Abstract
Background
Biomarkers of exposure to marijuana smoke can be detected in the urine of children with exposure to secondhand marijuana smoke, but the prevalence is unclear.
Methods
We studied children between the ages of 0 to 3 years who were coming in for well-child visits or hospitalized on the inpatient general pediatric unit between 2017 and 2018 at Kravis Children’s Hospital at Mount Sinai. Parents completed an anonymous survey, and urine samples were analyzed for cotinine and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (COOH-THC), a metabolite of Δ9-tetrahydrocannabinol.
Results
Fifty-three children had urine samples available for analysis. COOH-THC was detectable in 20.8% of the samples analyzed and urinary cotinine was detectable in 90.2%. High levels of tobacco exposure (defined as cotinine ≥2.0 ng/ml) were significantly associated with COOH-THC detection (p < 0.01). We found that 34.8% of children who lived in attached housing where smoking was allowed within the property had detectable COOH-THC compared to 13.0% of children who lived in housing where smoking was not allowed at all.
Conclusions
This study adds to the growing evidence that children are being exposed to marijuana smoke, even in places where recreational marijuana use is illegal. It is critical that more research be done on the impact of marijuana smoke exposure on children’s health and development.
Impact
-
We found that 20.8% of the 53 children recruited from Mount Sinai Hospital had detectable marijuana metabolites in their urine.
-
Children with household tobacco smoke exposure and children who lived in attached housing where smoking was allowed on the premises were more likely to have detectable marijuana smoke metabolites.
-
This study adds to the growing evidence that children are being exposed to marijuana smoke, even in places where marijuana remains illegal by state law. As states consider marijuana legalization, it is critical that the potential adverse health effects from marijuana exposure in children be taken into account.
Similar content being viewed by others
Introduction
The adverse health effects of secondhand tobacco smoke exposure are well established; however, information on the prevalence and health effects of secondhand marijuana smoke (SHMS) exposure is limited. As of 5 March 2019, 33 states, the District of Columbia, Guam, and Puerto Rico, have legalized medical use of marijuana, while 11 states and the District of Columbia now allow for the non-medical (recreational) use of marijuana.1,2 According to the 2017 National Survey on Drug Use and Health, 26 million Americans, or 9.6% of the population aged 12 years and older, are current (past month) marijuana users,3 representing a steady increase from 6.9% of the population in 2010 and 8.9% in 2016.4,5
As of 2015, an estimated 5.3–8.0 million US children (~7–11%)6 live with a parent who is a current marijuana user.7 Among US adults, marijuana is most commonly consumed via smoking.8 Since marijuana smoking is generally prohibited in public areas8 and generally confined to the home, young children who spend more time at home are at greater risk for marijuana smoke exposure.9 Studies have demonstrated that secondhand tobacco smoke can leave a potentially harmful chemical residue known as thirdhand smoke that remains on indoor surfaces long after the smoke has cleared from the air.10,11 While research on thirdhand marijuana smoke is limited, a recent study shows that cannabinoids can be detected on surfaces and objects due to deposition of marijuana smoke.12 Thus, it is reasonable to expect that children could be at risk of exposure to marijuana smoke even if smoking occurs when they are not present. A study conducted in Colorado between 2013 and 2015 found detectable levels of marijuana smoke metabolites in 16% of children between the ages of 1 month to 2 years who were hospitalized for bronchiolitis.13
While active marijuana use is associated with some negative health outcomes, including impairments in neurocognitive function14,15,16 and increased risk of respiratory complications,17 the effects of SHMS exposure on children are not well characterized. Studies have demonstrated that marijuana smoke contains many of the same carcinogens and respiratory irritants as tobacco smoke,18 and exposure to marijuana smoke chemicals extends to bystanders.19 Additionally, a study in rats found that even 1 min of SHMS exposure impaired endothelial function for at least 90 min.20
Research data shows that there is a higher prevalence of detectable urinary marijuana smoke metabolites among children whose parents are tobacco smokers than children whose parents are nonsmokers.7,13,21 This raises concern as children with dual exposure to tobacco and marijuana smoke could be at a higher risk for damaging effects of smoke exposure and adverse health outcomes. As secondhand tobacco smoke exposure is highest among low-income individuals, African Americans, and children under the age of 11 years,22 these vulnerable groups may be at higher risk for exposure to smoke from marijuana as well.
