Abstract
Plerixafor inhibits CXCR4, thus inducing the mobilization of hematopoietic stem/progenitor cells in lymphoma and multiple myeloma (MM) patients eligible for autologous stem cell transplantation (ASCT). However, the kinetics of plerixafor-induced mobilization of lymphocyte subsets is poorly known. Here, we evaluated the graft content, the engraftment, and the immunological reconstitution of MM patients receiving plerixafor. Thirty-seven patients undergoing one or tandem ASCT were enrolled. After mobilization with cyclophosphamide plus G-CSF, plerixafor was added at hematological recovery regardless of CD34+ cell count. We evaluated the number of CD34+, CD34+/CD38−, CD3+, CD4+, CD8+, CD19+, CD56+/CD3−, CD4+/CD25+/FOXP3+, and CD138+/CD38+ cells on each apheresis. Hematological and immunological recovery were determined at 30 days, 3, 6, 9, and 12 months after ASCT. Overall, 34/37 patients mobilized a median of 10.1 × 106 CD34+ cells/Kg (IQ 7.7–13.4). Patients with <20/µL CD34+ cells at plerixafor administration (18/33) had a significantly higher CD34+ cell fold increase, but not a higher absolute number, than 16/33 patients with ≥20/µL CD34+ cells. A similar CD34+ and immune graft composition was reported. A higher number of CD3+ and CD8+ cells/µL was observed at 3 months after first ASCT (p < 0.05) in the group with ≥20 CD34+ cells/µL. Thus, in MM patients, the timing of plerixafor administration influences immunological recovery.
Similar content being viewed by others
Introduction
High-dose chemotherapy followed by transplantation of autologous peripheral blood stem cell (PBSCs) is widely considered the standard of care for patients with multiple myeloma (MM) [1, 2]. Successful engraftment of PBSCs is correlated with the number of infused CD34+ stem/progenitor cells [3, 4]. PBSCs are mobilized into peripheral blood (PB) with granulocyte colony-stimulating factor (G-CSF) with or without disease-specific chemotherapy [5]. However, a significant proportion of MM patients fail to mobilize adequate numbers of PBSCs (“poor mobilizers”) [6], regardless the mobilization regimen [7], and cannot proceed to autologous stem cell transplantation (ASCT) [8].
Plerixafor is a CXCR4 chemokine receptor antagonist which has been shown to increase the number of PB CD34+ cells in healthy stem cell donors and cancer patients, when used alone or added to G-CSF [9,10,11]. Moreover, the results published so far demonstrate that the addition of plerixafor to G-CSF, with or without chemotherapy [5, 12,13,14,15,16,17,18], significantly reduces the risk of mobilization failure in MM and lymphoma patients and allows the rescue of “poor mobilizers” [6]. However, several issues, including the optimal timing for plerixafor administration and its effect on immunological recovery after ASCT, are still unclear.
The optimal timing for the addition of plerixafor to G-CSF, with or without chemotherapy, to improve PBSC mobilization has been recently explored. Risk-based algorithms have been developed to decrease resources utilization while optimizing stem cell collection [6, 19, 20]. In particular, a low CD34+ cell count on day 4 [21] or 5 [21] of G-CSF treatment and/or the insufficient collection of PBSCs on the first day of apheresis [22, 23] are considered predictors of collection failure and suggest the “preemptive” addition of plerixafor [5, 14, 20]. However, the identification of stringent criteria to start plerixafor in this setting is still lacking due to the individual variability in hematological recovery after chemotherapy and the heterogeneous kinetics of stem cell mobilization following different chemotherapy regimens. In this scenario, few and contrasting papers, based on the retrospective analysis of early cut-off CD34+ cell values (absolute numbers and percentage of leukocytes), either alone [21] or combined with white blood cell counts [24,25,26] or clinical parameters [8], proposed algorithms for the preemptive use of plerixafor after chemomobilization. Here, we report the results of a prospective multicenter trial involving MM patients treated homogeneously with 4 g/m2 of cyclophosphamide (CY) and G-CSF with the early addition of plerixafor, administered at the time of initial hematological recovery, regardless of CD34+ cell count. The aim of our study was to assess the effects of the timing of plerixafor administration on the kinetics of mobilization of myeloid and lymphoid sub-populations and their impact on posttransplant hematological and immunological recovery.
Patients and methods
This multicenter phase IV clinical trial was approved by the Ethical Committees (EUDRACT number: 2010-023029-39). Written informed consent was obtained before patient enrollment. Sanofi provided plerixafor vials free of charge, and approved the original protocol and its amendments, but had no role in the design of the study, the collection, analysis, and interpretation of the data, or the preparation of the manuscript.
