Abstract
Giant cell tumor of bone typically involves the epiphysis of the long bones of skeletally mature patients. It is genetically characterized by highly recurrent and specific mutations of the H3F3A gene, which encodes histone H3.3. The most common mutation H3F3A G34W can readily be detected by a recently developed mutation-specific antibody. Giant cell tumor of bone rarely transforms to a sarcoma (malignant giant cell tumor of bone), which has not been genetically characterized in detail. We studied seven clinicopathologically defined malignant giant cell tumors, as well as two H3F3A-mutant bone sarcomas without giant cell tumor histology using a combination of clinicopathological, immunohistochemical, and molecular methods (Sanger sequencing + pyrosequencing or next generation sequencing). The cases included five men and four women, with a median age at initial diagnosis of 27 years. The two H3F3A G34W-positive sarcomas without giant cell tumor histology involved the subarticular epiphyseal sites, suggesting relatedness with giant cell tumor of bone. In two of the seven clinicopathologically defined malignant giant cell tumor cases, the sarcoma tissue showed the H3F3A G34W mutation. However, in the remaining five cases, in contrast to their associated H3F3A G34W-mutant giant cell tumor, the sarcoma lacked the H3F3A G34W mutation, either entirely or sub-clonally in the samples tested. This discordant mutation status was confirmed in all instances by immunohistochemistry and sequencing. A FISH analysis suggested that the absence of the H3F3A G34W mutation may be related to deletion of the H3F3A gene. Therefore, we have demonstrated that H3F3A G34W mutation, a critical driver in giant cell tumor, is absent in a subset of malignant giant cell tumor of bone. This novel recurrent phenomenon has potential biological and diagnostic implications, and further study is required to better characterize this progression pathway and understand its mechanism.
Similar content being viewed by others
Introduction
Giant cell tumor of bone is a relatively common tumor in skeletally mature patients that typically involves the epiphysis of the long bones, often involving the subarticular site [1, 2]. It is histologically characterized by proliferation of bland oval to short-spindled mononuclear neoplastic cells uniformly interspersed with osteoclast-like multinucleated giant cells. The histological spectrum can be broad, including a variety of secondary changes. This tumor is typically treated by curettage or resection; however, it can locally recur in ~25–35% of cases, mostly within 3 years after surgery [1]. Administration of denosumab, a monoclonal antibody to the receptor activator of nuclear factor kappa-B ligand (RANKL), inhibits the RANK/RANKL axis, reducing the formation and function of osteoclasts, thus providing benefit to a subset of patients [3]. Although conventional giant cell tumor rarely metastasizes to the lung, even metastatic tumors typically behave indolently [1, 2].
Malignant transformation of giant cell tumor of bone, also known as malignant giant cell tumor, malignancy in giant cell tumor, or dedifferentiated giant cell tumor, is rare and is a clinicopathologically-defined diagnostic concept. We used the malignant giant cell tumor of bone terminology here as it is the best established and succinct, although it should not be confused with giant-cell-rich sarcoma. Primary malignant giant cell tumor of bone pertains to a tumor in which conventional giant cell tumor and sarcoma components coexist at presentation. Secondary malignant giant cell tumor of bone refers to a sarcoma that develops subsequent to conventional giant cell tumor, usually 5 years or more after the treatment of giant cell tumor, often in association with prior radiotherapy. Secondary malignant giant cell tumor is the most common, whereas primary malignant giant cell tumor is considered extremely rare [1, 2]. The sarcoma in these malignancies is usually high grade and is in the form of undifferentiated pleomorphic sarcoma, osteosarcoma, or fibrosarcoma. The prognosis of malignant giant cell tumor of bone is similar to that of high-grade sarcoma, and the secondary malignant subtype reportedly has a worse prognosis than the primary malignant subtype [4].
Giant cell tumor of bone is genetically characterized by a highly recurrent mutation (>90% of cases) at the G34 position of the H3F3A gene, which encodes histone H3.3, with the G34W substitution being the most common (~96% of G34 mutations) [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]. Rare mutations include H3F3A G34V, G34R, and G34L, among others. Although these G34 mutations can be detected using formalin-fixed paraffin-embedded samples, Sanger sequencing may suffer from low sensitivity because of the large number of non-neoplastic components, including giant cells as well as inflammatory cells, which dilute the fraction of mutant alleles in the neoplastic mononuclear spindle cells [15]. Other sequencing methods with higher degrees of sensitivity can be used to detect G34 mutation, including next generation sequencing, high-resolution melting analysis, and pyrosequencing [10, 15]. In addition, the recent development of commercially available mutation-specific antibodies has facilitated the detection of the most common H3.3 G34 mutations (i.e., G34W, G34V, and G34R). Diffuse staining typically decorates the mononuclear tumor cells, consistent with the suspected early driver role of H3F3A mutation [6]. The H3F3A G34 mutation is highly specific for giant cell tumor of bone, and virtually all histological mimics lack this genetic signature [6, 8, 10, 12, 14, 16, 17, 19, 20]. Accordingly, H3.3 G34 mutation-specific immunohistochemistry is recognized as a powerful tool for confirming a diagnosis [6, 12, 19].