Residents of multiunit housing are also at increased risk of secondhand smoke (SHS) exposure from smoking neighbors as SHS can transfer between different units.23,24 In addition, non-smoking residents in housing units that have a partial smoke-free policy are more likely to report SHS incursions than residents in housing units with comprehensive smoke-free policies.25 While those earlier studies focused on SHS exposure resulting from tobacco smoking, marijuana smoking is likely to lead to similar passive exposures to adjacent non-users. A study conducted among Hispanic residents in multiunit housing developments in Los Angeles, California found that while residents perceived SHMS as a health hazard, they were less likely to confront marijuana smokers regarding their smoking than tobacco smokers.26 Thus, building policies and personal beliefs about smoking marijuana may impact resident agency on limiting marijuana smoke exposure through secondhand incursions. In this study, we examine the prevalence of marijuana smoke exposure in children between the ages of 0 to 3 years in the pediatric outpatient and inpatient departments of Mount Sinai Hospital, New York and its association with demographic characteristics, tobacco smoke exposure, and housing policies around smoking.
Methods
Study design
This is a cross-sectional study designed to examine the prevalence of marijuana smoke exposure among young children through both biomarker assessment and self-report questionnaire. The inclusion criteria of the study population included children aged 0 to up to 3 years. All information was collected anonymously, with no means of linking questionnaire data or sample results to the patient or parent. The study was approved by the Mount Sinai Institutional Review Board.
Study recruitment and sample collection
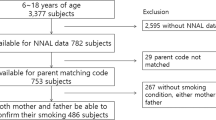
A trained study team member or a member of the patient’s care team recruited children between the ages of 0 to 3 years old from Mount Sinai Pediatric Associates Clinic who were coming in for well-child visits (74%) or hospitalized on the inpatient general pediatric unit (26%) at Mount Sinai Hospital. While Pediatrics Associates is a resident and physician run clinic that primarily serves the surrounding East Harlem community, the inpatient general pediatric unit is a tertiary care center that serves the greater New York City area. The recruitment occurred between July 2017 and November 2018, based on coordinator availability. Fifteen of the 46 (32.6%) families approached in the inpatient general pediatric unit agreed to the study. Seventy-two of the 118 families (61.0%) approached in the Pediatric Associates Clinic agreed to the study. Of the 87 families who agreed to the study, 72 families completed a parent interview as some families left the doctor’s appointment or were discharged before the study was administered. Of the 72 families, sufficient urine for urine analysis was collected from 53 participants. Participants were informed that the study intended to examine marijuana and tobacco exposure in children.
After consent, the study team member and the parent/guardian completed a 14-item questionnaire on demographics and marijuana use in the household. Questions on assessing tobacco/marijuana use and SHS exposure were adapted from a core questionnaire by the American Academy of Pediatrics.27
Participants living in various types of attached housing, including an apartment building, a dormitory or similar boarding house, or a house attached to one or more houses (duplex, triplex, townhouse, or rowhouse), were asked to describe their apartment or attached housing policies around smoking. Housing policies were determined by prompting families to pick from the following options: “smoking is not allowed at all-not even inside individual apartments or units,” “smoking is allowed on the property in shared areas and inside the apartment or units,” “smoking is only allowed inside apartments or units,” “smoking is allowed only outside of the apartments or units, in common areas,” or “there is no policy-smoking is permitted anywhere.”
A urine sample was obtained from the child using a collection bag or cotton balls placed in the child’s diaper. The cotton balls were then removed, and urine was extracted using a syringe. About 2 ml of urine was collected from each participant and stored at −80 °C immediately. These samples were sent to the Centers for Disease Control and Prevention for measuring biomarkers of exposure to marijuana and tobacco smoke.
