Abstract
Study design
Population-based prospective study.
Objectives
To provide a population-based description of length of stay (LOS) and person-related risk factors following unplanned hospital admission due to a secondary health condition (SHC) in persons with spinal cord injury (SCI).
Setting
Specialized SCI hospital and rehabilitation center in Switzerland.
Methods
Descriptive analysis of LOS using routine clinical data of persons with SCI, who were acutely hospitalized between 01.01.2017–30.06.2018. Multivariable regression analysis was used to derive marginal predictions of LOS by acute SHCs and person characteristics.
Results
The study included 183 persons, 83% were male, and the median age was 57 years (interquartile range, IQR, 49–67 years). SCI cause was traumatic in 160 (88.4%) cases, 92 (50.3%) were persons with tetraplegia, 147 (80.3%) were classified as motor complete lesions (American Spinal Injury Association Impairment Scale (AIS) A or B) and median time since injury (TSI) was 24 (IQR 13–34) years. Median LOS was 19 (IQR 9–39) days, varying from 74 (IQR 39–92) days for pressure ulcers, 13 (IQR 8–24) days for urinary tract infections (UTI), to 27 (IQR 18–47) days for fractures. LOS was prolonged in persons with multiple co-morbidities or those developing complications during hospitalization. Sex, SCI etiology and lesion level were not associated with LOS.
Conclusions
This population-based description identified substantial variation in LOS between acute SHCs and clinical complications as the main, potentially modifiable, person-related risk factors for extended hospital stay.
Similar content being viewed by others
Introduction
Evidence-based estimations of number of admissions and length of stay (LOS) are key parameters for hospitals in optimizing the planning of clinical resources, such as the management of hospital beds and medical personnel. Unplanned hospital admissions are especially challenging, as involving unplanned and immediate treatment. Persons with spinal cord injury (SCI) are especially prone to endure an unplanned hospital admission and are hospitalized more frequently compared to the general population, typically related to the acute occurrence or aggravation of a secondary health condition (SHC) [1, 2]. Lifelong follow-up care programs aiming to prevent SHCs and thus avoid hospitalizations are well established and accessible for all persons with SCI. Yet, many SHCs eliciting unplanned hospital admissions in daily practice may neither be predictable nor preventable, particularly in persons not attending annual routine clinical check-up visits [3].
Contemporary studies in persons with SCI have indicated pressure ulcers, urinary tract infections (UTI), respiratory infections, circulatory problems, neuropathic pain, spasticity, osteoporosis and fractures, as well as bowel and bladder regulation as the most common SHCs [1, 4,5,6,7,8]. Most hospitalizations due to SHCs seem to occur in first few years after SCI [2, 6], but reliable data on causes for hospitalization and LOS are limited [9,10,11]. This lack of information on patient numbers and LOS by cause of unplanned hospital admission hampers the optimal planning of health care resources, including bed capacity, specific medical supplies and medical personnel [9, 12, 13]. The provisioning and improvement of LOS estimations by the clinical cause of unplanned hospital admission is also relevant from the person perspective and the societal and financial perspective. Patients, their family and employers need reliable informing regarding their anticipated LOS, while associated economic costs (usually calculated as total inpatient days) and indirect costs (for example work leave) need timely informing to health and social security organizations [9, 12].
The present study investigated unplanned hospital admissions using data from the Swiss Paraplegic Centre (SPC), which represents the largest of four specialized SCI clinics in Switzerland. In the Swiss setting persons with SCI incurring a SHC are commonly directly admitted to the most proximate specialized SCI center and related to catchment area of the SPC the study population is for the most part representative of German-speaking Switzerland. The objective of this study is to provide a population-based description of LOS following unplanned hospital admission due to SHCs in persons with SCI. The first aim is to provide a description of number of persons, causes for unplanned hospital admissions (patient case-mix), and LOS due to SHCs. The second aim is to evaluate the determinants for LOS for common SHCs.
Methods
Study design and study population
We conducted a prospective population-based study using routine clinical data from digital medical records and study specific data of the SPC in Nottwil, Switzerland. The SPC offers 24 × 7 in-hospital specialty services including outpatient and inpatient emergency (intensive care unit and acute wards) and rehabilitation facilities. The study site is the largest Swiss facility for SCI care with annually between 600 and 700 hospitalizations due to SHCs. In this study we included all persons admitted within 24 h after first contact with the clinic (unplanned hospital admissions) from 01.01.2017 to 30.06.2018 (18 months). Inclusion criteria were: persons with SCI due to traumatic or non-traumatic cause and having an acute SHC with “the need for emergency admission within 24 h after first contact”. Excluded were persons without a diagnosis of SCI (for example: amyotrophic lateral sclerosis or cerebral palsy), persons admitted outside the defined time frame of 24 h after first contact, or persons with direct referral to the intensive care unit.
