Abstract
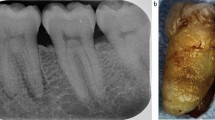
Although primarily classified as psychiatric disorders, eating disorders have a complex aetiology and presentation, with comorbidities spanning multiple disciplines, including dental complications. In some cases, general dental practitioners may be the first health professional to become aware that someone is struggling with an eating disorder. The dental team is in an ideal position to sensitively explore the presentation and signpost the patient to appropriate services while offering support and/or remedial management for dental complications of the eating disorder. Anyone from any background, gender or ethnicity may develop an eating disorder, of which the main diagnoses are anorexia nervosa, bulimia nervosa and binge eating disorder. Some of the frequently seen oral manifestations of these disorders include generalised dental erosion, caries, self-inflicted palatal or oropharyngeal trauma, atrophic mucosa, bilateral parotid gland enlargement, xerostomia and periodontal disease. The dentist's role is pivotal in recognising the possible implications of some of these findings, approaching the patient sensitively, and communicating empathetically to engage them in treatment, reducing the risk of further erosion and improving oral health and hygiene. The dental team may be able to signpost the patient to their general practitioner for onward referral or to a local eating disorder support network.
Key points
-
Eating disorders are relatively common and can affect anyone.
-
The dental team may be able to identify early signs of an eating disorder, perhaps even before the person has acknowledged that there is a problem.
-
Appropriate management within the dental service may support engagement in wider treatment of the eating disorder, improve self-esteem and support recovery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Nicholls D E, Lynn R, Viner R M. Childhood eating disorders: British national surveillance study. Br J Psychiatry 2011; 198: 295-301.
Steinhausen H-C, Jensen C M. Time trends in lifetime incidence rates of first-time diagnosed anorexia nervosa and bulimia nervosa across 16 years in a Danish nationwide psychiatric registry study. Int J Eat Disord 2015; 48: 845-850.
Micali N, Martini M G, Thomas J J et al. Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: a population-based study of diagnoses and risk factors. BMC Med 2017; 15: 12.
Franko D L, Keshaviah A, Eddy K T et al. A longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. Am J Psychiatry 2013; 170: 917-925.
Douglas L. Caring for dental patients with eating disorders. BDJ Team 2015; DOI: 10.1038/bdjteam.2015.9.
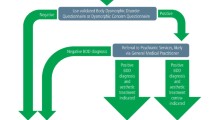
Chirravur P, Chirravur P, Gopi-Firth S. Seeking True Multidisciplinary Approach to Eating Disorders: Dentists as Case Finders. SVOA Dent 2022; 3: 123-126.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM5). 5th ed. Virginia: American Psychiatric Publishing, 2013.
Galmiche M, Déchelotte P, Lambert G, Tavolacci M P. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am J Clin Nutr 2019; 109: 1402-1413.
Ward Z J, Rodriguez P, Wright D R, Austin S B, Long M W. Estimation of Eating Disorders Prevalence by Age and Associations With Mortality in a Simulated Nationally Representative US Cohort. JAMA Netw Open 2019; DOI: 10.1001/jamanetworkopen.2019.12925.
Parker L L, Harriger J A. Eating disorders and disordered eating behaviors in the LGBT population: a review of the literature. J Eat Disord 2020; 8: 51.
Hazzard V M, Simone M, Borg S L et al. Disparities in eating disorder risk and diagnosis among sexual minority college students: Findings from the national Healthy Minds Study. Int J Eat Disord 2020; 53: 1563-1568.
Watson R J, Adjei J, Saewyc E, Homma Y, Goodenow C. Trends and disparities in disordered eating among heterosexual and sexual minority adolescents. Int J Eat Disord 2017; 50: 22-31.
Shearer A, Russon J, Herres J, Atte T, Kodish T, Diamond G. The relationship between disordered eating and sexuality amongst adolescents and young adults. Eat Behav 2015; 19: 115-119.
Chowbey P, Salway S, Ismail M. Influences on diagnosis and treatment of eating disorders among minority ethnic people in the UK. J Public Ment Health 2012; 11: 54-64.
Wales J, Brewin N, Raghavan R, Arcelus J. Exploring barriers to South Asian help-seeking for eating disorders. Ment Health Rev J 2017; 22: 40-50.
Abbas S, Damani S, Malik I, Button E, Aldridge S, Palmer R L. A comparative study of South Asian and non-Asian referrals to an eating disorders service in Leicester UK. Eur Eat Disord Rev 2010; 18: 404-409.
NHS Digital. Health Survey for England 2019. 2020. Available at https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2019/health-survey-for-england-2019-data-tables (accessed February 2023).
Stice E, Gau J M, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. J Abnorm Psychol 2017; 126: 38-51.
Fukotomi A, Austin A, McClelland J et al. First episode rapid early intervention for eating disorders: a two-year follow-up. Early Interv Psychiatry 2020; 14: 137-141.