Analysis of urinary biomarkers of marijuana and tobacco exposure
Cannabinoids and their metabolites were measured using a modification of the method by Wei et al.28 In brief, urine samples were equilibrated with isotopically labeled internal standards, deconjugated by enzymatic and alkaline hydrolysis, and extracted using C18 sorbent. The final extracts were concentrated and 10 μl of each sample was injected into an ultra-high-performance liquid chromatography and analyzed using tandem mass spectrometry (MS/MS) under electrospray ionization mode. This method has limits of detection (LODs) of 0.005, 0.015, and 0.009 ng/ml for Δ9-tetrahydrocannabinol (THC), 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (COOH-THC), and cannabinoid (CBN), respectively. THC and CBN are rapidly metabolized and indicate active or recent exposure, while COOH-THC, a metabolite of THC, has a longer half-life and is a more sensitive measure for detecting intermittent exposure.29 The urinary cannabinoid method was adequately sensitive to detect recent secondhand or thirdhand exposure to marijuana smoke.28
To assess tobacco exposure, urinary total cotinine was measured by isotope dilution high-performance liquid chromatography/atmospheric pressure chemical ionization MS/MS using a modified version of the method of Bernert et al.30 The LOD was 0.030 ng/ml.30
In accordance with Matt et al.,10 who found that urinary cotinine ≥2.0 ng/ml was associated with likely household contact tobacco exposure, we defined high levels of tobacco smoke exposure as a urinary cotinine value ≥2.0 ng/ml and moderate levels of tobacco smoke exposure as cotinine value between 0 and 2.0 ng/ml. As urinary cotinine was detected in 90% of participants, dichotomization using this cutoff allowed for analysis of different factors that might correlate with a high vs. moderate level of tobacco smoke exposure.
Self-reported exposure and other covariates
History of possible marijuana smoke exposure was obtained via questionnaire using the following question, “Does anyone who lives in your home or who cares for your child smoke marijuana?” History of possible exposure to tobacco smoke was obtained using the following question, “Does anyone who lives in your home or who cares for your child smoke tobacco?” We collected demographic information, such as age, sex, and race/ethnicity of the participating children and their parents, and the highest education level attained by the reporting parents. In addition, we asked about housing smoking policy and housing type.
Statistical analysis
Descriptive statistics were summarized using geometric means for biomarker data, mean ± standard deviation (SD) and median for age, and frequency with proportions for categorical variables. Due to the skewed distribution of biomarker data, we also reported the range and geometric mean and its standard deviation. In addition, we dichotomized the marijuana and cotinine biomarkers (≥LOD vs. <LOD), and dichotomized age (≥12 vs. <12 months) as infants <12 months who spend more time within the home may have different levels of smoke exposure.10 Data points with values below the LOD in COOH-THC (79.2%, LOD = 0.015 ng/ml) and cotinine (10%, LOD = 0.030 ng/ml) were replaced by LOD/√2. We calculated the Pearson’s correlation coefficient between natural log-transformed COOH-THC and natural log-transformed cotinine. We used Fisher’s exact tests to examine associations between marijuana exposure (dichotomized by LOD) and demographic, self-reported exposure, as well as housing smoking policies and housing type. No corrections for multiple comparisons were included in this pilot study. Results were considered significant if p ≤ 0.05.
Our sample size is small, and thus we may not have had the power to detect important associations. For example, our post hoc analysis showed that while we were sufficiently powered (power = 92%) to differentiate detectable COOH-THC levels between black and non-black groups, we were underpowered (power < 50%) to differentiate detectable COOH-THC levels between those with and without tobacco smoking exposure.