Compared to that of conventional giant cell tumor of bone, the H3F3A mutation status of malignant giant cell tumor has not been extensively studied. To date, ~40 cases of H3F3A G34-mutant bone sarcomas have been reported, [6, 7, 10, 11, 15, 16, 18, 19, 21,22,23] and about one-third of these cases were explicitly reported to be associated with giant cell tumor of bone, suggesting that H3F3A mutation may also play a role in malignant giant cell tumor. Although the remaining cases were not associated with giant cell tumor of bone, such tumors have been often found to affect subarticular sites in young adult patients [6, 11], reminiscent of a classic scenario of giant cell tumor of bone. It is therefore hypothesized that H3F3A G34-mutant bone sarcomas may originate from giant cell tumor even when the precursor lesion is histologically unapparent [6]. However, such a genetically expanded definition of primary malignant giant cell tumor of bone is still controversial.
The present study aims to better understand the H3F3A status in malignant giant cell tumor of bone in relation to the tumor phenotype, using a combined clinicopathological, immunohistochemical, and molecular approach. By longitudinally investigating tumors in their disease course and examining spatial distribution of mutations, we discovered that in a subset of malignant giant cell tumor cases, the H3F3A G34W mutation was absent in sarcoma in contrast to the associated conventional giant cell tumor.
Materials and Methods
Case selection
The study was approved by the institutional review board (2014–089). From the archive of the National Cancer Center Hospital, Tokyo, Japan, we retrieved two cases of primary malignant giant cell tumor of bone and four cases of secondary malignant giant cell tumor of bone. One case of secondary malignant giant cell tumor of bone was provided by Komagome Hospital, Tokyo Japan. In addition, we immunohistochemically screened tissue samples from 116 cases that were originally diagnosed as conventional osteosarcoma and four cases that were diagnosed as malignant fibrous histiocytoma (undifferentiated pleomorphic sarcoma) of the bone, using H3.3 G34W-specific immunohistochemistry; for the cases that were negative for H3.3 G34W staining, we used H3.3 G34V and H3.3 G34R immunohistochemistry based on the condition that the patients were 20 years of age or older. This screening identified one case each of an osteosarcoma and an undifferentiated pleomorphic sarcoma, both of which were rich in giant cells and were positive for H3.3 G34W immunohistochemistry. As histological review of these latter two cases failed to identify giant cell tumor component, they did not meet the clinicopathological definition of malignant giant cell tumor of bone. However, according to the recent proposal [6], we included these tumors in our study cohort as a distinctive subset for further characterization. Of note, although our screening cohort included 11 additional giant-cell-rich osteosarcomas, none of them was positive for H3.3 G34W, G34V, or G34R staining.
Immunohistochemistry
Four-micrometer-thick formalin-fixed paraffin-embedded sections were deparaffinized, and heat-induced epitope retrieval was performed with a Target Retrieval Solution pH 9 (Dako, Carpinteria, CA, USA). The slides were then treated with 3% hydrogen peroxide for 20 min to block endogenous peroxidase activity. The slides were incubated for 1 h at room temperature with the primary antibodies, including anti-histone H3.3 G34W (RM263, dilution 1:1000, RevMab Bioscience, South San Francisco, CA, USA), anti-histone H3.3 G34R (RM240, dilution 1:200, RevMab Bioscience), and anti-histone H3.3 G34V (RM307, dilution 1:4000, RevMab Bioscience). Immunostaining was detected using the EnVision system (Dako). LINKER (Dako) was used for H3.3 G34R staining. Diaminobenzidine was used as the chromogen, and hematoxylin was used as the counterstain. Appropriate positive and negative controls were also included in the immunohistochemical analysis. Staining was considered positive when strong nuclear reactivity was observed. Multiple tumor specimens along the disease course were longitudinally stained (i.e., primary, local recurrences, and metastases). In some cases, multiple sections from a single tumor nodule were stained.
Sequencing
DNA sequencing of the H3F3A gene was performed to confirm the immunohistochemical results when tissues were available. For those cases in which a block contained both immunopositive and -negative tumor areas, each area was macro-dissected and subjected to a separate analysis. The adequacy of the tumor cell contents was confirmed on H&E slides before sequencing.
