Abstract
Objective
To evaluate prevalence and risk factors of moderate-severe Bronchopulmonary dysplasia (BPD)/Death in extremely low gestation age neonates (ELGANs).
Study design
Study of 266 ELGANs born at gestational age (GA) ≤ 28 weeks (w). Primary Outcome measure—composite outcome of moderate-severe BPD/Death using the National Institute of Child Health and Human Development NICHD’s (2001) BPD definition.
Result
Cohort’s mean GA and birth-weight (BW) were 25.3 ± 1.4w and 724 ± 14 g respectively with an overall mortality of 19% and moderate-severe BPD of 67%. Prevalence of moderate-severe BPD/death decreased significantly with increasing GA (86–93%) at 23–24 w; to <60% at 27–28w (OR 0.63; 95% CI; 0.52–0.77). On univariate analysis, other risk factors included BW(OR 1.005; 95% CI; 1.003–1.007), Sepsis (OR 2.9; 95% CI, 1.3–6.4), PDA needing treatment (OR 2.2; 95% CI, 1.3–3.9); air leaks (OR 2.7; 95% CI; 1.02–7.3) FiO2 requirement >25%(OR 1.06; 95% CI; 1.01–1.11); and mechanical ventilation(MV) on Day7 (OR5.5; 95% CI; 2.8–10.8). Only need for Day7 MV was independently predictive of composite outcome (OR1.97; 95% CI; 1.3–3.1).
Conclusion
Risk factor identification will enable initiatives to implement lung protective strategies and develop prospective models for BPD prediction and prognostication.
Similar content being viewed by others
Introduction
Advances in modern perinatal and neonatal intensive care have improved the survival of extremely low gestational age neonates (ELGANs). However, the rates of bronchopulmonary dysplasia (BPD) have remained the same or even increased with increasing survival of ELGANs [1].
In the United States 10,000–15,000 new cases of BPD are reported every year [2, 3] with an incidence of 40–45% in surviving ELGANs over the last few decades [4].
BPD, a major neonatal morbidity, has short- and long-term sequelae including higher mortality, need for prolonged hospitalizations, pulmonary hypertension, asthma and chronic obstructive pulmonary disease as well as neurodevelopmental impairment [5,6,7,8]. It requires multidisciplinary care with increased health care costs and resource utilizations for families and health care systems [9, 10]. One probable reason for persistently high BPD rates in ELGANs is the pathogenesis of “New BPD”, a concept elaborated on by Jobe and Bancalari. They postulated that “New BPD” is a syndrome of inflammatory processes superimposed on a developmentally immature lung with variability in injury and repair and arrest in lung development after extremely preterm birth [11].
Furthermore, infections and inflammation, patent ductus arteriosus (PDA), pulmonary air leaks, ventilator and oxygen induced lung injury have been implicated in the “New BPD” [12,13,14].
As mortality and BPD may be competing outcomes in ELGANs, authors often define composite outcomes of BPD or death [15,16,17]. Data from South East Asia are limited, not recent and did not stratify the severity of BPD [18, 19]. Our neonatal network benchmarks its qualitative and quantitative data with the Vermont oxford data set. Regionally we have regular perinatal collaborations and meetings, with the aim of using evidence-based approaches and quality improvement initiatives for implementing potentially best practices. However, the regional studies reporting BPD outcomes are limited in number and have varied outcomes. In a recent review from the Ministry of Health, Malaysia the BPD rate in extremely low birth weight (ELBW)s was 38.5% but was accompanied by a high mortality rate of 51% in 2015 [20]. Data from the mid-2000s from the four Asian countries in the Asian Network on Maternal and New born Health network showed BPD rates to be only 26% but the denominator included all very low birth weight (VLBW)s and not the high risk ELGAN group unlike our data [21]. Thus, while we recognize the importance of comparing with Asian cohorts, the great heterogeneity in the population studied, the definitions of outcomes and differences between centers, makes this task challenging. Comparison of current data with potentially better practices from international networks will enable future quality improvement measures for BPD reduction. The primary aim of our study was to evaluate the prevalence of a composite outcome of moderate-severe BPD/death and to assess associated risk factors in a recent ELGAN cohort of Asian infants.