Patient population
The trial was designed for MM patients candidate for one or tandem ASCT (either front line or as rescue strategy), who received chemotherapy (CY 4 g/m2) plus G-CSF as mobilizing regimen to collect PBSC. In particular, adults (age ≥18 years) with a performance status ≥ 70% (Karnofsky) or ≤2 (WHO), WBC count ≥2.5 × 109/L and absolute neutrophil count (ANC) ≥1.5 × 109/L, PLT count ≥100 × 109/L, a normal renal (serum creatinine ≤2 mg/dL), pulmonary (SatO2 ≥96%), hepatic (AST/ALT <2.5 ULN), and cardiac function were included in the study.
Study design and objectives
Primary objective was the evaluation of the percentage of patients collecting ≥6 × 106 CD34+ cells/Kg in three or less apheresis. Secondary objectives included the evaluation of the number of apheresis to collect ≥6 × 106 CD34+ cells/Kg, evaluation of engraftment and immunological reconstitution after transplantation of plerixafor-mobilized PBSC, and the assessment of cellular graft content.
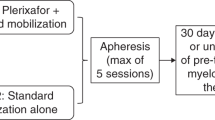
PBSC mobilization and collection
Patients enrolled in the study received mobilizing chemotherapy regimen with CY at the dose of 4 g/m2 administered in 1day (day 0). G-CSF (Filgrastim 10 µg/kg/day) was administered s.c. from day 6 after chemotherapy until the completion of PBSC collection. Plerixafor (240 µg/kg/day) was administered s.c., 11 h prior to initiation of apheresis. From day 10 after chemotherapy, WBC and CD34+ cells counts were performed daily by immunophenotypic analysis according to single platform ISHAGE protocol. To investigate the impact of plerixafor on early mobilization of myeloid and lymphoid sub-populations, the administration of study drug was started when WBC count was >1.0 × 109/L and unsupported PLT count was >20 × 109/L regardless of the concentration of CD34+ cells (i.e. even patients with no circulating CD34+ cells were potential candidates to receive plerixafor treatment). Up to five plerixafor injections were allowed to collect a minimum number of ≥6 × 106 CD34+ cells/kg, to allow tandem ASCT. In case of peripheral WBC >50 × 109/L, plerixafor administration was discontinued while G-CSF dose was halved. The first apheresis session was performed when CD34+ cell count was ≥10/µL.
Autologous stem cell transplantation
ASCT was performed within 3 months from last apheresis session, but later than 4 weeks after CY, in order to allow recovery from toxicities. Patients received melphalan 200 mg/m2 i.v. as conditioning regimen on day 2. G-CSF was administered after transplantation according to the standard clinical practice. Supportive care included the use of reverse isolation, prophylactic RBC and platelet transfusions, and antibacterial and antifungal prophyaxis. Febrile patients received empiric antibiotics according to local guidelines.
Evaluation of graft content, hematological, and immunological recovery
Patients were evaluated for hematological and immunological recovery at 30 days, 3, 6, 9, 12 months after transplantation for patients undergoing a single ASCT. Patients receiving tandem ASCT were evaluated at 30 days and 3 months after first ASCT and at 30 days, 3, 6, 9, and 12 months after second ASCT. In particular, PBSC were evaluated by immunophenotypic analysis for CD34+, CD34+/CD38−, CD3+, CD4+, CD8+, CD19+, CD16+/CD56+, and CD4+/CD25++FoxP3+ cells. Mobilization of neoplastic plasma cells was assessed by using anti-CD138, −CD38, −CD56, and −CD20 monoclonal antibodies. Hematological recovery was defined as an ANC higher than 0.5 × 109/L (first of 3 consecutive days) and an unsupported platelet count higher than 20 and 50 × 109/L after ASCT. Immunological reconstitution was evaluated by phenotypic analysis of total lymphocytes, CD3+, CD4+, CD8+, CD19+, CD16+/CD56+, and CD4+/CD25++FoxP3+ cells. We considered “good immunological recovery” CD3+ cells >700 × 106/L, CD4+ cells >200 × 106/L, CD8+ cells >500 × 106/L, CD19+ cells >50 × 106/L, and NK cells >100 × 106/L at 12 months after ASCT [27].
Statistical analysis
Sample size calculation was determined according to exact single-stage phase II design [28]. From previous data on CY chemotherapy and filgrastim, successful mobilization of PBSCs (defined as the collection of ≥6 × 106 CD34+ cells/Kg, suitable for tandem ASCT in 1 apheresis) was achieved in 65% of patients (Lemoli, data not shown). Setting p0 and p1 at the boundaries of the 95% confidence interval (p0 = 70% and p1 = 90%), the number of patients required, with α: 0.05 two sided and 1-ß = 90%, was 37.