LOS
LOS was defined as the length of the inpatient period of care, calculated from time from the day of hospitalization until the day of discharge, thus basically reflecting the number of overnight stays. For persons with admission and discharge on the same day (n = 2 persons) LOS was set at 0.5.
Demographic variables and lesion characteristics
Person-characteristics, including age (at admittance), sex and TSI, were categorized according to the recommendations of the International Spinal Cord Injury Core Data Sets [14], while collapsing adjacent groups in case of sparse data. Age groups for analysis thus included persons aged 15–29, 30–44, 45–59, and 60 years or older. TSI groups included less than 6, 6–15, 16–25, and 26 years or more. Level and severity of SCI was reported according to the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) [13]. SCI etiology was classified as traumatic and non-traumatic SCI, according to the definition of the International Spinal Cord Society (ISCoS) Core Data Set [13]. Discharge destination was classified as private home, nursing home, death, or unspecified.
Diagnosis of the SHC
We defined, according to the definition of Jensen, Molton [5], the following groups of SHC as admission causes: 1. pressure ulcers, 2. UTI, 3. respiratory infections, 4. fractures, 5. other urological causes, 6. autonomic dysregulation (AD), 7. other infections and 8. other acute health conditions (for example bowel problems, baclofen pump defect).
Comorbidities
For our study we chose the most relevant comorbidities, defined as a health condition that is likely to be associated with worse health outcome (especially prolonged LOS) [15]. For this study, following comorbidities were assessed: 1. Diabetes mellitus (American Diabetes Association (ADA) Classification 1–4) [16], 2. Osteoporosis (T–Value < 2.5) [17], 3. Arterial hypertension (American Society of Hypertension (ASH) Stage 1–3) [18], 4. Renal failure (KDIGO - Kidney Disease Improving Global Outcomes) [19], 5. Heart failure (definition according to the Heart Failure Society of America) [20], 6. Deep vein thrombosis or pulmonary embolism, 7. Vascular disease (peripheral artery disease), 8. Current treatment for cancer, and 9. Moderate and severe sleep apnea (Apnoe-Hypopnoe-Index > 15/h) [5].
Complications during hospital stay
We comprehensively assessed complications during hospital stay that are likely to influence LOS, including sepsis, UTIs, respiratory infections, severe pain, severe spasticity, autonomic dysregulation, and pressure ulcers. In statistical analysis complications were used as a binary variable, with 0 indicating “not occurring” and 1 indicating “occurring”.
Statistical method
All statistical analyses were performed using the Stata statistical software (Stata/SE version 16.1 for Windows; Stata Corp, College Station, TX, USA).
Descriptive analyses include crude numbers and percentages to depict the population and to evaluate differences in LOS across classes of demographic and lesion characteristic variables. Variation in LOS will be reported using the mean and standard deviation (SD) as well as median and interquartile rage (IQR). Univariable and multivariable linear regression analysis was used to identify main determinants of LOS (days) among predictor variables, including sex, age class, lesion level, completeness of SCI, SCI etiology, cause of admission, medical complications, and pre-existing comorbidities. Prior to analysis, the variable LOS was log-transformed (lnLOS) to achieve normal distribution as confirmed using a Kolmogorov-Smirnov’s test. Marginal predictions for LOS from the multivariable model were derived using exponentiation as to back-transform estimates and respective 95% CI to the original scale (days).
Results
Person characteristics
Table 1 provides an overview of the study population. Over the study period a total of 183 persons were admitted. In total 83% were male and the median age was 57 years (IQR 49–67) years, with persons over 60 years of age representing 41.5% of the population. The median TSI was 24 (IQR 13–34) years. The cause of SCI was traumatic in 88.4%, about 50% (n = 92) had a tetraplegia, and 147 lesions (80.3%) were classified as motor complete (AIS A & B).
The most common single cause of unplanned hospital admission was infection, either from a respiratory, urological or other cause (Table 1). UTI represented the most prevalent distinct cause of admission at nearly 18% of cases, followed by pressure ulcer (13.3%) and fractures (12.2%). The assorted group of acute health conditions (21.6%) included severe constipation, dysfunction of baclofen pump, and other unspecified health conditions requiring immediate medical care.
