Abstract
Therapy-related myeloid neoplasm (t-MN) arising in patients with prior cytotoxic treatments is considered a distinct entity due to its unfavorable prognosis. Latencies between the initial cytotoxic therapy and the occurrence of t-MNs vary but usually fall between 1 and 10 years. t-MNs with unusually short or long latencies are not well characterized. It is unclear if they are biologically similar to the ones with ordinary latencies and should be kept in the t-MN entity. We compiled a cohort of t-MN cases including short (<1 year), ordinary (1–10 years), and extended (>10 years) latencies from two tertiary medical centers. Both the t-MNs with ordinary and extended latencies showed high likelihood of high-risk genetic abnormalities and demonstrated no significant survival differences. But the t-MNs with extended latencies were more likely associated with history of multiple cancers (p = 0.007) and were younger at the time of cytotoxic treatments (p < 0.001) when compared to the t-MNs with ordinary latencies. The t-MN with short latencies appears to be a very rare and highly heterogeneous group. In summary, the genetic composition appears similar in the t-MNs with ordinary and extended latencies. However, the association between the t-MN with extended latencies and history of multiple cancers raises a possibility that cancer predisposition may contribute to the accumulation of genetic abnormalities in these patients. Investigation into potential germline mutations in the t-MN patients with extended latencies may provide important information for related family members.
Similar content being viewed by others
Introduction
Based on the current WHO classification, therapy-related myeloid neoplasms (t-MN) encompass myelodysplastic syndrome (MDS), acute myeloid leukemia (AML), and myelodysplastic/myeloproliferative neoplasm (MDS/MPN) arising in patients with prior histories of cytoreductive therapy (either chemotherapy or radiation therapy) for prior neoplastic or non-neoplastic disorders1. t-MNs demonstrate relatively poor prognosis when compared to de novo lesions and are thus deemed a distinct entity2,3,4,5,6.
Prior studies suggest two main subsets of t-MN with corresponding prior treatments3,4,5,7,8. The more common subset associated with alkylating agents and/or radiation therapy tends to occur 5–10 years after exposure and demonstrates chromosome abnormalities involving chromosome 5 and/or 7, complex karyotypes, and TP53 aberrations. The second subset associated with topoisomerase II inhibitors tends to occur with a shorter latency (1–5 years) and demonstrates translocations involving KMT2A at 11q23.3 and RUNX1 at 21q22.1. In reality, it may be difficult to classify patients receiving treatments comprising a mixture of agents and/or radiation into these two specific subsets. Utilizing advanced molecular tools, many studies have shown that t-MN tends to demonstrate adverse genetic abnormalities similar to those seen in other high-risk myeloid neoplasms9,10,11,12,13,14,15.
The incidence of t-MN varies in patients of different types of prior cancers. A population-based study has suggested pronounced relative risk of developing therapy-related acute myeloid leukemia (t-AML) for patients with malignancies of soft tissue, ovary, lung, Hodgkin lymphoma (HL) and myeloma16. However, probably due to the disease prevalence, roughly half of the t-AML patients showed histories of breast cancer and non-Hodgkin lymphoma (NHL). Interestingly, the study also identified variation in risks developing t-AML within the same primary cancer type during the decades of time covered by this population study, which was felt to reflect the changing treatments. The finding also highlights the association between the cytotoxic treatments and the development of t-MNs.
Although t-MN has long been thought to be a complication of the DNA damage caused by the cytoreductive therapy, the observation that not all the patients receiving cytoreductive treatments developed t-MN challenges the postulation that cytotoxic therapy is the only cause for t-MN. The current model of t-MN development highlights the interplay between the intrinsic and extrinsic factors, integrating components such as inherited cancer predisposition, exposure to cytotoxic therapy, clonal selection of cells with somatic mutations (clonal hematopoiesis of indeterminate potential), and damage to the bone marrow stroma niche17.
By definition, any myeloid neoplasm (excluding MPN) occurring in a patient with prior cytotoxic therapy can be considered as t-MN, regardless of the latencies after the exposures to cytoreductive treatments. Although most of the t-MNs appear to develop 1–10 years after the exposure3,4,5,7,8, some patients with t-MNs demonstrate either very short (<1 year) or extended (>10 years) latencies. It is unclear if these t-MNs with unusual latencies are phenotypically and genetically similar to the remaining t-MNs. In this study, utilizing the t-MN cohorts from two tertiary medical centers, we sought to characterize the clinicopathologic features of t-MNs with unusual latencies and compare them with the t-MNs with ordinary latencies that fall between 1–10 years.