Results
Eighty-seven out of 164 families approached agreed to participate the study, representing 53.0% of all potential participants approached by the study team. The recruitment rate was significantly lower among families who were approached in the inpatient unit (32.6%) compared to families who were approached in the outpatient clinic (61.0%). In cases where a trained study coordinator approached families, the reason for refusal to participate was recorded. Reasons for refusing to participate included time restraints, concerns about using the urine bag, the topic of marijuana and tobacco smoke exposure and ongoing child discomfort in the inpatient setting.
Of the 72 subjects enrolled in the study, 53 (73.6%) subjects were able to provide a urine sample without fecal contaminants. Of these, 56.6% were male and 43.4% were female (Table 1). Most (66.0%) identified as being of Hispanic or Latino ethnicity; 32.1% identified as black and/or African American, 32.1% identified as being multi-racial, 7.5% identified as Asian or Pacific Islander, and 32.1% identified as “other.” The mean age of the children at time of enrollment was 9.8 months (SD = 7.5, median = 8 months). Approximately 62.3% of caregivers surveyed had attended some college or technical school (Table 1).
THC and CBN were detected in urine of two (3.8%) patients. COOH-THC was detected in urine from 11 (20.8%) patients. The range in COOH-THC concentration was 0.017–0.678 ng/ml. The geometric mean of COOH-THC levels was 0.16 ± 1.40 ng/ml. Of the caregivers surveyed, 15.1% reported marijuana use by a caregiver in the home and 30% reported tobacco use (Table 2).
Of the 53 participants with urine samples, 51 (96.2%) subjects had sufficient remaining urine for analysis for cotinine levels. Forty-six (90.2%) had detectable urinary cotinine levels ranging from 0.045 to 19.4 ng/ml with a geometric mean of 0.77 ± 2.23 ng/ml. Fifteen (29.4%) had urinary cotinine ≥2.0 ng/ml, suggesting high levels of tobacco smoke exposure.10 High levels of tobacco smoke exposure (cotinine ≥ 2.0 ng/ml) was significantly associated with COOH-THC detection in urine (Table 3). The Pearson’s correlation coefficient between COOH-THC and cotinine was 0.5 (p = 0.0001).
Fifty (94.3%) families reported living in an apartment or other attached housing. Half of families living in attached housing who were aware of their housing smoking polices reported that smoking is not allowed at all (Table 4). Children who lived in attached housing where smoking was allowed within the property were almost three times more likely to have detectable urinary COOH-THC levels than children who lived in attached housing where smoking was not allowed at all (Table 4).
Discussion
Approximately one-fifth of the children enrolled in the study had detectable marijuana metabolites in their urine. This is comparable to exposure rates of 16% among children between the ages of 0 to 2 years hospitalized in Colorado,13 where recreational marijuana is legalized, indicating that children are being exposed to marijuana smoke even where marijuana is not legal under state law. Of the participants, 90.2% had detectable urinary cotinine levels, while 30.2% reported living in a home in which someone smokes tobacco. This is consistent with previous research demonstrating biochemical evidence of tobacco smoke exposure in a majority of children who live in homes where no one smokes, and increased risk of exposure among children who live in multiunit housing.31
Of the caregivers surveyed, 15.1% reported marijuana use by a caregiver at home. There was no correlation between COOH-THC levels and caregiver report of marijuana use within the household. This could represent underreporting of household marijuana use due to social desirability bias. As possession and non-medical use of marijuana is a punishable offense in the state of New York,32 caregivers might be hesitant to report use. Alternatively, children could also have detectable COOH-THC levels due to exposure to external sources of marijuana smoke such as marijuana smoke incursions from neighbors.
Cotinine levels ≥2.0 ng/ml, which indicates high levels of tobacco smoke exposure, were significantly correlated with detectable COOH-THC levels. This correlation is consistent with previous studies, which demonstrate that children exposed to tobacco smoke are more likely to be exposed to marijuana smoke.7,13 More research is needed to study the effects of dual tobacco and marijuana and tobacco smoke exposure on children’s development and health outcomes.