For case 4, the next generation sequencing data have been reported previously [15]. For the other cases, Sanger sequencing and pyrosequencing were performed using formalin-fixed paraffin-embedded tumor sections. The tumor sections were deparaffinized and DNA was extracted using a DNeasy Blood & Tissue Kit (Qiagen, Tokyo, Japan) or a GeneRead DNA FFPE Kit (Qiagen). Templates for pyrosequencing were prepared by PCR amplification using a Pyromark PCR Kit (Qiagen) and the following primers: (5′-AGCAACTGGCTACAAAAGC-3′) and (5′-biotinylated-CATACAAGAGAGACTTTGTCCC-3′). PCR was carried out using 45 cycles with an annealing temperature of 60 °C. The PCR products were electrophoresed on an agarose gel stained with GelRed (Biotium, Fremont, CA, USA). When the amounts of the amplified product were small (cases 5 and 6), a second round of PCR amplification using an aliquot of the initial PCR product was performed to obtain sufficient product. The primers and the reaction conditions used for the second round of PCR were the same as those for the first round. Pyrosequencing was performed using PyroGold Q96 SQA Reagents and PyroMark Q96 software (version 2.5.7) on a PSQ96 pyrosequencer (Qiagen) according to the manufacturer’s recommendations. The sequencing primer, sequence to analyze, and dispensation order were as follows; 5′-AGTGCGCCCTCTACTGGA-3′, 5′-NGGGTGAAGAAACCTCATCGTTACAG-3′, and 5′-ACTGGTGAGAC-3′, respectively. Sanger sequencing was carried out to validate the mutation status. The amplified DNA was purified using ExoSAP (Affymetrix Japan KK, Tokyo, Japan), and sequencing was performed with the BigDye Terminator v3.1 cycle sequencing kit (Applied Biosystems, Foster City, CA, USA) and the same primers used for the amplification of the genomic DNA.
Fluorescence in situ hybridization (FISH)
To examine H3F3A copy number alterations in relation to H3F3A mutation status, we used an H3F3A/CEN1q Dual Color FISH Probe (GSP Laboratory, Kobe, Japan). This probe was previously validated not to hybridize to H3F3B using a metaphase spread. FISH images were captured using the Metafer Slide Scanning Platform to facilitate analysis (MetaSystems, Altlußheim, Germany). We evaluated >100 non-overlapping mononuclear tumor cells that had at least one evaluable signal and interpreted the signals as previously described by Scheie et al. [24] with modification. Briefly, we defined the H3F3A deletion signal pattern when a mononuclear tumor cell contained CEN1q signals (green) whose number exceeded that of H3F3A signals (red). We then interpreted a tumor tissue as having an H3F3A deletion, when the proportion of cells with H3F3A deletion signal pattern exceeded the mean + 3 standard deviations (40.9%), which was determined based on five control cases of conventional giant cell tumor of bone that were immunopositive for H3.3 G34W (average, 18.3%, standard deviation, 7.5%). In evaluation, particular attention was paid to the morphologic differentiation between neoplastic versus non-neoplastic cells.
Results
Clinicopathological summary
As summarized in Table 1, the nine patients included five men and four women, with a median age at initial diagnosis of 27 years (20–45 years). The primary tumor sites were the distal femur (N = 4), proximal femur (N = 1), distal radius (N = 1), rib (N = 1), proximal humerus (N = 1), and lumbar vertebra (N = 1), seven of which involved subarticular sites. Seven cases were clinicopathologically defined malignant giant cell tumors of bone, whereas the remaining two cases, which were identified by immunohistochemical screening, presented with sarcoma histology without a giant cell tumor component. Of the former seven cases, the sarcoma was identified concurrently with the giant cell tumor histology in two cases (primary malignant giant cell tumor of bone) and as local or distant recurrences in the other five cases 10–28 years after the initial treatment for giant cell tumor (secondary malignant giant cell tumor of bone). In the latter five cases, the sarcoma histologies were osteosarcoma (N = 1) and undifferentiated sarcoma (N = 4).
Immunohistochemistry and sequencing results
H3.3 G34W immunohistochemistry was positive in all nine cases at least once during the disease course, and the immunohistochemical results were concordant with the sequencing data in all instances.
Sarcomas with no association with giant cell tumor histology
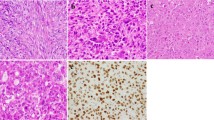
Both cases that presented as sarcoma without giant cell tumor histology (cases 1 and 8) were positive for the H3F3A G34W mutation (Fig. 1), and positive immunoreactivity was retained at recurrence/metastasis. Both cases involved the subarticular epiphyseal sites in young adults.