Results
Patients’ characteristics
A total of 37 patients were enrolled in the study. Main clinical patients’ characteristics are reported in Table 1. Eleven out of thirty- seven patients presented abnormalities on the chromosome 1, one showed del(17p), 6 showed t(4;14), and 1 showed t(14;16) as reported in Table 1S. Five out of thirty-seven had received previous tandem transplantation.
PBSC mobilization and harvesting
Ninety-two percent of patients (34/37) mobilized a sufficient number of PBSC to proceed to leukapheresis. Out of the three cases who did not mobilize, one patient reported an anaphylactic reaction (severe dyspnea with angioedema, nausea, vomiting, and hyperthermia with chills and tachycardia) after the first plerixafor injection and was withdrawn from the study. The harvest was delayed by 24 h, and it was not possible to achieve the minimum target of CD34+ cells. The two additional patients who did not mobilize were >60 years old and heavily pretreated with multiple VTD cycles, and both already underwent double ASCT after melphalan 200 mg/m2 conditioning. Moreover, one of those patients could not proceed to leukapheresis for uncontrolled atrial fibrillation. Two thirds of patients were predicted poor mobilizers on the basis of previous chemotherapy [29]. The median day of starting plerixafor was 13 (±IQ 12–13) and the median day for the first apheresis was 14 (±IQ 13–14). The median number of G-CSF injections was 8 (±IQ 7–10). The median number of plerixafor injections was 1 (±IQ 1–2). Mobilization and harvesting data are shown in Table 2. Seventy-five percent of patients (28/37) achieved the primary objective of the study, collecting more than 6 × 106 CD34+/Kg in a median of 1 apheresis. Moreover, 33 patients underwent ASCT as planned: 18 as single ASCT, and 15 as tandem ASCT. One patient underwent ASCT with a reduced condition regimen (melphalan 100 mg/m2) due to the low CD34+ graft content and poor clinical conditions.
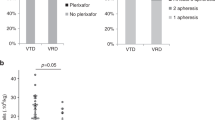
To study the kinetics of circulating CD34+ cells after plerixafor administration, we divided patients in two groups according to the number of CD34+ cells/µL the day of plerixafor administration (i.e. more or less than 20 cells/µL). The cut-off of 20 cells/µL was selected as currently used in normal clinical practice. We noted that 18/33 patients who received plerixafor with <20/µL CD34+ cells, had a significantly higher increase of circulating CD34+ cells (median fold change 9.6) than patients (16/33) with ≥20/µL CD34+ cells (median fold change 3.6) (Fig. 1a; p = 0.0004). Consequently, CD34+ cell graft content (×106/Kg) was similar within the two groups (Fig. 1b). Importantly, no significant differences among the two groups were observed regarding previous treatments (Table 2S), thus suggesting that differences in bone marrow cellularity and/or microenvironment due to previous treatments may not account for the observed differential response to plerixafor in the two groups.
Effect of plerixafor administration on circulating CD34+ cell numbers and CD34+ cell harvest. Patients were divided in two groups according to the number of CD34+ cells/µL before plerixafor administration (i.e. more or less than 20 cells/µL). a Fold change in circulating CD34+ cell numbers before and after plerixafor administration in the two groups of patients. b Graft CD34+ cell dose (×106/Kg recipient body weight) in the two groups of patients. Columns represent median values. Error bars represent interquartile ranges. Means, standard deviations, and minimum and maximum values were calculated for all continuous parameters. For comparisons, we used paired T-test, multivariate analysis of variances, and analysis of variances with the Bonferroni correction for multiple comparisons
Graft composition
We then compared the graft composition of patients who had received plerixafor with < and ≥20 CD34+ cells/µL. No differences were observed regarding the number of early CD34+/CD38− progenitor cells. The median number of CD3+ T cells in the group who received plerixafor with <20/µL vs ≥20/µL CD34+ cells was 75.1 (±IQ 55.4–96.4) vs 60.2 × 106/Kg (±IQ 46.7–92.3) (p = 0.373). The median number of CD4+ cells was 50.8 (±IQ 37–70) vs 41 × 106/Kg (±IQ 33.3–52) (p = 0.266), the median number of CD16+/CD56+ NK cells was 6.9 (±IQ 3.2–15) vs 2.8 × 106/Kg (±IQ 2.4–5.7) (p = 0.141). In particular, we did not observe a significant difference of the Treg cell content in the two groups. Specifically, the median number of Tregs cells was 15.7 (±IQ 9.8–28.7) vs 10.9 × 106/Kg (±IQ 8.1–16.6) (p = 0.181). A very similar pattern was also observed for total CD8+ cells and of CD19+ cells (Fig. 2).
