Abstract
Aim Service evaluation of our dental hospital paediatric liaison nursing (DH-PLN) service which provides an additional route for information sharing about safeguarding concerns via an agreed pathway for two-way communication with public health nurses.
Method Retrospective analysis of clinical records of all children referred by DH teams to PLN in the three months October-December 2016.
Results One hundred and four children were referred; mean age was 6.2 years, 89.4% from Index of Multiple Deprivation (IMD) quintiles 4 and 5, and 70.2% were attending for dental general anaesthesia. The most common referral reason was dental neglect in 66.3%, followed by missed appointments in 50.0%. The PLN checked child health databases and shared information with health visitors and school nurses (46.2% and 53.8% respectively). Feedback retrieved included known child maltreatment risk factors in 7.7%. This prompted additional child protection referrals to children's social services for seven children (6.7%). Dental outcomes six months later were: treatment complete in 50.0%, treatment ongoing 28.8%, discharged to original referrer with treatment incomplete in 21.1%.
Conclusion This DH-PLN service promotes integrated multidisciplinary working, helping overcome barriers to dentistry's involvement in safeguarding. It facilitates more accurate assessments of risk of harm to children receiving dental care and prompts additional child protection referrals to social services.
Similar content being viewed by others
Key points
-
Describes the role of a dental hospital-based paediatric liaison nurse in a formal two-way communication pathway between hospital dental teams and public health nurses (health visitors and school nurses).
-
Evaluates the reasons for referral to the paediatric liaison nurse, further information retrieved, impact on number of referrals to children's social services and dental outcomes.
-
Discusses how this role alongside hospital dental teams can help expand dentistry's contribution to safeguarding children.
Introduction
Healthcare professionals have a duty to safeguard children and promote their wellbeing by cooperating with colleagues within health services and with other agencies such as education, early years and social services.1,2 In this context our understanding of the dental team's responsibility and potential to recognise concerns about child maltreatment has increased considerably in recent years,3,4 yet research continues to show that dentists worryingly lack knowledge about thresholds for action.5 Sharing information with health visitors and school nurses or with the child's general medical practitioner is often an appropriate first step in the process when a practitioner is considering whether a child may be at risk of harm.6,7 However, communication pathways are often poorly developed,5,8,9 and it has long been recognised that innovative changes in working practices are needed to support dental teams to participate effectively.10
Health visitors and school nurses, described hereafter as 'public health nurses', provide universal and targeted community-based services to children and young people across the 0 to 19 age range. They make an important contribution to the prevention of child maltreatment and to the early identification, recognition and referral of children who are at risk of or are suffering harm.11,12 In order to successfully fulfil this role they need access to information about a child and their family, including all relevant health issues and events such as hospital admissions. Historically, clinical correspondence about hospital dental care has routinely only been addressed to the referrer, usually the child's general dental practitioner. Sharing information beyond this, while desirable and considered good practice,6 is hampered by the lack of joined up healthcare systems.
Since the early 1990s Sheffield has benefited from a paediatric liaison service, a dedicated service for two-way communication between hospitals and community-based health professionals, mainly public health nurses. Its purpose is to promote integrated working across acute and primary care settings in the region, in order to safeguard children and promote their wellbeing. Sheffield Children's Hospital is commissioned to provide and manage this service which is staffed by a team of registered general nurses. Initially based in the three acute hospitals in the city and with the adult substance misuse service, it was expanded to include Charles Clifford Dental Hospital in 2011 as a result of the recommendations of a serious case review. Since that time, a paediatric liaison nurse (PLN) has worked three days a week in the dental hospital.
Dentists and dental care professionals (DCPs) in all departments can refer children to the dental hospital PLN (DH-PLN) using a standard proforma to initiate information sharing. This process follows an agreed pathway, as described in Figure 1. On receipt of referrals, the PLN accesses the child's electronic record on a range of healthcare databases to look for indicators of vulnerability. They note any alerts which highlight, for example, that the child is the subject of a child protection plan, is a looked after child, or that domestic violence has previously been reported in the family. They then contact the child's public health nurse by telephone to discuss directly. The PLN provides feedback to the referring dentist and offers them support to complete any further necessary actions arising as a result of new information. This includes advice and assistance to make a child protection referral to children's social care (hereafter referred to as 'social services') if the child is thought to be at risk of significant harm, if not already done.
In addition to documenting in the dental clinical records, the PLN service maintains a password-protected spreadsheet on a secure computer with details of referral information, any additional information retrieved, and all actions undertaken. The spreadsheet serves both as a method of organising workflow and tracking case management, and also as a record of service provision for generating activity reports to management for monitoring against the service level agreement.