A representative case of an H3F3A G34W-mutant sarcoma that was not associated with giant cell tumor histology (case 1). This 21-year-old man presented with a lytic lesion in the proximal femoral epiphysis (a computed tomography). The tumor was composed of a diffuse proliferation of markedly atypical mononuclear cells intermixed with osteoclast-like giant cells (b note an atypical mitosis). The tumor cells were positive for H3F3A G34W (c H3.3G34W immunohistochemistry; d pyrosequencing; e Sanger sequencing). This tumor would be considered as malignant giant cell tumor of bone by some investigators [6], who advocate for the genetically expanded definition of this disease
Clinicopathologically defined malignant giant cell tumors of bone
Conventional giant cell tumor tissues were available for immunohistochemistry and/or mutation assay in all but 1 case (case 2), and they were invariably positive for the H3F3A G34W mutation. Sarcoma tissues in two malignant giant cell tumor cases (cases 2 and 3) showed the presence of the H3F3A G34W mutation. However, in the remaining five cases (cases 4, 5, 6, 7, and 9), the sarcoma tissues lacked the H3F3A G34W mutation based on immunohistochemistry and sequencing. The absence of the H3F3A G34W mutation was observed either entirely within a tested specimen or sub-clonally juxtaposed to H3F3A G34W-mutant sarcoma areas. The absence of the H3F3A G34W mutation was identified in the primary tumor (case 4), local recurrences (cases 5 and 7), and metastases (cases 6 and 9).
Representative case description of the absence of H3F3A G34W in malignant giant cell tumor of bone
Case 5
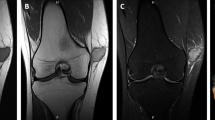
This female patient underwent curettage for giant cell tumor, which was positive for the H3F3A G34W mutation, in the femur at the age of 26 years. The first local recurrence occurred 20 years later (Fig. 2). A biopsy of the anterior part of the large recurrent tumor showed a giant cell-rich spindle cell tumor that was negative for H3F3A G34W. As this biopsy was originally interpreted as atypical and not as high-grade sarcoma, the patient was initially treated with denosumab. However, because the radiological response fell short of clinical expectation, a re-biopsy was performed on the posterior part of the recurrence, which then showed a spindle cell sarcoma positive for H3F3A G34W. The first biopsy was reviewed and the diagnosis revised to sarcoma. The femur was resected and grossly showed a single tan mass surrounding the abundant hydroxyapatite grafted at the time of curettage of the primary giant cell tumor. Immunostaining using 15 different blocks from this resection specimen produced identical results to the biopsy samples, with the posterior part of the tumor being positive for H3F3A G34W mutation and the anterior part being negative for H3F3A G34W. We were unable to identify the transition zone between the mutation-positive and -negative components because immunohistochemistry was mostly unsuccessful in the central part of the specimen, which had been heavily decalcified by acid due to abundant hydroxyapatite and associated osteoinduction. Multiple bone metastases (vertebrae and sacrum) appeared 5 months after the resection, and the patient is currently alive with disease.
A representative case of malignant giant cell tumor of bone that lacked H3F3A G34W mutation (case 5). Top: Primary conventional giant cell tumor in a patient of age 26 showing the typical histology and the H3F3A G34W mutation (a H&E staining; b H3.3G34W immunohistochemistry; c pyrosequencing; d Sanger sequencing). Bottom: The tumor locally recurred 20 years later as a sarcoma. Grossly, the resected femur in the sagittal section showed the presence of a tan mass surrounding the abundant hydroxyapatite placed at the time of curettage of the primary giant cell tumor (e). The posterior part (outlined in red) was positive for H3F3A G34W (f H&E staining; g H3.3G34W immunohistochemistry; h pyrosequencing; i Sanger sequencing), whereas the anterior part of the recurrence (outlined in blue) was negative for H3F3A G34W (j H&E staining; k H3.3G34W immunohistochemistry; l pyrosequencing; m Sanger sequencing)
Case 6
This male patient underwent curettage for H3F3A G34W-positive giant cell tumor in the distal radius at the age of 27 years (Fig. 3). The first local recurrence occurred at 3 months, which was treated with curettage and showed H3.3 G34W-positive giant cell tumor. Twenty-seven years later, a 2.1-cm lung metastasis developed, which was removed by wedge resection. Approximately 75% of the metastatic tumor consisted of giant cell-rich sarcoma, whereas the remaining 25% consisted of a spindle cell sarcoma with only a few giant cells. The giant cell-rich areas were negative for H3F3A G34W, whereas the giant cell poor component was positive for H3F3A G34W. Immunostaining was performed using four different blocks and showed identical results. Although these two areas were relatively sharply demarcated, there were a few H3.3 G34W immunopositive cells scattered within the H3.3 G34W immunonegative area at the transition zone (Supplementary Fig. 1). Altogether, these two components formed a single smooth-contoured mass. At age 59, the patient developed multiple metastases to the lung and vertebrae. The thoracic vertebral metastasis was resected, and showed a giant cell-rich sarcoma that was negative for the H3F3A G34W mutation. The patient subsequently died of the disease.
