Abstract
Background
The pathogenesis of neonatal meconium aspiration syndrome (MAS) involves meconium-induced lung inflammation and surfactant inactivation. Bronchoalveolar lavage (BAL) with diluted surfactant facilitates the removal of meconium. CHF5633, one of the most promising synthetic surfactants, is effective in neonatal respiratory distress syndrome. Here we investigated its efficacy via BAL in an experimental MAS model.
Methods
Experimental MAS was induced at birth in near-term newborn rabbits by intratracheal instillation of reconstituted human meconium. First, undiluted CHF5633 was compared with a porcine-derived surfactant (Poractant alfa) via intratracheal bolus (200 mg/kg). Second, the efficacy of BAL with diluted CHF5633 (5 mg/mL, 20 ml/kg) alone, or followed by undiluted boluses (100 or 300 mg/kg), was investigated.
Results
Meconium instillation caused severe lung injury, reduced endogenous surfactant pool, and poor survival. CHF5633 had similar benefits in improving survival and alleviating lung injury as Poractant alfa. CHF5633 BAL plus higher boluses exerted better effects than BAL or bolus alone in lung injury alleviation by reversing phospholipid pools and mitigating proinflammatory cytokine mRNA expression, without fluid retention and function deterioration.
Conclusions
CHF5633 improved survival and alleviated meconium-induced lung injury, the same as Poractant alfa. CHF5633 BAL plus boluses was the optimal modality, which warrants further clinical investigation.
Impact
-
To explore the efficacy of a synthetic surfactant, CHF5633, in neonatal lung protection comparing with Poractant alfa in a near-term newborn rabbit model with meconium-induced lung injury.
-
Similar effects on improving survival and alleviating lung injury were found between CHF5633 and Poractant alfa.
-
Optimal therapeutic effects were identified from the diluted CHF5633 bronchoalveolar lavage followed by its undiluted bolus instillation compared to the lavage or bolus alone regimens.
-
Animals with CHF5633 lavage plus bolus regimen exerted neither substantial lung fluid retention nor lung mechanics deterioration but a trend of higher pulmonary surfactant-associated phospholipid pools.
Similar content being viewed by others
Introduction
Meconium aspiration syndrome (MAS) is a severe complication of intrauterine distress and intrapartum asphyxia, especially in term or post-term newborns, which often leads to respiratory failure, and requires critical care to survive.1,2 However, in neonatal intensive care units with limited resources, access to advanced supportive therapies such as extracorporeal membrane oxygenation (ECMO) is generally lacking or very limited.3 It incurs the high case-fatality rate of MAS4 and increased risks of long-term consequences of chronic respiratory and neurodevelopmental morbidities in survivors.5,6 Therefore, seeking more cost-effective and applicable therapies at early postnatal life should be imperative to reverse the adverse outcome of intractable MAS in perinatal–neonatal perspectives.
Airway obstruction, chemical pneumonia, persistent hypoxemia and pulmonary hypertension, and inactivation of endogenous pulmonary surfactant (PS) are the critical pathophysiological mechanisms of MAS.1,2,7 As reported, the components of meconium such as bile salts may directly inactivate PS, i.e., fragmentation of dipalmitoylphosphatidylcholine (DPPC), other surfactant phospholipids, and surfactant proteins.7 Meconium also induces dissolution of tight junctions, apoptosis and necrosis of type I and type II pneumocytes, disrupts the alveolar–capillary barrier, and synthesis of endogenous surfactant.1,2 Furthermore, meconium-induced inflammation, oxidative stress, and edema may aggravate lung injury and indirectly damage PS.2,7 Since the early 1990s, many clinical studies have reported the effects of various PS preparations in MAS.8,9,10,11,12,13,14 An updated systemic review suggested that PS administration may reduce the severity of respiratory failure in MAS patients by decreasing ECMO support and length of hospital stay.15 However, no solid evidence has been disclosed to improve survival.8,9,10,11,12,13,14,15 A gap remains from bench to bedside regarding translational improvement in technology toward clinical applicability of PS in the context of animal model-based efficacy.16,17,18,19,20
Although the rationales are sound, in clinical practice, the efficacy of PS in MAS may vary due to different types, dosages, administration modalities, and adjunct therapies.1,3,8,9,10,11,12,13,14,15 The most widely used surfactant preparations in neonatal respiratory distress syndrome (RDS) are animal lung-derived natural PS (nPS).15,21,22,23 However, due to their complex preparation procedure, high costs, batch-to-batch variability,21,23 and less resistance to inactivation by leaking plasma proteins,24 developing a more cost-effective synthetic PS (sPS) is long sought. As for the surfactant delivery maneuver in administration for MAS, there existed mainly two ways.8,9,10,11,12,13,14,15,16,17,18,19,20,21,22 Bolus surfactants via endotracheal tube are the most commonly used ones.8,9,10,14,15,16,17,18 Bronchoalveolar lavage (BAL) with diluted surfactants is developed as an alternative, with the advantage of removing meconium particles from airways or alveoli.11,12,13,19,20,22
The new generation of sPS, CHF5633, contains phosphatidylcholine, phosphatidylglycerol, and is enriched with peptide analogs of the hydrophobic human surfactant proteins B (SP-B) and C (SP-C),25,26,27 with resistance to inactivation and efficacy in both in vivo and in vitro pre-clinical studies.25,26,27,28,29,30 Preliminary but promising results from clinical trials with CHF5633 for treating preterm infants with RDS also indicate favorable toleration, short- and long-term safety, and a profile similar to Poractant alfa.31,32,33 However, the overall efficacy and recommended use of CHF5633 in MAS have not been assessed clinically.
