Abstract
While clinical indicators, or so-called surrogate outcomes in periodontology, allow us to assess periodontal health and evaluate outcomes of periodontal therapy from a clinician's perspective, they cannot be used to evaluate patients' subjective perceptions of their health status or satisfaction with the received treatment. These can be assessed through patient-based outcomes, such as quality of life. The aim of this paper is to give an overview of the multidimensional concept of oral health-related quality of life (OHRQoL), its measures and association with plaque-induced, inflammatory periodontal diseases. Periodontitis and its clinical consequences, such as tooth loss, have a considerable negative effect on OHRQoL, while periodontal treatment and alleviation of the symptoms can lead to improvement in OHRQoL. Implant rehabilitation of missing teeth also seems to positively influence OHRQoL
Similar content being viewed by others
Key points
-
Highlights that patient-based outcomes, such as quality of life, should complement clinical indicators of periodontal status, providing a better understanding of the patient's perceptions of the disease and treatment.
-
Explores the association between plaque-induced, inflammatory periodontal diseases and their clinical consequences, and impairment of oral health-related quality of life.
-
Highlights that periodontal therapy has a well-documented positive impact on OHRQoL, while implant rehabilitation of missing teeth also seems to improve OHRQoL, particularly in edentulous individuals.
Patient-based outcomes: why do we need them?
Periodontitis is an infectious disease, resulting from an imbalance between the dento-gingival biofilm and host response. Inflammation of the tooth's supportive tissues leads to the destruction of the periodontal ligament and the supportive bone and, as a final result of the disease, it can eventually lead to tooth loss.1
Periodontal health is an indivisible component of oral and general health. The World Health Organisation, in its definition of health, has emphasised the patient's wellbeing, physical, mental and social states, as opposed to the traditional definitions of health as a mere absence of the disease.2 In periodontology, in order to clinically assess and monitor the status of periodontal health, we employ surrogate markers such as clinical attachment level, probing pocket depth, recession, plaque scores and bleeding on probing. Their relevance in the research and clinical work is indisputable, yet these outcomes are intangible in the patient's mind.3 Our medical acts encompass much more than reducing millimetres of pocket depth. Periodontal treatment, as it will be discussed in this article, reduces symptoms, disability and, importantly, improves quality of life. These patient-based outcomes (PBOs) can be assessed only by the patients themselves.4
The importance of the use of PBOs in periodontal therapy lies in the fact that patients' perceived assessments and opinions can differ from clinical indicators.5 Their priority in the research field was identified and emphasised 15 years ago.6 PBOs can thus give both the clinicians and the researchers a comprehensive insight and better understanding of the effects of the disease, and the provided therapy, on patients' symptoms, function, psychosocial factors and satisfaction.
What is oral health-related quality of life and what tools do we use to measure it?
Oral health, as much as general health, strongly influences quality of life, even though the means of this connection is extremely complex and, in a way, influenced by a mosaic of personal beliefs and subjective values.7 Patients' quality of life, as defined by the World Health Organisation, is 'perceptions of their position in life in the context of culture and value systems in which they live, and in relation to their goals, expectations, standards, and concerns'. It is highly subjective and can change over time as it is influenced by health, social and environmental factors.8
Oral health-related quality of life (OHRQoL) is one of the patient-based outcomes. It is a multidimensional, intangible and subjective concept and its measurement is complex. OHRQoL can be measured by questionnaires and/or related forms of assessment of the physical, psychological and social wellbeing, focusing on the possible impact an oral disease and/or treatment have on different dimensions of a person's life. Research in the OHRQoL domain has increased significantly since the mid-nineties,8 henceforth there has been an increase in the number of oral health-specific measures and instruments used to evaluate the quality of life. What gives the oral-specific measures an advantage over the generic measures is their increased sensitivity, providing more information on the influence of a specific oral condition or disease and the benefits of its treatment on quality of life. Furthermore, oral-specific measures have better responsiveness, meaning they are more likely to detect subtle changes in the assessed condition.8,9,10
The most widely used measures in the domain of OHRQoL research, also often employed in studies on periodontal patients,5,11,12,13,14,15,16 are the Oral Health Impact Profile (OHIP-14),17,18 the Oral Impacts on Daily Performances (OIDP),19,20 the Geriatric/General Oral Health Assessment Index (GOHAI),18 and the UK Oral Health-related Quality of Life measure (OHQoL-UK).21 The content of the presented measures varies, however they all tend to cover how oral conditions affect the physical, psychological and social aspects of life.9 Questionnaires and related instruments employ scales, originating from psychometrics, to assess OHRQoL. The two most commonly used types of scales are the VAS (visual analogue scale) and the Likert scale.7
Is there an association between periodontal diseases and OHRQoL?