Graft composition of lymphocyte subsets. Patients were divided in two groups according to the number of CD34+ cells/µL before plerixafor administration (i.e. more or less than 20 cells/µL). Lymphocyte doses are expressed ×106/Kg recipient body weight. Columns represent median values. Error bars represent interquartile ranges. p value of the comparison of the number of Tregs in the graft between two groups mobilized with chemotherapy plus G-CSF plus plerixafor
Reinfusion and engraftment evaluation of plerixafor-mobilized PBSCs
Reinfusion and engraftment data of plerixafor-mobilized PBSCs after ASCT were analyzed. Since the number of patients undergoing double ASCT was limited, we mainly focused our attention on the results after first ASCT (Table 3). Results after second ASCT are reported as Supplementary Results (Table 3S). No differences were observed in the hematological recovery (Table 3) as well as in the clinical parameters after ASCT (e.g. hospitalization, extra-hematological toxicity, infectious complications etc.) (data not shown). No severe infections during neutropenia after high-dose chemotherapy were reported. Extra-hematologic toxicities were mostly of grade I–II. Although the statistical power of the study was not centered on the evaluation of clinical outcome, we compared clinical results of patients who had received plerixafor with < and ≥20 CD34+ cells/µL. No significant differences were observed. In particular, at a median follow-up of 47 months, in the patient group with < and ≥20 CD34+ cells/µL we registered 2 vs 4 patients died for progression of MM, respectively, and 6 vs 8 patients with progression of disease currently on second or ≥ third line of therapy, respectively.
Immunological reconstitution
Patients who received plerixafor with a CD34+ cell count ≥20/µL, showed a median number of CD3+ cells >700 × 106/L, of CD4+ cells >200 × 106/L, and of CD8+ cells >500 × 106/L at all time points up to 12 months after first ASCT (Fig. 3a–c). In particular, at the 3-months time-point, a significantly higher median number of CD3+ cells/µL (Fig. 4a) and CD8+ cells/µL (Fig. 4b) was observed (p < 0.05) in the group with ≥20 CD34+ cells/µL at the time of plerixafor administration as compared with the group with <20 CD34+ cells/µL, respectively, (p < 0.05) [median number of CD3+ cells 1139/µL (±IQ 1001–2019), and CD8+ cells/µL 907.8 (±IQ 838–1354.3) vs CD3+ cells 695.5 /µL (±IQ 520.6–1117) and CD8+ cells 604.4/µL (±IQ 466.9–902.7)]. Moreover, we found a trend for an early recovery of CD4+ cells at 3 months after first ASCT in the group with CD34+ cell count ≥ 20/µL. In this group, the median number of CD4+ cells/µL was 260 (±IQ 182–544) vs 175 (±IQ 109–261) (p = 0.068, Fig. 4c). Between the two groups, no statistically significant difference in the recovery of CD19+ cells (p = 0.827), CD16+/CD56+ NK cells (p = 0.225), and CD4+/CD25++FoxP3+ cells was observed (p = 0.446). After 6 months the number of available samples was too low for a meaningful analysis. We found a similar trend of better immunological recovery of CD3+, CD4+, and CD8+ cells also at 3 months after second ASCT, but due to the limited number of samples analyzed, these results were not statistically significant (Table 4S), and have to be confirmed. Between the two groups, no significant difference in the immunological recovery of CD19+ cells, CD16+/CD56+, NK cells, and CD4+/CD25++FoxP3+ cells was observed (Table 4S). Indeed, these subsets had a good reconstitution at 12 months after first and second ASCT in both groups.
Recovery of lymphocyte subsets following first autologous transplant. Patients were divided in two groups according to the number of CD34+ cells/µL before plerixafor administration (i.e. more or less than 20 cells/µL). Symbols indicate median numbers (×106/L) of circulating a CD3+ T cells, b CD4+ T cells and c CD8+ T cells are reported at the indicated time-point after transplant. Error bars indicate interquartile ranges. *p value of the comparison of PB cell numbers at 3 months after transplantation in the group with more vs less than 20 CD34+ cells//µL before plerixafor administration
Timing of plerixafor administration according to the number of CD34+ cells/µL correlates with the lymphocyte immunological recovery. Linear regression analysis of the number of CD34+ cell/µL at plerixafor administration with the immunological recovery of a CD3+ T cells, b CD8+ T cells, c CD4+ T cells. The relationship between log-transformed peripheral CD34+ cells at the time of plerixafor administration versus CD3+, CD4+ and CD8+ count recovery at 3 and 6 months was analyzed by linear regression
Discussion
In this phase IV prospective study we evaluated the effects of plerixafor on the kinetics of myeloid and lymphoid cells mobilized with chemotherapy (CY at the dose of 4 g/m2) and G-CSF in a population of consecutive MM patients. Although the safety and efficacy of plerixafor in combination with G-CSF have been recently reported in a prospective study on a population of MM and lymphoma patients [16], there are only few data on plerixafor administration plus chemotherapy (and G-CSF). Moreover, most studies are conducted on populations of “predicted or proven poor mobilizers” [5, 13,14,15, 30], whereas in our trial plerixafor was used regardless of poor mobilization. This setting allowed us to investigate some crucial aspects of plerixafor-driven PBSC mobilization, i.e kinetics of mobilization, graft composition, and immune cell reconstitution after ASCT, without the clinical bias represented by poor mobilization condition.