A representative case of malignant giant cell tumor of bone that lacked H3F3A G34W mutation (case 6). Top: Primary giant cell tumor in a patient at age 27 showing the typical histology and the H3F3A G34W mutation (a H&E staining; b H3.3 G34W immunohistochemistry; c pyrosequencing; d Sanger sequencing). Middle: Pulmonary metastasis occurred 27 years later. The wedge resection specimen showed a single smooth-contoured mass (e), with heterogeneous staining by H3.3 G34W immunohistochemistry (f). Three fourths of the tumor (outlined in blue) exhibited a giant cell-rich sarcoma that was negative for H3F3A G34W (g H&E staining; h H3.3 G34W immunohistochemistry; i pyrosequencing; j Sanger sequencing), whereas the remaining 1/4 (outlined in red) showed giant cell poor sarcoma histology that was positive for H3F3A G34W (k H&E staining; l H3.3 G34W immunohistochemistry; m pyrosequencing; n Sanger sequencing). Bottom: Vertebral metastasis, resected 5 years later, showed a giant cell-rich sarcoma that was negative for H3F3A G34W (o H&E staining; p H3.3 G34W immunohistochemistry; q pyrosequencing; r Sanger sequencing)
Absence of H3F3A mutation may be related to H3F3A gene deletion
We examined H3F3A copy number using FISH in cases 4, 5, 6, 7, and 9, where the mutation status was discordant. For cases 5, 6, and 7, we found that the H3F3A G34W-negative component harbored a H3F3A copy number deletion in relation to CEN1q, whereas the H3F3A G34W-positive component of the respective tumors had an intact H3F3A copy number (Table 2 and Fig. 4). In case 4, both the H3F3A G34W-positive and -negative components showed an intact H3F3A copy number. In case 9, the only autopsy case, the FISH analysis was unsuccessful. When we performed FISH on the remaining sarcoma cases (cases 1, 2, 3, and 8), where the H3F3A mutation was present, the H3F3A deletion was not found in cases 1, 3, and 8, whereas, in case 2, there was H3F3A deletion in the recurrence despite being positive for H3F3A G34W.
H3F3A copy number analysis using FISH (lung metastasis in case 6 that was illustrated in Fig. 3). Top (outlined in red): The H3F3A G34W-positive giant cell poor component showing intact copies of the H3F3A gene (i.e., two copies of H3F3A [red] and two copies of CEN1q [green]; a H3.3 G34W immunohistochemistry; b FISH). Bottom (outlined in blue): The H3F3A G34W-negative giant cell-rich component showed the monoallelic loss of H3F3A (i.e., one copy of H3F3A [red] and two copies of CEN1q [green]; c H3.3 G34W immunohistochemistry; d FISH)
Discussion
Characterization of malignant giant cell tumor of bone is challenging because of its rarity, broad histological spectrum of conventional giant cell tumor, and occasional presence of abundant giant cells in unrelated sarcomas. Taking advantage of a recent discovery of a specific H3F3A G34 mutation in >90% of giant cell tumors of bone, we analyzed a cohort of clinicopathologically defined malignant giant cell tumors and a few H3F3A-mutant bone sarcomas without giant cell tumor histology to better delineate their clinicopathological and molecular features. Among a total of nine cases, seven were associated with conventional giant cell tumor but had no previous history of radiotherapy for their primary tumors. In two of these cases, the H3F3A G34W mutation was present in the sarcoma tissue, in agreement with previously reported cases of malignant giant cell tumor of bone [6, 10, 22, 23]. The two H3F3A G34W-mutant sarcomas that were not associated with giant cell tumor histology developed in epiphyseal subarticular sites in young adults, hinting their relatedness to giant cell tumor, which may support the genetically expanded definition of primary malignant giant cell tumor of bone, as originally posited by Amary et al. [6].
In addition, we demonstrated an interesting finding that the H3F3A G34W mutation was absent, either entirely or sub-clonally, in five cases of malignant giant cell tumor of bone, whereas it was present in the associated giant cell tumor tissues. This absence of the mutation was confirmed in all the available specimens using at least two orthogonal methods (i.e., immunohistochemistry coupled with sequencing by one or two different methods). The mutation could not be detected even using pyrosequencing or next generation sequencing techniques that are known to be more sensitive than Sanger sequencing, despite the fact that the tumor cell contents were estimated to be adequate based on H&E sections for all the sequenced tissue samples. Although a few malignant giant cell tumors in which H3F3A mutations were undetected have been reported [15, 25], none of them was studied in detail.