Studies conducted so far established a clear association between OHRQoL and plaque-induced, inflammatory periodontal diseases, gingivitis and periodontitis. A large body of evidence corroborates a correlation between periodontitis in particular and OHRQoL. This connection has been explored and established in patients with chronic periodontitis11,22,23,24,25,26,27,28,29,30,31,32,33,34 and also in younger individuals and those with aggressive periodontitis.35,36,37,38 One of the earliest important studies in this area of research, was by Needleman et al.,16 employing the OHQoL-UK questionnaire, known as OHIP-14. This study reported a considerable effect of periodontal status on quality of life. When assessed through OHIP-14, results showed that there were significant differences for functional limitations, physical pain, psychological discomfort, and physical and psychological disabilities between individuals with periodontitis and healthy individuals.5,16,39 Interestingly, the aforementioned study further showed a correlation between the OHRQoL scores and the number of >5 mm pockets, suggesting that there is an association between the severity of the disease and overall quality of life. This was further confirmed by other studies23,26,28,33,39,40,41 and one systematic review looking into the extent and the severity of the disease and their association with worse OHRQoL.7
There also seems to be an association between gingivitis and impaired OHRQoL, albeit weak, although there are some inconsistencies among the reported data. On the one hand, studies in children and preadolescents with gingivitis recruited from public schools,42 children attending an examination at a dental hospital and dental practice,43 adolescents and adults up to 30 years of age undergoing orthodontic treatment,44 and the household population of Brazilian adolescents45 reported no significant association with impaired OHRQoL. Conversely, there are a number of studies on large, representative samples supporting an association between gingivitis and impaired OHRQoL. A study on Belgian young adults36 and three studies including schoolchildren and adolescents in Sudan,46 Thailand47 and Brazil,48 reported that worse OHRQoL is indeed associated with gingivitis. The possible discrepancy between the reported results could be explained by the differences and variations between the study samples, use of different OHRQoL measures and/or the clinical examination of the gingival status (eg partial versus full mouth examination).
Finally, presented data suggest there is a proportionate effect; the higher the periodontal involvement, the higher the impairment of OHRQoL. Future trials should also capture what is the minimal extent of gingival inflammation that is capable of affecting patients' quality of life.
Clinical consequences of periodontitis: how do they affect OHRQoL?
Research in the domain of OHRQoL of periodontal patients focuses mainly on certain key aspects leading to its impairment: symptoms, functionality and psychosocial impacts.
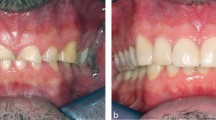
Symptoms of periodontal disease such as swollen, sore and/or receding gums, drifting and missing teeth, and oral malodour have a significant impact on all aspects of a patient's quality of life: physical, social and psychological.49 As reported in the literature, these symptoms influence function, comfort, appearance and self-confidence.16
Oral functionality, in particular chewing, is imperative for maintenance of wellbeing. Periodontitis, particularly when undiagnosed and/or untreated, is a major determinant of tooth loss in adults.50 Tooth loss leads to functional deterioration in terms of chewing,51,52 which can have far-reaching consequences such as temporomandibular disorders29 and changes in an individual's diet and nutritional intake. Thus, it is of no surprise that tooth loss is significantly associated with an impaired OHRQoL, as confirmed by a systematic review and meta-analysis by Gerritsen et al.,53 which provided evidence corroborating this association. Furthermore, the results of the same study suggest that the severity of impairment is heavily impacted by the location (loss of anterior teeth) and distribution (fewer occluding units) of missing teeth. When discussing tooth loss and its effects on quality of life, it is as equally important to acknowledge its impact on the self-perceived aesthetics and social wellbeing. Namely, loss of teeth is associated with limitations in normal daily activities such as smiling in public, formation of relationships and consumption of food, all of which leads to loss of self-appreciation and confidence.54
Stress, a state of mental or emotional strain resulting from demanding circumstances, can be put in both direct and indirect association with periodontitis.55 Work-related stress in regards to demanding and increased workload, combined with low flexibility at the workplace, inability to make phone calls or leave work for personal reasons, lead to worse OHRQoL and personal self-care. Those with strict working environments and obligations have higher levels of dental plaque as they are more likely not to follow regular oral hygiene practice.56 Such prolonged strain and allostatic load are not only related to poor oral hygiene but other unhealthy behaviours, including smoking, drinking and irregular sleeping patterns, all of which further increase susceptibility to periodontitis.57
Social life, life experiences and self-confidence are aspects of human nature deeply interwoven with perceptions of happiness and quality of life; all these aspects are negatively affected by periodontitis.16 Periodontitis can almost be seen as a taboo. Patients would rather not discuss or share thoughts and feelings about the condition, in terms of tooth loss and shame, causing them to cover their mouth while smiling and even frustration towards clinicians that have not recognised their disease initially.58 Patients seem to enjoy everyday activities less, with evidence pointing to a lower frequency of smiling and not opening their mouths wide, as well as more subdued reactions when watching funny shows on television.30
Can the treatment of periodontitis improve OHRQoL?
