121:1331–40.
Li J, Chen H, Li X, Wang M, Zhang X, Cao J, et al. Differing toxicity of ambient particulate matter (PM) in global cities. Atmos Environ. 2019;212:305–15.
Bates JT, Weber RJ, Abrams J, Verma V, Fang T, Klein M, et al. Reactive oxygen species generation linked to sources of atmospheric particulate matter and cardiorespiratory effects. Environ Sci Technol. 2015;49:13605–12.
Weichenthal S, Crouse DL, Pinault L, Godri-Pollitt K, Lavigne E, Evans G, et al. Oxidative burden of fine particulate air pollution and risk of cause-specific mortality in the Canadian Census Health and Environment Cohort (CanCHEC). Environ Res. 2016;146:92–99.
Zhang X, Staimer N, Tjoa T, Gillen DL, Schauer JJ, Shafer MM, et al. Associations between microvascular function and short-term exposure to traffic-related air pollution and particulate matter oxidative potential. Environ Health. 2016;15:81.
Weichenthal S, Lavigne E, Evans G, Pollitt K, Burnett RT. Ambient PM2.5 and risk of emergency room visits for myocardial infarction: impact of regional PM2.5 oxidative potential: a case-crossover study. Environ Health. 2016;15:46.
Abrams JY, Weber RJ, Klein M, Sarnat SE, Chang HH, Strickland MJ, et al. Associations between ambient fine particulate oxidative potential and cardiorespiratory emergency department visits. Environ Health Perspect. 2017;125:107008.
Gauvin S, Reungoat P, Cassadou S, Déchenaux J, Momas I, Just J, et al. Contribution of indoor and outdoor environments to PM2.5 personal exposure of children—VESTA study. Sci Total Environ. 2002;297:175–81.
Brehmer C, Norris C, Barkjohn KK, Bergin MH, Zhang J, Cui X, et al. The impact of household air cleaners on the oxidative potential of PM2.5 and the role of metals and sources associated with indoor and outdoor exposure. Environ Res. 2020;181:108919.
Chen X-C, Chuang H-C, Ward TJ, Sarkar C, Webster C, Cao J, et al. Toxicological effects of personal exposure to fine particles in adult residents of Hong Kong. Environ Pollut. 2021;275:116633.
George S, Chua ML, ZheWei DZ, Das R, Bijin VA, Connolly JE, et al. Personal level exposure and hazard potential of particulate matter during haze and non-haze periods in Singapore. Chemosphere. 2020;243:125401.
He L, Norris C, Cui X, Li Z, Barkjohn KK, Brehmer C, et al. Personal exposure to PM 2.5 oxidative potential in association with pulmonary pathophysiologic outcomes in children with asthma. Environ Sci Technol. 2021;55:3101–11.
Shah PS, Balkhair T. Air pollution and birth outcomes: a systematic review. Environ Int. 2011;37:498–516.
Tjoa ML, Cindrova-Davies T, Spasic-Boskovic O, Bianchi DW, Burton GJ. Trophoblastic oxidative stress and the release of cell-free feto-placental DNA. Am J Pathol. 2006;169:400–4.
Huang X, Liu Z, Liu J, Hu B, Wen T, Tang G et al. Chemical characterization and synergetic source apportionment of PM2.5 at multiple sites in the Beijing–Tianjin–Hebei region, China. Atmos Chem Phys Discuss. 2017;17:1–34.
Rashid CS, Bansal A, Simmons RA. Oxidative stress, intrauterine growth restriction, and developmental programming of type 2 diabetes. Physiology. 2018;33:348–59.
Saenen ND, Martens DS, Neven KY, Alfano R, Bové H, Janssen BG, et al. Air pollution-induced placental alterations: an interplay of oxidative stress, epigenetics, and the aging phenotype? Clin Epigenet. 2019;11:124.
Duhig K, Chappell LC, Shennan AH. Oxidative stress in pregnancy and reproduction. Obstet Med. 2016;9:113–6.
Lavigne É, Burnett RT, Stieb DM, Evans GJ, Godri Pollitt KJ, Chen H, et al. Fine particulate air pollution and adverse birth outcomes: effect modification by regional nonvolatile oxidative potential. Environ Health Perspect. 2018;126:077012.
Mostofsky E, Schwartz J, Coull BA, Koutrakis P, Wellenius GA, Suh HH, et al. Modeling the association between particle constituents of air pollution and health outcomes. Am J Epidemiol. 2012;176:317–26.
Borlaza LJS, Weber S, Jaffrezo J-L, Houdier S, Slama R, Rieux C, et al. Disparities in particulate matter (PM<sub>10</sub>) origins and oxidative potential at a city scale (Grenoble, France) – Part 2: Sources of PM<sub>10</sub> oxidative potential using multiple linear regression analysis and the predictive applicability of multilayer perceptron neural network analysis. Atmos Chem Phys. 2021;21:9719–39.