Approximately 94.2% of the families surveyed reported living in an apartment or other attached housing. When asked about their apartment or attached housing policies on smoking, half of the families surveyed picked the option “smoking is not allowed at all-not even inside individual apartments or units.” The other half indicated that smoking was allowed on the property to some extent. Children who lived in attached housing where smoking was allowed were nearly three times more likely to have detectable COOH-THC levels. This is consistent with previous research which demonstrates that residents of multiunit housing are at increased risk of secondhand tobacco smoke exposure from their neighbors.20,21 This has important public health implications as children who live in multiunit housing where smoking is allowed might have an increased risk of marijuana smoke exposure, as we know they do for tobacco smoke exposure.25
Further research is needed to assess the impact of smoking policies on exposure by assessing factors such as the frequency of marijuana smoke incursions within homes. Despite legalization at the state level, marijuana is currently illegal according to federal law and defined as a Schedule I drug or a “substance with a very high potential for abuse and no accepted medical use in the United States.”33 Currently, the US Department of Housing and Urban Policy (HUD) prohibits marijuana use in federally subsidized buildings34 and as of 30 July 2018, requires implementation of a smoke-free policy in public health agency homes.35 In a study conducted in 2017 among public housing residents in New York City, residents reported equal prevalence of marijuana and tobacco smoke exposure within their buildings and expressed skepticism regarding HUD’s capacity to enforce a smoke-free policy.36 More research is necessary to determine the implications of this mandated smoke-free housing policy on the prevalence tobacco and marijuana smoke exposure in public housing.
Our study has several limitations. Due to our small sample size, we may not have had the power to detect important associations. Nonetheless, results from this pilot study provided information for sample size and power calculation needed for planning future studies. Another possible limitation of this study is the potential for selection bias in the recruitment process. Fifty-three percent of all potential participants approached by the study team agreed to participate in the study. As potential participants were informed of the study’s objective of assessing marijuana and tobacco smoke exposure in children, it is possible that families who use tobacco and/or marijuana were less likely to participate. We used parent report for many of the variables, including household marijuana use, and parents may not have responded accurately. Another potential limitation is that our findings could underestimate SHMS exposure because we included only health-seeking families in the study.
Finally, our results may not be generalizable outside this convenience sample of children in New York City. Seventy-four percent of study participants were recruited from the Pediatrics Associates clinic, which primarily serves the surrounding East Harlem community. East Harlem has a predominantly black and Hispanic population, in which 31% of residents live below the federal poverty level and 75% of all homes are regulated by a government agency.37 Additionally, a 2015 community health report demonstrated that East Harlem has a significantly higher prevalence of housing maintenance defects, poorer air quality, and higher rate of child asthma hospitalizations compared to other neighborhoods in New York City.38 The study also showed that SHMS exposure was significantly associated with self-identified black race. Given that secondhand tobacco smoke exposure is higher among low-income individuals, African Americans, and children, it is especially important to assess SHMS exposure in such vulnerable populations.22 Given that a fifth of children in the study had detectable urine marijuana smoke metabolites, future studies that examine associations between SHMS and child health and development outcomes are crucial.
This study adds to the growing evidence that children are being exposed to marijuana smoke, even in places where marijuana remains illegal by state law. As states consider marijuana legalization, it is critical that the potential adverse health effects from marijuana exposure in children be taken into account, and more research must be done on the impact of marijuana smoke exposure on children’s health and development. In addition, it will be critical to understand how housing policies around smoking affect children’s exposure to marijuana and tobacco smoke.
References
State Medical Marijuana Laws. 3/5/2019 ed. ncsl.org: National Conference of State Legislatures.
State Marijuana Laws in 2019 Map. https://www.governing.com/gov-data/safety-justice/state-marijuana-laws-map-medical-recreational.html (2019).
Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53) (Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, 2017).
Sacco, L. N., Bagalman, E., Finkela, K. & Lowry S. The Marijuana Policy Gap and the Path Forward (Library of Congress. Congressional Research Service, 2017).
Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2015 National Survey on Drug Use and Health http://www.samhsa.gov/data/ (2016).
Bureau USC. Estimates of the population of the United States by single years of age, color, and sex: 1900 to 1959 (Series P-25, No. 311); Estimates of the population of the United States, by age, sex, and race: April 1, 1960, to July 1, 1973 (Series P-25, No. 519); Preliminary estimates of the population of the United States by age, sex, and race: 1970 to 1981 (Series P-25, No. 917); and Intercensal estimates for 1980–1989, 1990–1999, and 2000–2009 https://www.childstats.gov/americaschildren/tables/pop1.asp (2018).
Goodwin, R. D. et al. Trends in cannabis and cigarette use among parents with children at home: 2002 to 2015. Pediatrics 141 (2018). https://doi.org/10.1542/peds.2017-3506.
Pepin, D., Hoss, A., Schauer, G. L. & Holmes, C. B. Public use of recreational marijuana: a legal landscape of state law. Seton Hall Legis. J. 41, 283–303 (2016).
Posis, A. et al. Indoor cannabis smoke and children’s health. Prev. Med. Rep. 14, 100853 (2019).
Matt, G. E. et al. Households contaminated by environmental tobacco smoke: sources of infant exposures. Tob. Control 13, 29–37 (2004).
Jacob, P. 3rd et al. Thirdhand smoke: new evidence, challenges, and future directions. Chem. Res. Toxicol. 30, 270–294 (2017).
Sempio, C. et al. Surface detection of THC attributable to vaporizer use in the indoor environment. Sci. Rep. 9, 18587 (2019).
Wilson, K. M. et al. Detecting biomarkers of secondhand marijuana smoke in young children. Pediatr. Res. 81, 589–592 (2017).
Tortoriello, G. et al. Miswiring the brain: Delta9-tetrahydrocannabinol disrupts cortical development by inducing an SCG10/stathmin-2 degradation pathway. EMBO J. 33, 668–685 (2014).
Meier, M. H. et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc. Natl Acad. Sci. USA 109, E2657–E2664 (2012).
Volkow, N. D., Baler, R. D., Compton, W. M. & Weiss, S. R. Adverse health effects of marijuana use. N. Engl. J. Med. 370, 2219–2227 (2014).
Tetrault, J. M. et al. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch. Intern. Med. 167, 221–228 (2007).
Moir, D. et al. A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chem. Res. Toxicol. 21, 494–502 (2008).
Cone, E. J. et al. Non-smoker exposure to secondhand cannabis smoke. I. Urine screening and confirmation results. J. Anal. Toxicol. 39, 1–12 (2015).
Wang, X. et al. One minute of marijuana secondhand smoke exposure substantially impairs vascular endothelial function. J. Am. Heart Assoc. 5 (2016). https://doi.org/10.1161/JAHA.116.003858.
Wilson, K. M. et al. Marijuana and tobacco coexposure in hospitalized children. Pediatrics 142 (2018). https://doi.org/10.1542/peds.2018-0820.
Homa, D. M. et al. Vital signs: disparities in nonsmokers’ exposure to secondhand smoke—United States, 1999–2012. MMWR Rep. 64, 103–108 (2015).
King, B. A., Travers, M. J., Cummings, K. M., Mahoney, M. C. & Hyland, A. J. Secondhand smoke transfer in multiunit housing. Nicotine Tob. Res. 12, 1133–1141 (2010).
Kraev, T. A., Adamkiewicz, G., Hammond, S. K. & Spengler, J. D. Indoor concentrations of nicotine in low-income, multi-unit housing: associations with smoking behaviours and housing characteristics. Tob. control 18, 438–444 (2009).
Wilson, K. M. et al. Tobacco smoke incursions in multiunit housing. Am. J. Public health 104, 1445–1453 (2014).
Rendon, A. D., Unger, J. B., Cruz, T., Soto, D. W. & Baezconde-Garbanati, L. Perceptions of secondhand and thirdhand smoke among hispanic residents of multiunit housing. J. Immigr. Minor. Health 19, 162–169 (2017).