Locally it is generally accepted that the PLN service enables health visitors and school nurses to better detect emerging problems and risk factors and so to plan targeted interventions to support vulnerable families. However, to our knowledge, the impact of such a service from the perspective of a host dental hospital has not been formally evaluated nor has such a service been described in the dental literature to date. We set out to do so for clinical governance purposes in our own organisation and in order to share any learning. Therefore, the aim of this paper is to describe the DH-PLN service and report the findings of our evaluation. Our objectives were to identify the reasons why the dental team refer to the PLN, to determine what additional information is retrieved by the PLN to add to the dentist's assessment, whether any additional actions by the dental team are required on receipt of feedback from the PLN, and what proportion of patients referred to the PLN go on to complete necessary dental care.
Methods
A service evaluation project proposal was registered with and approved by the host NHS trust (reference number 8092). Clinical records of all patients referred to the DH-PLN service in a three-month period between 1 October and 31 December 2016 were retrieved and examined by a single examiner (CS). Data collected on a standard proforma included age, gender, postcode and reason for PLN referral. The dental treatment modality (general anaesthetic, inhalation sedation, local anaesthetic and/or non-pharmacological management) was noted and number of teeth scheduled for extraction (if extractions were needed). An arbitrary cut-off point six months after the date of PLN referral was calculated, at which the outcome of dental treatment was noted: whether treatment complete and discharged, complete and placed on recall, treatment still in progress, or discharged with incomplete treatment. Further data were collected from the PLN's spreadsheet. This included professionals contacted, information received and whether a social services child protection referral was subsequently made.
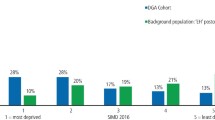
Data were entered into a spreadsheet (Microsoft Excel) and held on a secure trust computer. The Index of Multiple Deprivation IMD online tool13 was used to determine deprivation scores using children's home postcodes and descriptive statistics were generated. Paediatric dentistry departmental information on incoming referrals, proportion requiring GA and average number of teeth extracted, was obtained from routine service monitoring records for comparison.
Results
Patient characteristics
A total of 104 (53 male and 51 female) children were referred to the DH-PLN in the three-month study period, a mean of 35 per month. Of these, 102 were referred from the paediatric dentistry department and two from orthodontics. There were no referrals from other clinical dental specialties. The mean age at referral was 6.2 years (standard deviation 3.7 years, range 0.7-17.4 years). Analysis of postcode data indicated that 89.4% of referred children lived in the two most deprived Index of Multiple Deprivation (IMD) quintiles (quintile 1 = 1.9%; 2 = 1.9%, 3 = 6.7%, 4 = 25.0%, 5 = 64.4%). For the majority of children (70.2%) the dental treatment modality was general anaesthesia. When extractions were needed, the mean number of teeth extracted was 9.2.
For comparison, paediatric dentistry departmental information indicated that the mean age of children referred to the department for all reasons was 7.2 years, 47% required treatment under general anaesthesia and, when extractions were needed, the mean number of teeth extracted was 7.4. The mean number of children referred to PLN per quarter in the two years 2016-17 was 106, as derived from PLN records.
Reasons for referral to PLN
The main reasons for referral are shown in Table 1. Seventy-five percent of patients had more than one reason for referral category. The commonest category was 'significant caries and/or dental neglect' in 69 of 104 cases (66.3%), followed by 'failure to attend appointments' in 50.0% of children. Nine children had been discussed with or referred to children's social services by the dental team before PLN involvement, for example to discuss with the child's named social worker (if they had one) or to make an informal enquiry or a child protection referral. Additional 'free text' reasons for referral and further information relevant to the child's wellbeing were frequently shared with the PLN (Box 1).
Information sharing
Information sharing, social services referrals, dental treatment modality and outcome are shown in Table 2. The person contacted by the PLN to share information with was the child's health visitor in 46.2% of cases and school nurse in 53.8%. Information gained from this discussion was shared back to the dental team (Box 2). In eight cases, or 7.7% of children referred to the PLN, new information was received about previously documented risk factors for child maltreatment and this, when considered together with information already known to the dental team, directly prompted making a child protection referral to social services in seven cases (6.7%).
Six months after PLN referral, the required course of dental treatment had been completed for 50.0% of children. For 28.8%, treatment was ongoing and 21.1% of children had been discharged to the original referrer, usually their general dental practitioner, with treatment incomplete (Table 2).