Methods
The study was conducted at KK Women’s and Children’s Hospital (KKH), Singapore’s largest tertiary perinatal referral center, which annually manages 12,000 live births including 200 VLBW infants, of which 90 are ELBW. The study period was from January 2012– December 2015 and included ELGANs born at gestational age (GA) ≤ 28 weeks with birth weight (BW) ≤ 1000 g and who survived beyond 12 h. Infants with congenital malformations or provided palliative care were excluded along with infants born <23 weeks.
Demographic data and neonatal outcomes
Relevant data was obtained from a prospectively maintained neonatal database and individual case records. The variables collected included maternal data such as maternal age, ethnicity, use of antenatal steroids (ANS), premature rupture of membranes, chorioamnionitis, pregnancy induced hypertension, and delivery mode. Neonatal data included BW, GA, type of delivery room resuscitation needed, surfactant therapy, mode of assisted ventilatory support and FiO2 requirements in the first week of life. Neonatal outcomes included major neonatal morbidities and mortality. GA assessment was based on an early dating scan or date of the last menstrual period. Intensive delivery room resuscitation included the need for endotracheal intubation, cardiac massage or adrenaline. The hospital follows a structured resuscitation policy where limit of viability is set at 23 weeks gestation. No resuscitation was instituted at 23 weeks except at parental request. At 24 weeks the resuscitation was provided unless parents indicated otherwise and all infants born >25 weeks were resuscitated.
The definitions for complete ANS, respiratory distress syndrome (RDS), hemodynamically significant patent ductus arteriosus (HsPDA), chorioamnionitis, sepsis, necrotizing enterocolitis were standardized as per Neonatal Research Network (NRN) as explained in our earlier publication [18].
Modes of assisted ventilator support were mechanical ventilation (MV), high-frequency oscillatory ventilation, nasal continuous positive airway pressure (CPAP), or nasal intermittent mandatory ventilation (NIMV). Maximal ventilatory support mode needed on Days 1 and 7 were recorded along with oxygen (O2) requirements needed to maintain SpO2 levels between 88% and 95%. Standard respiratory management included early NCPAP, early surfactant therapy, prophylactic caffeine, and extubation to NCPAP/NIMV.
BPD definitions and severity classifications were based on the physiologic definition of BPD at 36 weeks postmenstrual age (PMA) as developed by the National Institute of Child Health and Human Development (NICHD 2001) [11, 22]. The BPD was classified as the following: No BPD as not receiving supplemental O2 for 28 days or at 36 weeks PMA; mild BPD as receiving O2 for ≥28 days but not at 36 weeks PMA; moderate BPD as receiving O2 for ≥28 days and FiO2 < 0.30 at 36 weeks PMA, and severe BPD as O2 for ≥28 days and FiO2 ≥ 0.30 or positive pressure at 36 weeks PMA. For our study, this classification was further stratified into two groups with Group 1 being defined as infants having no/mild BPD while Group 2 infants had the composite “adverse outcome” of moderate/severe BPD and/or Death ≤36 weeks PMA. Ethics approval and the waiver of consent were obtained by the hospital’s Institutional Review Board.
Statistics
Statistical analysis was performed using χ2-test or Fisher’s exact test for categorical variables and Student’s t test for continuous variables. Univariate analysis was performed to assess the risk factors for an adverse outcome. Multivariate logistic regression analysis was performed to identify independent significant risk factors associated with an adverse outcome and Odds ratios (OR) with 95% Confidence Interval (CI) were reported. All statistical analyses were performed by using SPSS version 18 and the analysis performed was two tailed with significance set at P < 0.05.