Secondhand Tobacco Smoke Exposure (SHS) and Use Items. https://doi.org/https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Richmond-Center/_layouts/15/WopiFrame.aspx?sourcedoc=/en-us/advocacyand-policy/aap-health-initiatives/Richmond-Center/Documents/SHSExposure.doc&action=default.
Wei, B., Wang, L. & Blount, B. C. Analysis of cannabinoids and their metabolites in human urine. Anal. Chem. 87, 10183–10187 (2015).
Goodwin, R. S. et al. Urinary elimination of 11-nor-9-carboxy-delta9-tetrahydrocannnabinol in cannabis users during continuously monitored abstinence. J. Anal. Toxicol. 32, 562–569 (2008).
Bernert, J. T., Harmon, T. L., Sosnoff, C. S. & McGuffey, J. E. Use of continine immunoassay test strips for preclassifying urine samples from smokers and nonsmokers prior to analysis by LC-MS-MS. J. Anal. Toxicol. 29, 814–818 (2005).
Wilson, K. M., Klein, J. D., Blumkin, A. K., Gottlieb, M. & Winickoff, J. P. Tobacco-smoke exposure in children who live in multiunit housing. Pediatrics 127, 85–92 (2011).
New York State Law. Consolidated Laws of New York’s Penal code (2019).
US Drug Enforcement Administration. Drug scheduling (2020). https://www.dea.gov/druginfo/ds.shtml.
Metclaf, B. T. Use of Marijuana in Multifamily Assisted Properties (US Department of Housing and Urban Developlment, 2014).
US Department of Housing and Urban Development. Implementing HUD’s smoke-free policy in public housing: HUD guidebook https://www.hud.gov/sites/documents/SMOKEFREE_GUIDEBK.PDF (2017).
Jiang, N., Thorpe, L., Kaplan, S. & Shelley D. Perceptions about the federally mandated smoke-free housing policy among residents living in public housing in New York City. Int. J. Environ. Res. Public Health 15 (2018). https://doi.org/10.3390/ijerph15102062.
Housing New York. East Harlem Housing Plan (Office of Neighborhood Strategies, NYC Department of Housing Preservation & Development, 2018).
King, L. H. K. et al. Community Health Profiles 2015 1–16 (Manhattan Community District 11, East Harlem, 2015).
Acknowledgements
This work was supported by the Children’s Center Foundation and the Icahn School of Medicine at Mount Sinai. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
K.M.W. conceptualized the study, supervised the data collection and analyses, and critically revised the manuscript for important intellectual content; L.S. contributed to data collection, analyzed the data, and drafted the manuscript; B.L. oversaw the data analysis and critically revised the manuscript for important intellectual content; T.B. contributed to data collection, contributed to the manuscript, and critically revised the manuscript for important intellectual content; L.W. oversaw laboratory analysis, and critically revised the manuscript for important intellectual content; L.Z. oversaw laboratory analysis, and critically revised the manuscript for important intellectual content; C.S.S. oversaw laboratory analysis, and critically revised the manuscript for important intellectual content; B.C.B. oversaw laboratory analysis, and critically revised the manuscript for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent was obtained; the study was approved by the Institutional Review Board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sangmo, L., Braune, T., Liu, B. et al. Secondhand marijuana exposure in a convenience sample of young children in New York City. Pediatr Res 89, 905–910 (2021). https://doi.org/10.1038/s41390-020-0958-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0958-7
This article is cited by
-
Prenatal Exposure to Cannabis: Effects on Childhood Obesity and Cardiometabolic Health
Current Obesity Reports (2024)
-
Perception of pregnant individuals, health providers and decision makers on interventions to cease substance consumption during pregnancy: a qualitative study
BMC Public Health (2024)
-
Consensus recommendations on dosing and administration of medical cannabis to treat chronic pain: results of a modified Delphi process
Journal of Cannabis Research (2021)