Abstract
Background
Sodium-glucose cotransporter 2 (SGLT2) inhibitors are a relatively new class of antidiabetic drugs with demonstrated renal and cardiovascular disease benefit. This study evaluates the role of SGLT2 inhibitors on the survival of non-small cell lung cancer (NSCLC) patients.
Methods
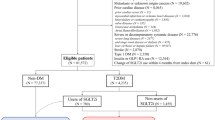
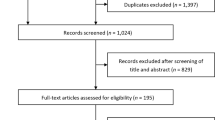
We used National Surveillance, Epidemiology and End Results (SEER)-Medicare linked data. Twenty four thousand nine hundred fifteen NSCLC patients newly diagnosed between 2014 and 2017 with pre-exiting diabetes and aged 66 years or older were included and followed to the end of 2019. Information on SGLT2 inhibitors use was extracted from the Medicare Part D file.
Results
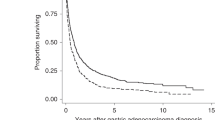
SGLT2 inhibitor use was associated with significantly reduced mortality risk after adjusting for potential confounders (HR = 0.68, 95% CI = 0.60–0.77) with stronger association for longer duration of use (HR = 0.54, 85% CI = 0.44–0.68). Further, we found that SGLT2 inhibitor use was associated with a significant reduced risk of mortality regardless of patients’ demographic, tumour characteristics and cancer treatments.
Conclusion
Our large SEER-Medicare linked data study indicates that SGLT2 inhibitors use was associated with improved overall survival of NSCLC patients with pre-existing diabetes. Further studies are needed to confirm our findings and elucidate the possible mechanisms behind the association.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data were available from the SEER-Medicare website (https://healthcaredelivery.cancer.gov/seermedicare/obtain/) on reasonable request.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu, M et al. SEER Cancer Statistics Review, 1975-2016. 2019. https://seer.cancer.gov/csr/1975_2016/. Accessed 15 Oct 2015.
Lin CC, Virgo KS, Robbins AS, Jemal A, Ward EM. Comparison of comorbid medical conditions in the national cancer database and the SEER-medicare database. Ann Surg Oncol. 2016;23:4139–48.
Deng HY, Zheng X, Zha P, Peng L, Huang KL, Qiu XM. Diabetes mellitus and survival of non-small cell lung cancer patients after surgery: a comprehensive systematic review and meta-analysis. Thorac Cancer. 2019;10:571–8.
Zhu L, Cao H, Zhang T, Shen H, Dong W, Wang L, et al. The effect of diabetes mellitus on lung cancer prognosis: a PRISMA-compliant meta-analysis of cohort studies. Medicine (Baltim). 2016;95:e3528.
Bi, G, Yao G, Bian Y, Xue L, Zhang Y, Lu T, et al. The effect of diabetes mellitus on prognosis of patients with non-small-cell lung cancer: a systematic review and meta-analysis. Ann Thorac Cardiovasc Surg. 2019. https://doi.org/10.5761/atcs.ra.19-00170.
Blonde L. Current antihyperglycemic treatment guidelines and algorithms for patients with type 2 diabetes mellitus. Am J Med. 2010;123:S12–18.
Tentolouris A, Vlachakis P, Tzeravini E, Eleftheriadou I, Tentolouris N SGLT2 inhibitors: a review of their antidiabetic and cardioprotective effects. Int J Environ Res Public Health. 2019;16:2965.
Nainggolan L FDA approves Canagliflozin, a first-in-class diabetes drug. 2013. https://www.medscape.com/viewarticle/781709 Accessed 30 Sept 2019.
ClinCalc. The top 200 of 2021. Provided by the ClinCalc Drugstats database. 2021. https://clincalc.com/DrugStats/Top200Drugs.aspx Accessed 11 Jan 2021.
CADTH. Canagliflozin (Invokana) for Type 2 Diabetes Mellitus [Internet]. Ottawa: Canadian Agency for Drugs and Technology in Health; 2015.
Zhang XL, Zhu QQ, Chen YH Li, XL Chen F, Huang JA, et al. Cardiovascular safety, long-term noncardiovascular safety, and efficacy of sodium-glucose cotransporter 2 inhibitors in patients with type 2 diabetes mellitus: a systemic review and meta-analysis with trial sequential analysis. J Am Heart Assoc. 2018;7:e007165.
Wright EM, Loo DD, Hirayama BA. Biology of human sodium glucose transporters. Physiol Rev. 2011;91:733–94.
Rosenwasser RF, Sultan S, Sutton D, Choksi R, Epstein BJ. SGLT-2 inhibitors and their potential in the treatment of diabetes. Diabetes Metab Syndr Obes. 2013;6:453–67.
Gallwitz B. The cardiovascular benefits associated with the use of sodium-glucose cotransporter 2 inhibitors—real-world data. Eur Endocrinol. 2018;14:17–23.
Cavaiola TS, Pettus J. Cardiovascular effects of sodium glucose cotransporter 2 inhibitors. Diabetes Metab Syndr Obes. 2018;11:133–48.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41:2669–701.
Kaji K, Nishimura N, Seki K, Sato S, Saikawa S, Nakanishi K, et al. Sodium glucose cotransporter 2 inhibitor canagliflozin attenuates liver cancer cell growth and angiogenic activity by inhibiting glucose uptake. Int J Cancer. 2018;142:1712–22.
Scafoglio CR, Villegas B, Abdelhady G, Bailey ST, Liu J, Shirali AS, et al. Sodium-glucose transporter 2 is a diagnostic and therapeutic target for early-stage lung adenocarcinoma. Sci Transl Med. 2018;10:eaat5933.