Knowing the effect periodontitis has on OHRQoL, it is of interest to further explore the potential effect periodontal treatment and the alleviation of symptoms of the disease have on quality of life. The efficacy and effectiveness of periodontal therapy in treating and controlling the disease, which can be measured with improvements in its clinical indicators, is well established.59 Studies published thus far almost consistently confirm the effect periodontal therapy has on improvement of quality of life. 11,12,15,60,61,62,63,64,65,66,67,68,69
A systematic review by Shanbhag et al.70 confirmed the improvement of OHRQoL following non-surgical periodontal therapy. These improvements seem to be stable over a one-year time period following non-surgical treatment, as reported in a clinical study by Wong et al.61 The quality of life improvement seems to not be affected by the type of non-surgical treatment employed, in regards to instruments (traditional instrumentation versus lasers) or treatment approaches (quadrant versus one stage full-mouth approach).15,70 Surgical periodontal therapy does not appear to significantly amplify any improvements to quality of life.65,68,70,71 This observation could be explained by the dramatic alleviation of symptoms and already improved quality of life following non-surgical treatment. Therefore, further changes in the condition may not be appreciated or perceived.
Does implant rehabilitation of missing teeth improve OHRQoL?
Both periodontitis and dental caries are the leading causes of tooth loss.72,73,74 Thus a significant number of individuals might experience tooth loss during their lifetime which, as discussed previously, is significantly associated with impairment of OHRQoL.53 On this basis, we have further explored the degree to which tooth rehabilitation, in particular implant therapy, affects OHRQoL. This may give clinicians further insight as to how tooth rehabilitation, being the goal of treatment for patients with a periodontally-affected dentition, may positively influence their quality of life.
There is a variety of treatment modalities for those affected by tooth loss, both partially dentate and edentulous. Knowledge of the extent to which tooth loss and certain prosthetic treatment modalities affect OHRQoL is relevant for clinical decision-making and the provision of appropriate treatment options for the patient. Several systematic reviews of the literature evaluating the impact of implant-supported prostheses on OHRQoL in partially dentate75,76,77,78 and/or edentulous patients37,75,76,77,78,79,80,81 have been published thus far.
Edentulous patients
The majority of the studies evaluating the impact of implant placement on OHRQoL focus on the edentulous population and mandibular overdentures in particular, as patients wearing conventional complete mandibular prostheses may often experience poor retention and consequently chewing, aesthetic and social problems.82,83
Even though a large body of evidence suggests that implant-supported overdentures (IODs) are indeed associated with an increase in OHRQoL, data have to be interpreted with caution as there is considerable methodological variation and inconsistencies across studies. Systematic reviews by Kutkut et al.37 and Thomason et al.75 report the superiority of IODs over conventional dentures (CDs) in terms of masticatory performance37 and improvements in OHRQoL.37,75 The systematic review by Strassburger et al.77,78 also suggests an increase in OHRQoL in IOD wearers following treatment, yet reports that no further improvements in terms of OHRQoL or patient satisfaction can be achieved with placement of more than two implants.
Boven et al.80 reviewed literature assessing masticatory performance, bite force, nutritional state, patient satisfaction and quality of life in edentulous patients receiving mandibular IOD and/or maxillary IOD instead of a CD. And while patients' satisfaction improved after treatment with IOD, this did not necessarily lead to improvement in general quality of life or OHRQoL. Emami et al.79 identified only randomised controlled trials comparing CDs and IODs in edentulous patients in terms of patient satisfaction, oral and general quality of life, eight of which were included in the meta-analysis. Analysis of the data demonstrated that treatment with mandibular IODs instead of new a CD may yield better scores in term of patients' satisfaction and OHRQoL, yet due to significant heterogeneity between the studies the true effect is left uncertain. A systematic review and meta-analysis by Sivaramakrishnan and Sridhara analysed five studies assessing OHIP improvements between OID and CD treatment patient groups.81 The OID group exhibited statistically significant improvement of total scores, and in all subgroups except the domain of physical pain. The review was, however, greatly limited due to the high risk of bias in selection and ascertainment of outcome measures.