Materials and methods
Case selection
t-MN cases were retrieved from the pathology archives at the University of Pittsburgh Medical Center and Weill Cornell Medicine between 2011 and 2020. A review of the clinical records and pathology material was performed. This study was approved by the Institutional Review Boards at both institutions.
Cytogenetic studies
Conventional cytogenetic analysis was performed on G-banded metaphase cells prepared from BM aspirate unstimulated cultures according to the standard protocol18. Twenty metaphases were analyzed, and the results were reported using the ISCN nomenclature19. A complex karyotype was defined as ≥3 chromosomal abnormalities.
Mutation analysis
A polymerase chain reaction (PCR)-based Amplicon target enrichment sequencing assay as well as CEBPA mutation analysis by fragment length analysis were performed as described in a prior study20. The mutation hotspots of the following genes were interrogated: ABL1, ASXL1, BCOR, BCORL1, BRAF, CALR, CBL, CDKN2A, CEBPA, CSF3R, DNMT3A, ETV6, EZH2, FBXW7, FLT3, GATA2, HRAS, IDH1, IDH2, JAK2, KIT, KRAS, MPL, MYD88, NPM1, NRAS, PHF6, PTEN, PTPN11, RUNX1, SETBP1, SF3B1, SRSF2, TET2, TP53, U2AF1, WT1, and ZRSR2. A subset of cases underwent updated sequencing assays with expanded panels, including hotspot regions of additional genes such as ATM, CBLB, KDM6A, KMT2A, NF1, PPM1D, RAD21, and STAG2.
Statistical analysis
Continuous variables were analyzed using standard parametric statistical assays such as the t-test and non-parametric tests such as the Mann–Whitney test as appropriate. Categorical variables were analyzed using the Fisher exact test and the Chi-squared test. Logistic regression analysis was used as appropriate. Survival analysis was performed by the Kaplan–Meier method, and the log-rank test was used to compare survival curves. The time at diagnosis of t-MN was used as the start time point to calculate survival. Statistical analyses were performed using Stata version 15.1 (StataCorp) and GraphPad Prism version 9.0.2 (GraphPad Software).
Results
One hundred and ninety-six cases of t-MN were identified between 2011 and 2020. Our t-MN cohort included one pediatric patient (12 years old) and four young adults (defined as <30 years old). The mean age of the patients at diagnoses was 67 years old (median: 68 years old). The male:female ratio was 1:1.08. Among them, 167/196 patients had histories of chemotherapy, whereas 95/196 patients underwent radiation therapy; 66/196 of the t-MN patients received both chemotherapy and radiation therapy. The morphologic findings classified 108/196 cases as t-MDS or t-MDS/MPN based on the 2017 WHO classification, whereas 88/196 cases were classified as t-AML. Seventy-three of the 108 t-MDS or t-MDS/MPN patients had follow-up bone marrow examinations after the diagnosis of t-MN; 36/73 t-MN patients developed progression into t-AML. Among the cases with documented prior cytoreductive treatments (194/196), the latencies between the patient’s initial cytoreductive therapies and the diagnoses of t-MNs ranged from less than a year to 36 years (Fig. 1). The mean latency was 8.5 years, whereas the median was 6 years (the 5th–95th percentile: 1–26.35 years). In our cohort, a latency of 10 years was estimated to be at the 70th percentile of the distribution.
The box covers values from the 1st quartile to the 3rd quartile. The whiskers cover values outside the box extending to the 5th percentile and the 95th percentile on each end. A latency of 1 year was estimated to be at the 5th percentile, whereas a latency of 10 years was estimated to be at the 70th percentile.
The t-MN cases with documented prior cytotoxic treatments were classified as t-MN-short (with a latency of less than a year), t-MN-ordinary (with a latency over 1–10 years), and t-MN-long (with an extended latency of more than 10 years) based on the common notion that most of the t-MNs occur within 1–10 years after the initial exposure to the cytotoxic treatments. Laboratory and demographic data from each group were summarized in Table 1. Statistical analyses were performed to compare t-MNs with ordinary and long latencies; t-MN-short group was not included in the analyses considering the low number of cases in the group (n = 4). There were no significant differences in the parameters such as male/female ratio, incidence of disease progression as well as history of chemotherapy and/or radiation exposure between the t-MNs with ordinary and extended latencies. The t-MN patients with extended latencies appeared to be older at diagnosis when compared to the patients with ordinary latencies (p = 0.036). Cases of t-MN with short latencies appeared to have higher platelet counts.