Borlaza LJS, Weber S, Uzu G, Jacob V, Cañete T, Micallef S, et al. Disparities in particulate matter (PM<sub>10</sub>) origins and oxidative potential at a city scale (Grenoble, France) – Part 1: Source apportionment at three neighbouring sites. Atmos Chem Phys. 2021;21:5415–37.
INSEE. Naissances de 2014 à 2020. Institut national de la statistique et des études économiques: France https://www.insee.fr/fr/statistiques/1893255 (accessed 22 Sep 2020).
Calas A, Uzu G, Martins JMF, Voisin D, Spadini L, Lacroix T, et al. The importance of simulated lung fluid (SLF) extractions for a more relevant evaluation of the oxidative potential of particulate matter. Sci Rep. 2017;7:11617.
Cho AK, Sioutas C, Miguel AH, Kumagai Y, Schmitz DA, Singh M, et al. Redox activity of airborne particulate matter at different sites in the Los Angeles Basin. Environ Res. 2005;99:40–47.
van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16:219–42.
Pedersen M, Giorgis-Allemand L, Bernard C, Aguilera I, Andersen A-MN, Ballester F, et al. Ambient air pollution and low birthweight: a European cohort study (ESCAPE). Lancet Respiratory Med. 2013;1:695–704.
Ouidir M, Seyve E, Rivière E, Bernard J, Cheminat M, Cortinovis J, et al. Maternal ambient exposure to atmospheric pollutants during pregnancy and offspring term birth weight in the nationwide ELFE cohort. IJERPH. 2021;18:5806.
Bell ML, Ebisu K, Belanger K. Ambient air pollution and low birth weight in Connecticut and Massachusetts. Environ Health Perspect. 2007;115:1118–24.
Fossati S, Valvi D, Martinez D, Cirach M, Estarlich M, Fernández-Somoano A, et al. Prenatal air pollution exposure and growth and cardio-metabolic risk in preschoolers. Environ Int. 2020;138:105619.
Fu L, Chen Y, Yang X, Yang Z, Liu S, Pei L, et al. The associations of air pollution exposure during pregnancy with fetal growth and anthropometric measurements at birth: a systematic review and meta-analysis. Environ Sci Pollut Res. 2019;26:20137–47.
Jedrychowski W, Bendkowska I, Flak E, Penar A, Jacek R, Kaim I, et al. Estimated risk for altered fetal growth resulting from exposure to fine particles during pregnancy: an epidemiologic prospective cohort study in Poland. Environ Health Perspect. 2004;112:1398–402.
U.S. EPA. Air Quality Criteria for Particulate Matter. Fourth External Review Draft. U.S. Environmental Protection Agency: Washington D.C., 2003.
Kannan S, Misra DP, Dvonch JT, Krishnakumar A. Exposures to airborne particulate matter and adverse perinatal outcomes: a biologically plausible mechanistic framework for exploring potential effect modification by nutrition. Environ Health Perspect. 2006;114:1636–42.
Pizzino G, Irrera N, Cucinotta M, Pallio G, Mannino F, Arcoraci V, et al. Oxidative stress: harms and benefits for human health. Oxid Med Cell Longev. 2017;2017:1–13.
Kim Y, Hong Y, Lee K, Park H, Park E, Moon H, et al. Oxidative stress in pregnant women and birth weight reduction. Reprod Toxicol. 2005;19:487–92.
Yang A, Janssen NAH, Brunekreef B, Cassee FR, Hoek G, Gehring U. Children’s respiratory health and oxidative potential of PM 2.5: the PIAMA birth cohort study. Occup Environ Med. 2016;73:154–60.
Lyon-Caen S, Siroux V, Lepeule J, Lorimier P, Hainaut P, Mossuz P, et al. Deciphering the impact of early-life exposures to highly variable environmental factors on foetal and child health: design of SEPAGES couple-child cohort. IJERPH. 2019;16:3888.
Rothman KJ, Gallacher JE, Hatch EE. Why representativeness should be avoided. Int J Epidemiol. 2013;42:1012–4.
Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7:147–77.