A systematic review by Reissmann et al.,76 analysing data from 32 studies conducted in edentulous patients, reported that OHRQoL improves both with IODs and CDs, yet the improvement is slightly increased for IODs. The authors do argue that this finding is not observed in all reviewed studies. One of the possible explanations for increased OHRQoL in patients with IODs could be that implants are usually requested by, and could be more beneficial to, patients with advanced alveolar bone resorption and severe denture problems; this has also been hypothesised by other authors.78,84,85 Thus, the authors further suggest that, in patients willingly seeking implant treatment, with initially highly impaired OHRQoL, superior quality of life improvements will be reported than in those receiving a CD treatment. Indeed, the level of satisfaction of patients that are already content with their existing CD does not improve significantly after implant placement.86 A study including all patients who believed they would receive new CDs showed no significant differences post-treatment between those receiving OIDs or CDs,87 even though it has to be taken into consideration that the treatment effect may be masked by application of 'intention to treat' analysis.
One of the major challenges and drawbacks in understanding the real impact of OID treatment on OHRQoL is that, despite the large number of published studies, there is a substantial variety in reported outcome assessment measures. This complicates and/or prevents the comparison of results of different studies, leading to a deficiency of robust evidence. As a limitation of the studies published thus far, it is also worth noting that short-term follow-ups do not enable the observation of potential deterioration in OHRQoL as a result of implant failures or incidence of peri-implant diseases.
Partially dentate patients
In terms of association between OHRQoL and implant-supported fixed prostheses in partially dentate patients, there is not a sufficient body of evidence that would imply that implant-supported fixed prostheses (FDP) are superior in OHRQoL improvement when compared to conventional, teeth-supported FDPs.76 There is some evidence that patients with implant-supported FDPs report better OHRQoL than those with removable partial dentures (RPDs).76 Studies also report that significant implant-related improvements in OHRQoL were positively associated with the number of missing teeth in the anterior region,88,89 which also supports the aforementioned effect that loss of anterior teeth has on OHRQoL and perceived aesthetics. Other treatment approaches for partially dentate patients are not well represented enough in the literature to be able to quantify the effect of treatment choice.
How to interpret changes in OHRQoL measures?
Studies mostly focus on the statistical differences of OHRQoL scores without highlighting whether these differences are actually clinically meaningful for the patient or clinician. Thus, interpreting changes in PBO scores should be based on the calculation of minimal important difference (MID).90 From a patient's perspective, MID is the smallest difference in a PBO measure score that they can perceive as favourable or harmful. For a clinician, MID may imply a consideration of the change of treatment. MID for OHRQoL measures has been calculated and reported in certain studies on patients with periodontitis67 and dentine hypersensitivity91 of patients undergoing supportive periodontal therapy.
Conclusion
Periodontal diseases and tooth loss associated with untreated periodontitis have a well-documented influence on patients' quality of life. In the past two decades there has been a significant increase in research in the domain of OHRQoL, yet some clinicians are still not familiar with the concept, its value and the implications it might have on their clinical work. Thus, this paper highlights and emphasises that traditionally recorded clinical measurements taken by the periodontal probe should be supplemented with patient-based outcomes, such as OHRQoL. It also aims to give a comprehensive view on why there is real merit in the awareness of patients' subjective perceptions and assessments of their disease, and the treatment they're undergoing, both periodontal therapy and tooth rehabilitation. Taking all of this into account could give a better insight and understanding of the effects of the disease and provided therapy on symptoms, function, psychosocial factors and patients' satisfaction with treatment. This knowledge could, therefore, facilitate the provision of patient-centred care. We should aim not only to treat patients' disease, but also to make their lives better.
References
Savage A, Eaton K A, Moles D R, Needleman I. A systematic review of definitions of periodontitis and methods that have been used to identify this disease. J Clin Periodontol 2009; 36: 458-467.
World Health Organization. Constitution of the World Health Organization. 2006. Available at https://www.who.int/governance/eb/who_constitution_en.pdf (accessed September 2019).
Hujoel P P. Endpoints in periodontal trials: the need for an evidence-based research approach. Periodontol 2000 2004; 36: 196-204.
Black N. Patient reported outcome measures could help transform healthcare. BMJ 2013; 346: f167.