Results
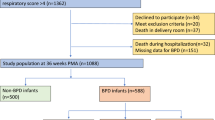
Between January 2012 and December 2015of 355 ELBW infants born in KKH, 266 met the study’s inclusion criteria. (Fig. 1). The mean GA and BW for the entire cohort was 25.5 ± 1.47 weeks and 748 ± 142 g respectively. Of these, 71 (27%) and 195 (73%) belonged to Groups 1and 2, respectively.
Overall mortality was 19% (50/266) at 36 weeks PMA and 67% (145/216) of infants alive at 36 weeks had moderate to severe BPD. The incidence of death, moderate/severe BPD and survival without BPD/Mild BPD at each week of GA are shown in Fig. 2 with an inverse relationship between an adverse outcome and increasing GA except at 23 weeks. Of the 22 infants born at 23 weeks survival was lower and 8/22(36%) were provided with palliative care. Mortality rates decreased from 43% at 23 weeks to 25% at 24 weeks, 20% at 25 weeks, and then was between 11–12% in 26–28 weeks. The incidence of moderate to severe BPD was noted to be 43% at 23 weeks; 68% at 24 weeks and then gradually decreased to 55% at 25 and 26 weeks and between 44 and 46% at 27 and 28 weeks GA. The composite adverse outcome of moderate to severe BPD/Death decreased significantly from 86–93% at 23–24 weeks to 67–75% at 25–26 weeks and to <60% at 27 and 28 weeks (OR 0.63; 95% CI;0.52–0.77, P < 0.001).
Antenatal, perinatal, neonatal demographics and neonatal outcomes
The perinatal and neonatal demographic characteristics of the two groups are compared in Table 1. Mean GA and BW of ELGANS in Group 2 were significantly lower than Group1with a higher proportion of infants <26 weeks and BW < 750 g (Table 1).
Of 141 ELGANs with GA 23–25 weeks, 119 (84%) had an adverse outcome compared to 76/125 (61%) infants between 26 and 28 weeks (OR 3.4; 95% CI; 1.93–6.13, P < 0.001).
Similarly of 144 ELGANs with BW < 750 g, 119(83%) had an adverse outcome compared to 76/122 (62%) infants with BW > 750 g (OR 2.9; 95% CI; 1.61–5.04, P < 0.001).
The need for intensive resuscitation and surfactant therapy was significantly higher in Group 2 as were neonatal morbidities, culture proven sepsis, HsPDA and air leaks compared to Group1. A nonsignificant lower rate of ANS use and delivery by cesarean section in Group 2 was also noted.
Resource utilizations in the form of respiratory support and NICU occupancy are compared in Table 2. Nearly all Group 2 infants needed MV support on Day 1 and nearly half of them continued to need MV on Day 7 as well. In contrast, in Group 1 less than one fifth needed MV support by Day 7. Median number of days on oxygen, MV and NICU stay were also higher in Group 2 as were Maximum FiO2 requirements on Days 1 and 7. On regression analysis, only MV support need on Day 7 was independently associated with an adverse outcome (OR1.97, 95%CI; 1.30–3.07, P < 0.001), while other factors significant on univariate analysis such as GA, BW, gender, sepsis, HsPDA, air leaks, oxygen requirements at day 1 and 7 were no longer significant.
Discussion
In our study of high risk ELGANs born from 2012 to 2015, moderate/severe BPD was present in 67% of survivors at 36 weeks and composite adverse outcome of BPD/death occurred in 73% of the cohort. Our overall mortality rate of 19% was similar to the 24% mortality rate in the NRN for infants born between 22 and 28 weeks from 2008 to 2012 [4]. Mortality decreased from 43% at 23 weeks to 12% at 27 weeks in our cohort, and was comparable with the NRN for gestational ages between 25 and 27 weeks. Our lower mortality rate of 43% at 23 weeks compared to 68% in the NRN may be due to fewer numbers resuscitated in our cohort with exclusion of eight infants provided with palliative care.