Potential interpretations for this discordant mutation status include: (1) incidental coexistence of two genetically distinct independent tumors (also referred to as a collision when such tumors juxtapose to each other); (2) clonal replacement [26], with a minor population of preexisting H3F3A G34-wild-type clone in giant cell tumor of bone outgrowing an H3F3A-mutant clone; and (3) loss of H3F3A mutation during linear clonal evolution. The very fact that discordance was observed recurrently, accounting for half of the cases, seems incompatible with an incidental coexistence of unrelated tumors. In addition, in cases 4–6, mutation-positive and -negative components presented as a smooth contoured single mass, which does not support the collision theory. Clonal replacement may be possible; however, in all these 5 cases, the giant cell tumor component diffusely expressed the mutant protein without any tangible evidence of a subclone that lacked the mutation, although it is difficult to completely exclude the possibility that rare H3.3 G34W-negative tumor cells might be admixed. The remaining hypothesis of loss of H3F3A mutation during linear clonal evolution is the simplest but unexpected in light of the suspected critical gain-of-function driver role of the H3F3A mutation in giant cell tumor of bone. In many human neoplasms, the early driver mutation lies at the trunk of the phylogenetic tree and is generally preserved after tumor progression [27,28,29].
The mechanism underlying this perplexing discordance would be best clarified by in-depth genetic comparison between mutation-positive and -negative tissues using comprehensive methods such as whole exome sequencing. However, because of the unavailability of fresh frozen specimens and old age of paraffin blocks in many cases, we used FISH to compare H3F3A copy number with mutation status. We showed that absence of H3F3A G34W coincided with relative allelic deletion of H3F3A in 3 out of 4 malignant giant cell tumor cases, whereas H3F3A deletion did not occur in 3 out of 4 cases that harbored H3F3A mutation. Despite the small sample number, these data raise the possibility that the gene deletion occurred in the mutant allele, which would support the theory that H3F3A G34W mutation is lost during clonal evolution. This is reminiscent of a finding reported by Sekine et al. [30], in which two-thirds of adenocarcinomas of the large intestine arising from GNAS-mutant villous adenoma lacked GNAS mutation, with a few of these carcinomas harboring loss of heterozygosity of the GNAS locus. Pusch et al. [31] also reported an exceptional case of IDH1-mutant low-grade astrocytoma, which progressed to glioblastoma showing an IDH1-mutation-negative component with loss of heterozygosity of the IDH1 locus. A recent study has suggested a role for H3F3A G34W in chromatin modulation and RNA processing in giant cell tumor of bone [32], and such downstream oncogenic effects might be compensated or become unnecessary by the acquisition of new driver mutations in malignant giant cell tumor that has lost H3F3A mutation.
Nonetheless, our data cannot provide definitive answers. For case 4, the H3F3A copy number was intact in the H3F3A G34W-negative component. Although copy number neutral mutation loss is a possibility, this case had been previously analyzed by targeted next generation sequencing [15], which showed that the several other mutations in giant cell tumor were also not shared by the sarcoma component. These results could be compatible with the clonal replacement theory that these two components might have arisen from earlier diversification than the acquisition of the H3F3A mutation or the possibility of collision. In contrast, in case 2, the H3F3A deletion was detected in the sarcoma despite the presence of the H3F3A G34W mutation.
In conclusion, we confirmed that malignant transformation of giant cell tumor of bone occurs either de novo or secondarily, in the absence of any prior radiotherapy. Two H3F3A G34W-positive tumors that were not associated with giant cell tumor affected the subarticular sites of young adults, which may support the genetically expanded definition of primary malignant giant cell tumor of bone. We discovered that the H3F3A G34W mutation was absent in a subset of malignant giant cell tumor, a novel recurrent phenomenon that has potential biological and diagnostic implications. The underlying mechanism of this discordance is unknown, although a deletion of the H3F3A gene may play a role in some cases. From a diagnostic standpoint, our findings caution that a discrepant H3F3A mutation status cannot be exclusively relied upon in determining the relationship between giant cell tumor and sarcomas. Further studies are required to better characterize the H3F3A mutation-negative progression pathway of giant cell tumor of bone.
References
Czerniak B. Giant cell lesions. In: Czerniak B, editor. Dorfman and Czerniak’s bone tumors. 2nd edn. Philadelphia: Elsevier; 2016. p. 692–759.