Over three-quarter of persons had one or more comorbidities, the median number of comorbidities among those persons being 2 (IQR 1–3). The three most common comorbidities were: moderate/severe sleep apnea (33%), arterial hypertension (28.5%) and osteoporosis (26.8%). A total of 112 (62.6%) persons developed medical complications during hospital stay. Three persons died during hospital stay, over 90% of the persons (n = 167) were discharged home or to the nursing home where they were formerly living, the other persons were discharged to another hospital for specific medical treatment (Table 1).
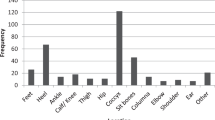
The median LOS was 19 (IQR 9–39) days, for a total range of 0 (2 persons were referred to other hospitals within the same day) to 311 days. Median LOS varied considerable between different cause of hospitalization, ranging from a maximum duration of 73.5 (38.5–92) days for pressure ulcers to a minimum duration of 5.5 (4–11) days for other urological causes (Fig. 1).
Crude, univariable, analyses indicated a statistical association of LOS with cause of admission, medical complications and number of comorbidities. In contrast, demographics, lesion characteristics and also discharge destination showed no distinct relationship with LOS (Table 1). Adjusted, multivariable, analysis confirmed an association of LOS with cause of admission and medical complications, but not with number of comorbidities (Supplemental Table 1). Marginal prediction of LOS as function of cause of admission and the occurrence of medical complications are provided in Table 2. Medical complications are projected to prolong LOS between 1.8 days for “Other urological causes” to 16 days for “Pressure ulcer”. For comparison, marginal estimates from a model allowing for effect modification (i.e., interaction term involving cause of admission and occurrence of medical complications) are also provided, recognizing that current data provided weak statistical support (likelihood ratio test comparing hierarchical models, F–test6142 = 0.45, P = 0.85).
Discussion
Causes for unplanned hospital admissions
This study indicated infections as the leading cause for unplanned hospital admissions (accounting for 43.2% of cases), followed by pressure ulcers (13.3%) and fractures (12.2%). Our findings contribute to the so far meager evidence base for specialized SCI care in high- and middle-income countries [12], which show similar predominance of clinical issues in the patient case-mix [2, 9,10,11]. The ordering in relative frequency among other health issues such as UTIs and urinary tract problems varies between settings, which may be indicative of differences between patient populations in patient characteristics, the quality of clinical follow-up, referral practice of emergency cases, or a combination of these factors. For instance, the present documentation of a relatively high frequency of respiratory infections may be explained by comparatively large share of persons with tetraplegia in our study population. This again might be explained by the possibility to admit persons to the intensive care unit at our center. Also, the lower frequency of urological problem and infections among unplanned hospital admissions might be due to the annual neuro-urological follow-up appointments provided in Switzerland [2, 8,9,10]. Finally, methodological differences in study design, involving defining of the sampling frame as well as timepoints and procedures of data collection, may also have affected the recorded patient case-mix of unplanned hospital admissions.
LOS and person-related risk factors for extended LOS
Mean LOS for unplanned hospital admission due to SHC in the total population was 31.5 days (SD 56.5 days) with a large variation between SHCs. Especially LOS in persons admitted with pressure ulcers was found to be long (median LOS of 73.5 days, range 0 till 311 days). This can be explained by the treatment approach of pressure ulcers usually involving surgery followed by an additional rehabilitation program with graded mobilization [1, 21]. Comparison of LOS with other settings is difficult [2, 9, 10, 22] and might be strongly depending on, for example, national situation in finances and health care provision
The most important finding was that development of complications during admission, such as in-hospital acquired infections and pressure ulcers during hospital admission was found to be the main potentially modifiable risk factor for extended LOS in all groups of SHC. This finding is likely not be unique for the Swiss population and is therefore of relevance for other settings. Although, the study center is one of the biggest specialized centers in the treatment of persons with SCI, even in this study almost 63% of the admitted persons developed one or more complications during admission which were found to be relevant for prolonged LOS. Development of better in-hospital monitoring strategies to prevent or early diagnose complications, such as hospital acquired pressure ulcers, hospital-acquired infections is thus of outmost importance. Development of those strategies is depending on prognostic models for specific complications such as hospital acquired pneumonia [23] or hospital acquired infections [24].
It is noticeable that, contrary above-mentioned studies older age, gender, injury severity and TSI did not influence LOS due to SHC.