In the NRN, BPD rates increased from 2009 to 2012 in ELGANs for all gestational ages except at 28 weeks. Similarly, at our institute, BPD rates increased from 29% between 2000 and 2009, to 67% in the period 2012–2015 [18]. This higher prevalence may be due to the significantly higher proportion of neonates between 23 and 25 weeks GA group in our recent cohort (141/266(53%) compared to 253/835 (30%) in our earlier study (P < 0.0001). Notably more parents opted for resuscitation in our current study with 14/22(67%) at 23 weeks gestation opting for active care compared to 23/47(49%) in our earlier study.
A systematic review done by Csaba et al. documented global variation with the incidence of moderate BPD ranging from 13% to 31% and severe BPD from 17% to 42% in ELGANs with heterogeneity among different populations [23]. Persistent or increasing BPD rates in recent cohorts reflect the limits of support that advanced technology can provide to the extremely vulnerable immature ELGAN lung.
Over the years, varying BPD definitions have caused difficulty in risk estimation for adverse pulmonary and neurodevelopmental outcomes. Standardized definitions to identify varying severity of BPD first outlined in 2001 by Jobe and Bancalari [11], were revised in 2004 and more recently the Canadian Neonatal network in 2017 used 40 weeks PMA as cut off point rather than 36 weeks PMA [24]. The NICHD also held a workshop in 2016 where refinements were suggested to the definition of BPD taking into account newer modes of noninvasive ventilation. As mentioned by Higgins et al., the limitation of using the 40 weeks’ time point would be loss of data as many infants are discharged prior to 40 weeks PMA [25]. We continued to use the original NICHD classification for this study as individual data on nasal cannula flow rates was not captured.
Using a standardized BPD definition and expanded measures of respiratory insufficiency will enable us to objectively compare our data with international benchmarks and estimate correlations of BPD and its risk factors with longer term respiratory and neurodevelopmental outcome.
Risk factors for an adverse outcome
A composite adverse outcome for BPD/death [15,16,17] is used in ELGANS as they are often competing outcomes. Adverse outcomes for gestational ages 23–28 weeks ranged from 86% to 57% in our study, and similar rates of 45–89% were reported in extremely preterm Korean infants by Joe et al. [17]. In the large California perinatal quality care collaborative (CPCQCC) study of 166 NICU’s, BPD/death occurred in 44.8% of the cohort but ranged widely from 17.3% to 73.4% and also included infants at 29 weeks gestation [15].
Our rates of moderate/severe BPD steadily decreased with increasing GA from 68% to 44% from 24 to 27 weeks, respectively and this inverse relationship between decreasing GA and increasing adverse outcome especially below 26 weeks GA has been well documented [26, 27]. In a large NICHD study nearly 100% of surviving infants born before 23 weeks developed BPD, whereas the rate reduced to 1% at 30 weeks GA [27]. The phenomenon of rising prevalence of “New BPD” has been postulated to be due to the ELGAN lungs’ extreme immaturity at birth with an arrest in the canalicular or early saccular phase, disruption of alveolarisation, impaired and dysregulated microvascular development and high pulmonary vascular resistance with abnormal vascular reactivity. [28]. Later phases of lung development may be subsequently affected by postnatal events including resuscitation, oxygen toxicity, sepsis, and HsPDA [15,16,17]. We could not demonstrate any antenatal factors such as chorioamnionitis or lack of ANS to be associated with an adverse outcome [29, 30]. In recent studies though chorioamnionitis has been shown to be associated with BPD, Villamor-Martinez et al. in the systematic review concluded that the association of chorioamnionitis and BPD was modulated by GA and RDS [31].
