Abstract
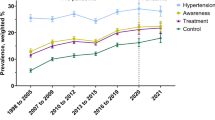
Effective control of hypertension at the population level is a global public health challenge. This study shows how improving population coverages at different hypertension care cascade levels could impact population-level hypertension management. We developed an analytical framework and a companion Excel model of multi-level hypertension care cascade entailing awareness, treatment, and control. The model estimates the prevalence of uncontrolled hypertension for different level of population coverages at certain cascade levels. We applied the model to data from Bangladesh and reported prevalence estimates associated with coverage interventions at different cascade levels. The model estimated that if 50% of the unaware hypertensive patients became aware of their hypertensive condition, the prevalence of uncontrolled hypertension would decrease by 1.8 and 1.3 percentage points (8.2% and 5.8% relative reduction), respectively, for constant and variable rates in the status quo setting. When 50% of the aware, but untreated individuals received treatment, the prevalence would decrease by around 0.7 percentage points (3.3% relative reduction). A 50% decrease in the share of treated individuals who did not have hypertension under control, would result in decreasing the prevalence by 2.8 percentage points (12.7% relative reduction). By providing an analytical tool that demonstrates the probable impact of population coverage interventions at certain hypertension care cascade levels, our study endows public health practitioners with vital information to identify gaps and design effective policies for hypertension management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organization. Hypertension – fact sheet. 2019. https://www.who.int/news-room/fact-sheets/detail/hypertension. Accessed 4 Dec 2020.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Centers for Disease Control and Prevention. Underlying cause of death, 1999–2018. CDC WONDER Online Database. Atlanta, GA: Centers for Disease Control and Prevention; 2018. http://wonder.cdc.gov/ucd-icd10.html. Accessed 11 Dec 2020.
Arima H, Barzi F, Chalmers J. Mortality patterns in hypertension. J Hypertens. 2011;29:S3–7.
United Nations Development Programme. Sustainable development goals – goal 3: good health and well-being. 2020. https://www.undp.org/content/undp/en/home/sustainable-development-goals/goal-3-good-health-and-well-being.html#targets. Accessed 4 Dec 2020.
World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: WHO; 2013. https://www.who.int/nmh/publications/ncd-action-plan/en/. Accessed 29 Dec 2020.
Akl C, Akik C, Ghattas H, Obermeyer CM. The cascade of care in managing hypertension in the Arab world: a systematic assessment of the evidence on awareness, treatment and control. BMC Public Health. 2020;20:1–3.
Geldsetzer P, Manne-Goehler J, Marcus ME, Ebert C, Zhumadilov Z, Wesseh CS, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1· 1 million adults. Lancet. 2019;394:652–62.
Foti K, Wang D, Appel LJ, Selvin E. Hypertension awareness, treatment, and control in US adults: trends in the hypertension control cascade by population subgroup (National Health and Nutrition Examination Survey, 1999–2016). Am J Epidemiol. 2019;188:2165–74.
Mishra SR, Ghimire S, Shrestha N, Shrestha A, Virani SS. Socio-economic inequalities in hypertension burden and cascade of services: nationwide cross-sectional study in Nepal. J Hum Hypertens. 2019;33:613–25.
Berry KM, Parker WA, Mchiza ZJ, Sewpaul R, Labadarios D, Rosen S, et al. Quantifying unmet need for hypertension care in South Africa through a care cascade: evidence from the SANHANES, 2011–2012. BMJ. Glob Health. 2017;2:e000348.
Wozniak G, Khan T, Gillespie C, Sifuentes L, Hasan O, Ritchey M, et al. Hypertension control cascade: a framework to improve hypertension awareness, treatment, and control. J Clin Hypertens. 2016;18:232–9.
Chowdhury MZ, Rahman M, Akter T, Akhter T, Ahmed A, Shovon MA, et al. Hypertension prevalence and its trend in Bangladesh: evidence from a systematic review and meta-analysis. Clin Hypertens. 2020;26:1–9.
World Bank. Hypertension and type-2 diabetes in Bangladesh: continuum of care assessment and opportunities for action. 2019. http://documents1.worldbank.org/curated/en/914751528271293762/pdf/Hypertension-and-Type-2-Diabetes-in-Bangladesh-Continuum-of-Care-Assessment-and-Opportunities-for-Action.pdf. Accessed 29 December 2020.
World Health Organization - Country Office for Bangladesh. National STEPS survey for non-communicable diseases risk factors in Bangladesh. 2018. https://apps.who.int/iris/handle/10665/332886. Accessed 4 December 2020.
Riaz BK, Islam MZ, Islam AS, Zaman MM, Hossain MA, Rahman MM, et al. Risk factors for non-communicable diseases in Bangladesh: findings of the population-based cross-sectional national survey 2018. BMJ Open. 2020;10:e041334.
United Nations. World population prospects 2019. Department of Economic and Social Affairs, Population Division. New York: UN; 2019. Accessed 1 Sep 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Datta, B.K., Ansa, B.E. & Husain, M.J. An analytical model of population level uncontrolled hypertension management: a care cascade approach. J Hum Hypertens 36, 726–731 (2022). https://doi.org/10.1038/s41371-021-00572-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00572-x
This article is cited by
-
The hypertension cascade of care in the midst of conflict: the case of the Gaza Strip
Journal of Human Hypertension (2022)