Clinical, person and policy implications
This population-based description of unplanned hospitalizations due to SHC and potentially person-related risk factors of extended hospital stay provides us with evidence-based information to optimize health care and health care provision for persons with SCI. For efficient planning of health care resources, clinics (number of emergency beds, planning of personal and facilities like laboratory and radiology opening times, discharge planning) dependent on better knowledge of patient case-mix. Since studies on hospital nurse-staffing models also show that optimizing planning of health care resources is related to better outcomes for patients, the current study is also relevant with regard to patient outcomes [25, 26].
Besides the clinical perspective this study is also relevant from a person perspective, allowing us to better inform persons with SCI, their relatives and employers on estimated LOS. Furthermore, from a societal/cost-benefit perspective the current study provides evidence on leading causes of SHCs leading to (expensive) hospital admissions and therefore future targets of interventions such as initiation of focused vaccination campaigns to prevent respiratory infections [27] and implementation of evidence based clinical follow-up programs [18]. Unfortunately, literature regarding LOS due to SCHs in able bodies persons is scarce. A representative, recent Swiss study regarding LOS due to SHCs and costs due to (hip) fractures documented a mean LOS of 13 days (SD 11 days), which is considerably shorter than in the SCI population [28].
Last, as already mentioned earlier, the finding that development of complications during in-hospital stay result in prolonged LOS shows an urgent need for the development of better prevention strategies.
Methodological considerations
The center where this study was performed is the largest specialized SCI center with emergency care facilities as well as rehabilitation facilities in Switzerland and serves as primary referral facility for persons with SCI. Although it could be that we might have missed some persons with less severe (ambulatory) SCI our study is one of the few studies population-based studies. The prospective design of the study is a strength, avoiding methodological problems such as recall or reporting bias.
Unfortunately, the number of persons per subgroup did not allow us to perform further, in-depth analysis on the relation of SHC with the development of comorbidities.
Future research
Prevention of SHC plays a key factor in avoiding unplanned hospital admissions. Evaluation of future prevention strategies for SHC, such as vaccination campaigns should be target of future research. Also, to evaluate the effect of inpatient strategies to prevent complication during hospital stay should be topic of future research.
Conclusion
This population-based and prospective study contributes to the scant evidence base regarding the characteristics of the patient case-mix as well as LOS in relation to the emergence or worsening of existing SHCs. Clinical management strategies should particularly seek to reduce the incidence of complications in order to avoid extended LOS following unplanned hospital admissions.
Data availability
Additional data are available from the corresponding author on reasonable request.
References
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil. 2004;85:1757–63.
Savic G, Short DJ, Weitzenkamp D, Charlifue S, Gardner BP. Hospital readmissions in people with chronic spinal cord injury. Spinal Cord. 2000;38:371–7.
Chamberlain JD, Eriks-Hoogland IE, Hug K, Jordan X, Schubert M, Brinkhof MWG. Attrition from specialised rehabilitation associated with an elevated mortality risk: results from a vital status tracing study in swiss spinal cord injured patients. BMJ Open. 2020;10:e035752.
Brinkhof MW, Al-Khodairy A, Eriks-Hoogland I, Fekete C, Hinrichs T, Hund-Georgiadis M, et al. Health conditions in people with spinal cord injury: contemporary evidence from a population-based community survey in Switzerland. J Rehabil Med. 2016;48:197–209.
Jensen MP, Molton IR, Groah SL, Campbell ML, Charlifue S, Chiodo A, et al. Secondary health conditions in individuals aging with SCI: terminology, concepts and analytic approaches. Spinal cord. 2012;50:373–8.
Adriaansen JJ, Post MW, de Groot S, van Asbeck FW, Stolwijk-Swuste JM, Tepper M, et al. Secondary health conditions in persons with spinal cord injury: a longitudinal study from one to five years post-discharge. J Rehabil Med. 2013;45:1016–22.
Buzzell A, Chamberlain JD, Gmunder HP, Hug K, Jordan X, Schubert M, et al. Survival after non-traumatic spinal cord injury: evidence from a population-based rehabilitation cohort in Switzerland. Spinal cord. 2019;57:267–75.
Wannapakhe J, Arrayawichanon P, Saengsuwan J, Amatachaya S. Medical complications and falls in patients with spinal cord injury during the immediate phase after completing a rehabilitation program. J Spinal Cord Med. 2015;38:84–90.
Gabbe BJ, Nunn A. Profile and costs of secondary conditions resulting in emergency department presentations and readmission to hospital following traumatic spinal cord injury. Injury 2016;47:1847–55.