Ng S K, Leung W K. Oral health-related quality of life and periodontal status. Community Dent Oral Epidemiol 2006; 34: 114-122.
Tonetti M S, Fourmousis I, Suvan J et al. Healing, post-operative morbidity and patient perception of outcomes following regenerative therapy of deep intrabony defects. J Clin Periodontol 2004; 31: 1092-1098.
Buset S L, Walter C, Friedmann A, Weiger R, Borgnakke W S, Zitzmann N U. Are periodontal diseases really silent? A systematic review of their effect on quality of life. J Clin Periodontol 2016; 43: 333-344.
Locker D, Allen F. What do measures of 'oral health-related quality of life' measure? Community Dent Oral Epidemiol 2007; 35: 401-411.
Sischo L, Broder H L. Oral health-related quality of life: what, why, how, and future implications. J Dent Res 2011; 90: 1264-1270.
Allen P F. Assessment of oral health related quality of life. Health Qual Life Outcomes 2003; 1: 40.
Aslund M, Pjetursson B E, Lang N P. Measuring oral health-related quality-of-life using OHQoL-GE in periodontal patients presenting at the University of Berne, Switzerland. Oral Health Prev Dent 2008; 6: 191-197.
Jönsson B, Öhrn K. Evaluation of the effect of non-surgical periodontal treatment on oral health-related quality of life: Estimation of minimal important differences 1 year after treatment. J Clin Periodontol 2014; 41: 275-282.
Ozcelik O, Haytac M C, Seydaoglu G. Immediate post-operative effects of different periodontal treatment modalities on oral health-related quality of life: a randomized clinical trial. J Clin Periodontol 2007; 34: 788-796.
Costa F O, Miranda Cota L O, Pereira Lages E J et al. Oral impact on daily performance, personality traits, and compliance in periodontal maintenance therapy. J Periodontol 2011; 82: 1146-1154.
Santuchi C C, Cortelli J R, Cortelli S C et al. Scaling and root planing per quadrant versus one-stage full-mouth disinfection: assessment of the impact of chronic periodontitis treatment on quality of life - a clinical randomized, controlled trial. J Periodontol 2016; 87: 114-123.
Needleman I, McGrath C, Floyd P, Biddle A. Impact of oral health on the life quality of periodontal patients. J Clin Periodontol 2004; 31: 454-457.
Slade G D, Spencer A J. Development and evaluation of the Oral Health Impact Profile. Community Dent Health 1994; 11: 3-11.
Slade G D. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 1997; 25: 284-290.
Adulyanon S, Sheiham A. Oral impacts on daily performances. In Slade G D (ed) Measuring oral health and quality of life. pp 152-161. Chapel Hill: University of North Carolina, 1997.
Tsakos G, Marcenes W, Sheiham A. Evaluation of a modified version of the index of Oral Impacts On Daily Performances (OIDP) in elderly populations in two European countries. Gerodontology 2001; 18: 121-130.
McGrath C, Bedi R. Population based norming of the UK oral health related quality of life measure (OHQoL-UK). Br Dent J 2002; 193: 521-524.
Slade G D, Sanders A E. The paradox of better subjective oral health in older age. J Dent Res 2011; 90: 1279-1285.
Meusel D R, Ramacciato J C, Motta R H, Brito Junior R B, Florio F M. Impact of the severity of chronic periodontal disease on quality of life. J Oral Sci 2015; 57: 87-94.
Acharya S, Pentapati K C. Work stress and oral health-related quality of life among Indian information technology workers: An exploratory study. Int Dent J 2012; 62: 132-136.
Durham J, Fraser H M, McCracken G I, Stone K M, John M T, Preshaw P M. Impact of periodontitis on oral health-related quality of life. J Dent 2013; 41: 370-376.
He S, Wei S, Wang J, Ji P. Chronic periodontitis and oral health-related quality of life in Chinese adults: A population-based, cross-sectional study. J Periodontol 2018; 89: 275-284.
Fotedar S, Sharma K R, Fotedar V, Bhardwaj V, Chauhan A, Manchanda K. Relationship between oral health status and oral health related quality of life in adults attending H.P Government Dental College, Shimla, Himachal Pradesh - India. Oral Heal Dent Manag 2014; 13: 661-665.
Al Habashneh R, Khader Y S, Salameh S. Use of the Arabic version of Oral Health Impact Profile-14 to evaluate the impact of periodontal disease on oral health-related quality of life among Jordanian adults. J Oral Sci 2012; 54: 113-120.