Thereupon, we established a ventilated near-term newborn rabbit model with acute lung injury and respiratory failure induced by meconium aspiration. We explored the efficacy of CHF5633 in two phases of experiments. First, we compared the efficacy of CHF5633 with a widely used nPS, Poractant alfa. Next, we compared the optimal administration route of CHF5633 through a dilution in BAL or BAL plus bolus, in contrast to bolus instillation only. We assumed that CHF5633 should have equivalent or non-inferior benefits to Poractant alfa, and BAL plus bolus regimen might be a relevant optimal method of CHF5633 for the treatment of MAS.
Materials and methods
Animals, meconium, and surfactants
The study protocol was approved by the Ethics Committees of Children’s Hospital of Fudan University (No.2019195). Thirty-eight healthy New Zealand White rabbit at 30 days of gestation (term 31 days) were obtained from Shanghai Songlian Experimental Animal Center. Does were sedated and underwent anesthesia and cesarean delivery.34,35 There were 307 newborn rabbits together for the whole study.
Fresh human meconium samples, kindly donated from several healthy term newborn babies, were mixed, lyophilized, and stored at −20 °C. When in use, it was ground, suspended with saline to 50 mg dry weight/mL,16,17,18,19,20,29 and instilled intratracheally at birth at a dosage of 4 mL/kg body weight (BW) to induce respiratory failure and lung injury, according to our pilot experiment and previously reported experience.16,17,18,19,20,29
All surfactants were supplied by Chiesi Pharmaceuticals, Parma, Italy. The sPS CHF5633 contains DPPC and 1-palmitoyl-2-oleoylglycero-3-phospho-1-glycerol (POPG) at 1:1 ratio (98.3%) and peptide analogs of SP-B (1.5%) and SP-C (0.2%), with phospholipid concentration of 80 mg/mL.23,25,26,27 The nPS Poractant alfa (Curosurf®) was a commercially available preparation from porcine lung extraction with almost exclusively polar lipids (about 70% of the total phospholipid content) and about 1% of SP-B and SP-C, with 80 mg phospholipid/mL.21,23
Ventilated animal model with MAS
After birth, rabbit pups were immediately intraperitoneally anesthetized, tracheotomized, and received meconium suspension via metal tracheal cannulas, with other littermates instilled with an equivalent dose of saline as control. Then pups were connected to a ventilator multi-plethysmograph system to enable parallel mechanical ventilation (MV) of 12 animals.34,35,36 The ventilator (Servo 900C, Siemens-Elema, Solna, Sweden) was set at a fraction of inspired oxygen (FiO2) 1.0, 40 breaths/min, 1:2 inspiratory/expiratory ratio, and 2–3 cmH2O positive end-expiratory pressure (PEEP). The peak inspiratory pressure (PIP) was adjusted individually to achieve a tidal volume (Vt) of 4–6 mL/kg BW, measured by a pneumotachometer (series 8421, RSS100-HR, Hans Rudulph, Inc., Kansas, KA). The parameters were monitored by an automated physiologic monitoring system (PowerLab, ADInstruments Pty Ltd, New South Wales, Australia). Time 0 was set when individual pups were connected to the ventilator and ventilation commenced. A mixed solution of glucose, bicarbonate and analgesic was given in 0.1 mL intraperitoneally every 1.5–2 h to each pup.34 During the ventilation period of 10 h, the box of the plethysmograph was warmed by a heating pad to maintain animal body temperature.
Experimental phases and surfactant regimens
In Experimental Phase I, a bolus of 2.5 mL/kg of saline, Poractant alfa (200 mg/kg) or CHF5633 (200 mg/kg) was administered endotracheally 1 h after the instillation of meconium, which were accordingly named as: MAS (meconium aspiration), NS200 (one-bolus Poractant alfa), SS200 (one-bolus CHF5633). Those with CHF5633 treatment at 1 h and further received an additional 200 mg/kg dose at 3 h were grouped as SS400 (two-bolus CHF5633). Animals in the Saline group were only treated with 4 mL/kg saline at birth.
In Experimental Phase II, animals with meconium aspiration were treated with diluted CHF5633 (5 mg/mL, 20 mL/kg) for BAL at 1 h of ventilation. The procedure of BAL was adapted from ref. 19 with details in Supplementary eMethod 1. Animals completed with BALs were given either null treatment, or a bolus of undiluted sPS at 100 mg/kg (1.25 mL/kg at 15 min after lavage), or 300 mg/kg (1.25 mL/kg at 15 min after lavage plus 2.5 mL/kg at 3 h of ventilation). They were denoted as SSL (CHF5633 lavage), SSL100 (CHF5633 lavage plus one-bolus), SSL300 (CHF5633 lavage plus two-bolus) group, whereas Saline, MAS, and SS200 groups were set concurrently as in the Phase I protocol.
In both phases, all animals were randomized for the intervention, and each group should have at least 24 animals to ensure subsequent lung sample processing for either histopathological or biochemical measurements with sample size ≥8. Besides, several animals were immediately euthanized after birth by intracranial injection of 0.5 mL 2% lidocaine,34,35,36 to serve as unventilated control group (C0) for biochemical measurements.