The best schedule of plerixafor administration after chemotherapy is a major issue for its clinical use under normal clinical practice [31, 32] and several algorithms have been proposed [18, 26, 31, 33,34,35]. In our study, we started plerixafor based only on hematological parameters (WBC >1.0 × 109/L and unsupported PLT >20 × 109/L) independently from the PB CD34+ cell count. Early plerixafor administration induced a median 9.6-fold increase of CD34+ cells in patients with <20 circulating CD34+ cells /µL. Accordingly, we found a similar PBSC harvest in these patients as compared with patients who received “late” plerixafor administration, when CD34+ cells were ≥20/µL. Perhaps more importantly, the results of our study demonstrate that in a population of nonproven poor mobilizers, the timing of plerixafor administration may influence lymphoid cell graft composition and post-ASCT immunological recovery. In particular, a higher level of CD34+ cells at the time of plerixafor administration (according to clinical practice) is correlated with a significant faster immunological recovery. Such effect is not explained by a difference in collected and infused CD34+ cells between the two groups of patients since comparable numbers of CD34+ cells were reinfused (>3 × 106/Kg for both first and second ASCT), and the timing of ANC and PLT engraftment was similar to data reported in literature for stem cells mobilized without plerixafor. On the contrary, slower immunologic reconstitution was not due to poor stem cell mobilization. In previous reports, the number of lymphocytes infused during ASCT was correlated with an early lymphocyte reconstitution and a better PFS and OS after ASCT in MM and lymphoma patients, supporting the hypothesis that the number, and quality, of infused lymphocytes is associated with better immunological recovery and increased antitumor immune control of disease [36,37,38,39,40]. Moreover, the addition of plerixafor to G-CSF, with or without chemotherapy, [41, 42] has been associated with an increased percentage of more activated CD3+, CD4+, and CD8+ cells in the graft [43, 44]. In our study, a significantly higher median number of CD3+ cells/µL and CD8+ cells/µL was observed at 3 months after first ASCT in the group with ≥20 CD34+ cells/µL at the time of plerixafor administration, suggesting that the timing of plerixafor administration during the mobilization process may have impact on immunological recovery after ASCT. Of note, the timing of plerixafor administration did not have an impact on the immunological recovery of Tregs. This finding on Tregs may be correlated with previous reports, where no differences in the percentage of Tregs mobilized with plerixafor plus G-CSF vs G-CSF alone were shown (Gaugler et al. [43]). However, these authors suggested different functional properties between Tregs mobilized with or without plerixafor. Although, functional assays on immune cells of the graft and/or collected at different time after ASCT were not part of our clinical study, a better understanding of the impact of the timing of plerixafor administration on the functionality of immune cell subets, including Tregs, is highly warranted. Indeed, adding plerixafor at different timing during mobilization could lead to harvest a graft with different functional properties, thus collecting a subset of Tregs more susceptible to potential target of endogenous or therapeutic IL-7 (CD127 low) as shown by Simonetta et al. [45].
In conclusion, for the first time, our data indicate that the timing (defined as “early” in patients with CD34+ <20/µL and “late” with CD34+ >20/µl) of plerixafor administration during the mobilization process may have a different impact on the kinetics of CD34+ cells mobilization and on the immunological recovery after ASCT. Based on these findings, pre-plerixafor PB CD34 could be used as a possible predictive biomarker for more rapid immune recovery in patients undergoing chemomobilization plus G-CSF. These data need to be validated in a larger cohort of patients, where a potential correlation between pre-plerixafor PB CD34 and clinical outcome may be specifically addressed. However, our findings may support later administration of plerixafor and, given its well-known capacity of influencing immunological content of the graft, underline the relevance of systematically evaluating graft composition and immunological recovery in plerixafor-treated patients.