In our cohort, complex karyotypes (51%, 98/191) as well as deletions of the long arm/whole chromosome of chromosome 5 and 7 (48%, 84/176) were identified in high percentage of t-MN cases. Other alterations such as chromosome 17p loss (20%, 37/189), translocations involving KMT2A/MLL at 11q23.3 (8%, 14/175), and translocations involving RUNX1 at 21q22.1 (3%, 4/149) were also identified. Similar to that reported in other studies, recurrent chromosome abnormalities associated with favorable prognosis such as t(8;21)(q22;q22); RUNX1-RUNX1T1, inv(16)(p13.1q22); CBFB-MYH11, and t(15;17)(q24;q21); PML-RARA were only identified in low percentage of t-MN cases (1%, 2%, and 2%, respectively). Mutation analyses, using amplicon target enrichment of coding and non-coding regions of the genes recurrently mutated in myeloid neoplasms, demonstrated TP53 mutation as the most common mutation in the cohort (48%, 72/149). NPM1 mutation was seen in only 3% of the t-MN cases (4/149).
Data from the cytogenetic and mutation analysis in t-MNs with different latencies were shown in Table 2 and Fig. 2. In our study, the small number of t-MNs with short latencies appeared to be more likely to show normal karyotypes (3/4) when compared to t-MNs with ordinary latencies (14/133) and extended latencies (9/54). t-MN with ordinary and extended latencies did not demonstrate significant differences in the incidence of cytogenetic abnormalities examined by the chromosome analysis and mutations characterized by the next-generation sequencing assay targeting genes recurrently mutated in myeloid neoplasms.
Colored squares indicate the presence of the specified chromosome abnormality, mutation, or the history of disease/treatment. Different colors are used in different t-MN groups (green: t-MN short; orange: t-MN ordinary; red: t-MN long). Gray squares indicate the absence of the specified aberration or history. White squares indicate that information is not available.
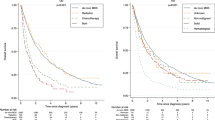
The median survival of the whole t-MN cohort was 11.88 months. In consideration of the limited numbers of t-MNs with short latencies (n = 4), these cases were excluded from the survival analysis shown in Fig. 3. There was no statistically significant difference in overall survival between the t-MNs with ordinary and extended latencies. Excluding the pediatric and young adult patients from the analysis did not alter the results. Though it was unclear if the survival data from the four t-MN patients with short latencies were representative, the 4 t-MN patients with short latencies were all alive at the last follow-up (with a follow-up time ranging from 8 to 60 months). Despite the retrospective nature of the study, there were no statistically significant differences in the percentages of patients receiving induction therapy or bone marrow/stem cell transplant among groups of t-MN with different latencies.
Intriguingly, we found that the patients who had t-MNs with extended latencies were more likely to have histories of multiple cancers (other than the t-MN) (15/56) (vs. 14/136 in t-MNs with ordinary latencies, p = 0.007), more likely to have histories of HL (6/56) (vs. 2/134 in t-MNs with ordinary latencies, p = 0.008) and were likely to be younger at the time of initial cytoreductive treatment (vs. t-MNs with ordinary latencies, p < 0.001) (Table 3). t-MN with extended latencies did not show statistically significant associations with prior histories of carcinoma, NHL and sarcoma when compared to the other t-MN groups. However, in the multivariable logistic regression analysis, t-MNs with extended latencies were only associated with history of multiple cancers and younger age at initial exposure, not history of HL.