Measurement of lung mechanics, survival status
Parameters of lung mechanics (PIP, PEEP, Vt) were recorded at 5, 15, 30, 45, 60, and hourly to 600 min, or ceased at last recording prior to early death. Dynamic compliance of the respiratory system (Cdyn, mL/kg/cmH2O) was calculated by Vt/BW/(PIP − PEEP) at each time point. Meconium-induced lung injury, i.e., experimental MAS model, was defined as >30% reduction of Cdyn within 60 min of ventilation compared to the Saline group, as previously reported.16,17,18,19,20 Color of lips, limbs, trunks, and precordium pulsation as a sign of heartbeat were closely visualized to determine animal survival status.34,35 Those animals still alive after 10-h ventilation were sacrificed. The survival time of all animals was recorded. Pneumothorax (PTX) and sex was inspected through anatomical observation. Right ventricular heart blood was collected for serum lactate (LA) measurement with a commercial testing kit (Nanjing Jiancheng Bioengineering Institute, Nanjing, China).
Lung sample processing
Both lungs of animals were randomly allocated for either histopathological or biochemical measurements. The accessory lobe of the right lung was removed to measure the wet-to-dry weight ratio (W/D) to estimate fluid content in the whole lung tissue.34,35
Lung histopathology
In each group, both right and left lungs from approximately half numbers were fixed en bloc for hematoxylin–eosin staining and semi-quantitative evaluation of lung injury score (LIS), alveolar expansion (Vv), and coefficient of variation of alveolar expansion [CV(Vv)] as described elsewhere.34,35
Biochemical analysis
For those pups assigned to biochemical analysis, the left lung (no PTX) was processed with cold saline lavage by 15 mL/kg BW, three times, and BAL fluid (BALF) was pooled and the volume was measured.35 After BAL, the lung tissue was homogenized. Both BALF and lung tissue homogenate (LH) were subjected to identical extraction through quantitative measurements of total phospholipids (TPL) and disaturated phosphatidylcholine (DSPC)37,38 with correction by BALF volume and BW35 (details in eMethod 2). Total proteins (TP) were quantified by BCA kit (Pierce BCA Assay Kit 23225, Thermo Scientific, Rockford, IL). The activity of secretory phospholipase A2 (sPLA2) in BALF, a key enzyme for surfactant degradation,7 was detected according to the kit manual (ADI-907-002, Enzo Life Sciences, Inc., Farmingdale, NY, www.enzolifesciences.com).
A part of the right lung tissue was homogenized for biochemical analyses of malondialdehyde (MDA), glutathione (GSH), activities of myeloperoxidase (MPO), and superoxide dismutase (SOD) by corresponding kits (Nanjing Jiancheng Bioengineering Institute, Nanjing, China).
Quantification of mRNA expression by quantitative PCR (qPCR)
The rest of the right lung tissue was used to measure mRNA expression by qPCR analysis by Roche LightCycler 480 II (Roche, Basel, Switzerland). Sequence information of target mRNA genes was obtained from nucleotide databases (www.ncbi.nlm.nih.gov/gene/), and the primers were designed by Sangon Biotech (Shanghai, China). These genes were categorized as: (1) inflammatory mediators, including toll-like receptor (TLR)-4, nuclear transcription factor-kappa B (NF-κB, subunit p50), tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6, IL-8, IL-10, intracellular adhesion molecule-1, inducible nitric oxide synthase; (2) surfactant proteins (SP-A, B, C, D) and cytidine triphosphate:phosphocholine cytidylyltransferase (CCT); (3) growth factors (GFs): insulin-like GF (IGF)-1, IGF-2, vascular endothelial GF, and keratinocyte GF. The amplification reaction was carried out in 10 μL volume containing 5 μL SYBR®Premix Ex Taq™ (Takara Bio Inc., Otsu, Shiga, Japan). The mRNA expression of each gene was normalized to β-actin, with ΔΔCT method for calculating mean fold changes. All primer sequences are listed in Supplementary eTable 1.
Statistical analysis
All statistical comparisons were performed by the SPSS software (version 23.0, IBM, Armonk, NY) with figures produced by GraphPad Prism (version 6.02, GraphPad Software, La Jolla, CA). Survival curves were obtained using Kaplan–Meier survival analysis with log-rank tests for group comparisons. Continuous variables are presented as mean ± standard deviation (SD) or median ± interquartile range according to the normality tested by Shapiro–Wilk test. Based on data distribution and homogeneity of variance, variables were subjected to one-way analysis of variance or Kruskal–Wallis test for differences among the groups, followed by Student–Newman–Keuls post hoc test or Mann–Whitney U-test, respectively, for between-group comparison where appropriate. For the time trend analysis of Cdyn, a linear mixed model was used with the fixed effect of time, treatment, and their interaction, as well as the random effect of the subjects, along with the estimated mean differences of Cdyn between different treatments being calculated. Categorical variables are presented as numbers (proportions) and analyzed by Chi-square or Fisher’s exact test. A p value <0.05 was considered statistically significant.