References
Passweg JR, Baldomero H, Bader P, Bonini C, Cesaro S, Dreger P, et al. Hematopoietic stem cell transplantation in Europe 2014: more than 40000 transplants annually. Bone Marrow Transplant. 2016;51:786–92.
Palumbo A, Cavallo F, Gay F, Raimondo Di, D BY F, Petrucci MT. Autologous transplantation and maintenance therapy in multiple myeloma. N Engl J Med. 2014;371:895–905.
Bensinger W, Appelbaum F, Rowley S, Storb R, Sanders J, Lilleby K, et al. Factors that influence collection and engraftment of autologous peripheral-blood stem cells. J Clin Oncol. 1995;13:2547–55.
Allan DS, Keeney M, Howson-Jan K, Popma J, Weir K, Bhatia M, et al. Number of viable CD34+ cells reinfused predicts engraftment in autologous hematopoietic stem cell transplantation. Bone Marrow Transplant. 2002;29:967.
D’addio A, Curti A, Worel N, Douglas K, Motta MR, Rizzi S. The addition of plerixafor is safe and allows adequate PBSC collection in multiple myeloma and lymphoma patients poor mobilizers after chemotherapy and G-CSF. Bone marrow Transplant. 2011;46:356–63.
Olivieri A, Marchetti M, Lemoli R, Tarella C, Iacone A, Lanza F. Proposed definition of “poor mobilizer” in lymphoma and multiple myeloma: an analytic hierarchy process by ad hoc working group Gruppo ItalianoTrapianto di Midollo Osseo. Bone marrow Transplant. 2012;47:342–51.
Pusic I, Jiang SY, Landua S, Uy GL, Rettig MP, Cashen AF, et al. Impact of mobilization and remobilization strategies on achieving sufficient stem cell yields for autologous transplantation. Biol Blood Marrow Transplant. 2008;14:1045–56.
Musto P, Simeon V, Grossi A, Gay F, Bringhen S, Larocca A, et al. Predicting poor peripheral blood stem cell collection in patients with multiple myeloma receiving pre-transplant induction therapy with novel agents and mobilized with cyclophosphamide plus granulocyte-colony stimulating factor: results from a Gruppo Italiano Malattie EMatologiche dell’Adulto Multiple Myeloma Working Party study. Stem Cell Res Ther. 2015;6:64.
Steinberg M, Silva M. Plerixafor: a chemokine receptor-4 antagonist for mobilization of hematopoietic stem cells for transplantation after high-dose chemotherapy for non-Hodgkin’s lymphoma or multiple myeloma. Clin Ther. 2010;32:821–43.
DiPersio JF, Stadtmauer EA, Nademanee A, Micallef INM, Stiff PJ, Kaufman JL, et al. Plerixafor and G-CSF versus placebo and G-CSF to mobilize hematopoietic stem cells for autologous stem cell transplantation in patients with multiple myeloma. Blood. 2009;113:5720–6.
DiPersio JF, Micallef IN, Stiff PJ, Bolwell BJ, Maziarz RT, Jacobsen E, et al. Phase III prospective randomized double-blind placebo-controlled trial of plerixafor plus granulocyte colony-stimulating factor compared with placebo plus granulocyte colony-stimulating factor for autologous stem-cell mobilization and transplantation for patients with non-Hodgkin’s lymphoma. J Clin Oncol. 2009;27:4767–73.
Dugan MJ, Maziarz RT, Bensinger WI, Nademanee A, Liesveld J, Badel K, et al. Safety and preliminary efficacy of plerixafor (Mozobil) in combination with chemotherapy and G-CSF: an open-label, multicenter, exploratory trial in patients with multiple myeloma and non-Hodgkin’s lymphoma undergoing stem cell mobilization. Bone Marrow Transplant. 2010;45:39–47.
Jantunen E, Penttilä K, Pyörälä M, Mahlamäki E, Kuittinen T, Nousiainen T. Addition of plerixafor to a chemotherapy plus G-CSF mobilization in hard-to-mobilize patients. Bone Marrow Transplant. 2011;46:308–9.
Attolico I, Pavone V, Ostuni A, Rossini B, Musso M, Crescimanno A, et al. Plerixafor added to chemotherapy plus G-CSF is safe and allows adequate PBSC collection in predicted poor mobilizer patients with multiple myeloma or lymphoma. Biol Blood Marrow Transplant. 2012;18:241–9.
Hübel K, Fresen MM, Salwender H, Basara N, Beier R, Theurich S, et al. Plerixafor with and without chemotherapy in poor mobilizers: results from the German compassionate use program. Bone Marrow Transplant. 2011;46:1045–52.