Apart from decreasing GA and BW, other significant perinatal/neonatal risk factors on univariate analysis for an adverse outcome included the need for intensive neonatal resuscitation, surfactant use, air leaks, sepsis, HsPDA needing treatment, higher oxygen requirement, and the persistent MV at the end of the 1st week of life. While surfactant use was associated with increased risk of BPD the association of surfactant with BPD in our study was not likely to be causal, and was probably reflective of underlying lung immaturity and increasing survival of very preterm infants [32]. Similar to the CPCQCC and Korean national registry findings [33, 34] post natal sepsis was associated with nearly threefold higher odds of BPD/death (OR 2.9, 95% CI: 1.27, 6.37) in our cohort and possibly could be attributed to effect of systemic inflammation and pro-inflammatory cytokines. [35, 36].
While HsPDA and surgical closure of the duct was associated with an adverse outcome in our data and in other studies, it was not an independent risk factor and this may be due to confounders such as timing of treatment, magnitude of the shunt, gestational age, illness severity, and increased need for MV in the presence of a HsPDA [17, 23, 37].
Research from clinical studies and animal models has consistently shown mechanical ventilation and large tidal volume breaths at resuscitation being associated with injury to the small and large airways of the lung. In a recent review Jobe again emphasized that, assisted ventilation during resuscitation potentially damaged the surfactant deficient structurally immature lung by exposure to high pressures, volume and oxygen through amplication of inflammatory pathways. This possibly may be a major contributory pathway for “New BPD” [38]. The importance of the golden first hour is being increasingly recognized with trials looking at noninvasive respiratory support, less invasive surfactant administration and use of nebulized surfactant during CPAP [39]. A systematic review by Schmolzer showed significant benefits with early CPAP in reducing BPD/death [40].
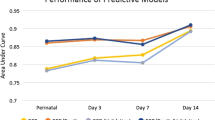
The significantly higher need for and duration of mechanical ventilation and oxygen supplementation in Group 2 infants in our study has been consistently corroborated in clinical studies and systemic reviews [16, 41] and used to develop predictive models of BPD [27, 42, 43].
Of all the risk factors associated with an adverse outcome on univariate analysis only the persistent need for mechanical ventilatory support on Day 7 was found to be independently predictive of an adverse outcome on multivariate analysis.
The striking association between MV and BPD has been attributed to ventilator associated lung injury (VALI) with a clear link between MV induced barotrauma, volutrauma, atelectrauma, and “biotrauma” of pathological structural and inflammatory lung changes. Given our knowledge about VALI and the awareness that longer duration of ventilation is associated with BPD due to increasing ventilator induced lung injury, identifying the risk factors for the prediction of BPD/death with advancing postnatal age would be a useful tool for prognostication and selecting high risk infants for preventive therapies [16, 26].
Bhering developed a predictive model where infants needing MV for >48 h in the first week of life had a greater risk for BPD [42]. In our study the need for MV on day 7 was significantly associated with an adverse outcome similar to findings by Laughon et al. [27].
Resource utilization in infants with an adverse outcome in our study was significantly higher with increased NICU days and longer duration of MV support. The high financial, emotional, and psychological costs of BPD in the neonatal period and throughout childhood for families and health care systems need to be addressed [10].
The strengths of our study include the use of a structured BPD definition and stratification of BPD which will enable objective comparison of our data with international benchmarks and implement future QI measures. Another strength is the availability of detailed data on antenatal, perinatal, and postnatal risk factors in our multiethnic Asian population. Lastly our data is from a recent cohort of ELGANs born after 2010, reflecting the current state of modern NICU care.
Limitations of our study include its retrospective nature and single center data. However, this may be mitigated by our hospital being Singapore’s leading tertiary perinatal center managing more than two thirds of its ELBW population. Another limitation as mentioned previously is the lack of granular data on newer modes of noninvasive ventilation preventing the implementation of the proposed NICHD refinement of BPD classification.