In the t-MN patients with histories of multiple cancers, the latencies for development of t-MN ranged from 1 to 32 years with the mean being 12.5 years (median: 12 years). The latency for t-MN in patients with multiple cancers was significantly longer than that seen in the t-MN patients without multiple malignancies (mean: 7.8 years, median: 6 year; p < 0.05 for both parametric and non-parametric tests) (Fig. 4A). When comparing t-MNs undergoing genetic characterization in the patients with and without multiple malignancies, t-MNs in the patients with multiple cancers were more likely to demonstrate BCOR mutations though they were present only in 3 out of 21 cases (vs. 2/123 in patients without multiple cancers; p = 0.02). There were no statistically significant differences in the incidence of other cytogenetic abnormalities and mutations characterized by the target-panel next-generation sequencing assay (Fig. 3). A high percentage of the t-MN patients with histories of multiple cancers had carcinoma (25/29), which was a significantly higher percentage than that in the t-MN patients without multiple cancers (vs. 91/167; p = 0.001). Among the t-MN patients with multiple malignancies, 13/29 patients had histories of breast cancer, 5/29 patients had histories of gynecologic cancers, 3/29 had melanoma and 6/29 patients had non-melanoma skin cancers (Fig. 4B). Regarding the history of cytoreductive treatments, higher percentage of t-MN patients with multiple cancers had histories of both chemotherapy and radiation therapy (15/29), when compared to the patients without multiple cancers (vs. 51/167, p = 0.026). There were no statistically significant differences in the percentage of patients with histories of chemotherapy only or radiation therapy only between the t-MN groups with and without multiple cancers (11/29 vs. 90/167 for CT only; 3/29 vs. 26/167 for RT only).
Among the four cases with t-MNs diagnosed within 1 year of the cytoreductive treatment, one case was an AML with mutated NPM1. One case was a myeloid neoplasm with myeloproliferative and myelodysplastic features showing MPL and SF3B1 mutation. One case with no prior bone marrow examination was diagnosed as t-MN with a complex karyotype. The remaining t-MN case with short latency presented with normal karyotype but 5% blasts at diagnosis. Follow-up bone marrows of this patient demonstrated clonal evolution showing acquired del(7q) and the subsequent presence of a concurrent separate clone with trisomy 1 and der(1;15)(q10;q10).
In an attempt to further characterize the t-MN group with short latencies, we extended the analysis for t-MN-short to include all the cases with latencies less than 2 years (N = 23). The definition of the t-MN-ordinary was modified as t-MNs with latencies of 2–10 years accordingly (N = 117). All the findings described above regarding t-MN-ordinary and t-MN-long groups remain unchanged except for the difference in the age at diagnosis of t-MN, which was no longer statistically significant. Comparing the now expanded short latency group to the remaining t-MNs revealed a new statistically significant association with increased presence of inversion 16 in the expanded t-MN-short group. The number of t-MN cases with inversion 16 was 3/22 (14%) in the expanded t-MN-short group, compared with 1/105 in the t-MN-ordinary group (p = 0.016) and 0/48 in the t-MN-long group (p = 0.028). There were no significant survival differences among the 3 t-MN groups when using 2 and 10 years, instead of 1 and 10 years, to define the t-MNs with short and long latencies (Supplementary Fig. 1). The findings from the re-analysis are summarized as Supplementary Tables 1–3.
Discussion
t-MN is considered a distinct entity based on the WHO classification due to its overall poor prognosis when compared to the de novo lesions2,3,4,5,6. Population studies suggested the majority of the t-MNs occurred within 10 years after the diagnoses of prior malignancies, though patients with extended latencies were also observed11. A prior study utilizing Surveillance, Epidemiology, and End Results data estimated the risk of developing t-MN in a patient with solid tumor peaked at 2 years but returned to the baseline in 10–15 years, while the risk of t-MN in patients with prior hematologic malignancies showed a different time course21. It was hypothesized that the t-MNs with extended latencies might represent random second cancers or second cancers arising in patients with cancer predisposition.
The interesting association between t-MN with extended latencies and history of multiple cancers we identified highlights the potential role of cancer predisposition in the development of these t-MNs. It is known that cancer patients were more likely to have inherited mutations in cancer-associated genes when compared to people without cancer22,23,24. Pathogenic germline mutations in DNA repair genes were identified in a significant portion of the t-MN patients25,26,27 and reportedly increased the risk for subsequent tumors in the patients with childhood malignancies28. Many of the germline mutations identified in the t-MN patients involve DNA damage-sensing, DNA repair, and drug metabolism25,29,30,31,32, which presumably make these patients more susceptible to the DNA damage caused by the cytoreductive treatments. We found a study describing a cohort of 47 patients with t-MN or therapy-related acute lymphoblastic leukemia after breast cancer; the study showed extended latencies between the diagnosis of breast cancer and therapy-related hematologic malignancies in patients with germline BRCA1 or BRCA2 mutations (median 133 months, 30–408 months)25. The finding, together with our results, supports the hypothesis that increased cancer susceptibility contributes to the development of t-MNs with long latencies. Our finding also warrants the investigation for possible germline cancer predisposition in the t-MN patients with long latencies, which can provide important information for the related family members. However, since a similarly extended latency was not observed in the small number of patients with germline mutations in TP53, PALB2, and CHEK2 in the prior study of breast cancer patients with therapy-related hematologic malignancies, the development of t-MNs likely involves various mechanisms in different genetic backgrounds.