Villani LA, Smith BK, Marcinko K, Ford RJ, Broadfield LA, Green AE, et al. The diabetes medication Canagliflozin reduces cancer cell proliferation by inhibiting mitochondrial complex-I supported respiration. Mol Metab. 2016;5:1048–56.
Li H, Tong CW, Leung Y, Wong MH, To KK, Leung KS. Identification of clinically approved drugs indacaterol and canagliflozin for repurposing to treat epidermal growth factor tyrosine kinase inhibitor-resistant lung cancer. Front Oncol. 2017;7:288.
Lin HW, Tseng CH. A review on the relationship between SGLT2 inhibitors and cancer. Int J Endocrinol. 2014;2014:719578.
Tang H, Dai Q, Shi W, Zhai S, Song Y, Han J. SGLT2 inhibitors and risk of cancer in type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Diabetologia. 2017;60:1862–72.
Molina JR, Yang PG, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008;83:584–94.
SEER. Overview of the SEER Program. https://seer.cancer.gov/about/overview.html. Accessed 2 Nov 2021.
CMS. Medicare Program - General Information. http://www.cms.gov/MedicareGenInfo/. Accessed 24 Nov 2021.
SEER-Medicare:: Brief Description of the SEER-Medicare Database. https://healthcaredelivery.cancer.gov/seermedicare/overview/. Accessed 29 Oct 2021.
Engels EA, Pfeiffer RM, Ricker W, Wheeler W, Parsons R, Warren JL. Use of Surveillance, Epidemiology, and End Results-Medicare Data to Conduct Case-Control Studies of Cancer Among the US Elderly. Am J Epidemiol. 2011;174:860–70.
Noone AM, Lund JL, Mariotto A, Cronin K, McNeel T, Deapen D, et al. Comparison of SEER treatment data with medicare claims. Med Care. 2016;54:e55–64.
Yamamoto L, Yamashita S, Nomiyama T, Kawanami T, Hamaguchi Y, Shigeoka T, et al. Sodium-glucose cotransporter 2 inhibitor canagliflozin attenuates lung cancer cell proliferation in vitro. Diabetol Int. 2021;12:389–98.
Scafoglio C, Hirayama BA, Kepe V, Liu J, Ghezzi C, Satyamurthy N, et al. Functional expression of sodium-glucose transporters in cancer. Proc Natl Acad Sci USA. 2015;112:E4111–4119.
Blair SL, Heerdt P, Sachar S, Abolhoda A, Hochwald S, Cheng H, et al. Glutathione metabolism in patients with non-small cell lung cancers. Cancer Res. 1997;57:152–5.
Hochwald SN, Harrison LE, Rose DM, Anderson M, Burt ME. gamma-Glutamyl transpeptidase mediation of tumor glutathione utilization in vivo. J Natl Cancer Inst. 1996;88:193–7.
Kan O, Baldwin SA, Whetton AD. Apoptosis is regulated by the rate of glucose-transport in an interleukin-3 dependent cell-line. J Exp Med. 1994;180:917–23.
Shim H, Chun YS, Lewis BC, Dang CV. A unique glucose-dependent apoptotic pathway induced by c-Myc. Proc Natl Acad Sci USA. 1998;95:1511–6.
Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324:1029–33.
Yaribeygi H, Atkin SL, Butler AE, Sahebkar A. Sodium-glucose cotransporter inhibitors and oxidative stress: an update. J Cell Physiol. 2019;234:3231–7.
Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med. 2010;49:1603–16.
Multhoff G, Molls M, Radons J. Chronic inflammation in cancer development. Front Immunol. 2011;2:98.
Sugizaki T, Zhu S, Guo G, Matsumoto A, Zhao J, Endo M, et al. Treatment of diabetic mice with the SGLT2 inhibitor TA-1887 antagonizes diabetic cachexia and decreases mortality. npj Aging Mech Dis. 2017;3:12.
Ishibashi Y, Matsui T, Yamagishi S. Tofogliflozin, a highly selective inhibitor of SGLT2 blocks proinflammatory and proapoptotic effects of glucose overload on proximal tubular cells partly by suppressing oxidative stress generation. Horm Metab Res. 2016;48:191–5.
Osorio H, Coronel I, Arellano A, Pacheco U, Bautista R, Franco M, et al. Sodium-glucose cotransporter inhibition prevents oxidative stress in the kidney of diabetic rats. Oxid Med Cell Longev. 2012;2012:542042.
Ishikawa N, Oguri T, Isobe T, Fujitaka K, Kohno N. SGLT gene expression in primary lung cancers and their metastatic lesions. Jpn J Cancer Res. 2001;92:874–9.
Funding
This study is supported by the National Institutes of Health (R03CA256238).
Author information
Authors and Affiliations
Contributions
JL: Conceptualisation, methodology, formal analysis, writing–original draft and writing-review and editing. MH: Conceptualisation, methodology and writing-review and editing. YD: Conceptualisation and writing-review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was reviewed and approved by the Human Research Protection Program (HRPP) Office of Research Compliance—Indiana University, Protocol #: 2012984604.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, J., Hendryx, M. & Dong, Y. Sodium-glucose cotransporter 2 (SGLT2) inhibitors and non-small cell lung cancer survival. Br J Cancer 128, 1541–1547 (2023). https://doi.org/10.1038/s41416-023-02177-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02177-2
This article is cited by
-
Moving Beyond Cardiotoxicity Detection to Prevention: A Pharmacologic Review
Current Treatment Options in Cardiovascular Medicine (2024)