Conclusions
Rates of BPD continued to be high in our cohort of ELGANs ≤ 28 weeks with the most significant predictive risk factor being the need for MV support at the end of the first week of life. Our data would enable us to focus our attention to explore strategies targeted at limiting MV induced lung damage. Areas of possible quality improvement projects include delivery room resuscitation with increased use of noninvasive ventilation, minimally invasive surfactant therapy, lung protective ventilation strategies, incorporating evidence-based practices for intubation/extubation criteria, and standardized post-extubation support aimed at preventing reintubation. Furthermore, this data will enable us to develop prospective models for BPD prediction and prognostication.
References
Stoll BJ, Hansen NI, Bell EF, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56. https://doi.org/10.1542/peds.2009-2959
Jensen EA, Schmidt B. Epidemiology of bronchopulmonary dysplasia. Birth Defect Res Part A Clin Mol Teratol. 2014;100:145–57.
Berkelhamer SK, Mestan KK, Steinhorn RH. Pulmonary hypertension in bronchopulmonary dysplasia. Semin Perinatol. 2013;37:124–31.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network: trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51. https://doi.org/10.1001/jama.2015.10244
Northway WH Jr, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967;276:357–68. https://doi.org/10.1056/NEJM196702162760701
Vollsaeter M, Røksund OD, Eide GE, Markestad T, Halvorsen T. Lung function after preterm birth: development from mid-childhood to adulthood. Thorax. 2013;68:767 https://doi.org/10.1136/thoraxjnl-2012-202980
Kugelman A, Reichman B, Chistyakov I.Israel Neonatal Network et al. Postdischarge infant mortality among very low-birth weight infants: a population-based study. Pediatrics. 2007;120:e788–e794. https://doi.org/10.1542/peds.2006-3765.
Van Marter LJ, Kuban KC, Allred E, et al. Does bronchopulmonary dysplasia contribute to the occurrence of cerebral palsy among infants born before 28 weeks of gestation? Arch Dis Child Fetal Neonatal Ed. 2011;96:F20–F29. https://doi.org/10.1136/adc.2010.183012. ELGAN Study Investigators
Russell RB, Green NS, Steiner CA, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120:e1–e9. https://doi.org/10.1542/peds.2006-2386
Lapcharoensap W, Bennett MV, Xu X, Lee HC, Dukhovny D. Hospitalization costs associated with bronchopulmonary dysplasia in the first year of life. J Perinatol. 2020;40:130–7. https://doi.org/10.1038/s41372-019-0548-x
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9. https://doi.org/10.1164/ajrccm.163.7.2011060
Cokyaman T, Kavuncuoglu S. Bronchopulmonary dysplasia frequency and risk factors in very low birth weight infants: a 3-year retrospective study. North Clin Istanb. 2019;7:124–30. https://doi.org/10.14744/nci.2019.23427. Published 2019 Aug 9
Ambalavanan N, Van Meurs KP, Perritt R, et al. Predictors of death or bronchopulmonary dysplasia in preterm infants with respiratory failure. J Perinatol. 2008;28:420–6. https://doi.org/10.1038/jp.2008.18
Klinger G, Sokolover N, Boyko V, et al. Perinatal risk factors for bronchopulmonary dysplasia in a national cohort of very-low-birthweight infants. Am J Obstet Gynecol. 2013;208:115.e1–9. https://doi.org/10.1016/j.ajog.2012.11.026
Lapcharoensap W, Gage SC, Kan P, et al. Hospital variation and risk factors for bronchopulmonary dysplasia in a population-based cohort. JAMA Pediatr. 2015;169:e143676 https://doi.org/10.1001/jamapediatrics.2014.3676
Keszler M, Sant’Anna G. Mechanical ventilation and bronchopulmonary dysplasia. Clin Perinatol. 2015;42:781–96. https://doi.org/10.1016/j.clp.2015.08.006
Jo HS, Cho KH, Cho SI, Song ES, Kim BI. Recent changes in the incidence of bronchopulmonary dysplasia among very-low-birth-weight infants in Korea. J Korean Med Sci. 2015;30:S81–S87. https://doi.org/10.3346/jkms.2015.30.S1.S81
Agarwal P, Sriram B, Rajadurai VS. Neonatal outcome of extremely preterm Asian infants ≤28 weeks over a decade in the new millennium. J Perinatol. 2015;35:297–303.