Sheiham A, Steele J G, Marcenes W, Tsakos G, Finch S, Walls A W. Prevalence of impacts of dental and oral disorders and their effects on eating among older people; a national survey in Great Britain. Community Dent Oral Epidemiol 2001; 29: 195-203.
Patel R R, Richards P S, Inglehart M R. Periodontal health, quality of life, and smiling patterns - an exploration. J Periodontol 2008; 79: 224-231.
De Pinho A M, Borges C M, de Abreu M H, E Ferreira E F, Vargas A M. Impact of periodontal disease on the quality of life of diabetics based on different clinical diagnostic criteria. Int J Dent 2012; 986412. DOI: 10.1155/2012/986412.
Araújo A C, Gusmão E S, Batista J E, Cimões R. Impact of periodontal disease on quality of life. Quintessence Int 2010; 41: e111-e118.
Palma P V, Caetano P L, Leite I C. Impact of periodontal diseases on health-related quality of life of users of the Brazilian unified health system. Int J Dent 2013; 150357. DOI: 10.1155/2013/150357.
Batista M J, Lawrence H P, de Sousa Mda L. Impact of tooth loss related to number and position on oral health quality of life among adults. Health Qual Life Outcomes 2014; 12: 165.
O'Dowd L K, Durham J, McCracken G I, Preshaw P M. Patients' experiences of the impact of periodontal disease. J Clin Periodontol 2010; 37: 334-339.
Carvalho J C, Mestrinho H D, Stevens S, van Wijk A J. Do oral health conditions adversely impact young adults? Caries Res 2015; 49: 266-274.
Kutkut A, Bertoli E, Frazer R, Pinto-Sinai G, Fuentealba Hidalgo R, Studts J. A systematic review of studies comparing conventional complete denture and implant retained overdenture. J Prosthodont Res 2018; 62: 1-9.
Llanos A H, Silva C G B, Ichimura K T et al. Impact of aggressive periodontitis and chronic periodontitis on oral health-related quality of life. Braz Oral Res 2018; 32: e006.
Jansson H, Wahlin Å, Johansson V et al. Impact of periodontal disease experience on oral health-related quality of life. J Periodontol 2014; 85: 438-445.
Brennan D S, Spencer A J, Roberts-Thomson K F. Quality of life and disability weights associated with periodontal disease. J Dent Res 2007; 86: 713-717.
Saletu A, Pirker-Frühauf H, Saletu F, Linzmayer L, Anderer P, Matejka M. Controlled clinical and psychometric studies on the relation between periodontitis and depressive mood. J Clin Periodontol 2005; 32: 1219-1225.
de Souza Barbosa T, Gaviao M B, Castelo P M, Leme M S. Factors associated with oral health-related quality of life in children and preadolescents: a cross-sectional study. Oral Health Prev Dent 2016; 14: 137-148.
Marshman Z, Rodd H, Stern M et al. An evaluation of the Child Perceptions Questionnaire in the UK. Community Dent Health 2005; 22: 151-155.
Zanatta F B, Ardenghi T M, Antoniazzi R P, Pinto T M, Rösing C K. Association between gingival bleeding and gingival enlargement and oral health-related quality of life (OHRQoL) of subjects under fixed orthodontic treatment: a cross-sectional study. BMC Oral Health 2012; 12: 53.
Biazevic M G, Rissotto R R, Michel-Crosato E, Mendes L A, Mendes M O. Relationship between oral health and its impact on quality of life among adolescents. Braz Oral Res 2008; 22: 36-42.
Nurelhuda N M, Ahmed M F, Trovik T A, Åstrøm A N. Evaluation of oral health-related quality of life among Sudanese schoolchildren using Child-OIDP inventory. Health Qual Life Outcomes 2010; 8: 152.
Krisdapong S, Prasertsom P, Rattanarangsima K, Sheiham A. Relationships between oral diseases and impacts on Thai schoolchildren's quality of life: evidence from a Thai national oral health survey of 12- and 15-year-olds. Community Dent Oral Epidemiol 2012; 40: 550-559.
Tomazoni F, Zanatta F B, Tuchtenhagen S, da Rosa G N, Del Fabro J P, Ardenghi T M. Association of gingivitis with child oral health-related quality of life. J Periodontol 2014; 85: 1557-1565.
Beikler T, Flemmig T F. Oral biofilm-associated diseases: trends and implications for quality of life, systemic health and expenditures. Periodontol 2000 2011; 55: 87-103.
Ramseier C A, Anerud A, Dulac M et al. Natural history of periodontitis: disease progression and tooth loss over 40 years. J Clin Periodontol 2017; 44: 1182-1191.