Results
Experimental Phase I: CHF5633 vs. Poractant alfa in bolus
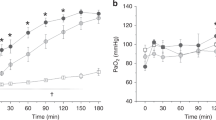
Figure 1a illustrates the study design in Phase I. In comparison with the Saline group, MAS group had significantly declined survival rates (26.5 vs. 96.3%, p < 0.001) and survival length (half survival time as 3.5 h vs. >10 h, p < 0.001), along with higher pneumothorax rate (26.5 vs. 0%, p = 0.003). Comparing to MAS group, NS200, SS200, SS400 had significantly higher survival length with 50% survival time >10 h (p = 0.005, 0.008, 0.009, respectively), higher survival rate (50–60%, p = 0.010, 0.045, 0.015, respectively), and <10% pneumothorax (Fig. 1b and eTable 2). Animals in MAS had significantly decreased Cdyn than in the Saline group, with >50% reduction throughout the ventilation course (p < 0.001), which was modestly improved (by 10–20%) in the three PS-treated groups (Fig. 1c and eTable 2). Significant time trend analysis of Cdyn, compared to Saline control, was seen in NS200 and SS200 (p = 0.002 and 0.036, respectively) (eTable 3). The estimated mean changes of Cdyn in SS200 were significantly higher than MAS (p < 0.001), but not in SS400 group (eTable 4). There was a 4-fold increase of serum LA in MAS than in the Saline group (p < 0.001), which markedly decreased in NS200, SS200, and SS400 (by 50–70%, vs. MAS, p = 0.047, 0.038, <0.001) (Fig. 1d).
a Protocol in Phase I study. b Kaplan–Meier survival curve. c Changes of dynamic compliance of respiratory system (Cdyn). d Serum lactate. Values are survival proportion (%) in b, mean ± standard deviation in c (n = 24–34 per group), or median ± interquartile range in d (n = 12–15). Group definitions and abbreviations: C0, unventilated control; Saline, ventilated control; MAS, meconium aspiration; NS200, one-bolus Poractant alfa (200 mg/kg); SS200, one-bolus CHF5633 (200 mg/kg); SS400, two-bolus CHF5633 (400 mg/kg). ***p < 0.001 vs. Saline; †p < 0.05 vs. MAS.
Figure 2 and eTable 5 show that the LIS value in the MAS group was significantly higher than Saline control (p < 0.001), along with lower Vv (p < 0.01) and higher CV(Vv) (p < 0.001). Compared to the MAS group, all PS-treated groups exerted the potential trend to lower LIS (by 10–20% on average), increase Vv, and decrease CV(Vv), as corroborated by decreased W/D and wet lung weight-to-BW ratio (Wlung/BW). Moreover, the mean mRNA expression levels of TLR-4 and NF-κB in animal lungs from the MAS group were increased by 1-fold compared to the Saline group, and 10–50-folds of TNF-α, IL-1β, IL-6, and IL-8. But the expression levels of those proinflammatory mediators were all declined in the three PS-treated groups, especially after repeated dosages of CHF5633 (SS400 vs. MAS, TLR-4, p = 0.035; TNF-α, p = 0.006; IL-1β, p = 0.007; IL-6, p = 0.002; IL-8, p = 0.009).
a Representative photomicrographs of the lungs. HE-stained lung slides under 200-fold amplification (scale bar = 100 μm). The black arrow marks the infiltrated leukocyte in the alveoli. b Total lung injury scores. c Alveolar expansion (Vv). d Variation of alveolar aeration (CV(Vv)). e Wet-to-dry lung weight ratio (W/D). f The mRNA expression of proinflammatory cytokines and mediators from lung tissue. For group definitions, see Fig. 1 legends. Vv volume density of alveolar spaces, CV(Vv) coefficient of variation of Vv, TLR Toll-like receptor, NF-κB nuclear transcription factor-κB, TNF-α tumor necrosis factor-α, IL interleukin, ICAM-1 intercellular adhesion molecule-1, iNOS inducible nitric oxide synthase. Values are mean ± standard deviation (n = 12–21 in b–d, 14–29 in e, and 10–12 in f). §p < 0.05, §§p < 0.01, §§§p < 0.001 vs. C0; *p < 0.05, **p < 0.01, ***p < 0.001 vs. Saline; †p < 0.05, ††p < 0.01 vs. MAS.
Figure 3 and eTable 6 show that TPL in BALF of non-ventilated lungs was around 40 mg/kg, with nearly 70% as DSPC. Within 10-h ventilation, there was 20–30% increment of both TPL (50 mg/kg) and DSPC (33 mg/kg) in BALF of Saline, which were decreased to about 15 and 10 mg/kg, respectively, in the MAS group, with 70% reduction (p < 0.001). There were significantly increased TPL and DSPC in BALF of NS200, by 90–100% on average over MAS (both p < 0.01). A similar but less prominent trend (~60% increment) was seen in both SS200 and SS400, though not statistically significant. These changes were not found in LH. There were no significant changes across the groups for DSPC/TPL and TP in BALF, whereas DSPC/TP was modestly increased in all PS-treated groups. The activity of sPLA2 was very low in C0 and Saline subsets, but with 3–5-folds increment in MAS (vs. Saline, p = 0.002), which was moderately decreased (by 40–60%) after both surfactants’ treatment.
a Total phospholipids (TPL). b Disaturated phosphatidylcholine (DSPC). c The ratio of DSPC/TPL. d Total proteins (TP). e The ratio of DSPC/TP. f The activity of secretory phospholipase A2 (sPLA2, normalized by total proteins). For group definitions, see Fig. 1 legends. Values are mean ± standard deviation (n = 8–12). §p < 0.05, §§p < 0.01, §§§p < 0.001 vs. C0; *p < 0.05, **p < 0.01, ***p < 0.001 vs. Saline; †p < 0.05, ††p < 0.01 vs. MAS.
As for other biochemical measures, the values of MPO were significantly higher in all meconium-exposed and PS-treated groups than the C0 and Saline groups, whereas no changes were found in MDA, SOD, and GSH (eFigure 1a–d). The mRNA expression of SPs, CCT, and GFs were variable and generally downregulated without statistical significance in the MAS group (eFigure 1e, f). However, compared with the MAS group, the expression levels of SP-A, -B, and -C were markedly suppressed only in NS200 (eFigure 1e).