Ameenudeen SA, Boo NY, Chan LG. Risk factors associated with chronic lung disease in Malaysian very low birthweight infants. Med J Malays. 2007;62:40–5.
Malaysian National Neonatal Registry and Clinical Research Centre, Ministry of Health Malaysia, Kuala Lumpur. 2017.
Wariki WM, Mori R, Boo NY, Cheah IG, Fujimura M, Lee J, et al. Risk factors associated with outcomes of very low birthweight infants in four Asian countries. J Paediatr Child Health. 2013;49:E23–7. https://doi.org/10.1111/jpc.12054. Epub 2013 Jan 3. PMID: 23282105
Ehrenkranz RA, Walsh MC, Vohr BR, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 2005;116:1353–60. https://doi.org/10.1542/peds.2005-024
Csaba Siffel, Kristin D. Kistler, Juliana F., Lewis, M. & Sujata P Sarda. Global incidence of bronchopulmonary dysplasia among extremely preterm infants: a systematic literature review, J Matern-Fetal Neonatal Med. 2019. https://doi.org/10.1080/14767058.2019.1646240
Isayama T, Lee SK, Yang J, et al. Revisiting the definition of bronchopulmonary dysplasia: effect of changing panoply of respiratory support for preterm neonates. JAMA Pediatr. 2017;171:271–9. https://doi.org/10.1001/jamapediatrics.2016.4141
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8. https://doi.org/10.1016/j.jpeds.2018.01.043. Epub 2018 Mar 16. PMID: 29551318; PMCID: PMC5970962
Kardum D, Filipović Grčić B, Müller A, Dessardo S. Incidence and risk factors for moderate and severe bronchopulmonary dysplasia in very low birth weight infants in two Croatian perinatal regions—a retrospective cohort study. J Pediatr Neonat Individ Med. 2019;8:e080129 https://doi.org/10.7363/080129
Laughon MM, Langer JC, Bose CL, et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med. 2011;183:1715–22.
Jain D, Bancalari E. Bronchopulmonary dysplasia: clinical perspective. Birth Defects Res A Clin Mol Teratol. 2014;100:134–44. https://doi.org/10.1002/bdra.23229
Hartling L, Liang Y, Lacaze-Masmonteil T. Chorioamnionitis as a risk factor for bronchopulmonary dysplasia: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2012;97:F8–F17.
Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006; CD004454. Published 19 Jul 2006. https://doi.org/10.1002/14651858.CD004454.pub2
Villamor-Martinez E, Álvarez-Fuente M, Ghazi AMT, et al. Association of chorioamnionitis with bronchopulmonary dysplasia among preterm infants: a systematic review,meta-analysis, and metaregression. JAMA Netw Open. 2019;2:e1914611 https://doi.org/10.1001/jamanetworkopen.2019.14611
Zysman-Colman Z, Tremblay GM, Bandeali S, Landry JS. Bronchopulmonary dysplasia–trends over three decades. Pediatr Child Health. 2013;18:86–9. https://doi.org/10.1093/pch/18.2.86
Lapcharoensap W, Kan P, Powers RJ, et al. The relationship of nosocomial infection reduction to changes in neonatal intensive care unit rates of bronchopulmonary dysplasia. J Pediatr. 2017;180:105–.e1. https://doi.org/10.1016/j.jpeds.2016.09.030
Jung E, Lee BS. Late-onset sepsis as a risk factor for bronchopulmonary dysplasia in extremely low birth weight infants: a nationwide cohort study. Sci Rep. 2019;9:15448 https://doi.org/10.1038/s41598-019-51617-8. Published 2019 Oct 29
Adams-Chapman I. Long-term impact of infection on the preterm neonate. Semin Perinatol. 2012;36:462–70. https://doi.org/10.1053/j.semperi.2012.06.009
Pryhuber GS. Postnatal infections and immunology affecting chronic lung disease of prematurity. Clin Perinatol. 2015;42:697–718. https://doi.org/10.1016/j.clp.2015.08.002