Russell N, Douglas K, Ho AD, Mohty M, Carlson K, Ossenkoppele GJ, et al. Plerixafor and granulocyte colony-stimulating factor for first-line steady-state autologous peripheral blood stem cell mobilization in lymphoma and multiple myeloma: results of the prospective PREDICT trial. Haematologica. 2013;98:172–8.
Baertsch M-A, Schlenzka J, Lisenko K, Krzykalla J, Becker N, Weisel K, et al. Cyclophosphamide-based stem cell mobilization in relapsed multiple myeloma patients: a subgroup analysis from the phase III trial ReLApsE. Eur J Haematol. 2017;99:42–50.
Lefrère F, Mauge L, Réa D, Ribeil J-A, Dal Cortivo L, Brignier AC, et al. A specific time course for mobilization of peripheral blood CD34+ cells after plerixafor injection in very poor mobilizer patients: impact on the timing of the apheresis procedure. Transfusion. 2013;53:564–9.
Lanza F, Lemoli RM, Olivieri A, Laszlo D, Martino M, Specchia G, et al. Factors affecting successful mobilization with plerixafor: an Italian prospective survey in 215 patients with multiple myeloma and lymphoma. Transfusion. 2014;54:331–9.
Olivieri J, Attolico I, Nuccorini R, Pascale SP, Chiarucci M, Poiani M, et al. Predicting failure of hematopoietic stem cell mobilization before it starts: the predicted poor mobilizer (pPM) score. Bone Marrow Transplant. 2018;53:461–73.
Sorasio R, Bonferroni M, Grasso M, Strola G, Rapezzi D, Marenchino D, et al. Peripheral blood CD34+ percentage at hematological recovery after chemotherapy is a good early predictor of harvest: a single-center experience. Biol Blood Marrow Transplant. 2014;20:717–23.
Costa LJ, Nista EJ, Buadi FK, Lacy MQ, Dispenzieri A, Kramer CP, et al. Prediction of poor mobilization of autologous CD34+ cells with growth factor in multiple myeloma patients: implications for risk-stratification. Biol Blood Marrow Transplant. 2014;20:222–8.
Costa LJ, Abbas J, Hogan KR, Kramer C, McDonald K, Butcher CD. Growth factor plus preemptive (’just-in-time') plerixafor successfully mobilizes hematopoietic stem cells in multiple myeloma patients despite prior lenalidomide exposure. Bone Marrow Transplant. 2012;47:1403–8. No
Milone G, Tripepi G. Algorithms for early identification of poor mobilization and for on-demand use of plerixafor in patients mobilized by chemotherapy and granulocyte-colony stimulating factor. Leuk Lymphoma. 2014;55:725–6.
Rossi G, Skert C, Morello E, Almici C, Arcaini L, Basilico C, et al. PBSC mobilization in lymphoma patients: analysis of risk factors for collection failure and development of a predictive score based on the kinetics of circulating CD34+ cells and WBC after chemotherapy and G-CSF mobilization. Hematol Oncol. 2015;33:125–32.
Farina L, Guidetti A, Spina F, Roncari L, Longoni P, Ravagnani F, et al. Plerixafor “on demand”: results of a strategy based on peripheral blood CD34+ cells in lymphoma patients at first or subsequent mobilization with chemotherapy+G-CSF. Bone Marrow Transplant. 2014;49:453.
Kim DH, Sohn SK, Won DI, Lee NY, Suh JS, Lee KB. Rapid helper T-cell recovery above 200 × 106/l at 3 months correlates to successful transplant outcomes after allogeneic stem cell transplantation. Bone Marrow Transplant. 2006;37:1119.
A’Hern RP. Sample size tables for exact single-stage phase II designs. Stat Med. 2001;20:859–66.
Olivieri A, Marchetti M, Lemoli R, Tarella C. Proposed definition of “poor mobilizer” in lymphoma and multiple myeloma: an analytic hierarchy process by ad hoc working group Gruppo ItalianoTrapianto di Midollo Osseo. Bone Marrow Transplant. 2012. https://www.nature.com/articles/bmt201182
Dugan MJ, Maziarz RT, Bensinger WI, Nademanee A, Liesveld J, Badel K, et al. Safety and preliminary efficacy of plerixafor (Mozobil) in combination with chemotherapy and G-CSF: an open-label, multicenter, exploratory trial in patients with multiple myeloma and non-Hodgkin’s lymphoma undergoing stem cell mobilization. Bone Marrow Transplant. 2010;45:39.
Jantunen E, Varmavuo V. Plerixafor for mobilization of blood stem cells in autologous transplantation: an update. Expert Opin Biol Ther. 2014;14:851–61.