Experimental Phase II: CHF5633 BAL vs. bolus
In Experimental Phase II, the study design was shown in Fig. 4a. The survival status and all other parameter levels of C0, Saline, MAS, and SS200 groups in this phase were generally similar to those in Phase I without significant differences. Compared to the MAS group, animals with surfactant treatments showed 30–100% improvement of survival rate, especially for the sPS BAL plus high boluses regimen that had the highest survival rate (62.5% vs. 33.3%, p = 0.037). Those in SS200, SSL, SSL100, and SSL300 also presented prolonged survival time with 50% survival length of >10 h (vs. 5 h in MAS, p = 0.047, 0.014, 0.002, 0.005, respectively) and improved Cdyn (by 20–30%) though not statistically significant (Fig. 4b, c and eTable 7). No significant time trend was shown among all surfactant-treated groups (eTable 8). However, SS200, SSL, SSL100, and SSL300 presented significantly improved mean changes of Cdyn compared to the MAS group (p = 0.012, <0.001, 0.016, and 0.001, respectively) (eTable 9). The lowered LA should reflect altered acidotic status during MV, which was markedly mitigated by the second bolus of sPS in the SSL300 group, with >80% reduction compared to the MAS group (p < 0.001) (Fig. 4d). SSL300 group also presented markedly decreased LIS (by 40% on average, p < 0.05), decreased mRNA expression levels of proinflammatory cytokines (TNF-α in particular, p < 0.001), and increased Vv (p < 0.05) and decreased CV(Vv) (p < 0.05) (Fig. 5a–f and eTable 10).
a Protocol in Phase II study. b Kaplan–Meier survival curve. c Cdyn. d Serum lactate. Values are survival proportion (%) in b, mean ± standard deviation in c (n = 18–27), or median ± interquartile range in d (n = 12–15). Group definitions and abbreviations: C0, unventilated control; Saline, ventilated control; MAS, meconium aspiration; SS200, one bolus of CHF5633 (200 mg/kg); SSL, diluted CHF5633 lavage (100 mg/kg); SSL100, diluted CHF5633 lavage plus one undiluted bolus (100 mg/kg); SSL300, diluted CHF5633 lavage plus two undiluted boluses (300 mg/kg). §p < 0.05 vs. C0; ***p < 0.001 vs. Saline; ††p < 0.01 vs. MAS.
a Photomicrographs of the lungs (HE×200, scale bar = 100 μm) with black arrows marking the infiltrated leukocyte. b Total lung injury scores. c Vv. d CV(Vv). e W/D. f The mRNA expressions of inflammatory mediators. For group definitions, see Fig. 4 legends and for abbreviations see Fig. 2 legends. Values are mean ± standard deviation (n = 8–14 in b–d, 17–26 in e, and 10–12 in f). §p < 0.05, §§p < 0.01, §§§p < 0.001 vs. C0; *p < 0.05, **p < 0.01, ***p < 0.001 vs. Saline; †p < 0.05, ††p < 0.01, †††p < 0.001 vs. MAS; ‡p < 0.05, ‡‡p < 0.01, ‡‡‡p < 0.001 vs. SSL300.
As the recovery rate of BAL fluid of diluted sPS (20 mL/kg) was about 30–40%, it corresponded to 12–14 mL/kg extra surfactant phospholipid-containing fluid that remained in the lungs. However, no significant changes were found in W/D and Wlung/BW in the sPS BAL-treated groups compared to MAS, along with the modestly lowered LIS in edema (eTable 10). In comparison with the MAS group, SSL100 and SSL300 also had significantly increased TPL (by 100–140%, both p < 0.001) and DSPC (by 80–90%, p < 0.01) in BALF (Fig. 6) and DSPC in LH (by 85–100%, p < 0.001) (eTable 11). Compared with the SS200 and SSL group, both TPL and DSPC in LH also significantly increased in SSL300 (p < 0.05) (eTable 11).
a TPL. b DSPC. c The ratio of DSPC/TPL. d TP. e The ratio of DSPC/TP. f The activity of sPLA2 (normalized by total proteins). For group definitions, see Fig. 4 legends and for abbreviations see Fig. 3 legends. Values are mean ± standard deviation (n = 8–12). §p < 0.05, §§p < 0.01, §§§p < 0.001 vs. C0; *p < 0.05, **p < 0.01, ***p < 0.001 vs. Saline; †p < 0.05, ††p < 0.01, †††p < 0.001 vs. MAS; ‡p < 0.05 vs. SSL300.
The activity of sPLA2 in BALF decreased in the groups subjected to sPS BAL and bolus, especially in SSL (p = 0.001) and SSL300 (p = 0.017), with 70–80% reduction on average compared to the MAS group (Fig. 6f). Both sPS bolus and BAL plus bolus had limited impacts on MPO, MDA, GSH, and SOD (eFigure 2a–d). Compared to the MAS and SS200 groups, those groups with BAL tended to have increased mRNA expression of SPs though without significant differences, and no regularly changes were found for CCT and GFs (eFigure 2e, f).
Discussion
This study revealed the feasibility of the ventilated near-term newborn rabbit model with meconium aspiration at birth, which enabled the exploration of the therapeutic efficacy (vs. Poractant alfa) and treatment modalities (BAL vs. bolus) of CHF5633.