Discussion
Sharing information is essential if the dental team is to meet its duty to safeguard and promote children's wellbeing. Indeed information sharing is described in government guidance as 'an intrinsic part of any frontline practitioner's job when working with children and young people.'15 It helps to ensure that a child 'receives the right services at the right time and prevents a need from becoming more acute and difficult to meet.'15 In an in-depth analysis of 66 serious case review reports in England between 2011 and 2014, undertaken to find out what went wrong and learn lessons when a child has died or been seriously harmed by maltreatment, only one was found where information sharing was not specifically mentioned.16 The authors stated: 'the centrality of information sharing to effective child safeguarding cannot be stressed enough'.16 They went on to stress the importance that communication must be two-way, must follow agreed pathways and be triangulated and verified; all features of our DH-PLN pathway.
Safeguarding concerns may present to the dental team with signs and symptoms of maltreatment, as concerning behaviour or interaction between children and parents or as direct disclosure of abuse.7,17,18 Furthermore, a wide range of other signs of vulnerability can become apparent in the course of providing dental care.4 Dentists must follow local safeguarding children procedures, including pathways for child protection referral to social services when concerned that the child is currently experiencing or is at risk of significant harm from abuse or neglect.1 This DH-PLN pathway presents an additional route for information sharing and, particularly for less specific concerns, an opportunity to explore whether further action would be indicated, such as referral for early help for families needing additional support.
Unsurprisingly, our evaluation showed that referrals to the DH-PLN were primarily from the department of paediatric dentistry. In comparison to all children newly seen in the department, children referred to the PLN were younger (6.2 vs 7.2 years), more likely to require general anaesthesia (70% vs 47%) and to need more teeth extracted (9.2 vs 7.4). The most common reasons given were dental neglect (66.3% of referrals to PLN) or the child not being brought to appointments (50.0%). Note that PLN referrals are not a direct equivalent, but these findings echo those of two recent robust research studies in Sweden19 and Norway18 in which the same two reasons were most frequent when dentists made child maltreatment reports (child protection referrals) to social services: dental neglect/grave caries; and missed appointments/not brought. Children living in areas of deprivation predominated in our sample, as in that of Kvist and colleagues.19
It is already known that UK dentists with an interest in paediatric dentistry commonly encounter dental neglect. In a 2005 survey, 80% reported seeing children with neglected dentitions weekly or more frequently.10 At that time 42% said they rarely or never 'discuss these cases with another health professional' and 96% rarely or never 'refer to social services.' While we would expect practice to have improved now that clear guidance6 and more training are available, barriers still remain. A UK study using fictitious vignettes found that fewer dentists correctly planned child protection actions for a child having multiple extractions of carious teeth under general anaesthesia, when compared to nurses and doctors.5 Differentiating between dental caries and dental neglect can be challenging, although evidence to inform decisions is available.20 Furthermore, paediatric dentists describe facing clinical and ethical dilemmas21 which may result in fewer referrals to social services than would be expected if guidelines were followed completely. Our DH-PLN service provides a ready opportunity for discussion to be initiated on the dental team's behalf as a first step. In our study this process, specifically the information retrieved and feedback obtained from public health nurses, culminated in the dental team making a child protection referral to social services for an additional 6.7% of cases (seven cases in three months) where otherwise they would not have done so. Additional information retrieved was mainly alerts to known risk factors for child maltreatment, such as domestic abuse or parental alcohol dependence.
Six months after PLN referral, half the children had completed their dental treatment. For 28.8% it was still in progress and 21.1% had been discharged from the dental hospital with treatment incomplete. Without a control group it is not possible to say whether these dental outcomes had been improved by PLN involvement. Nevertheless, we are encouraged that research elsewhere demonstrates that public health nurses are both keen to receive feedback from dental services8 and are enthusiastic about supporting attendance and improving oral health in those most in need.9
It is important to note that children were only discharged back to the referring dentist with treatment incomplete if deemed not at risk of pain or infection. It is likely that some simply required preventive care, which could be provided more conveniently close to home by the primary care dentist, or the problem for which they had originally been referred had now resolved. All necessary safeguarding actions were first completed and a copy of the discharge letter was sent to the general medical practitioner. A question remaining is whether those children subsequently went on to complete dental care outside the timeframe of the study, whether in primary care or following re-referral to the dental hospital.