Österberg T, Steen B. Relationship between dental state and dietary intake in 70-year-old males and females in Göteborg, Sweden: a population study. J Oral Rehabil 1982; 9: 509-521.
Boretti G, Bickel M, Geering A H. A review of masticatory ability and efficiency. J Prosthet Dent 1995; 74: 400-403.
Gerritsen A E, Allen P F, Witter D J, Bronkhorst E M, Creugers N H. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes 2010; 8: 126.
Craddock H L. Consequences of tooth loss: 1. The patient perspective - aesthetic and functional implications. Dent Update 2009; 36: 616-619.
Boyapati L, Wang H L. The role of stress in periodontal disease and wound healing. Periodontol 2000 2007; 44: 195-210.
Abegg C, Marcenes W, Croucher R, Sheiham A. The relationship between tooth cleaning behaviour and flexibility of working time schedule. J Clin Periodontol 1999; 26: 448-452.
Borrell L N, Crawford N D. Social disparities in periodontitis among US adults: the effect of allostatic load. J Epidemiol Community Health 2011; 65: 144-149.
Abrahamsson K H, Wennström J L, Hallberg U. Patients' views on periodontal disease; attitudes to oral health and expectancy of periodontal treatment: a qualitative interview study. Oral Health Prev Dent 2008; 6: 209-216.
Graziani F, Karapetsa D, Alonso B, Herrera D. Nonsurgical and surgical treatment of periodontitis: how many options for one disease? Periodontol 2000 2017; 75: 152-188.
Cortelli S C, Costa F O, Gargioni-Filho A et al. Impact of gingivitis treatment for diabetic patients on quality of life related to periodontal objective parameters: a randomized controlled clinical trial. Arch Oral Biol 2018; 86: 80-86.
Wong R M, Ng S K, Corbet E F, Keung Leung W. Non-surgical periodontal therapy improves oral health-related quality of life. J Clin Periodontol 2012; 39: 53-61.
Goel K, Baral D. A comparison of impact of chronic periodontal diseases and nonsurgical periodontal therapy on oral health-related quality of life. Int J Dent 2017; 9352562. DOI: 10.1155/2017/9352562.
Pereira L J, Gazolla C M, Magalhães I B et al. Treatment of chronic periodontitis and its impact on mastication. J Periodontol 2011; 82: 243-250.
Jowett A K, Orr M T, Rawlinson A, Robinson P G. Psychosocial impact of periodontal disease and its treatment with 24-h root surface debridement. J Clin Periodontol 2009; 36: 413-418.
Ozcelik O, Cenk Haytac M, Seydaoglu G. Enamel matrix derivative and low-level laser therapy in the treatment of intra-bony defects: a randomized placebo-controlled clinical trial. J Clin Periodontol 2008; 35: 147-156.
Shah M, Kumar S. Improvement of oral health related quality of life in periodontitis patients after non-surgical periodontal therapy. J Int Oral Health 2011; 3: 15-21.
Tsakos G, Bernabé E, D'Aiuto F et al. Assessing the minimally important difference in the oral impact on daily performances index in patients treated for periodontitis. J Clin Periodontol 2010; 37: 903-909.
Saito A, Ota K, Hosaka Y et al. Potential impact of surgical periodontal therapy on oral health-related quality of life in patients with periodontitis: a pilot study. J Clin Periodontol 2011; 38: 1115-1121.
Saito A, Hosaka Y, Kikuchi M et al. Effect of initial periodontal therapy on oral health-related quality of life in patients with periodontitis in Japan. J Periodontol 2010; 81: 1001-1009.
Shanbhag S, Dahiya M, Croucher R. The impact of periodontal therapy on oral health-related quality of life in adults: a systematic review. J Clin Periodontol 2012; 39: 725-735.
Makino-Oi A, Ishii Y, Hoshino T et al. Effect of periodontal surgery on oral health-related quality of life in patients who have completed initial periodontal therapy. J Periodontal Res 2016; 51: 212-220.
Kassebaum N J, Bernabé E, Dahiya M, Bhandari B, Murray C J, Marcenes W. Global burden of severe tooth loss: a systematic review and meta-analysis. J Dent Res 2014; 93 (Spec Iss): 20S-28S.
Kassebaum N J, Bernabé E, Dahiya M, Bhandari B, Murray C J, Marcenes W. Global burden of severe periodontitis in 1990-2010: a systematic review and meta-regression. J Dent Res 2014; 93: 1045-1053.