Synthetic surfactant preparations have long been investigated since the late 1970s. A variety of sPS, such as colfosceril palmitate (Exosurf®), lusupultide (Venticute®), and lucinactant (Surfaxin®), have been introduced into clinical use for neonatal RDS21,23 and adults with acute RDS (ARDS).39 However, most of the clinical efforts were ended with inferior outcomes of these sPS taking nPS into account regarding survival, oxygenation, lung mechanics, and air leaking, among others.21,40 The main reason was argued by the design of peptide analogs based on either single or combined surfactant proteins (SP-B and SP-C), which generally determine surface tension-lowering activity and alveolar stability during cyclic breathing and lung expansion.21,23 CHF5633, as a new generation of sPS, is the first preparation containing both SP-B and SP-C peptide analogs. In comparison with nPS (Poractant alfa or Survanta®, a bovine surfactant), CHF5633 exerted similar efficiency in reducing surface tension, improving lung mechanics and mitigating inflammation, as confirmed in both laboratory and clinical investigations for RDS,23,25,26,27,31,32,33 and other lung injury diseases.28,29,30 As recently reported by Mikolka et al.,30 a single dose of CHF5633 improved lung function and attenuated inflammation as effectively as Poractant alfa in experimental ARDS caused by injurious ventilation. The current study showed similar effects of both surfactants via bolus on improving Cdyn in a single dose but not in double doses. The excess fluid load might offset the benefits of exogenous surfactant when meconium remained in alveolar space, causing injury to the lung. However, in the second phase, all CHF5633 BAL groups presented a significantly improved trend of Cdyn compared to the MAS group, even under high fluid load (12–18 mL/kg). It revealed the potential of sPS to improve lung function with the clearance of meconium, consolidating the safety and tolerance of BAL with a relatively large volume of diluted CHF5633 in the experimental MAS model.
In the current Phase I study, we found almost identical effects of CHF5633 and Poractant alfa in the improvement of survival, mitigation of acidosis, alleviation of lung injury, and the potential of reversing the impairment of endogenous PS system. CHF5633 also had the potential in modulating pro- and anti-inflammation balance, as reflected by the mRNA expression in the lungs. The reported potential of CHF5633 as stronger resistance to inactivation by albumin,27 prevention of lipid peroxidation caused by meconium,29 and immunomodulatory properties in reducing infection-induced cytokine release,28 was proposed for the higher proportion of POPG and SP-B analog as anti-inflammatory elements.23,25,26 It might account for the downregulation of mRNA expression of pro-inflammatory cytokines such as TNF-α, especially in those with repeated dosage. It also indicates that, in MAS, a repeated dosage of PS bolus might have better anti-inflammatory effects rather than a single dose, as reported by Findlay et al.8
As there were equivalent or non-inferior effects between sPS (CHF5633) and nPS (Poractant alfa) via bolus in MAS in the Phase I study, we further explored the optimal regimen of CHF5633 in Phase II study. The results suggested that the diluted sPS BAL was safe and effective for meconium removal, thereby mitigating meconium-induced inflammatory injury and airway obstruction. It also incurred no substantial lung fluid retention, as evidenced by no increased W/D, Wlung/BW, and edema in LIS, but leftover surfactant without jeopardizing lung mechanics and gas exchange, as reported by other studies.11,12,13,19,20 Thus, additionally high doses of bolus sPS should have led to the lower values of serum LA, LIS, and mRNA expression of TNF-α among all groups in both phases. It strongly suggests that diluted CHF5633 BAL plus high boluses regimen tended to be the optimal modality. The removal of meconium and other noxious particles (neutrophils, lipid and protein debris, etc), as well as mitigated inflammatory process, in turn, should have protected endogenous and exogenous surfactant from dysfunction, inactivation, and metabolic deterioration.1,2,7 Therefore, the additional doses of exogenous PS might be more readily utilized and absorbed by lung tissue and increase the synthesis of endogenous PS, as supported by further increased TPL and DSPC pools in both BALF and lung tissue compartments, and lowered activity of sPLA2 in BALF, comparing to those receiving PS treatment via lavage or bolus only.
Notably, there was a mild enhancement of mRNA expression in TLR-4 and NF-κB induced by meconium, which tended to lower with the surfactant treatments in both phases. It suggests that the response of proinflammatory cytokine mRNA may be associated with other pathways rather than the classical TLR/NF-κB inflammatory signaling one.1,2,7 Kopincova et al.7 suggested that sPLA2, the primary enzyme responsible for surfactant phospholipid hydrolysis, was one of the most relevant components of meconium and the key effector activated by enhanced inflammation cascade, which may link different pathways engaged in balancing endogenous surfactant homeostasis and functional integrity. In this regard, the results from Experimental Phase II indicate that diluted surfactant lavage may reduce the intrapulmonary meconium-derived sPLA2 concentration, thereby enhancing the activity of endogenous and exogenous surfactant. Although we found no substantial variations in several antioxidant biomarkers, we did not implement, in the study design, any specific measures in defining oxidative stress-associated efficacy with type and dosage of PS regimens, e.g., FiO2 was maximized at 1.0.
The limitation of the current study is mainly related to the lung injury model itself, as meconium was instilled at birth without prior intrauterine hypoxic distress, and PS was deliberately given at 1 h of ventilation. In contrast, clinically MAS encounters prenatal and peripartum stress and resuscitation at birth. Therefore, the interpretation of our data should be cautious. Furthermore, despite setting up experimental conditions to “standardize” the care as proposed elsewhere,16,17,18,19,20 we did not monitor blood gas or hemodynamics due to animal body size and experimental length. In both experimental phases, the sample sizes for the biochemical and molecular marker measurements were relatively small. Therefore, the judgment and conclusion of the optimal modalities were mainly based on survival length, lung mechanics, and lung morphometries, which should be validated by more experimental and clinical studies.