These findings serve as a reminder, as primary care dental practitioners will be well aware, that, despite best efforts, children discharged from dental hospital care may have both unresolved dental treatment needs and other vulnerabilities that require further management; a responsibility that is shared between hospital and primary care providers. Long waiting lists for treatment or long waits between consecutive appointments can make it particularly difficult to monitor children's progress in overstretched services, thus requiring practitioners to be constantly vigilant.
Interestingly, the department of orthodontics made low use of the PLN service relative to the number of children and young people attending. This is probably because the most common dental safeguarding concerns (dental neglect and missed appointments) apply less frequently to orthodontic patients, who are not usually accepted for treatment unless they have excellent oral health and motivation. However, children and young people with important safeguarding concerns have previously been identified by our orthodontic colleagues and we consider it essential that the DH-PLN maintains regular contact with all dental specialties which treat either children or adults who are parents, even those specialties that make less frequent use of the service.
This service evaluation generated a number of action points for our own attention, notably the aforementioned need to raise awareness of the service and for the PLN to maintain regular contact with all dental specialties. In addition, it provides evidence of impact on the number of referrals made to social services. Beyond this, our findings will to be of interest to others who are looking for innovative ways of supporting safeguarding practice in dentistry and may want to consider implementing something similar, perhaps prompted by new commissioning standards.22 We found a wide variety of models of liaison nursing services described in the literature, including in mental health, intensive care, maternity and child health,23 and safeguarding,24 but none for dentistry. To find out more we contacted 15 UK hospital paediatric dentistry units by email and received 14 replies. Five reported access to dental-specific PLN support or equivalent (of which one had just been withdrawn due to lack of funding), four had contact with multiple PLNs at associated children's hospitals and the remaining five had no PLN service. In one unit 'safeguarding champion' was an alternative name for the role.
This service evaluation has a number of limitations. Had available resources allowed us to examine a larger sample of records, we would almost certainly have detected a wider range of less commonly encountered types of concern, risk factors and vulnerabilities. It is also important to acknowledge factors that were beyond the scope of this study. We do not know whether all children who might have benefited were referred to the PLN. Our results will have underestimated the total number of children with safeguarding concerns seen in the dental hospital, since some concerns will have been identified and fully handled by the dentists themselves without recourse to the PLN.
Evaluating what action the health visitors and school nurses took as a result of information received from the dental hospital via the PLN was also outside our scope. Anecdotally, although keen to avoid being used as a 'was not brought' follow-up service, they frequently contacted families to encourage dental attendance. We do not know to what extent they provided any other support to families or themselves made additional referrals to social services as a result of dental information sharing. Nor could we determine whether children's lives improved as a consequence of any of this activity.
The PLN role is a rare opportunity for paediatric nurses and the dental team to work together so closely, and we have observed that staff value this working relationship, but any wider benefits to both professional groups of this multidisciplinary approach remain unexplored. Further work would be beneficial to address these questions, to include an economic evaluation and to compare with a dental nurse acting in the liaison role.
Conclusion
The DH-PLN service enables two-way communication between the dental hospital and other healthcare professionals, mainly public health nurses, via an agreed pathway. This promotes integrated multidisciplinary working and helps overcome known barriers to dentistry's involvement in safeguarding children. The main reasons dentists refer to the DH-PLN to initiate information sharing are dental neglect or missed appointments. In addition, the DH-PLN retrieves additional information, which would be otherwise inaccessible to the dental team, from health records and discussion with public health nurses. Dentists receive feedback if other concerns have been identified elsewhere, such as domestic abuse or parental alcohol or substance misuse. This facilitates more accurate assessments of risk of harm to children receiving dental care and sometimes prompts additional dental team action such as making a child protection referral to social services.
References
National Institute for Health and Care Excellence. Child maltreatment: when to suspect maltreatment in under 18s. 2009. Available at https://www.nice.org.uk/guidance/cg89 (accessed June 2019).
HM Government. Working together to safeguard children. A guide to inter-agency working to safeguard and promote the welfare of children. 2018. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/779401/Working_Together_to_Safeguard-Children.pdf (accessed June 2019).
Harris C M, Welbury R, Cairns A M. The Scottish dental practitioner's role in managing child abuse and neglect. Br Dent J 2013; 214: E24.
Harris J C. The mouth and maltreatment: safeguarding issues in child dental health. Arch Dis Child 2018; 103: 722-729.
Olive S, Tuthill D, Hingston E J, Chadwick B, Maguire S. Do you see what I see? Identification of child protection concerns by hospital staff and general dental practitioners. Br Dent J 2016; 220: 451-457.