t-MN with long latencies, despite their association with multiple cancers, showed comparable genetic features and survival when compared to the t-MNs with ordinary latencies. The similar genetic composition and lack of survival difference did not particularly support the notion to exclude t-MNs with long latencies from the t-MN entity. t-MN, like other malignancies, is the result of a clonal selection process17. Irrespective of the mechanisms generating the genetic aberrations, such as aging, exposure to cytotoxic therapies, and impaired DNA damage response related to cancer predisposition, the genotype in the final selected clone presumptively is one of the most important parameters dictating the prognosis and outcome. Disregarding latencies, it has been reported that although the history of prior cytotoxic treatment disadvantageously impacts the survival in cases with favorable cytogenetic abnormalities6, the negative impact of prior cytotoxic therapy on survival is less pronounced in older patients and in patients with adverse cytogenetics11. The finding likely reflects the fact that both t-MNs and the myeloid neoplasms in the elderly frequently demonstrate high-risk genotypes33,34.
Another interesting finding in our study was that t-MN patients with extended latencies were younger at the time of cytotoxic treatments. Younger age at exposure was implicated in increasing the risk of t-MNs16,35, although confirming a true susceptibility in young individuals is challenging based on the population studies alone, since it is difficult to ascertain that the increased risk is not just a reflection of the lower background incidence of myeloid neoplasms in younger people. The fact that the association between t-MNs with long latencies and HL was no longer significant in the multivariable logistic regression analysis suggested HL may be related to cancer predisposition or the younger age at the diagnosis and treatment for the primary cancers. HL had peak incidence among young individuals and HL was also recognized as one of the malignancies with greater familial risk. For example, the risk of HL with a diseased sibling was higher than the risk of NHL in a similar scenario36,37. In addition, the risk of HL increased if the HL relative was diagnosed at a younger age. This observation, not seen in NHL families, implies a possibly stronger association with cancer predisposition in HL37.
When focusing on t-MN patients with multiple cancers, they showed variable but overall longer latencies than those without multiple malignancies. They were also more likely to have BCOR mutations though these mutations were only identified in a small portion of cases showing different cytogenetic abnormalities and co-mutations. BCOR is a component of the PRC1.1 complex, one of the 6 mammalian Polycomb Repressive Complex-1 catalyzing repressive histone modifications and participating in stemness and differentiation38. It is intriguing to hypothesize that BCOR aberrations are associated with specific cancer predisposition mutations and thus were only identified in a subset of t-MN cases with histories of multiple cancers. The finding that higher percentage of the t-MN patients with multiple cancers had histories of both chemotherapy and radiation therapy may potentially reflect the treatment modalities adopted for different cancers in these patients; but further studies are required to elucidate its potential biologic significance.
Our observations in the t-MN cases with short latency likely highlight the heterogeneity in this rare group of patients. The presence of strong driver mutations (i.e., mutated NPM1, concurrent mutations in MPL and SF3B1 or inversion 16) suggested some genetic similarities to the de novo cases in a subset of t-MN patients with short latencies. In the case presenting with a complex karyotype, the possibility that a pre-existent t-MN stayed undiagnosed until the worsening cytopenia caused by treatment for concurrent malignancy cannot be excluded. The t-MN case that demonstrated clonal evolution after the initial diagnosis may suggest that the t-MN diagnosis was made at a relatively early stage of the disease course, which may be a potential explanation for the short latency in this case. Larger studies are desirable to confirm the findings.
Regarding the limitations of the study, we acknowledge that it is difficult to precisely determine the latencies in t-MNs since the disease may precede the diagnosis. The latencies recorded in our cohort reflected the time these lesions caught clinical attention. However, even without explicit latencies, the observations in our study still offer useful guidance for daily practice considering the information was collected from a comparable clinical setting. Target-panel mutation analysis covering genes recurrently mutated in myeloid neoplasms was used to characterize the t-MN cases in our study. With high-risk genetic abnormalities identified in the majority of the t-MNs, it is less likely that a significant portion of these t-MN cases will show additional critical somatic driver mutations. Future studies with more extensive genetic characterization in t-MNs with different latencies will help uncover potential germline or somatic mutations outside the panel to further elucidate the mechanisms of t-MN development.