Benitz WE, Bhombal S. The use of non-steroidal anti-inflammatory drugs for patent ductus arteriosus closure in preterm infants. Semin Fetal Neonatal Med. 2017;22:302–7. https://doi.org/10.1016/j.siny.2017.07.004
Jobe AH. Mechanisms of lung injury and bronchopulmonary dysplasia. Am J Perinatol. 2016;33:1076–8. https://doi.org/10.1055/s-0036-1586107
Lau CSM, Chamberlain RS, Sun S. Less invasive surfactant administration reduces the need for mechanical ventilation in preterm infants: a meta-analysis. Glob Pediatr Health. 2017;4:2333794X17696683 https://doi.org/10.1177/2333794X17696683. Published 2017 Mar 24
Schmölzer GM, Kumar M, Pichler G, Aziz K, O’Reilly M, Cheung PY. Non-invasive versus invasive respiratory support in preterm infants at birth: systematic review and meta-analysis. BMJ. 2013;347:f5980.
Trembath A, Laughon MM. Predictors of bronchopulmonary dysplasia. Clin Perinatol. 2012;39:585–601. https://doi.org/10.1016/j.clp.2012.06.014
Bhering CA, Mochdece CC, Moreira ME, Rocco JR, Sant’Anna GM. Bronchopulmonary dysplasia prediction model for 7-day-old infants. J Pediatr. 2007;83:163–70.
Wai KC, Kohn MA, Ballard RA, Truog WE, Black DM, Asselin JM, et al. Early cumulative supplemental oxygen predicts bronchopulmonary dysplasia in high risk extremely low gestational age newborns. J Pediatr. 2016;177:97–102, e2.
Acknowledgements
We thank and appreciate Prof Lourdes Mary Daniel for her valuable input and suggestions on the manuscript and associate executives Nuratiqah Khirwadon and Ang Cheng Hiang in editing the charts and in formatting the manuscript.
Author information
Authors and Affiliations
Contributions
Odattil Geetha had full access to all of the data in this study, takes responsibility for the integrity of the data and the accuracy of the analyses. She conceptualized and designed the study, did the data collection and review of case notes, selected data for inclusion in analyses, and drafted initial manuscript. Pratibha Agarwal was the senior mentor and was involved in the study concept and design, data analysis and interpretation along with revision of the initial manuscript. Victor Samuel Rajadurai was involved in the study concept and in the review and revision of the manuscript. Amudha Jayanthi Anand helped in data analysis and drafting of the manuscript. Khoo Poh Choo was involved in the review and revision of the manuscript. Quek Bin Huey was involved in the review and revision of the manuscript. Chua Mei Chien was involved in the review and revision and critical analysis of the manuscript. Staff Nurse Rowena Dela Puerta had full access to data in the study and takes responsibility for data integrity and was involved in the review of the manuscript. All authors approved the final manuscript as submitted and have no conflict of interest.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Geetha, O., Rajadurai, V.S., Anand, A.J. et al. New BPD-prevalence and risk factors for bronchopulmonary dysplasia/mortality in extremely low gestational age infants ≤28 weeks. J Perinatol 41, 1943–1950 (2021). https://doi.org/10.1038/s41372-021-01095-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01095-6
This article is cited by
-
Artificial intelligence in bronchopulmonary dysplasia- current research and unexplored frontiers
Pediatric Research (2023)
-
Risk factors for bronchopulmonary dysplasia infants with respiratory score greater than four: a multi-center, prospective, longitudinal cohort study in China
Scientific Reports (2023)