Acknowledgements
The SEPAGES cohort study group includes: E. Eyriey, A. Licinia, A. Vellement (Groupe Hospitalier Mutualiste, Grenoble), I. Pin, P. Hofmann, E. Hullo, C. Llerena (Grenoble University Hospital, La Tronche), X. Morin (Clinique des Cèdres, Echirolles), A. Morlot (Clinique Belledonne, Saint-Martin d’Hères), J. Lepeule, S. Lyon-Caen, C. Philippat, J. Quentin, V. Siroux, R. Slama (Inserm, CNRS, University Grenoble Alpes IAB research center). We thank Mrs. A. Benlakhryfa, Mrs. L. Borges, Mr. Y. Gioria, clinical research assistants; Mrs. J. Giraud, Mrs. M. Marceau, Mrs. M-P. Martin, nurses; Mrs. E. Charvet, Mrs A. Putod, midwives; Mrs. M. Graca, Mrs. K.Gridel, Mrs. C. Pelini, Mrs Maïlys Barbagallo fieldworkers; Mrs. A.Bossant, K. Guichardet, J-T Iltis A. Levanic, C. Martel, E. Quinteiro, S.Raffin neuropsychologists; the staff from Grenoble Center for Clinical Investigation (CIC): Prof. J.-L. Cracowski, Dr. C. Cracowski, Dr. E. Hodaj, Mrs. D. Abry, Mr. N. Gonnet and Mrs. A. Tournier. A warm thank you also to Dr. M. Althuser, Mr. S. Althuser, Dr. F. Camus-Chauvet, Mr. P. Dusonchet, Mrs. S. Dusonchet, Dr. L. Emery, Mrs. P.Fabbrizio, Prof. P. Hoffmann, Dr. D. Marchal André, Dr. X. Morin, Dr. E.Opoix, Dr. L. Pacteau, Dr. P. Rivoire, Mrs. A. Royannais, Dr. C.Tomasella, Dr. T. Tomasella, Dr. D. Tournadre, Mr. P. Viossat, Mrs. E.Volpi, Mrs. S. Rey, Dr. E. Warembourg and clinicians from Grenoble University Hospital for their support in the recruitment of the study volunteers. We also thank Mrs. A. Buchet, Mrs. SF. Caraby, Dr. J-N.Canonica, Mrs. J. Dujourdil, Dr. E. Eyriey, Prof. P. Hoffmann, Mrs. M.Jeannin, Mrs. A. Licina, Dr. X. Morin, Mrs. A. Nicolas, and all midwives from the four maternity wards of Grenoble urban areas. SEPAGES data are stored thanks to Inserm RE-CO-NAI platform funded by Commissariat Général à l’Investissement, with the implication of Sophiede Visme (Inserm DSI). Many thanks to Dr. M.A. Charles, RE-CO-NAI coordinator, for her support. Finally, and importantly, we would like to express our sincere thanks to participants of the SEPAGES study. The SEPAGES cohort was supported by the European Research Council (N°311765-E-DOHaD), the European Community’s Seventh Framework Programme (FP7/2007-206 - N°308333-892 HELIX), the European Union’s Horizon 2020 research and innovation program (N° 874583 ATHLETE Project, N°825712 OBERON Project), the French Research Agency - ANR (PAPER project ANR-12-PDOC-0029-01, SHALCOH project ANR-14-CE21-0007, ANR-15-IDEX-02 and ANR-15-IDEX5, GUMME project ANR-18-CE36-005, ETAPE project ANR - EDeN project ANR -19-CE36-0003-01), the French Agency for Food, Environmental and Occupational Health & Safety - ANSES (CNAP project EST-2016-121, PENDORE project EST-2016-121, HyPAxE project EST-2019/1/039), the Plan Cancer (Canc’Air project), the French Cancer Research Foundation Association de Recherche sur le Cancer – ARC, the French Endowment Fund AGIR for chronic diseases – APMC (projects PRENAPAR and LCI-FOT), the French Endowment Fund for Respiratory Health, the French Fund – Fondation de France (CLIMATHES – 00081169, SEPAGES 5 - 00099903).We acknowledge the support of ANSES, Inserm and AGIR pour les maladies chroniques, for SEPAGES feasibility study. The support of “SCUSI 2017” Région Auvergne-Rhône-Alpes programme is also acknowledged. OP analysis were supported by the MobilAir program (ANR-15-IDEX-02) and ANR Get OP Stand OP program (ANR-19-CE34-0002-01), and were analyzed at the Air-O-Sol facility at IGE, made possible with the funding of some laboratory equipment by the Labex OSUG@2020 (ANR10 LABX56). The postdoc of Lucille Joanna Borlaza is funded by the Predict’air project (grant Fondation UGA-UGA 2022-16 and grant PR-PRE-2021 FUGA-Fondation Air Liquide).
Author information
Authors and Affiliations
Consortia
Contributions
GU, JLJ, and RS designed the study and the statistical analysis protocol. GU developed the OP assays for the group. LJSB, AM, and SW processed the data. SLC, JL, and AB handled all data management of the SEPAGES cohort. LJSB wrote the paper. GU, JLJ, and RS revised the original draft. All authors reviewed and edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Borlaza, L.J.S., Uzu, G., Ouidir, M. et al. Personal exposure to PM2.5 oxidative potential and its association to birth outcomes. J Expo Sci Environ Epidemiol 33, 416–426 (2023). https://doi.org/10.1038/s41370-022-00487-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-022-00487-w
Keywords
This article is cited by
-
In-utero exposure to multiple air pollutants and childhood undernutrition in India
Journal of Exposure Science & Environmental Epidemiology (2023)