In summary, our study demonstrated t-MNs with ordinary and extended latencies showed similar genetic features common in high-risk genotypes. The findings, in conjunction with the absence of significant survival differences, did not support the argument to exclude the t-MNs with long latencies from the t-MN classification. However, the association between the t-MNs with extended latencies and history of multiple cancers highlighted the possibility that increased cancer susceptibility contributed to the genetic abnormalities seen in these lesions. t-MN with short latency likely represents a heterogeneous group with a subset showing features more similar to the de novo lesions.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
Swerdlow S. H., et al (eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (Revised 4th edition). (IARC, Lyon, 2017).
Churpek, J. E. & Larson, R. A. The evolving challenge of therapy-related myeloid neoplasms. Best Pract. Res. Clin. Haematol. 26, 309–317 (2013).
Larson, R. A. Therapy-related myeloid neoplasms. Haematologica 94, 454–459 (2009).
Rowley, J. D. & Olney, H. J. International workshop on the relationship of prior therapy to balanced chromosome aberrations in therapy-related myelodysplastic syndromes and acute leukemia: overview report. Genes Chromosomes Cancer. 33, 331–345 (2002).
Smith, S. M. et al. Clinical-cytogenetic associations in 306 patients with therapy-related myelodysplasia and myeloid leukemia: the University of Chicago series. Blood 102, 43–52 (2003).
Rogers, H. J. et al. Comparison of therapy-related and de novo core binding factor acute myeloid leukemia: A bone marrow pathology group study. Am. J. Hematol. 95, 799–808 (2020).
Kayser, S. et al. The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood 117, 2137–2145 (2011).
Pedersen-Bjergaard, J., Pedersen, M., Roulston, D. & Philip, P. Different genetic pathways in leukemogenesis for patients presenting with therapy-related myelodysplasia and therapy-related acute myeloid leukemia. Blood 86, 3542–3552 (1995).
Kuzmanovic, T. et al. Genomics of therapy-related myeloid neoplasms. Haematologica 105, e98–e101 (2020).
Shih, A. H. et al. Mutational analysis of therapy-related myelodysplastic syndromes and acute myelogenous leukemia. Haematologica 98, 908–912 (2013).
Granfeldt Ostgard, L. S. et al. Epidemiology and clinical significance of secondary and therapy-related acute myeloid leukemia: a National Population-Based Cohort Study. J. Clin. Oncol. 33, 3641–3649 (2015).
Lindsley, R. C. et al. Acute myeloid leukemia ontogeny is defined by distinct somatic mutations. Blood 125, 1367–1376 (2015).
Ok, C. Y. et al. Mutational profiling of therapy-related myelodysplastic syndromes and acute myeloid leukemia by next generation sequencing, a comparison with de novo diseases. Leuk. Res. 39, 348–354 (2015).
Wong, T. N. et al. Role of TP53 mutations in the origin and evolution of therapy-related acute myeloid leukaemia. Nature 518, 552–555 (2015).
Qian, Z. et al. Cytogenetic and genetic pathways in therapy-related acute myeloid leukemia. Chem. Biol. Interact. 184, 50–57 (2010).
Morton, L. M. et al. Evolving risk of therapy-related acute myeloid leukemia following cancer chemotherapy among adults in the United States, 1975-2008. Blood 121, 2996–3004 (2013).
McNerney, M. E., Godley, L. A. & Le Beau, M. M. Therapy-related myeloid neoplasms: when genetics and environment collide. Nat. Rev. Cancer 17, 513–527 (2017).
Mikhail, F. M. et al. Section E6.1-6.4 of the ACMG technical standards and guidelines: chromosome studies of neoplastic blood and bone marrow-acquired chromosomal abnormalities. Genet. Med. 18, 635–642 (2016).
McGowan-Jordan, J. ISCN 2016: An International System for Human Cytogenomic Nomenclature (2016): Recommendations of the International Standing Committee on Human Cytogenomic Nomenclature Including New Sequenc-based Cytogenetic Nomenclature Developed in Collaboraton with the Human Genome Variation Society (HGVS) Sequence Variant Description Working Group. (Karger, 2016).