Mashola MK, Olorunju SAS, Mothabeng J. Factors related to hospital readmissions in people with spinal cord injury in South Africa. S Afr Med J. 2019;109:107–11.
DiPiro ND, Murday D, Corley EH, Krause JS. The primary and secondary causes of hospitalizations during the first five years after spinal cord injury. Spinal Cord. 2022;60:574–9.
Haeusler JM, Tobler B, Arnet B, Huesler J, Zimmermann H. Pilot study on the comprehensive economic costs of major trauma: Consequential costs are well in excess of medical costs. J Trauma. 2006;61:723–31.
Kirshblum SC, Biering-Sorensen F, Betz R, Burns S, Donovan W, Graves DE, et al. International standards for neurological classification of spinal cord injury: cases with classification challenges. Top Spinal Cord Inj Rehabil. 2014;20:81–9.
DeVivo MJ, Biering-Sorensen F, New P, Chen Y, International Spinal Cord Injury Data S. Standardization of data analysis and reporting of results from the international spinal cord injury core data set. Spinal Cord. 2011;49:596–9.
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7:357–63.
American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37:81–90.
Kanis JA. An update on the diagnosis of osteoporosis. Curr Rheumatol Rep. 2000;2:62–6.
Giles TD, Materson BJ, Cohn JN, Kostis JB. Definition and classification of hypertension: an update. J Clin Hypertens (Greenwich). 2009;11:611–4.
Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, et al. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138.
Bozkurt B, Coats AJ, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure: a report of the heart failure society of america, heart failure association of the European society of cardiology, japanese heart failure society and writing committee of the universal definition of heart failure. J Card Fail. 2021;23:352–80.
DeJong G, Tian W, Hsieh CH, Junn C, Karam C, Ballard PH, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil. 2013;94:87–97.
Cao Y, Murday D, Corley EH, DiPiro ND, Krause JS. Rehospitalization during the first five years after the onset of traumatic spinal cord injury: a population-based study using administrative billing records. Arch Phys Med Rehabil. 2022;103:1263–8.
Scheel-Sailer A, Wyss A, Boldt C, Post MW, Lay V. Prevalence, location, grade of pressure ulcers and association with specific patient characteristics in adult spinal cord injury patients during the hospital stay: a prospective cohort study. Spinal cord. 2013;51:828–33.
Raab AM, Mueller G, Elsig S, Gandevia SC, Zwahlen M, Hopman MTE, et al. Systematic review of incidence studies of pneumonia in persons with spinal cord injury. J Clin Med. 2021;11:211.
Butler M, Schultz TJ, Halligan P, Sheridan A, Kinsman L, Rotter T, et al. Hospital nurse-staffing models and patient- and staff-related outcomes. Cochrane Database Syst Rev. 2019;4:CD007019.
Griffiths P, Maruotti A, Recio Saucedo A, Redfern OC, Ball JE, Briggs J, et al. Nurse staffing, nursing assistants and hospital mortality: retrospective longitudinal cohort study. BMJ Qual Saf. 2019;28:609–17.
Ronca E, Miller M, Brinkhof MWG, Swi SCISG. Poor adherence to influenza vaccination guidelines in spinal cord injury: results from a community-based survey in Switzerland. Spinal Cord. 2020;58:18–24.
Mehra T, Moos RM, Seifert B, Bopp M, Senn O, Simmen HP, et al. Impact of structural and economic factors on hospitalization costs, inpatient mortality, and treatment type of traumatic hip fractures in Switzerland. Arch Osteoporos. 2017;12:7.
Author information
Authors and Affiliations
Contributions
AJ and SM proposed the study, and AJ, LM, and IEH accomplished its design, conceptualization and implementation. Study data were collected by AJ and SM. Statistical analysis was performed by LM and MB. AJ, LM, MB and IEH examined and interpreted the data. The manuscript was drafted by AJ, with support of LM, MB, and IEH. All authors provided critical feedback on the manuscript regarding important intellectual content, and provided their approval on the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was formally approved by regional medical ethics committee of northwest and central Switzerland (Project-ID 2020-01629). All the participants included in the study consented to anonymized use of data for research purposes and had the option to opt out.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jedrusik, A.M., Brinkhof, M.W.G., Müller, L.L. et al. Unplanned hospital admissions due to secondary health conditions after spinal cord injury: a population-based description of determinants of length of stay. Spinal Cord 61, 290–295 (2023). https://doi.org/10.1038/s41393-023-00880-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00880-8