Brown A, McClelland J, Boysen E, Mountford V, Glennon D, Schmidt U. The FREED Project (first episode and rapid early intervention in eating disorders): service model, feasibility and acceptability. Early Interv Psychiatry 2018; 12: 250-257.
Eddy K T, Tabri N, Thomas J J et al. Recovery From Anorexia Nervosa and Bulimia Nervosa at 22-Year Follow-Up. J Clin Psychiatry 2017; 78: 184-189.
General Dental Council. Preparing for Practice: dental team learning outcomes for registration. 2015. Available at https://www.gdc-uk.org/education-cpd/quality-assurance/learning-outcomes-review-process (accessed March 2022).
Elliott E, Sharma S, Omar A, Hurst D. How confidently do students address patients with psychiatric conditions in the dental clinic? A service evaluation in a UK dental school. Br Dent J 2020; 228: 376-380.
Elliott E, Sharma S, Omar A et al. A multi-centre early evaluation of the effectiveness of workshop teaching to improve the confidence of UK and Irish dental students when addressing patient mental health. Br Dent J 2021; DOI: 10.1038/s41415-021-3613-8.
Scottish Government. Scottish Eating Disorder Services Review: Full Report. 2021. Available at https://www.gov.scot/binaries/content/documents/govscot/publications/independent-report/2021/06/national-review-eating-disorder-services/documents/scottish-eating-disorder-services-review-full-report/scottish-eating-disorder-services-review-full-report/govscot%3Adocument/scottish-eating-disorder-services-review-full-report.pdf (accessed December 2022).
Westgarth D. What should the role of the dentist be in managing patients with eating disorders? BDJ In Pract 2021; 34: 12-15.
Gaspar M C M P, Sato P M, Scagliusi F B. Under the 'weight' of norms: Social representations of overweight and obesity among Brazilian, French and Spanish dietitians and laywomen. Soc Sci Med 2022; 298: 114861.
Cazzato V, Makris S. Implicit preference towards slim bodies and weight-stigma modulate the understanding of observed familiar actions. Psychol Res 2019; 83: 1825-1835.
Tomiyama A J, Carr D, Granberg E M et al. How and why weight stigma drives the obesity 'epidemic' and harms health. BMC Med 2018; 16: 123.
Russell G. Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med 1979; 9: 429-448.
Mandel L, Surattanont F. Bilateral parotid swelling: A review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93: 221-237.
Mandel L. Salivary gland disorders. Dent Clin North Am 2011; 55: 121-140.
Lo Russo L, Campisi G, di Fede O, di Liberto C, Panzarella V, Lo Muzio L. Oral manifestations of eating disorders: A critical review. Oral Dis 2008; 14: 479-484.
Monda M, Costacurta M, Maffei L, Docimo R. Oral manifestations of eating disorders in adolescent patients. A review. Eur J Paediatr Dent 2021; 22: 155-158.
Milosevic A. Eating disorders and the dentist. Br Dent J 1999; 186: 109-113.
Kisely S, Baghaie H, Lalloo R, Johnson N W. Association between poor oral health and eating disorders: Systematic review and meta-analysis. Br J Psychiatry 2015; 207: 299-305.
Bern E M, Woods E R, Rodriguez L. Gastrointestinal Manifestations of Eating Disorders. J Pediatr Gastroenterol Nutr 2016; DOI: 10.1097/MPG.0000000000001394.
Lourenço M, Azevedo Á, Brandão I, Gomes P S. Orofacial manifestations in outpatients with anorexia nervosa and bulimia nervosa focusing on the vomiting behavior. Clin Oral Investig 2018; 22: 1915-1922.
Dynesen A W, Gehrt C A, Klinker S E, Christensen L B. Eating disorders: experiences of and attitudes toward oral health and oral health behavior. Eur J Oral Sci 2018; 126: 500-506.
Douglas L M. Trauma-informed, sensitive practice. BDJ Team 2017; DOI: 10.1038/bdjteam.2017.176.
Beat. Beat eating disorders. Available at https://www.beateatingdisorders.org.uk (accessed July 2022).
Beat. Training for Medical Students and Foundation Doctors. Available at https://www.beateatingdisorders.org.uk/training-events/find-training/eating-disorders-training-for-medical-students-and-foundation-doctors (accessed July 2022).
Beat. Training for dieticians, community pharmacy and oral health teams. Available at https://www.beateatingdisorders.org.uk/training-events/find-training/training-dieticians-community-pharmacy-oral-health/ (accessed December 2022).
Author information
Authors and Affiliations
Contributions
Stephen Anderson delivered a presentation on this topic to the first UK Restorative Dentistry Conference in 2021 and subsequently wrote the paper. Shridevi Gopi-Firth reviewed and developed the paper further.
Corresponding author
Ethics declarations
Stephen Anderson is on the Board of Trustees of Beat. The authors declare no other conflicts of interest.
Rights and permissions
About this article
Cite this article
Anderson, S., Gopi-Firth, S. Eating disorders and the role of the dental team. Br Dent J 234, 445–449 (2023). https://doi.org/10.1038/s41415-023-5619-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-023-5619-x