Rea, B., Aggarwal, N., Yatsenko, S. A., Bailey, N. & Liu, Y. C. Acute myeloid leukemia with isolated del(5q) is associated with IDH1/IDH2 mutations and better prognosis when compared to acute myeloid leukemia with complex karyotype including del(5q). Mod. Pathol. 33, 566–575 (2020).
Radivoyevitch, T. et al. Defining AML and MDS second cancer risk dynamics after diagnoses of first cancers treated or not with radiation. Leukemia 30, 285–294 (2016).
Pritchard, C. C. et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N. Engl. J. Med. 375, 443–453 (2016).
Schrader, K. A. et al. Germline variants in targeted tumor sequencing using matched normal DNA. JAMA Oncol. 2, 104–111 (2016).
Zhang, J. et al. Germline mutations in predisposition genes in pediatric cancer. N. Engl. J. Med. 373, 2336–2346 (2015).
Churpek, J. E. et al. Inherited mutations in cancer susceptibility genes are common among survivors of breast cancer who develop therapy-related leukemia. Cancer 122, 304–311 (2016).
Schulz, E. et al. Germline mutations in the DNA damage response genes BRCA1, BRCA2, BARD1 and TP53 in patients with therapy related myeloid neoplasms. J. Med. Genet. 49, 422–428 (2012).
Voso, M. T. et al. Fanconi anemia gene variants in therapy-related myeloid neoplasms. Blood Cancer J. 5, e323 (2015).
Qin, N. et al. Pathogenic germline mutations in DNA repair genes in combination with cancer treatment exposures and risk of subsequent neoplasms among long-term survivors of childhood cancer. J. Clin. Oncol. 38, 2728–2740 (2020).
Allan, J. M. et al. Polymorphism in glutathione S-transferase P1 is associated with susceptibility to chemotherapy-induced leukemia. Proc. Natl Acad. Sci. 98, 11592–11597 (2001).
Guillem, V. M. et al. Role of MTHFR (677, 1298) haplotype in the risk of developing secondary leukemia after treatment of breast cancer and hematological malignancies. Leukemia 21, 1413–1422 (2007).
Larson, R. A. et al. Prevalence of the inactivating 609C–>T polymorphism in the NAD(P)H:quinone oxidoreductase (NQO1) gene in patients with primary and therapy-related myeloid leukemia. Blood 94, 803–807 (1999).
Link, D. C. et al. Identification of a novel TP53 cancer susceptibility mutation through whole-genome sequencing of a patient with therapy-related AML. JAMA 305, 1568–1576 (2011).
Appelbaum, F. R. et al. Age and acute myeloid leukemia. Blood 107, 3481–3485 (2006).
Bello, C. et al. Outcomes after induction chemotherapy in patients with acute myeloid leukemia arising from myelodysplastic syndrome. Cancer 117, 1463–1469 (2011).
Morton, L. M. et al. Risk of myeloid neoplasms after solid organ transplantation. Leukemia 28, 2317–2323 (2014).
Fallah, M. et al. Familial risk of non-Hodgkin lymphoma by sex, relationship, age at diagnosis and histology: a joint study from five Nordic countries. Leukemia 30, 373–378 (2016).
Kharazmi, E. et al. Risk of familial classical Hodgkin lymphoma by relationship, histology, age, and sex: a joint study from five Nordic countries. Blood 126, 1990–1995 (2015).
Astolfi, A. et al. BCOR involvement in cancer. Epigenomics 11, 835–855 (2019).
Author information
Authors and Affiliations
Contributions
Y.L. and J.G. performed study concept and design; Y.L. and J.G. performed writing, review, and revision of the paper; Y.L., G.I., R.A., B.C., B.R., and J.G. performed acquisition of data; Y.L. performed analysis and interpretation of the data as well as statistical analysis. S.Y. performed the interpretation of the cytogenetic data. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was approved by the Institutional Review Boards at University of Pittsburgh and Weill Cornell Medicine with a waiver of consent. It was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liu, YC., Illar, G.M., Al Amri, R. et al. Therapy-related myeloid neoplasms with different latencies: a detailed clinicopathologic analysis. Mod Pathol 35, 625–631 (2022). https://doi.org/10.1038/s41379-021-00958-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-021-00958-9