In summary, this study assessed the efficacy of the synthetic surfactant CHF5633 delivered with two treatment modalities in experimental MAS. The major findings suggest that its BAL plus bolus regimen is optimal and safe in reinstalling lung function and structural integrity. It warrants the design of clinical investigation to verify its efficacy in future for intractable MAS.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lindenskov, P. H., Castellheim, A., Saugstad, O. D. & Mollnes, T. E. Meconium aspiration syndrome: possible pathophysiological mechanisms and future potential therapies. Neonatology 107, 225–230 (2015).
Vain, N. E. & Batton, D. G. Meconium “aspiration” (or respiratory distress associated with meconium-stained amniotic fluid?). Semin. Fetal Neonatal Med. 22, 214–219 (2017).
Sun, B., Shao, X., Cao, Y., Xia, S. & Yue, H. Neonatal-perinatal medicine in a transitional period of China. Arch. Dis. Child. Fetal Neonatal Ed. 98, 440–444 (2013).
Wang, H. et al. Morbidity and mortality of neonatal respiratory failure in China: surfactant treatment in very immature infants. Pediatrics 129, e731–e740 (2012).
Macfarlane, P. I. & Heaf, D. P. Pulmonary function in children after neonatal meconium aspiration syndrome. Arch. Dis. Child. 63, 368–372 (1988).
Beligere, N. & Rao, R. Neurodevelopmental outcome of infants with meconium aspiration syndrome: report of a study and literature review. J. Perinatol. 28, S93–S101 (2008).
Kopincova, J. & Calkovska, A. Meconium-induced inflammation and surfactant inactivation: specifics of molecular mechanisms. Pediatr. Res. 79, 514–521 (2016).
Findlay, R. D., Taeusch, H. W. & Walther, F. J. Surfactant replacement therapy for meconium aspiration syndrome. Pediatrics 97, 48–52 (1996).
Lotze, A. et al. H. Multicenter study of surfactant (beractant) use in the treatment of term infants with severe respiratory failure. Survanta in term infants study group. J. Pediatr. 132, 40–47 (1998).
Chinese Collaborative Study Group for Neonatal Respiratory Diseases. Treatment of severe meconium aspiration syndrome with porcine surfactant: a multicentre, randomized, controlled trial. Acta Paediatr. 94, 896–902 (2005).
Wiswell, T. E. et al. A multicenter, randomized, controlled trial comparing Surfaxin (Lucinactant) lavage with standard care for treatment of meconium aspiration syndrome. Pediatrics 109, 1081–1087 (2002).
Gadzinowski, J., Kowalska, K. & Vidyasagar, D. Treatment of MAS with PPHN using combined therapy: SLL, bolus surfactant and iNO. J. Perinatol. 28, S56–S66 (2008).
Dargaville, P. A. et al. Randomized controlled trial of lung lavage with dilute surfactant for meconium aspiration syndrome. J. Pediatr. 158, 383–389 (2011).
Challis, P., Nydert, P., Håkansson, S. & Norman, M. Association of adherence to surfactant best practice uses with clinical outcomes among neonates in Sweden. JAMA Netw. Open 4, e217269 (2021).
El. Shahed., A. I., Dargaville, P. A., Ohlsson, A. & Soll, R. Surfactant for meconium aspiration syndrome in term and late preterm infants. Cochrane Database Syst. Rev. 2014, CD002054 (2014).
Sun, B., Curstedt, T., Song, G. W. & Robertson, B. Surfactant improves lung function and morphology in newborn rabbits with meconium aspiration. Biol. Neonate 63, 96–104 (1993).
Sun, B., Herting, E., Curstedt, T. & Robertson, B. Exogenous surfactant improves lung compliance and oxygenation in adult rats with meconium aspiration. J. Appl. Physiol. 77, 1961–1971 (1994).
Sun, B., Curstedt, T. & Robertson, B. Exogenous surfactant improves ventilation efficiency and alveolar expansion in rats with meconium aspiration. Am. J. Respir. Crit. Care Med. 154, 764–770 (1996).
Dargaville, P. A. et al. Therapeutic lung lavage in the piglet model of meconium aspiration syndrome. Am. J. Respir. Crit. Care Med. 168, 456–463 (2003).
Calkovska, A., Mokra, D., Drgova, A., Zila, I. & Javorka, K. Bronchoalveolar lavage with pulmonary surfactant/dextran mixture improves meconium clearance and lung functions in experimental meconium aspiration syndrome. Eur. J. Pediatr. 167, 851–857 (2008).
Sardesai, S., Biniwale, M., Wertheimer, F., Garingo, A. & Ramanathan, R. Evolution of surfactant therapy for respiratory distress syndrome: past, present, and future. Pediatr. Res. 81, 240–248 (2017).
Hahn, S., Choi, H. J., Soll, R. & Dargaville, P. A. Lung lavage for meconium aspiration syndrome in newborn infants. Cochrane Database Syst. Rev. 4, CD003486 (2013).
Johansson, J. & Curstedt, T. Synthetic surfactants with SP-B and SP-C analogues to enable worldwide treatment of neonatal respiratory distress syndrome and other lung diseases. J. Intern. Med. 285, 165–186 (2019).