Athanasou NA, Bansal M, Forsyth R, Reid RP, Sapi Z. Giant cell tumour of bone. In: Fletcher CD, Bridge J, Hogendoorn P, et al. editors. Pathology and genetics of tumours of soft tissue and bone. 4th edn. Lyon: IARC Press; 2013. p. 321–4.
Branstetter DG, Nelson SD, Manivel JC, Blay JY, Chawla S, Thomas DM, et al. Denosumab induces tumor reduction and bone formation in patients with giant-cell tumor of bone. Clin Cancer Res. 2012;18:4415–24.
Nascimento AG, Huvos AG, Marcove RC. Primary malignant giant cell tumor of bone: a study of eight cases and review of the literature. Cancer. 1979;44:1393–402.
Al-Ibraheemi A, Inwards CY, Zreik RT, Wenger DE, Jenkins SM, Carter JM, et al. Histologic spectrum of giant cell tumor (GCT) of bone in patients 18 years of age and below: a study of 63 patients. Am J Surg Pathol. 2016;40:1702–12.
Amary F, Berisha F, Ye H, Gupta M, Gutteridge A, Baumhoer D, et al. H3F3A (Histone 3.3) G34W immunohistochemistry: a reliable marker defining benign and malignant giant cell tumor of bone. Am J Surg Pathol. 2017;41:1059–68.
Behjati S, Tarpey PS, Presneau N, Scheipl S, Pillay N, Van Loo P, et al. Distinct H3F3A and H3F3B driver mutations define chondroblastoma and giant cell tumor of bone. Nat Genet. 2013;45:1479–82.
Cleven AH, Hocker S, Briaire-de Bruijn I, Szuhai K, Cleton-Jansen AM, Bovee JV. Mutation analysis of H3F3A and H3F3B as a diagnostic tool for giant cell tumor of bone and chondroblastoma. Am J Surg Pathol. 2015;39:1576–83.
Kato I, Furuya M, Matsuo K, Kawabata Y, Tanaka R, Ohashi K. Giant cell tumours of bone treated with denosumab: histological, immunohistochemical and H3F3A mutation analyses. Histopathology. 2018;72:914–22.
Kervarrec T, Collin C, Larousserie F, Bouvier C, Aubert S, Gomez-Brouchet A, et al. H3F3 mutation status of giant cell tumors of the bone, chondroblastomas and their mimics: a combined high resolution melting and pyrosequencing approach. Mod Pathol. 2017;30:393–406.
Koelsche C, Schrimpf D, Tharun L, Roth E, Sturm D, Jones DT, et al. Histone 3.3 hotspot mutations in conventional osteosarcomas: a comprehensive clinical and molecular characterization of six H3F3A mutated cases. Clin Sarcoma Res. 2017;7:9.
Luke J, von Baer A, Schreiber J, Lubbehusen C, Breining T, Mellert K, et al. H3F3A mutation in giant cell tumour of the bone is detected by immunohistochemistry using a monoclonal antibody against the G34W mutated site of the histone H3.3 variant. Histopathology. 2017;71:125–33.
Noh BJ, Park YK. Giant cell tumor of bone: updated molecular pathogenesis and tumor biology. Hum Pathol. 2018;81:1–8.
Nohr E, Lee LH, Cates JM, Perizzolo M, Itani D. Diagnostic value of histone 3 mutations in osteoclast-rich bone tumors. Hum Pathol. 2017;68:119–27.
Ogura K, Hosoda F, Nakamura H, Hama N, Totoki Y, Yoshida A, et al. Highly recurrent H3F3A mutations with additional epigenetic regulator alterations in giant cell tumor of bone. Genes Chromosomes Cancer. 2017;56:711–8.
Presneau N, Baumhoer D, Behjati S, Pillay N, Tarpey P, Campbell PJ, et al. Diagnostic value of H3F3A mutations in giant cell tumour of bone compared to osteoclast-rich mimics. J Pathol Clin Res. 2015;1:113–23.
Rehkamper J, Steinestel K, Jeiler B, Elges S, Hekeler E, Huss S, et al. Diagnostic tools in the differential diagnosis of giant cell-rich lesions of bone at biopsy. Oncotarget. 2018;9:30106–14.
Righi A, Mancini I, Gambarotti M, Picci P, Gamberi G, Marraccini C, et al. Histone 3.3 mutations in giant cell tumor and giant cell-rich sarcomas of bone. Hum Pathol. 2017;68:128–35.
Yamamoto H, Iwasaki T, Yamada Y, Matsumoto Y, Otsuka H, Yoshimoto M, et al. Diagnostic utility of histone H3.3 G34W, G34R, and G34V mutant-specific antibodies for giant cell tumors of bone. Hum Pathol. 2018;73:41–50.