Yuan S, Nademanee A, Krishnan A, Kogut N, Shayani S, Wang S. Second time a charm? Remobilization of peripheral blood stem cells with plerixafor in patients who previously mobilized poorly despite using plerixafor as a salvage agent. Transfusion. 2013;53:3244–50.
Sancho J-M, Duarte R, Medina L, Querol S, Marín P, Sureda A, et al. Mobilization of peripheral blood stem cells with plerixafor in poor mobilizer patients. Med Clin. 2016;147:223.e1–223.e7.
Farina L, Spina F, Guidetti A, Longoni P, Ravagnani F, Dodero A, et al. Peripheral blood CD34+ cell monitoring after cyclophosphamide and granulocyte-colony-stimulating factor: an algorithm for the pre-emptive use of plerixafor. Leuk Lymphoma. 2014;55:331–6.
Milone G, Martino M, Spadaro A, Leotta S, Di Marco A, Scalzulli P. Plerixafor on‐demand combined with chemotherapy and granulocyte colony‐stimulating factor: significant improvement in peripheral blood stem cells mobilization and harvest with no increase in costs. Br J Haematol. 2014;164:113–23.
Porrata LF, Gertz MA, Geyer SM, Litzow MR, Gastineau DA, Moore SB, et al. The dose of infused lymphocytes in the autograft directly correlates with clinical outcome after autologous peripheral blood hematopoietic stem cell transplantation in multiple myeloma. Leukemia. 2004;18:1085–92.
Porrata LF, Litzow MR, Inwards DJ, Gastineau DA, Moore SB, Pineda AA, et al. Infused peripheral blood autograft absolute lymphocyte count correlates with day 15 absolute lymphocyte count and clinical outcome after autologous peripheral hematopoietic stem cell transplantation in non-Hodgkin’s lymphoma. Bone Marrow Transplant. 2004;33:291–8.
Hiwase DK, Hiwase S, Bailey M, Bollard G, Schwarer AP. Higher infused lymphocyte dose predicts higher lymphocyte recovery, which in turn, predicts superior overall survival following autologous hematopoietic stem cell transplantation for multiple myeloma. Biol Blood Marrow Transplant. 2008;14:116–24.
Atta EH, de Azevedo AM, Maiolino A, Coelho CJBP, Sarcinelli SMP de Alvarenga Máximo C, et al. High CD8+ lymphocyte dose in the autograft predicts early absolute lymphocyte count recovery after peripheral hematopoietic stem cell transplantation. Am J Hematol. 2009;84:21–8.
Arteche-López A, Kreutzman A, Alegre A, Sanz Martín P, Aguado B, González-Pardo M, et al. Multiple myeloma patients in long-term complete response after autologous stem cell transplantation express a particular immune signature with potential prognostic implication. Bone Marrow Transplant. 2017;52:832–8.
Varmavuo V, Mäntymaa P, Silvennoinen R, Nousiainen T, Kuittinen T, Jantunen E. CD34+ cell subclasses and lymphocyte subsets in blood grafts collected after various mobilization methods in myeloma patients. Transfusion. 2013;53:1024–32.
Holtan SG, Porrata LF, Micallef INM, Padley DJ, Inwards DJ, Ansell SA, et al. AMD3100 affects autograft lymphocyte collection and progression-free survival after autologous stem cell transplantation in non-Hodgkin lymphoma. Clin Lymphoma Myeloma. 2007;7:315–8.
Gaugler B, Arbez J, Legouill S, Tiberghien P, Moreau P, Derenne S, et al. Characterization of peripheral blood stem cell grafts mobilized by granulocyte colony-stimulating factor and plerixafor compared with granulocyte colony-stimulating factor alone. Cytotherapy. 2013;15:861–8.
Roug AS, Hokland LB, Segel E, Nielsen K, Toft-Petersen M, Van Kooten Niekerk PB, et al. Unraveling stem cell and progenitor subsets in autologous grafts according to methods of mobilization: implications for prediction of hematopoietic recovery. Cytotherapy. 2014;16:392–401.
Simonetta F, Chiali A, Cordier C, Urrutia A, Girault I, Bloquet S, et al. Increased CD127 expression on activated FOXP3+CD4+ regulatory T cells. Eur J Immunol. 2010;40:2528–38.
Acknowledgements
This research is supported in part by Sanofi which provided Plerixafor vials free of charge.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
RML received travel grants by Sanofi. All other authors declare no relevant competing financial interests in relation to the work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tolomelli, G., Mancuso, K., Tacchetti, P. et al. The timing of plerixafor addition to G-Csf and chemotherapy affects immunological recovery after autologous stem cell transplant in multiple myeloma. Bone Marrow Transplant 55, 946–954 (2020). https://doi.org/10.1038/s41409-019-0756-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0756-1