Sun, B. et al. Biophysical and physiological properties of a modified porcine surfactant enriched with surfactant protein A. Eur. Respir. J. 10, 1967–1974 (1997).
Sato, A. & Ikegami, M. SP-B and SP-C containing new synthetic surfactant for treatment of extremely immature lamb lung. PLoS ONE 7, e39392 (2012).
Ricci, F., Murgia, X., Razzetti, R., Pelizzi, N. & Salomone, F. In vitro and in vivo comparison between Poractant alfa and the new generation synthetic surfactant CHF5633. Pediatr. Res. 81, 369–375 (2017).
Seehase, M. et al. New surfactant with SP-B and C analogs gives survival benefit after inactivation in preterm lambs. PLoS ONE 7, e47631 (2012).
Glaser, K. et al. Anti-inflammatory effects of the new generation synthetic surfactant CHF5633 on Ureaplasma-induced cytokine responses in human monocytes. Expert Rev. Antiinfect. Ther. 15, 181–189 (2017).
Salvesen, B., Curstedt, T., Mollnes, T. E. & Saugstad, O. D. Effects of natural versus synthetic surfactant with SP-B and SP-C analogs in a porcine model of meconium aspiration syndrome. Neonatology 105, 128–135 (2014).
Mikolka, P. et al. Impact of synthetic surfactant CHF5633 with SP-B and SP-C analogues on lung function and inflammation in rabbit model of acute respiratory distress syndrome. Physiol. Rep. 9, e14700 (2021).
Sweet, D. G. et al. A first-in-human clinical study of a new SP-B and SP-C enriched synthetic surfactant (CHF5633) in preterm babies with respiratory distress syndrome. Arch. Dis. Child. Fetal Neonatal Ed. 102, 1497–1503 (2017).
Sweet, D. G. et al. A first-in-human clinical study of a new SP-B and SP-C enriched synthetic surfactant (CHF5633) in preterm babies with respiratory distress syndrome: two-year outcomes. J. Matern. Fetal Neonatal Med. https://doi.org/10.1080/14767058.2020.1863363 (2020).
Ramanathan, R. et al. Synthetic surfactant CHF5633 compared with Poractant alfa in the treatment of neonatal respiratory distress syndrome: a multicenter, double-blind, randomized, controlled clinical trial. J. Pediatr. 225, 90–96 (2020).
Xu, Y., Dong, Y., Guo, X. & Sun, B. Suppression of pulmonary group B streptococcal proliferation and translocation by surfactants in ventilated near-term newborn rabbits. Pediatr. Res. 86, 208–215 (2019).
Luo, S. et al. Comparison of survival of preterm newborn rabbits at 25-28 days of gestation with perinatal therapies at birth transition. J. Appl. Physiol. 131, 220–228 (2021).
Sun, B. et al. Application of a new ventilator-multi- plethysmograph system for testing efficacy of surfactant replacement in newborn rabbits. Eur. Respir. J. 4, 364–370 (1991).
Bartlett, G. R. Phosphorus assay in column chromatography. J. Biol. Chem. 234, 466–468 (1959).
Mason, R. J., Nellenbogen, J. & Clements, J. A. Isolation of disaturated phosphatidylcholine with osmium tetroxide. J. Lipid Res. 17, 281–284 (1976).
Lewis, S. R., Pritchard, M. W., Thomas, C. M. & Smith, A. F. Pharmacological agents for adults with acute respiratory distress syndrome. Cochrane Database Syst. Rev. 7, CD004477 (2019).
Ardell, S., Pfister, R. H. & Soll, R. Animal derived surfactant extract versus protein free synthetic surfactant for the prevention and treatment of respiratory distress syndrome. Cochrane Database Syst. Rev. 8, CD000144 (2015).
Acknowledgements
We cordially thank the parents for generous donation of their babies’ meconium, and Dr. Hongyi He and Dr. Yangyang Ma for kind advice in the measurements of lung histology and morphometry.
Funding
This research was supported by Chiesi Farmaceutici S.p.A. The company contributed to the study design but had no influence in the performance, analysis, and interpretation of experimental data and in writing the manuscript. B.S. is a recipient of research grants from Laboratory of Neonatal Diseases, National Commission of Health, and Children’s Hospital of Fudan University.
Author information
Authors and Affiliations
Contributions
Y.X. performed animal experiments, analyzed data, and drafted the manuscript; X.G. and M.C. contributed to animal experiments and data analysis; F.R., F.S., and X.M. conceptualized the study plan, supervised experiment protocol, and reviewed and modified manuscript; B.S. conceptualized the study plan, designed the experiment, interpreted the data, and edited and finalized the manuscript. All the authors agreed and approved this version to be submitted for publication.
Corresponding author
Ethics declarations
Competing interests
This research was supported by Chiesi Farmaceutici S.p.A, which owns the marketing rights for Poractant alfa and patent rights of CHF5633. F.R. and F.S. are Chiesi Farmaceutici employees. X.M. is a Chiesi consultant. The company contributed to the study design but had neither influence on the performance, analysis, and interpretation of experimental data nor in writing the manuscript.
Ethics approval and consent to participate
Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Xu, Y., Guo, X., Chen, M. et al. Efficacy of synthetic surfactant (CHF5633) bolus and/or lavage in meconium-induced lung injury in ventilated newborn rabbits. Pediatr Res 93, 541–550 (2023). https://doi.org/10.1038/s41390-022-02152-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02152-2