Sarungbam J, Agaram N, Hwang S, Lu C, Wang L, Healey J, et al. Symplastic/pseudoanaplastic giant cell tumor of the bone. Skelet Radio. 2016;45:929–35.
Joseph CG, Hwang H, Jiao Y, Wood LD, Kinde I, Wu J, et al. Exomic analysis of myxoid liposarcomas, synovial sarcomas, and osteosarcomas. Genes Chromosomes Cancer. 2014;53:15–24.
Tsukamoto Y, Futani H, Kihara T, Watanabe T, Kumanishi S, Matsuo S, et al. An extremely rare case of primary malignancy in giant cell tumor of bone, arising in the right femur and harboring H3F3A mutation. Pathol Res Pr. 2018;214:1504–9.
Emori M, Nagoya S, Sugawara M, Mizushima E, Shimizu J, Murahashi Y, et al. Secondary malignant giant cell tumor of bone with histone H3.3 mutation: a case series. J Orthop Sci. 2018. [Epub ahead of print].
Scheie D, Andresen PA, Cvancarova M, Bo AS, Helseth E, Skullerud K, et al. Fluorescence in situ hybridization (FISH) on touch preparations: a reliable method for detecting loss of heterozygosity at 1p and 19q in oligodendroglial tumors. Am J Surg Pathol. 2006;30:828–37.
Tsukamoto S, Righi A, Vanel D, Honoki K, Donati DM, Errani C. Development of high-grade osteosarcoma in a patient with recurrent giant cell tumor of the ischium while receiving treatment with denosumab. Jpn J Clin Oncol. 2017;47:1090–6.
Caswell-Jin JL, McNamara K, Reiter JG, Sun R, Hu Z, Ma Z, et al. Clonal replacement and heterogeneity in breast tumors treated with neoadjuvant HER2-targeted therapy. Nat Commun. 2019;10:657.
Yates LR, Campbell PJ. Evolution of the cancer genome. Nat Rev Genet. 2012;13:795–806.
Jamal-Hanjani M, Wilson GA, McGranahan N, Birkback NJ, Watkins TBK, Veeriah S, et al. Tracking the evolution of non-small-cell lung cancer. N Engl J Med. 2017;376:2109–21.
Suzuki H, Aoki K, Chiba K, Sato Y, Shiozawa Y, Shiraishi Y, et al. Mutational landscape and clonal architecture in grade II and III gliomas. Nat Genet. 2015;47:458–68.
Sekine S, Ogawa R, Oshiro T, Kanemitsu Y, Taniguchi H, Kushima R, et al. Frequent lack of GNAS mutations in colorectal adenocarcinoma associated with GNAS-mutated villous adenoma. Genes Chromosomes Cancer. 2014;53:366–72.
Pusch S, Sahm F, Meyer J, Mittelbronn M, Hartmann C, von Deimling A. Glioma IDH1 mutation patterns off the beaten track. Neuropathol Appl Neurobiol. 2011;37:428–30.
Lim J, Park JH, Baude A, Yoo Y, Lee YK, Schmidt CR, et al. The histone variant H3.3 G34W substitution in giant cell tumor of the bone link chromatin and RNA processing. Sci Rep. 2017;7:13459.
Acknowledgements
We thank Sachiko Miura, Toshiko Sakaguchi, and Chizu Kina for superb technical assistance. We also thank Dr. Shigeki Sekine for discussion and Dr. Naohiro Makise for support. This study was presented in part at the 107th Annual Meeting of the Japanese Society of Pathology at Sapporo, Hokkaido, in June, 2018. This work was supported in part by the National Cancer Center Research and Development Fund (30-A-2), and JSPS Grant-in-Aid for Young Scientists (18K15108).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yoshida, Ki., Nakano, Y., Honda-Kitahara, M. et al. Absence of H3F3A mutation in a subset of malignant giant cell tumor of bone. Mod Pathol 32, 1751–1761 (2019). https://doi.org/10.1038/s41379-019-0318-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-019-0318-5
This article is cited by
-
Blue lacy matrix in giant cell tumour of bone with or without denosumab therapy
Virchows Archiv (2023)
-
Histological and immunohistochemical features and genetic alterations in the malignant progression of giant cell tumor of bone: a possible association with TP53 mutation and loss of H3K27 trimethylation
Modern Pathology (2022)
-
Aberrant paracrine signalling for bone remodelling underlies the mutant histone-driven giant cell tumour of bone
Cell Death & Differentiation (2022)
-
The epigenomics of sarcoma
Nature Reviews Cancer (2020)
-
Soft Tissue Special Issue: Giant Cell-Rich Lesions of the Head and Neck Region
Head and Neck Pathology (2020)