Harris J C, Balmer R C, Sidebotham P D. British Society of Paediatric Dentistry: a policy document on dental neglect in children. Int J Paediatr Dent 2009; DOI: 10.1111/j.1365-263X.2009.00996.x.
Harris J, Sidebotham P, Welbury R et al. Child protection and the dental team: an introduction to safeguarding children in dental practice. Sheffield: COPDEND, 2006 (updated online 2013). Available at https://bda.org/childprotection/ (accessed June 2019).
Bradbury-Jones C, Innes N, Evans D, Ballantyne F, Taylor J. Dental neglect as a marker of broader neglect: a qualitative investigation of public health nurses' assessments of oral health in pre-school children. BMC Public Health 2013; 13: 370.
Lewney J, Holmes R D, Rankin J, Exley C. Health visitors' views on promoting oral health and supporting clients with dental health problems: a qualitative study. J Public Health (Oxf) 2018; 41: e013-e108.
Harris J C, Elcock C, Sidebotham P D, Welbury R R. Safeguarding children in dentistry: 2. Do paediatric dentists neglect child dental neglect? Br Dent J 2009; 206: 465-470.
Institute of Health Visiting. Local Authority Child Public Health Briefing (2): The health visiting contribution to early help and prevention of child abuse and neglect. 2015. Available at https://ihv.org.uk/wp-content/uploads/2015/06/iHV_public_health_Briefing_2_V3.pdf (accessed June 2019).
Department for Education, Department of Health. Health Visiting and School Nurse Programme: Supporting implementation of the new service offer No. 5: Safeguarding children and young people: enhancing professional practice - working with children and families. 2012. Available at http://media.dh.gov.uk/network/387/files/2012/11/SAFEGUARDING_ENHANCING-PROFESSIONAL-GUIDANCE.pdf (accessed June 2019).
National Perinatal Epidemiology Unit. IMD tool. Available at https://tools.npeu.ox.ac.uk/imd/ (accessed June 2019).
Roe M. Child patients: WNB not DNA. BMJ 2010; 341: c6332.
HM Government. Information sharing: Advice for practitioners providing safeguarding services to children, young people, parents and carers. 2018, p6. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/721581/Information_sharing_advice_practitioners_safeguarding_services.pdf (accessed June 2019).
Sidebotham P, Brandon M, Bailey S et al. Pathways to harm, pathways to protection: a triennial analysis of serious case reviews 2011 to 2014. London: Department for Education, 2016, pp163-169, p195. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/533826/Triennial_Analysis_of_SCRs_2011-2014_-__Pathways_to_harm_and_protection.pdf (accessed June 2019).
Fisher-Owens S A, Lukefahr J L, Tate A R, American Academy of Pediatrics, American Academy of Pediatric Dentistry. Oral and Dental Aspects of Child Abuse and Neglect. Paediatrics 2017; 140: e20171487.
Brattabø I V, Bjørknes R, Åstrøm A N. Reasons for reported suspicion of child maltreatment and responses from the child welfare - a cross-sectional study of Norwegian public dental health personnel. BMC Oral Health 2018; 18: 29.
Kvist T, Cocozza M, Annerbäck E M, Dahllöf G. Child maltreatment - prevalence and characteristics of mandatory reports from dental professionals to the social services. Int J Paediatr Dent 2017; 27: 3-10.
Bhatia S K, Maguire S A, Chadwick B L et al. Characteristics of child dental neglect: a systematic review. J Dent 2014; 42: 229-239.
Kvist T, Wickström A, Miglis I, Dahllöf G. The dilemma of reporting suspicions of child maltreatment in paediatric dentistry. Eur J Oral Sci 2014; 122: 332-338.
Office of the Chief Dental Officer England. Commissioning Standard for Dental Specialties: Paediatric Dentistry. London: NHS England, 2018, p18. Available at https://www.england.nhs.uk/wp-content/uploads/2018/04/commissioning-standard-for-dental-specialties-paediatric-dentristry.pdf (accessed June 2019).
Olley H, Psaila K, Fowler C, Kruske S, Homer C, Schmied V. 'Being the bridge and the beacon': a qualitative study of the characteristics and functions of the liaison role in child and family health services in Australia. J Clin Nurs 2017; 26: 91-102.
Wild P. A project to improve links between paediatric liaison nurses and school nurse teams. Community Pract 2014; 87: 42-43.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spencer, C., Zaitoun, H., White, E. et al. Role of the dental hospital-based paediatric liaison nurse in safeguarding children. Br Dent J 227, 158–163 (2019). https://doi.org/10.1038/s41415-019-0488-z
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0488-z