Kassebaum N J, Bernabé E, Dahiya M, Bhandari B, Murray C J, Marcenes W. Global burden of untreated caries: a systematic review and metaregression. J Dent Res 2015; 94: 650-658.
Thomason J M, Heydecke G, Feine J S, Ellis J S. How do patients perceive the benefit of reconstructive dentistry with regard to oral health-related quality of life and patient satisfaction? A systematic review. Clin Oral Implants Res 2007; 18 (Spec Iss): 168-188.
Reissmann D R, Dard M, Lamprecht R, Struppek J, Heydecke G. Oral health-related quality of life in subjects with implant-supported prostheses: a systematic review. J Dent 2017; 65: 22-40.
Strassburger C, Heydecke G, Kerschbaum T. Influence of prosthetic and implant therapy on satisfaction and quality of life: a systematic literature review. Part 1 - Characteristics of the studies. Int J Prosthodont 2006; 17: 83-93.
Strassburger C, Kerschbaum T, Heydecke G. Influence of implant and conventional prostheses on satisfaction and quality of life: A literature review. Part 2: Qualitative analysis and evaluation of the studies. Int J Prosthodont 2006; 19: 339-348.
Emami E, Heydecke G, Rompré P H, de Grandmont P, Feine J S. Impact of implant support for mandibular dentures on satisfaction, oral and general health-related quality of life: a meta-analysis of randomized-controlled trials. Clin Oral Implants Res 2009; 20: 533-544.
Boven G C, Raghoebar G M, Vissink A, Meijer H J. Improving masticatory performance, bite force, nutritional state and patient's satisfaction with implant overdentures: a systematic review of the literature. J Oral Rehabil 2015; 42: 220-233.
Sivaramakrishnan G, Sridharan K. Comparison of implant supported mandibular overdentures and conventional dentures on quality of life: a systematic review and meta-analysis of randomized controlled studies. Aust Dent J 2016; 61: 482-488.
Redford M, Drury T F, Kingman A, Brown L J. Denture use and the technical quality of dental prostheses among persons 18-74 years of age: united states, 1988-1991. J Dent Res 1996; 75 (Spec Iss): 714-725.
Albrektsson T, Blomberg S, Brånemark A, Carlsson G E. Edentulousness - an oral handicap. Patient reactions to treatment with jawbone-anchored prostheses. J Oral Rehabil 1987; 14: 503-511.
Allen P F, McMillan A S. A longitudinal study of quality of life outcomes in older adults requesting implants prostheses and complete removable dentures. Clin Oral Implant Res 2003; 14: 173-179.
Fitzpatrick B. Standard of care for the edentulous mandible: a systematic review. J Prosthet Dent 2006; 95: 71-78.
Sadowsky S J. Treatment considerations for maxillary implant overdentures: a systematic review. J Prosthet Dent 2007; 97: 340-348.
Allen P F, Thomason J M, Jepson N J, Nohl F, Smith D G, Ellis J. A randomized controlled trial of implant-retained mandibular overdentures. J Dent Res 2006; 85: 547-551.
Pavel K, Seydlova M, Dostalova T et al. Dental implants and improvement of oral health-related quality of life. Community Dent Oral Epidemiol 2012; 40 (Spec Iss): 65-70.
Kriz P, Seydlova M, Dostalova T et al. Oral health-related quality of life and dental implants - preliminary study. Cent Eur J Med 2012; 7: 209-215.
Revicki D, Hays R D, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol 2008; 61: 102-109.
Goh V, Corbet E F, Leung W K. Impact of dentine hypersensitivity on oral health-related quality of life in individuals receiving supportive periodontal care. J Clin Periodontol 2016; 43: 595-602.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Graziani, F., Music, L., Bozic, D. et al. Is periodontitis and its treatment capable of changing the quality of life of a patient?. Br Dent J 227, 621–625 (2019). https://doi.org/10.1038/s41415-019-0735-3
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0735-3
This article is cited by
-
Modelling the national economic burden of non-surgical periodontal management in specialist clinics in Malaysia using a markov model
BMC Oral Health (2024)
-
Dental anxiety and oral health-related quality of life before and after non-surgical periodontal treatment
Clinical Oral Investigations (2023)
-
Periodontitis assessed with a new screening tool and oral health-related quality of life: cross-sectional findings among general-population adults
Quality of Life Research (2023)
-
Oral manifestations of patients with systemic sclerosis: a meta-analysis for case-controlled studies
BMC Oral Health (2021)
-
The impact of nonsurgical periodontal treatment on oral health-related quality of life: a systematic review and meta-analysis
Clinical Oral Investigations (2020)